Abstract
Background
The aging kidney is marked by a chronic inflammation, which may exacerbate the progression of renal dysfunction, as well as increase the susceptibility to acute injury. The identification of strategies to alleviate inflammation may have translational impact to attenuate kidney disease.
Methods
We tested the potential of ashwaganda, sutherlandia and elderberry on tumor necrosis factor-α (TNF-α) and lipopolysaccharide (LPS) induced chemokine (CCL2 and CCL5) expression in vitro.
Results
Elderberry water-soluble extract (WSE) was pro-inflammatory, while sutherlandia WSE only partially attenuated the TNF-α-induced changes in CCL5. However, ashwaganda WSE completely prevented TNF-α-induced increases in CCL5, while attenuating the increase in CCL2 expression and NF-κB activation. The same pattern of ashwagandha protection was seen using LPS as the pro-inflammatory stimuli.
Conclusions
Taken together, these results demonstrate the ashwaganda WSE as a valid candidate for evaluation of therapeutic potential for the treatment of chronic renal dysfunction.
Keywords: Ashwagandha, CCL2, CCL5, Kidney, NF-κB
Background
Inflammation is a key component of the aging kidney [1]; in both human [2, 3] and animal studies from our laboratory [4], it has been shown that a significant number of genes whose expression is increased in aging are pro-inflammatory. The kidney may be uniquely sensitive to inflammation as it is a source for cytokine and chemokine synthesis within the tubular epithelium [5], and due to the high blood flow, it is continually exposed to circulating pro-inflammatory mediators. There are significant data linking inflammation to the loss of renal function [6, 7]; the pro-inflammatory environment may also be one of the mechanisms contributing to the increased severity of acute injury in the aging kidney [8].
Fibrosis is an accumulation of matrix, predominantly collagen, which is associated with loss of organ function as normal tissue is replaced by scar tissue [9]. The kidney is a prototypical example of an organ in which progressive fibrosis leads to organ failure [10, 11]. A signaling pathway that links inflammation and fibrosis in the kidney is NF-κB. This transcription factor has a long-recognized role as a pro-inflammatory mediator [12, 13]. A number of stimuli induce NF-κB activity in the kidney, including TNF [14] and angiotensin II [15] – both of which are associated with chronic kidney disease (CKD) [16, 17]. The list of NF-κB target genes is lengthy but includes CCL2 and CCL5 (RANTES) [18, 19].
CCL5 is a chemoattractant for monocytes [20]; CCR1 and CCR5 are receptors for CCL5 [21]. A number of studies now link CCL5, and other chemokines, including CCL21 and its receptor CCR7, to renal fibrosis. There is a parallel increase in the gene expression of CCL5 and collagen 1α1 in a mouse model of progressive fibrosis [22]. In a rat model of CKD, attenuation of inflammation is associated with decreased CCL5 expression and reduced fibrosis [23]. A CCR1 antagonist (BX471) is associated with reduction in fibrosis in multiple animal models [24, 25]. CCL2 (monocyte chemotactic protein-1; MCP-1) is a C-C chemokine that is a ligand for the CCR2 receptor and is a potent chemoattractant for leukocytes, T lymphocytes and NK (natural killer) cells [26]. Elevated urinary CCL2 is associated with the development of fibrosis in human renal allografts and may be a poor predictor of outcome [27, 28]. Thus, elevation of CCL2 and CCL5 may contribute the progressive fibrosis important in CKD.
Published data demonstrates that sutherlandia [29] and elderberry [30, 31] have anti-inflammatory effects. It is unclear as to whether these effects extend to renoprotection and, in fact, an elderberry-rich extract enriched in anthocyanins did not improve renal function in a small clinical trial of postmenopausal women [32]. In contrast, ashwagandha (Withania somnifera) has been demonstrated to be renoprotective via both antioxidant [33–35] and anti-inflammatory effects [36]. The current studies were designed to screen water-soluble extracts of ashwaganda, sutherlandia and elderberry for anti-inflammatory effects in renal epithelial cells.
