Abstract
A total of 148 health and social care practitioners were trained in skills to support behaviour change: creating opportunities to discuss health behaviours, using open discovery questions, listening, reflecting and goal-setting. At three time points post-training, use of the skills was evaluated and compared with use of skills by untrained practitioners. Trained practitioners demonstrated significantly greater use of these client-centred skills to support behaviour change compared to their untrained peers up to one year post-training. Because it uses existing services to deliver support for behaviour change, this training intervention has the potential to improve public health at relatively low cost.
Keywords: Behaviour change, Evaluation, Health and social care practitioners, Healthy Conversation Skills, Intervention, Public health, Training
Introduction
Current public health policy stresses the potential of cumulative, small changes in individual behaviour to produce significant advancements in population health. The UK Cabinet Office’s Behavioural Insights Team (‘Nudge Unit’) advocates for health behaviour change through manipulations of environmental cues (Behavioural Insights Team, 2011;Marteau, Ogilvie, Roland et al., 2011). The movement in the National Health Service (NHS) to ‘make every contact count’ recognises the opportunity that practitioners have to improve public health through supporting behaviour change in the millions of people with whom they come into contact, though it is not clear that practitioners currently have the necessary skills to do so (NHS Future Forum, 2012). This paper evaluates the impact of training front-line staff in a brief intervention, designed to provide practitioners from a range of backgrounds with the skills to support individuals in improving their health behaviour.
Sustainability and reach
Research suggests that brief interventions can be effective in producing small but important changes in behaviour (Aveyard, Begh, Parsons et al., 2012;Moyer, Finney, Swearingen et al., 2002), particularly if the intervention is motivational in content (McCambridge and Strang, 2004). A major strength of such interventions is that they can be implemented by practitioners during routine contact with patients, which removes the need to recruit participants to more formal intervention programmes. This model of intervention has several important advantages. Training practitioners to support health behaviour change during routine contact has the potential for greater impact than setting up an intervention programme additional to routine care, onto which a sample of the target population is recruited. While the latter might be suited to patient groups with specific needs, the former is more appropriate for promoting population level change. Additionally, training interventions are a sustainable option because skills are not lost when the research team leave; programmatic interventions frequently end once the research or evaluation period is over. A training intervention can also be sustained by identifying champions within participating organisations, who can ensure ongoing implementation of training and support of newly trained staff (Aoun, Shahid, Le et al., 2013).
Formal behaviour change intervention programmes are not renowned for recruiting and retaining participants from low-income and disadvantaged groups (Michie, Jochelson, Markham et al., 2009). Training front-line practitioners enables interventions to have maximum reach into these populations because relationships between practitioner and client have already been established (Lawrence, Keyte, Tinati et al., 2012). Disadvantaged populations are simultaneously most at risk of chronic disease, and least likely to meet current guidelines for healthy lifestyles or to make changes to their health behaviours (Buck and Frosini, 2012). However, there has been little research effort devoted to exploiting the potential of staff training interventions to support health behaviour change in these groups (Spanou, Simpson, Hood et al., 2010).
‘Healthy Conversation Skills’ training
This paper describes the ‘Healthy Conversation Skills’ training programme for health and social care practitioners. The programme delivers a package of skills designed to support health behaviour change in patients and clients with whom practitioners work. Like Motivational Interviewing (Rollnick and Miller, 1995) and similar approaches, Healthy Conversation Skills training offers a client-centred counselling approach to supporting behaviour change. As with other such approaches, it is based on the understanding that giving clients knowledge is insufficient to change their behaviour; they must also be motivated to change. This therefore requires a style of communication that is not reliant on advice-giving and instruction – somewhat in contrast to traditional healthcare delivery. Client-centred approaches to behaviour change are characterised instead by exploratory conversations through which the practitioner attempts to understand the world of the client and the context of the presenting problem, and supports clients to plan their own solutions. As such, clients are involved in a process of empowerment in which they take control of their issues, and hence increase their sense of self-efficacy. Trials have shown this type of approach to be more effective than no treatment, and often more effective than comparable forms of psychotherapy in eliciting behaviour change (Lundahl and Burke, 2009).
Unlike Motivational Interviewing (Hettema, Steele and Miller, 2005), Healthy Conversation Skills are not particularly complex, limited in number and simple to learn. The training was designed in recognition of the need for a programme of skills to support behaviour change that was accessible to all practitioners, including those who have little or no formal education (Barker, Baird, Lawrence et al., 2011). In contrast to Motivational Interviewing, Healthy Conversation Skills can be used in an opportunistic fashion when time is limited and do not necessarily require the building of a therapeutic relationship. The training was developed in collaboration with local health service commissioners, whose needs assessment found that their healthcare providers lacked confidence to engage clients in empowering conversations leading to behaviour change (Davies and Johnson, 2008). At the same time, observation of practice in the locality identified that opportunities to initiate behaviour change with clients were frequently missed (Lawrence, Keyte, Tinati et al., 2012). Healthy Conversation Skills training was designed specifically to equip practitioners to support improvements in diet and physical activity behaviour in their clients. However, the skills are applicable to any area of behaviour. Appendix 1 provides a summary of the training philosophy, programme and skills. Details of the training development are provided elsewhere (Barker, Baird, Lawrence, et al., 2011), and training and evaluation materials are available from the authors on request. A logic model describing the hypothesised effect of the intervention was developed at the outset and is available from the first author.