Methods
Cell culture
NRK-52E cells (ATCC #CRL-1571) were grown in Dulbecco’s modified eagle medium F-12 (DMEM/F12, 1:1) without phenol red, but with L-glutamine and 15 mM HEPES (Gibco #11039-021). The growth media also contained 5 % fetal bovine serum (FBS; Atlanta Biologicals #S11150), 50 U/ml penicillin, and 50 mg/ml streptomycin (Gibco #15140-122). A NRK-52E:NF-κB reporter cell line was generated by stably transposing the insulated NF-κB pathway reporter DNA [37] into the chromatin of NRK-52E cells. The stable transfects were selected in DMEM/F12 containing 5 % FBS, and 1 μg/ml puromycin dihydrochloride (Sigma #P9620-10 ml). Both cell types were cultured at 37 °C in 5 % CO2. Cells were washed with 1X Dulbecco’s phosphate buffered saline (DPBS; Gibco #14190-144), harvested with TrypLE Express (Gibco #12604-021), and centrifuged at 1,500xrpm for 5 min at room temperature (RT).
Dosing
An aqueous extract of Sutherlandia frutescens was prepared using the method described by Fernandes [38]. Briefly, 10 g of S. frutescens (ground powder of vegetative parts of S. frutescens purchased from Big Tree Nutraceutical, Fish Hoek, South Africa) was added to 250 mL of boiling water. This mixture was kept in a 100 °C water bath for 1 h, with stirring every 10 min. This mixture was allowed to cool overnight, in the dark. The decoction was transferred into 50 mL sterilized centrifuge tubes, and centrifuged at 2000×g for 20 min. The supernatant was sterile-filtered using a 0.2 μm nylon filter (Fisher Scientific, Pittsburgh, PA, USA), and then stored in 1.0 mL aliquots at −80 °C until used. The product identity was confirmed using HPLC/ELSD and HPLC/UV [39], which determined that the S. frutescens used in this study contained 3.3 % (w/w) of sutherlandioside B, a specific biomarker of this medicinal plant [39, 40].
The Ashwagandha used for these experiments was obtained from a commercial supplement (Now Foods, Bloomingdale, IL, USA). Each capsule contained 450 mg of a standardized extract containing a minimum of 2.5 % total withanolides. The contents of several capsules were weighed and dissolved in endotoxin-free, double-distilled water at a 1:10 ratio (wt/vol). After vigorous mixing this solution was allowed to sit overnight in the dark. The following morning the mixture was vigorously mixed again for 1 min, then non-soluble components were removed by centrifugation (2000×g for 20 min). The supernatant was sterile-filtered using a 0.2 μm nylon filter, and then stored in 1.0 mL aliquots at −80 °C until used.
The elderberry juice used in these experiments was obtained from elderberries harvested from North American varieties (Sambucus nigra, L. subsp. canadensis (L. Bolli) near the peak of ripeness and immediately frozen. Andrew L. Thomas (University of Misosuri) collected the specimens from Eridu Farm, Hartsburg (Boone County), MO, in full bloom on June 7, 2012. Location 38.710512 lat., −92.316186 long. A voucher specimen (A. Thomas 120) from the field was preserved at the University of Missouri (UMO) [41]. While frozen the berries were manually separated from stems, leaves, insects, and other debris. Berries were thawed, juiced, then re-frozen. At a later time, the frozen juice was thawed, centrifuged (1000×g for 30 min), then the clarified juice was filtered through a 0.2 μm sterile, pyrogen-free nylon filter (Fisher Scientific, Inc.) and stored at −80 °C in 100 μL aliquots. Just prior to addition to cell culture medium, the frozen, sterile-filtered juice was thawed and diluted 1000-fold so as to supply a final concentration of ~100 μg of juice solids/mL.