The effectiveness of Healthy Conversation Skills training in improving the diets and lifestyles of the clients of trained practitioners has been evaluated in a non-randomised, controlled trial and will be published elsewhere (Baird, Jarman, Lawrence et al., 2013). This paper describes the implementation of the training intervention and evaluation of its impact on the professional practice of health and social care practitioners.
Methods
Setting
Healthy Conversation Skills training was delivered by a training team consisting of psychologists and public health practitioners to staff working in Sure Start Children’s Centres (SSCCs) in Southampton. A relatively deprived city in the affluent south of the UK, Southampton ranks in the most deprived quarter of local authorities in England (Southampton City Council: 2013). Sure Start is a UK government initiative that provides health, education and support services for young children and their families, where emphasis is placed on reaching the most vulnerable. Local SSCC data suggest that 70 percent of the city’s children under the age of five are registered with one of the 14 Children’s Centres in Southampton. These children tend to come from families living in one of the seven ‘core SSCC areas’ defined by their poor health profile as being priority areas for intervention (Wilkinson and Inskip, 2006). Healthy eating and physical activity are identified as target issues for SSCCs, so training practitioners who work with families attending Centres in Southampton therefore represents an effective way of reaching people from more disadvantaged populations to address these health behaviours.
Staff practice in Southampton SSCCs was compared with that of staff working in SSCCs in control sites where no Healthy Conversation Skills training was delivered. Gosport and Havant, two towns on the south coast of England were chosen as control sites as they have a similar demographic profile to Southampton. At the time of data collection, Gosport had five SSCCs and Havant another nine, at which 68% and 54% of the towns’ under-fives were registered respectively. As in Southampton, a large proportion of the families attending these Centres were those defined as vulnerable or disadvantaged – Havant 28% and Gosport 38%.
Participants
All play, family support and community development workers employed by SSCCs in Southampton were asked by their managers to attend Healthy Conversation Skills training. Administrative staff, community health nurses and oral health workers were also invited. All staff completing the training were invited to attend a follow-up workshop and to receive a follow-up phone call (see Appendix 1).
Materials and procedures
Assessment of training implementation
The effectiveness of training implementation was assessed in four ways:
-
(i)
The number of training sessions held over the intervention period was recorded;
-
(ii)
The proportion of eligible staff who attended the training and the distribution of the type of staff were calculated;
-
(iii)
Observations of the number of times trainers modelled the skills during training is an assessment of the fidelity with which the trainers adhered to the principles and methods of the training. Using Flanders Interaction Analysis Technique, every ten seconds throughout each of the training sessions being observed, researchers recorded whether the trainers were asking exploratory, open discovery questions (Skill 2) thus modelling the skills they were trying to impart, whether they were speaking using other forms of question or instruction, and whether the trainees were speaking or undertaking an activity. This method of ‘ten-second event coding’ has been used previously as a practical marker of the effectiveness of the training process (Skinner, Carey, Cradock et al., 2008). An effective session was defined as one where the trainees were doing most of the talking or undertaking activities. An effective trainer of Healthy Conversation Skills should be using a good proportion of open discovery questions. The percentage of time trainers were modelling Healthy Conversation Skills and trainees were undertaking activities in the observed training sessions were calculated as measures of fidelity to the training manual.
-
(iv)
How valuable trainees perceived the training to be was assessed by asking them at the end of the last training session to rate its value on a scale of one to ten, where one was ‘not valuable’ and ten was ‘very valuable’. Trainees gave consent to be contacted by a member of the research team for a follow-up telephone call. This call was generally made between five and eight weeks after their last training session to allow time for skills to be practised. Researchers followed a standardised, semi-structured script; consent was sought for the phone calls to be audio recorded; and the recordings were then transcribed verbatim. During the phone call, trainees were asked again how valuable they felt the training had been.
The median value rating trainees gave the training and the proportion who found it of low value (scoring it 5 or less) were calculated. Trainees’ responses to being asked during the follow-up phone call about the value of the training were subject to inductive content analysis (Krippendorff, 2004). The numbers and types of positive and negative comments about the training were subsequently calculated for an overview of trainee attitudes.
Assessment of training impact on staff practice: short, medium and long term
The impact of the training on staff practice was assessed in three ways:
-
1)
Short-term impact: trainees completed questionnaires at the beginning of the first and end of the third training sessions to measure change in use of open discovery questions.
In order to assess competence in asking open discovery questions (Skill 2) trainees were asked to write down the first thing they would say in response to four written statements that came from SSCC clients. The behaviours of interest in this study were eating healthily and being physically active so the statements were: “There are lovely vegetables outside the shops, but I don’t know what they are.”; “I just don’t seem to have time to do any exercise.”; “It’s more never being taught what to eat, to cook or whatever.”; “I can’t afford for us to join a gym.” A coding matrix was developed by the research team to code and score trainee responses to the four statements into one of seven possible categories, scored from zero to six. Responses were scored according to the extent to which they allowed a client to reflect on their issues and identify a solution for themselves. Giving information by telling or making suggestions was therefore given a low score of one, whilst asking open discovery questions to help reflect and plan for change was given the highest score of six. Other responses included closed questions, the practitioner sharing their own experiences, and empathy. A total score for responses to all four statements was calculated for each participant. All responses were double-coded by two researchers to ensure consistency of coding. Early in this process, coding discrepancies were reviewed and discussed until agreement was reached and these discrepancies largely ceased to occur.
-
2)
Medium-term impact: In a post-training telephone interview trainees were asked to reflect on their use of Healthy Conversation Skills and to share any behaviour change conversations they had had since the training, in order to assess competence in all five skills (Appendix 1). During the phone call, the researcher prompted the trainee to describe how a healthy conversation started (Skill 1); what open discovery questions they used (Skill 2); who did most of the talking/listening in the conversation (Skill 4); how they helped the person plan for change by supporting them to set SMARTER goals (Skill 5); how they felt the conversation went, what worked well, how their practice had changed, how they had used the skills learnt on the course and what they might now do differently (Skill 3). Two researchers independently read every transcript and used a coding matrix to rate the practitioners’ competence in using the five skills. Competence on each skill was rated from zero to four, where zero equalled no demonstration and four indicated the highest level of competence. Competence scores were summed and the two researchers discussed and agreed the final total score. The coding matrix evolved throughout this process until coders were coding consistently. The fidelity with which the researchers followed the interview script was also assessed by checking the questions they asked against those specified by the script. This was to ensure that researchers had given trainees the opportunity to demonstrate competence in each of the five skills.
-
3)
Long-term impact: Researchers observed conversations between trained practitioners and clients at SSCC group activity sessions one year post-training to assess competence in four of the five skills. These observations were compared with observations of staff in the control area. Most sessions were attended by two observers who undertook to observe different members of staff using an observation tool developed by the research team (available from the first author).
As well as recording details of the date, time and location of each group session observed, they captured staff use of four of the five Healthy Conversation Skills. In the context in which the observations were carried out, it was not possible to record use of reflection (Skill 3). We intended to observe all trainees and liaised with the Centres to attend as many sessions as possible in which trained staff members were working. Consent was at the Centre level initially, but staff members were briefed before the session commenced to explain the rationale for the observation. No-one made any objections to the presence of the observers. There were no specific sampling criteria as all trainees present in the session were observed and each was observed in one session only.
Competence in identifying or creating an opportunity to have a healthy conversation (Skill 1) was recorded in one of five categories which described how the healthy conversation began. Skill 2 was assessed through making a tally of the questions asked and categorising them into either open discovery questions or other responses. Observers recorded who did most of the talking in the conversation and how much of the total conversation time the practitioner spent asking open discovery questions as evidence of time spent listening (Skill 4). Any communication to support SMARTER planning was recorded and used as evidence of Skill 5.
Ethical considerations
As the training programme and associated evaluation were undertaken as part of staff continuing professional development, a submission was not required by the local ethics committee. However, researchers followed universal ethical principles throughout. All trainees completed a registration sheet and consented to take part in the training.
Results
Training implementation
Between May 2009 and January 2011, 22 courses of Healthy Conversation Skills training of three sessions each were delivered. Of the 210 practitioners working across 14 SSCCs in Southampton who were eligible to attend, 148 completed the training, giving a response rate or reach of 70%. The largest staff group who attended were play workers/supervisors (43%), followed by community development workers (18%) and family support workers (17%). Fewer community health nurses and oral health practitioners (15%), and management and administrative staff (7%) participated. The managers of some staff groups chose to make the training mandatory, while others did not. The higher proportions of play and community development workers who received training are a reflection of this decision. Three trainees were male.
One complete training programme was observed in November 2010. The majority of each training session (76% overall) was spent with the trainees involved in activities or speaking. When trainers were speaking, they were modelling the use of open discovery questions nearly a third of the time. When asked how valuable they felt the training had been on a scale from 1-10, trainees gave it a median rating of 8 (IQR:7-9). Only 6% of the trainees gave a score of less than 5, indicating little or no perceived value. Content analysis of the follow-up phone call transcripts showed that 84% of trainees gave some positive feedback and 45% some negative feedback (some made positive and negative comments about different aspects of the training). A breakdown of the positive feedback indicated that 35% of trainees commented on the training content (eg “I think examples of how it could be done was very useful; I think most of it was useful actually.”); 31% on using the skills in practice (eg “I think about how can I ask this question, making it an open question and letting them give me a solution”); 42% on reflection and professional development (eg “It made me really think about what I wasn’t saying as much as what I was”); and 48% made general observations (eg “I enjoyed it, it was really good”). Twenty-seven percent of trainees made a negative comment about the training content (eg “The recorder thing wasn’t very nice, it did really throw me actually”); 6% about using skills in practice (eg “I can’t say that going on that course has made any changes to how I would have a conversation; I wouldn’t stop and think about what I will be saying with someone”); 27% about the name and length of the training (eg “We went expecting it to be about food and of course it wasn’t when we got there”); and just 3% made a negative general observation (eg “not particularly useful to be quite honest”).