The presence and concentration of endotoxin in each of the extracts was quantified using the recombinant factor C endotoxin detection assay (Lonza Walkersville, Inc., Cat. 50-658U, Walkersville, MD, USA) following the instructions provided by the manufacturer. The principle of this kit is that the recombinant Factor C is activated by endotoxin binding, and the active moiety created then acts to cleave a synthetic substrate resulting in the generation of a fluorogenic compound. The highest concentration of endotoxin was found in the S. frutescens (i.e., ~0.8 ng LPS equivalents/mL), while the Ashwagandha extract and elderberry juice contained 0.004 and <0.001 ng of LPS equivalents/mL, respectively.
Recombinant Human Tumor Necrosis Factor alpha 1α (TNF-α; #rhtnf-α) and standard lipopolysaccharide from E. coli 0111:B4 strain- TLR4 ligand (LPS; #tlrl-eblps) were purchased from Invivogen. NRK-52E cells were plated at a density of 120,000 cells/well in 6-well plates and left to grow to confluency overnight. Cells were washed with 1X DPBS and then treated with water or botanical extract (1:100 dilution) for 24 h. Wells were washed and then treated with water, TNF-α or LPS, botanical extract, or a combination of TNF-α or LPS plus botanical extract for an additional 24 h. After 48 h treatment, cells were harvested for RNA extraction.
NF−κB activity assay
NRK-52E:NF-κB cells were plated at a density of 100,000 cells/well in 12-well plates and left to grow to confluency overnight. They were dosed as described above. Media was removed and cells were washed twice with 1X DPBS. Reporter lysis buffer was added to each well and the plates were allowed to rock for 15 min at RT, followed by a freeze/thaw cycle for 30 min at −80 °C and 30 min rocking at RT. Cell lysates were collected and centrifuged for 15 s. Lysates were transferred to a new tube and assayed for NF-κB green fluorescent protein (GFP)/luciferase activity using the Luciferase Assay System kit (#E4030) from Promega. Briefly, 100 μl of lysate was placed into each well of a 96-well flat bottom, opaque white plate. The fluorescence of samples was read for GFP expression at 485/20 nm excitation and 528/20 nm emission wavelengths. Then the luciferase assay reagent was added to each well and the luminescence of the wells was read for luciferase expression on a Synergy HT plate reader using Gen5 (version 1.11) software from Bio-TEK. NF-κB activation is expressed as the individual luciferase/GFP values divided by the average control luciferase/GFP value.
Real-time PCR
RNA was extracted from the cells using the NucleoSpin RNA kit (Macherey-Nagel #740955.50), with on-column DNase digestion. RNA was quantified by a spectrophotometric read using the Nanodrop 2000c (Thermo Scientific). cDNA was made from the quantified RNA using the High Capacity cDNA Reverse Transcription kit (Applied Biosystems #4368814), including a RNase inhibition step (Applied Biosystems #N8080119). Real-Time PCR was performed in duplicate using 200 ng cDNA/reaction in conjunction with Taqman assays (Applied Biosystems) using TaqProbe 2X qPCR Multiplex Master Mix (Bullseye #BEQPCR-PM) on the CFX96 Touch system (Bio-Rad). The following cycling conditions were followed: 95 °C for 20 s, then 95 °C for 1 s and 60 °C for 20 s repeated 40 times. TaqMan primer sets (Life Technologies) were used to determine Chemokine (C-C motif) ligand 2 (CCL2; RN00580555_m1) and chemokine (C-C motif) ligand 5 (CCL5; Rn00579590_m1). The Pfaffl method was used to determine relative quantitation, normalizing the data to cancer susceptibility candidate gene 3 (Casc3; RN00595941_m1) [42].
Statistics
Data is expressed as the mean +/- standard error. A two-tailed t-test, assuming two-sample equal variance, was used to determine significance. P-values of <0.05 were considered statistically significant.