Training impact
Short term impact on staff practice
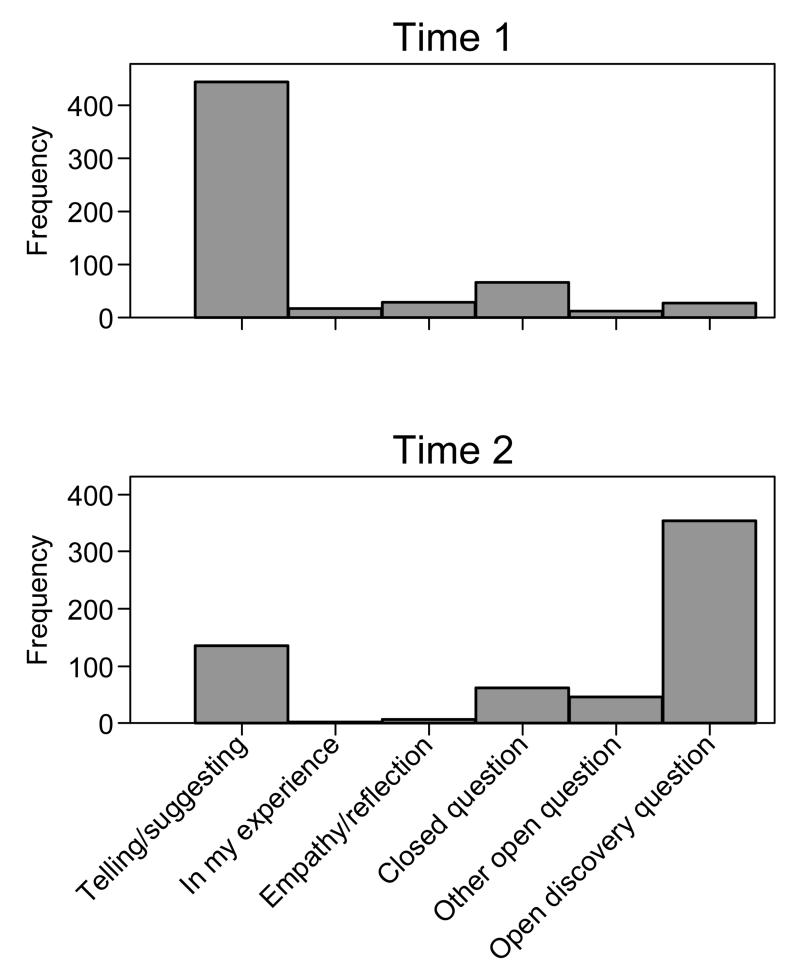
All 148 practitioners who completed Healthy Conversation Skills training provided responses to written statements before and immediately after training, and 143 of them provided at least one response that could be coded. Numbers of the seven possible responses to each of the statements were compared pre- and post-training using Wilcoxon matched-pairs signed rank test. Numbers of trainees using open discovery questions at each time point were compared using the same test. Trainees responded to these statements significantly differently after training (P<0.001) (Figure 1). Numbers of open discovery questions used by trainees increased after training from 16 to 321, and giving information or making suggestions decreased from 428 to 130. The number of trainees using open discovery questions went up from 13 to 114; 78% of trainees who had used no open discovery questions before training, used at least one afterwards.
Figure 1. Short term impact on staff practice.
Types of response provided by trainees to four written statements about health behaviours immediately before and after training.
(n = 143)
Medium term impact on staff practice
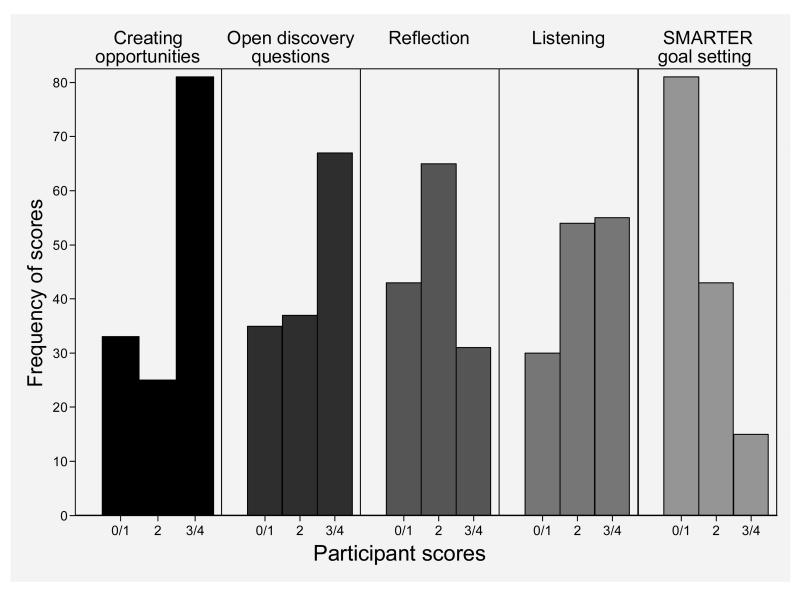
Data on trainees’ competence five to eight weeks after training were extracted from transcripts of the follow-up phone calls and were available for 139 trainees. Of the nine trainees for whom there are no data available, the recorder failed four times, three trainees asked not to be recorded, and two had left SSCC employment. Competence scores for trainees on each of the five skills demonstrated during the follow-up phone call were calculated, summed and multiplied by five to give an overall percentage rating of competence. Scores on each of the five skills were plotted and median scores for each skill calculated. The median overall competence rating for all these trainees was 55% (IQR: 35-70). Figure 2 shows the number of participants and their range of scores on each of the five competencies. Variation in the median scores suggests that trainees were more competent in some areas than others. They had moderate to high levels of skill in finding opportunities to have healthy conversations (median score 3 (IQR: 2-3)) and in using open discovery questions (median score 2 (IQR: 0-4)); however, these conversations did not include SMARTER goal-setting (median score 1 (IQR: 0-2)).
Figure 2. Medium term impact on staff practice.
Trainees’ scores on the five competencies (data extracted from the follow-up phone call).
(n = 139)
Long term impact on staff practice
One year post-training, 168 conversations with clients were observed involving 70 trainees at 12 SSCCs in Southampton. At the same time, 89 conversations were observed involving 41 practitioners at 10 SSCCs in the control areas, where staff had not been trained in Healthy Conversation Skills. Whilst the control area was demographically similar to the intervention area with a similar number of SSCCs, they had a smaller pool of staff, most of whom we observed.
Numbers of conversations observed and total numbers of practitioners involved in the observations were calculated for the intervention and control areas (Table 1). A practitioner was considered to have shown competence in Skill 1 if they created an opportunity or started a healthy conversation with a client. Asking more than two open discovery questions was considered evidence of competence in Skill 2. Competence in Skill 4 was reflected in the practitioner spending more time listening than talking, and at least half the total conversation time spent asking open discovery questions. Any communication to support SMARTER planning was used as evidence of Skill 5. A random effects logistic model was used to compare the frequencies with which these skills were used between the two areas. This analysis took account of the fact that some of the practitioners were observed in more than one conversation.
Table 1. Long term impact on staff practice.
Number(%) of conversations containing evidence of each of four competencies in Intervention and Control areas
| Intervention (Trained staff) n=168 | Control (Untrained staff) n=89 | P-value for comparison | |
|---|---|---|---|
| Practitioner created opportunity for a healthy conversation (skill 1) | 80 (48%) | 26 (29%) | 0.02 |
| More than two open discovery questions used (skill 2) | 99 (59%) | 18 (20%) | <0.001 |
| More time spent listening than giving information (skill 4) | 141 (84%) | 60 (67%) | 0.02 |
| At least half the time spent asking open discovery questions (skills 2 and 4) | 79 (47%) | 10 (11%) | <0.001 |
| Questions asked supporting SMARTER planning (skill 5) | 16 (10%) | 1 (1%) | 0.053 |
Skills 1, 2 and 4 were seen significantly more in the intervention site than in the control site. Although there were more occasions when Skill 5 was observed in the intervention site, there was no significant difference in its use (Table 1).
Discussion
These data suggest that health and social care practitioners can be trained to use communication skills to support behaviour change as a brief intervention. Healthy Conversation Skills training changed staff practice in the short, medium and long term. Thorough implementation of this training intervention is demonstrated by the fact that 22 training courses were successfully run and 70% of eligible practitioners in the intervention area were trained. This confirms that the intervention reached the target population of practitioners. In addition, the majority of trainees felt the training was valuable to their practice. Evidence of fidelity of training delivery and adherence to the training philosophy are shown by the way trainers ensured trainees’ involvement in activities and discussions for the great majority of time they were in training. When trainers were speaking, almost a third of this time was spent asking open discovery questions, modelling a key skill of the training.
The impact of the training intervention on staff practice was demonstrated by the dramatic increase in use of open discovery questions immediately post-training, indicating understanding of this key skill and the ability to produce a more exploratory response; high levels of competence in three of the five Healthy Conversation Skills several weeks post-training; and, compared to their untrained peers, significantly higher use of most skills in practice one year post-training. It should be noted however that not all five skills were taken up and used to the same degree. Unlike use of open discovery questions, listening, reflecting, and creating opportunities, the use of SMARTER goal-setting was minimal and not significantly higher in the intervention than the control area. Subsequent review and reflection on the training programme and data from the follow-up phone calls suggested that trainers may have provided insufficient support to trainees to allow them to acquire and practise SMARTER goal-setting. The training programme has subsequently been revised to address this issue.
Strengths and limitations
Not all practitioners working in SSCCs received Healthy Conversation Skills training, raising the possibility that the trainees represent a biased sample of those eligible. However, there are two aspects of the study design that make this unlikely. First, the large majority of eligible practitioners were trained; second, training was made mandatory for most staff groups and a considerable amount of energy was put into ensuring that trainees were available to attend all the training sessions. For these reasons, we are confident that the trainees were not in some way self-selected, and that the changes in practice we observed are not the result of this group being particularly motivated to change.
It is acknowledged that the evaluations rely on self-report data and phone calls and observations conducted by the research team, which may have biased the findings. Being interviewed by the training team may have led trainees to feel under pressure during the follow-up phone calls and thus exaggerate or invent evidence of Healthy Conversation Skills’ use. Similarly, trainees may not have behaved in the way they would usually whilst being observed. However, the use of a variety of evaluation tools, assessment at multiple time points and collection of a large amount of data from each trainee were methods adopted to overcome this potential for bias. Whilst the evaluation tools were not validated against other instruments, they were developed and piloted by the research team to be fit for purpose. Attention was paid to the rigour with which assessment criteria were applied. For example, the follow-up phone calls were conducted using a standardised script, and the fidelity with which the interviewers adhered to the script was assessed and considered when analysing the data. Each transcript was coded for evidence of competency in use of Healthy Conversation Skills by two researchers independently, and a final coding was produced through discussion. One member of the research team (WL) trained all the observers (CB, MJ, SC, TT, RB), attended many of the sessions with them and reviewed all the observation data regularly with them to ensure a consistent approach. The consistency of findings in the current study suggests that the change in staff practice is unlikely to be wholly due to bias or measurement artefact.
It would have been helpful to assess reflective skills at one year post-training and to have undertaken additional evaluations of use of all skills over time. The intention was to record reflection skills on the observation sheet but in the event it was not possible to interview a sufficient number of staff, so these data were not collected. Ongoing delivery of this training needs to address these limitations.