Results
Initial experiments were designed to determine an optimal concentration of TNF-α to induce CCL5 expression; published studies have shown that NRK-52E cells respond to 10 ng/ml for 6–48 h [43, 44]. In our experiments, higher concentrations (100 or 500 ng/ml) failed to substantially enhance CCL5 gene expression, while results with 50 ng/ml were highly variable (Fig. 1). A concentration of 10 ng/ml for 24 h induced an approximate 10-fold increase in CCL5 gene expression that was not seen at early (3 or 6 h) timepoints (Fig. 1). We then screened water-soluble extracts of ashwagandha, sutherlandia, or elderberry at a dilution of 1:100. We used two approaches – cells were exposed to the botanical extracts for 24 h prior to 10 ng/ml TNF-α challenge alone or in the continued presence of the botanical for 24 h. Interestingly, elderberry alone induced CCL5 expression to the extent of TNF-α, while pretreatment and co-treatment with sutherlandia attenuated TNF-α-induced CCL5 expression (Fig. 2). Ashwagandha, however, completely ablated the induction of CCL5 by TNF-α when cells were pretreated or cotreated (Fig. 2). Interestingly, both ashwaganda and sutherlandia also inhibited basal CCL5 gene expression in NRK-52E cells.
Fig. 1.
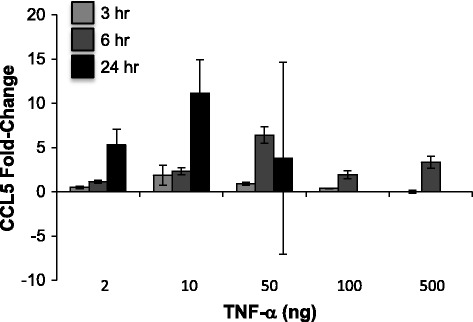
TNF-α induces CCL5 expression in NRK-52E cells. Confluent cells were challenged with varying concentrations of TNF-α for 3–24 h; CCL5 expression was assessed by qPCR. Each data point represents the mean ± SD of three replicate cultures
Fig. 2.
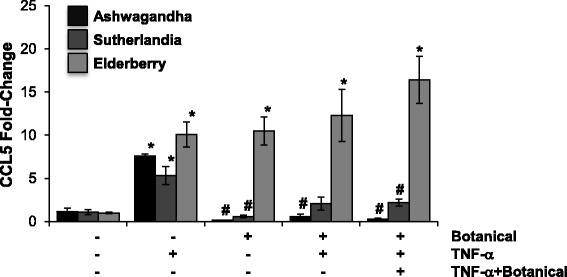
Ashwagandha prevents TNF-α-induced CCL5 gene expression. Confluent NRK-52E cells were treated for 24 h with water-soluble extracts of ashwagandha, sutherlandia or elderberry (1:100). After 24 h, cells were challenged with 10 ng/ml of TNF-α for 24 h alone or in the presence of the botanical extract. CCL5 gene expression was determined by qPCR. Each data point represents the mean ± SD of three replicate cultures, * indicates a significant difference as compared to control (no botanical, no TNF-α), # indicates a significant difference from TNF-α-challenged cultures
In Fig. 3, the same treatment regimens (pretreatment and pretreatment/cotreatment) were used with the ashwagandha (Ash) extracts. Pre-treatment with Ash inhibited both CCL2 and CCL5 expression induced by TNF-α. In the case of CCL2, which was induced to a higher extent than CCL5 by TNF-α, the protective effect was partial, but not complete (Fig. 3). TNF-α did not increase expression of CCL17, 19, or 21, or expression of COX-2 (data not shown). In addition, the pretreatment/co-treatment approach was most effective at attenuating CCL2 expression. Given that TNF-α induces NF-κB activation [14], and that NF-κB regulates CCL2 and 5 expression [18, 19], we used an NF-κB reporter cell line to investigate the potential of Ash to inhibit TNF-α-induced NF-κB activation. While pretreatment with Ash partially attenuated NF-kB activation following TNF-α challenge, the pretreatment/cotreatment regimen completely blocked TNF-α-induced NF-κB activation (Fig. 3). Ashwagandha did not, however, affect basal NF-kB activity parallel to the reduction in basal CCL5 expression.