Interpretation
There may be a number of reasons why Healthy Conversation Skills appear to be taken up more easily than other training interventions. In trials of the effectiveness of Motivational Interviewing training, little overall change in staff practice and a lack of basic proficiency have been reported (Forsberg, Ernst and Farbring, 2011;Moore, Moore and Murphy, 2012). It is recognised that Motivational Interviewing is a complex and skilful therapy, which needs to be learnt over time with skills embedded gradually through practice (Hettema, Steele and Miller, 2005). In contrast, Healthy Conversation Skills training was designed to be accessible to practitioners from a range of backgrounds, many with limited counselling experience, to equip them to support clients in an opportunistic way. Though the client-centred philosophy of Healthy Conversation Skills is similar to that of Motivational Interviewing, the five skills on which our training is based are easy to understand, and the techniques used to acquire these skills are uncomplicated. Healthy Conversation Skills training is also designed in a way that allows trainees to practise the skills between sessions, and offers on-going support using a variety of methods including self-reflection tools, the follow-up phone call and the workshop. We have also encouraged the Centres to identify champions and where this has been successful there is a clearer workplace support mechanism in place for the trainees, for instance a requirement for evidence of use of the skills in staff appraisals.
The style adopted for the delivery of Healthy Conversation Skills training may also have enhanced take-up of skills and increased trainees’ self-efficacy for supporting behaviour change. The trainers modelled the non-didactic, counselling, facilitative style they wished to promote in their trainees. Trainers used open discovery questions nearly a third of the time when they were talking, and trainees spent most of the training time talking and participating in activities. These findings indicate a more interactive, less didactic training style than traditional training methods which involve a great deal of instruction and a smaller contribution from trainees. This participatory style of interaction has shown to be more effective than traditional approaches in supporting clients and patients to change their lifestyles, partly because they increase client and patient self-efficacy (Abraham and Gardner, 2009;Lorig and Holman, 2003). A recent trial demonstrated that the self-efficacy of nutritionists working for the Women, Infants, and Children programme in the USA increased as their self-assessed level of Motivational Interviewing skills increased (Marley, Carbonneau, Lockner et al., 2011). Similarly, we have shown that increased practitioner competence in using Healthy Conversation Skills was associated with increased confidence in having conversations with clients about healthy eating (Black, Lawrence, Cradock et al., 2012). The process of learning and using these skills is somewhat circular; practitioners trained in Healthy Conversation Skills were more likely to feel they were able to use them with clients and hence more likely to see the benefits of using them (Tinati, Lawrence, Ntani et al., 2012). It is therefore crucial to provide opportunities to practise new skills when attempting to change staff practice.
One reason that Healthy Conversation Skills training reached a high proportion of practitioners was that it was developed and implemented in close collaboration with local commissioners and service providers who had identified a need for their practitioners to receive training in skills to support health behaviour change in patients and clients. Discussions with service providers of the findings from the research team’s formative work influenced the content and mode of delivery of the training (Lawrence, Keyte, Tinati, et al., 2012). In some cases, commissioners made Healthy Conversation Skills training a requirement of their service providers, therefore mandatory for all front-line staff. In this way, every effort was made to support the implementation of the training, recruitment of trainees and engagement in follow-up activities. Such alliances have been highlighted as an important step in improving population health (Campbell and Murray, 2004).
Implications for policy and practice
The findings of this study have implications for those wishing to improve public health through promoting health behaviour change. This study demonstrates that front-line practitioners at all levels can be given training in client-centred skills to support behaviour change and that changes to their practice seem to persist over time. We have shown that this training can be made accessible and acceptable to staff, who can use these skills during routine care.
An example of the power of a client-centred approach to improve health care services is provided by De Haan in her account of the transformation of maternity services in former USSR countries (de Haan, 2010). After ten days of training staff in client-centred techniques, with six biannual refresher sessions, the quality of maternity care was revolutionised and outcomes dramatically improved for women and their babies. She attributes the improvements to successful empowerment of both staff and patients, and concludes that training to improve client-provider communication is a sustainable and cost-effective way to enhance the quality of health services. Data from our training intervention suggest that this may also be true for health and social care services.
In the UK, the NHS Health Trainer Service is a demonstration of the value of brief, client-centred interventions in improving health behaviours in the community. Early evaluations of the service show that in the groups of clients who engage fully with a health trainer, body mass index decreases, diet quality and level of physical activity improve, and self-efficacy and perceptions of health and well-being increase (Gardner, Cane, Rumsey et al., 2012). However, these evaluations also show that recruitment and engagement of clients can be challenging. Models, such as the one adopted by Healthy Conversation Skills training, aim to improve the capability of existing services to deliver lifestyle change support to clients thus avoiding the problem of recruitment to a new service. This approach has huge potential, and unlike more programmatic interventions, is low in cost. A recent trial of this kind of intervention, where general practitioners were trained in behaviour change counselling, showed small by encouraging effects on patients’ intentions to change their health behaviour (Butler, Simpson, Hood et al., 2013).
Brief interventions delivered by large numbers of practitioners over a sustained period of time have the potential to initiate change in substantial numbers of individuals. Over a period of time, this may lead to population level shifts in behaviour and hence in risk factors for chronic disease. Delivering interventions to improve health behaviour through routine care also provides an opportunity to work with people living in disadvantaged communities, who are the group least likely to engage with formal intervention programmes but simultaneously at greatest risk of disease in UK society. Methods of supporting this target group to improve their health behaviour must therefore be a priority in efforts to improve population health. This paper provides support for the role of health psychology in the area of public health and community empowerment (Murphy and Bennett, 2004).
Acknowledgments
The staff of Sure Start Children’s Centres, Southampton City Council and NHS Southampton City are due our grateful thanks; in particular Sue Thompson, Liz Taylor, and Stephanie Ramsay, for their considerable help in facilitating the delivery and evaluation of the training programme. We are grateful to Jeanette Keyte for her contributions to the design and delivery of the training programme, to Vanessa Cox and the MRC LEU computing team for their invaluable help with the data, and to all working on the Southampton Initiative for Health. This project was supported by funding from the National Institute for Health Research, Nutrition Biomedical Research Centre, Southampton Centre for Biomedical Research.
Appendix
1. Healthy Conversation Skills training description
Communication is enhanced through practitioners developing the skill of asking open-ended, or open discovery, questions - those that generally begin with “how” and “what”. Such healthy conversations allow a patient or client to explore an issue, identify barriers, and generate solutions that can be reviewed with the practitioner at their next encounter. Training aims to increase self-efficacy and sense of control of both practitioners and their patients and clients. The five core skills are:
To be able to identify and create opportunities to hold “healthy conversations”.
To use open discovery questions (those that specifically support exploring of issues, barriers and priorities; problem-solving; and goal-setting).
To reflect on practice.
To listen rather than provide information.
To support goal-setting through SMARTER planning (Specific, Measurable, Action-oriented, Realistic, Timed, Evaluated, Reviewed goals).
Healthy Conversation Skills training consists of three 3-hour group sessions over three to five weeks to allow time for practising and reflecting on skills. Training is delivered by a team of researchers experienced in group work and behaviour change, to a group of between 5 and 15 trainees. This is followed by a period of on-going support, including a phone call from one of the trainers to find out how skills are being implemented in practice and a three hour follow-up workshop approximately three months after training. The phone call and workshop allow trainees to reflect on the training, how they have implemented their new skills, any barriers to their implementation and plans for continued or increased use, including embedding self and peer reflection as part of normal practice. Both follow-up activities are also opportunities to collect evaluation data to assess the effectiveness of the training. Undertaking these activities at approximately 1 month and 3 months post-training was based on an assumption that staff would have had opportunities to practise their new skills, and if they were finding this challenging, it would be a good time to reflect on this and make plans for progress.
Footnotes
“No conflicting interests”.
[The Training Manual and all materials mentioned within this article are available from the first author upon request]
References
- Abraham C, Gardner B. What psychological and behaviour changes are initiated by ‘expert patient’ training and what training techniques are most helpful? Psychology and Health. 2009;24(10):1153–1165. doi: 10.1080/08870440802521110. [DOI] [PubMed] [Google Scholar]
- Aoun S, Shahid S, Le L, Packer T. The role and influence of ‘Champions’ in a community-based lifestyle risk modification programme. Journal of Health Psychology. 2013;18(4):528–541. doi: 10.1177/1359105312449194. [DOI] [PubMed] [Google Scholar]
- Aveyard P, Begh R, Parsons A, West R. Brief opportunistic smoking cessation interventions: a systematic review and meta-analysis to compare advice to quit and offer of assistance. Addiction. 2012;107(6):1066–1073. doi: 10.1111/j.1360-0443.2011.03770.x. [DOI] [PubMed] [Google Scholar]
- Baird J, Jarman M, Lawrence W, Black C, Davies J, Tinati T, Begum R, Mortimore A, Robinson S, Margetts B, Cooper C, Barker M, Inskip H. What is the effect of a behaviour change intervention on the diets and physical activity levels of women attending Sure Start Children’s Centres in Southampton? Findings from a non-randomised controlled trial. 2013 doi: 10.1136/bmjopen-2014-005290. (Under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker M, Baird J, Lawrence W, Jarman M, Black C, Barnard K, Cradock S, Davies J, Margetts B, Inskip H, Cooper C. The Southampton Initiative for Health A Complex Intervention to Improve the Diets and Increase the Physical Activity Levels of Women from Disadvantaged Communities. Journal of Health Psychology. 2011;16(1):178–191. doi: 10.1177/1359105310371397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behavioural Insights Team . Behavioural Insights Team: annual update 2010-11. Crown; London: 2011. [Google Scholar]
- Black C, Lawrence W, Cradock S, Ntani G, Tinati T, Jarman M, Begum R, Inskip H, Cooper C, Barker M, Baird J. Healthy conversation skills: increasing competence and confidence in front-line staff. Public Health Nutrition. 2012;17(3):700–707. doi: 10.1017/S1368980012004089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buck D, Frosini F. Clustering of unhealthy behaviours over time: implications for policy and practice. The King’s Fund; London: 2012. [Google Scholar]
- Butler CC, Simpson SA, Hood K, Cohen D, Pickles T, Spanou C, McCambridge J, Moore L, Randell E, Alam M, Kinnersley P, Edwards A, Smith C, Rollnick S. Training practitioners to deliver opportunistic multiple behaviour change counselling in primary care: a cluster randomised trial. British Medical Journal. 2013;346 doi: 10.1136/bmj.f1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell C, Murray M. Community Health Psychology: Promoting Analysis and Action for Social Change. Journal of Health Psychology. 2004;9(2):187–195. doi: 10.1177/1359105304040886. [DOI] [PubMed] [Google Scholar]