Fig. 3.
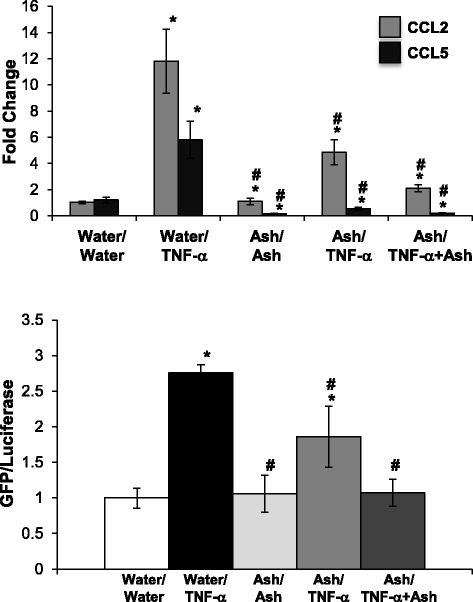
Ashwagandha attenuated TNF-α-induced CCL2 gene expression and NF-κB activation. Confluent NRK-52E cells were treated for 24 h with water-soluble extracts of ashwagandha (Ash; 1:100). After 24 h, cells were challenged with 10 ng/ml of TNF-α for 24 h alone or in the presence of the ashwaganda extract. CCL2 and 5 gene expression was determined by qPCR (top) while NF-κB activation was assessed using a reporter cell line (bottom). Each data point represents the mean ± SD of three replicate cultures, repeated twice, * indicates a significant difference as compared to control (no botanical, no TNF-α), # indicates a significant difference from TNF-α-challenged cultures
To ensure that the effects of ashwagandha were not limited to TNF-α, we then challenged cells with LPS using the same approach. NRK-52E cells have been challenged with 10–100 ng/ml LPS for 24 h [45]. We chose to use concentrations at the lower end of this range; 2 or 10 ng/ml LPS is associated with a robust increase in both CCL2 and CCL5 gene expression at 24 h (Fig. 4). Interestingly, the response is not dose-dependent in that the response was greater using 2 ng/ml. Pretreatment with Ash attenuated LPS-induced CCL2 and prevented CCL5 expression, while the pretreatment/cotreatment strategy further attenuated CCL2 expression and CCL5 expression was completely inhibited (Fig. 4). The pre-treatment with Ash attenuated LPS-induced NF-κB activity, while the pretreatment/cotreatment strategy prevented the effect (Fig. 4).
Fig. 4.
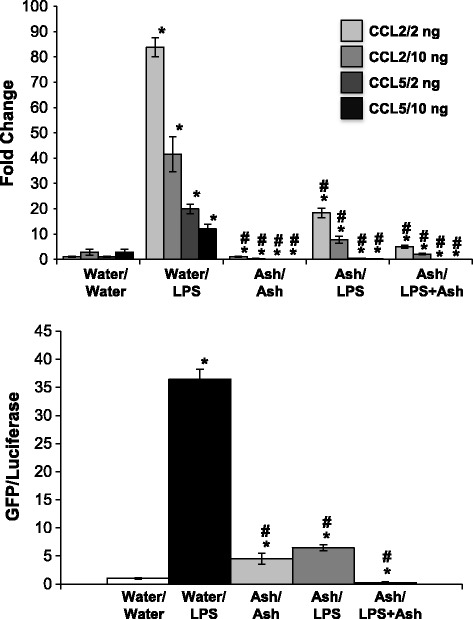
Ashwagandha attenuated LPS-induced CCL2 and CCL5 gene expression and NF-κB activation. Confluent NRK-52E cells were treated for 24 h with water-soluble extracts of ashwagandha (Ash; 1:100). After 24 h, cells were challenged with 2 or 10 ng/ml of LPS for 24 h alone or in the presence of the ashwaganda extract. CCL2 and 5 gene expression was determined by qPCR (top) while NF-κB activation was assessed using a reporter cell line (bottom). Each data point represents the mean ± SD of three replicate cultures, repeated twice, * indicates a significant difference as compared to control (no botanical, no LPS), # indicates a significant difference from LPS-challenged cultures
Discussion
The identification of specific strategies to slow the progression of chronic renal dysfunction, or to attenuate acute injury, has been a frustratingly slow process. Given the role of inflammation in injury and progression to dysfunction via pro-fibrogenic mechanisms, strategies to attenuate inflammation are promising therapeutics. There are a number of studies suggesting that botanicals are anti-inflammatory [29–31, 36]; however, the molecular pathways targeted by many of these remains poorly defined. In our studies, we developed an in vitro model to screen botanical extracts for anti-inflammatory cells in a rat proximal tubular epithelial cell line, NRK-52E, since the proximal tubular epithelium is both a source [5] and target of inflammation in the kidney. In these studies, cells were challenged with a pro-inflammatory stimuli either after exposure to the botanical, or simultaneously with the botanical.
Interestingly, an elderberry extract, which has reported anti-inflammatory effects [46], induced CCL5 expression to a similar extent as TNF-α in our model. A sutherlandia extract partially attenuated TNF-α-induced CCL5 gene expression, but ashwaganda completely inhibited the TNF-α effect on CCL5 expression. This anti-inflammatory effect of ashwagandha is further supported by our findings that the extract attenuates TNF-α and LPS-induced CCL2 expression and NF-κB activation, and inhibited LPS-induced CCL5 expression. Ashwagandha has been reported to be renoprotective in several studies, mainly as an antioxidant. Ashwagandha is renoprotective against bromobenzene-induced nephrotoxicity [35], gentamicin-induced nephrotoxicity [34, 47] and dehydration-induced oxidative stress [33]. Mechanistically, it has a positive effect on glutathione peroxidase, superoxide dismutase, and catalase levels [34].
An interesting finding was the ashwagandha decreased basal expression of CCL5, but did not affect basal CCL2 expression or NF-kB activation. The impact of ashwaganda on CCL2 expression paralleled the effects on NF-kB activation, i.e. attenuated TNF-α- or LPS-induced increases. These data suggest that ashwagandha affects other signaling pathways which regulate CCL5 expression; candidates include the p38 MAPK pathway which has been shown to inhibit CCL5 in smooth muscle cells [48]. Withaferin A, a bioactive component of ashwagandha [49], has been shown to increase p38 activity [50], as has another component of ashwagandha, withanolide D [51].
There are a number of papers demonstrating that withaferin A inhibits NF-κB signaling [52, 53]. Withaferin A also inhibits NF-κB activation by inhibiting IKKb catalytic activity [54]. In addition, there is data demonstrating that withaferin A inhbits TNF-α-induced effects in endothelial cells [55]. We examined withaferin A in our model system, however, at concentrations (1 μM) and timepoints (2 h) previously reported [54, 55], withaferin A induced substantial cytotoxicity in our cells (data not shown). As such, withaferin A induces apoptosis in a number of cell types [56, 57] putatively via down regulation of JAK/STAT3 in cancer cells [58]. Given that withaferin A is not readily-water soluble and that it was cytotoxic, our data suggest that withaferin A is not solely responsible for anti-inflammatory effects of ashwagandha. Future studies will focus on the pathway by which ashwaganda regulates both basal- and stimulus-induced chemokine expression. In addition, the confirmation of these findings in in vivo models of progressive renal injury and dysfunction represents an important progression of botanical-based renoprotection research.