- Davies J, Johnson M. Southampton Sure Start Children’s Centres Training Needs Assessment: Final Report. Southampton City PCT; Southampton: 2008. [Google Scholar]
- de Haan O. From patient to client. Patient Education and Counselling. 2010;81:442–447. doi: 10.1016/j.pec.2010.09.028. [DOI] [PubMed] [Google Scholar]
- Forsberg L, Ernst D, Farbring CA. Learning motivational interviewing in a real-life setting: A randomised controlled trial in the Swedish Prison Service. Criminal Behaviour and Mental Health. 2011;21(3):177–188. doi: 10.1002/cbm.792. [DOI] [PubMed] [Google Scholar]
- Gardner B, Cane J, Rumsey N, Michie S. Behaviour change among overweight and socially disadvantaged adults: A longitudinal study of the NHS Health Trainer Service. Psychology and Health. 2012;27(10):1178–1193. doi: 10.1080/08870446.2011.652112. [DOI] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational Interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Krippendorff K. Content Analysis: An Introduction to its Methodology. Second Edition ed Sage Publications, Inc.; 2004. [Google Scholar]
- Lawrence W, Keyte J, Tinati T, Haslam C, Baird J, Margetts B, Swift J, Cooper C, Barker M. A mixed-methods investigation to explore how women living in disadvantaged areas might be supported to improve their diets. Journal of Health Psychology. 2012;17(6):785–798. doi: 10.1177/1359105311425271. [DOI] [PubMed] [Google Scholar]
- Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Annals of Behavioral Medicine. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- Lundahl B, Burke BL. The effectiveness and applicability of Motivational Interviewing: a practice-friendly review of four meta-analyses. Journal of Child Psychology. 2009;65(1):1232–1245. doi: 10.1002/jclp.20638. [DOI] [PubMed] [Google Scholar]
- Marley SC, Carbonneau K, Lockner D, Kibbe D, Trowbridge F. Motivational Interviewing Skills are Positively Associated with Nutritionist Self-efficacy. Journal of Nutrition Education and Behavior. 2011;43(1):28–34. doi: 10.1016/j.jneb.2009.10.009. [DOI] [PubMed] [Google Scholar]
- Marteau TM, Ogilvie D, Roland M, Suhrcke M, Kelly MP. Judging nudging: can nudging improve population health? British Medical Journal. 2011;342:d228. doi: 10.1136/bmj.d228. [DOI] [PubMed] [Google Scholar]
- McCambridge J, Strang J. The efficacy of single-session Motivational Interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: results from a multi-site cluster randomised trial. Addiction. 2004;99:39–52. doi: 10.1111/j.1360-0443.2004.00564.x. [DOI] [PubMed] [Google Scholar]
- Michie S, Jochelson K, Markham W, Bridle C. Low-income groups and behaviour change interventions: a review of intervention content, effectiveness and theoretical frameworks. Journal of Epidemiology and Community Health. 2009;63(8):610–622. doi: 10.1136/jech.2008.078725. [DOI] [PubMed] [Google Scholar]
- Moore GF, Moore L, Murphy S. Integration of Motivational Interviewing into Practice in the National Exercise Referral Scheme in Wales: A Mixed Methods Study. Behavioural and Cognitive Psychotherapy. 2012;40(3):313–330. doi: 10.1017/S1352465811000531. [DOI] [PubMed] [Google Scholar]
- Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: a meta-analytic review of controllled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97:279–292. doi: 10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- Murphy S, Bennett P. Health Psychology and Public Health: Theoretical Possibilities. Journal of Health Psychology. 2004;9(1):13–27. doi: 10.1177/1359105304036099. [DOI] [PubMed] [Google Scholar]
- NHS Future Forum . NHS Future Forum - Summary Report second phase. Department of Health; London: 2012. [Google Scholar]
- Rollnick S, Miller WR. What is Motivational Interviewing? Behavioural and Cognitive Psychotherapy. 1995;23:325–334. doi: 10.1017/S1352465809005128. [DOI] [PubMed] [Google Scholar]
- Skinner TC, Carey ME, Cradock S, Dallosso HM, Daly H, Davies MJ, Doherty Y, Heller S, Khunti K, Oliver l, the DESMOND Collaborative ‘Educator talk’ and patient change: some insights from the DESMOND (Diabetes Education and Self-Management for Ongoing and Newly Diagrnosed) randomized controlled trial. Diabetic Medicine. 2008;25:1117–1120. doi: 10.1111/j.1464-5491.2008.02492.x. [DOI] [PubMed] [Google Scholar]
- Southampton City Council Index of Multiple Deprivation. 2013;2010:8-1–0013. [Google Scholar]
- Spanou C, Simpson SA, Hood K, Edwards A, Cohen D, Rollnick S, Carter B, McCambridge J, Moore L, Randall E, Pickles T, Smith C, Lane C, Wood F, Thornton H, Butler CC. Preventing disease through opportunistic, rapid engagement by primary care teams using behaviour change counselling (PRE-EMPT): protocol for a general practice-based cluster randomised trial. BMC Family Practice. 2010;11(69) doi: 10.1186/1471-2296-11-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinati T, Lawrence W, Ntani G, Black C, Cradock S, Jarman M, Pease A, Begum R, Inskip H, Cooper C, Baird J, Barker M. Implementation of new Healthy Conversation Skills to support lifestyle changes - what helps and what hinders? Health and Social Care in the Community. 2012;20(4):430–437. doi: 10.1111/j.1365-2524.2012.01063.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson R, Inskip H. The health and wellbeing of women in Southampton’s communities: An analysis of the Southampton Women’s Survey. Southampton City NHS Primary Care Trust; 2006. [Google Scholar]