Conclusions
A water-soluble extract of Ashwagandha has anti-inflammatory effects, specifically reducing gene expresison of CCL2 and CCL5 in response to TNFα or LPS stimulation. This may be mediated, in part, via a reduction in NF-κB activity. These data suggest that Ashwagandha may represent a botanical approach for the management of renal dysfunction.
Acknowledgements
Research reported in this publication was supported by grant P50 AT006723 from the National Center for Complementary and Alternative Medicine, the Office of Dietary Supplements, the National Cancer Institute, and the National Institute of Aging (RO1AG034154). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
VM developed the NF-κB reporter cell line (VM), KF was responsible for the botanical extract preparation, EG-B performed the cell culture/dosing/qPCR experiments and ARP prepared the initial draft of the manuscript. All authors read and approved the final manuscript.
References
- 1.Costello-White R, Ryff CD, Coe CL. Aging and low-grade inflammation reduce renal function in middle-aged and older adults in Japan the USA. AGE. 2015;37:9808. doi: 10.1007/s11357-015-9808-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodwell GE, Sonu R, Zahn JM, Lund J, Wilhelmy J, Wang L, et al. A transcriptional profile of aging in the human kidney. PLoS Biol. 2004;2:e427. doi: 10.1371/journal.pbio.0020427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Melk A, Mansfield ES, Hsieh SC, Hernandez-Boussard T, Grimm P, Rayner DC, et al. Transcriptional analysis of the molecular basis of human kidney aging using cDNA microarray profiling. Kidney Int. 2005;68:2667–79. doi: 10.1111/j.1523-1755.2005.00738.x. [DOI] [PubMed] [Google Scholar]
- 4.Chen G, Bridenbaugh EA, Akintola AD, Catania JM, Vaidya VS, Bonventre JV, et al. Increased susceptibility of aging kidney to ischemic injury: Identification of candidate genes changed during aging, but corrected by caloric restriction. Am J Physiol Renal Physiol. 2007;293:F1272–81. doi: 10.1152/ajprenal.00138.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lim AI, Chan LY, Tang SC, Yiu WH, Li R, Lai KN, et al. BMP-7 represses albumin-induced chemokine synthesis in kidney tubular epithelial cells through destabilization of NF-κB-inducing kinase. Immunol Cell Biol. 2014;92:427–35. doi: 10.1038/icb.2013.106. [DOI] [PubMed] [Google Scholar]
- 6.Wada J, Makino H. Inflammation and the pathogenesis of diabetic nephropathy. Clin Sci. 2013;124:139–52. doi: 10.1042/CS20120198. [DOI] [PubMed] [Google Scholar]
- 7.Filiopoulos V, Vlassopoulos D. Inflammatory syndrome in chronic kidney disease: Pathogenesis and influence on outcomes. Inflamm Allergy Drug Targets. 2009;8:369–82. doi: 10.2174/1871528110908050369. [DOI] [PubMed] [Google Scholar]
- 8.Izquierdo MC, Sanz AB, Sánchez-Niño MD, Pérez-Gómez MV, Ruiz-Ortega M, Poveda J, et al. Acute kidney injury transcriptomics unveils a relationship between inflammation and ageing. Nefrologia. 2012;32:715–23. doi: 10.3265/Nefrologia.pre2012.Aug.11667. [DOI] [PubMed] [Google Scholar]
- 9.Hewitson TD. Renal tubulointerstitial fibrosis: Common but never simple. Am J Physiol Renal Physiol. 2009;296:F1239–44. doi: 10.1152/ajprenal.90521.2008. [DOI] [PubMed] [Google Scholar]
- 10.Zeisberg M, Neilson EG. Mechanisms of tubulointerstitial fibrosis. J Am Soc Nephrol. 2010;21:1819–34. doi: 10.1681/ASN.2010080793. [DOI] [PubMed] [Google Scholar]
- 11.Boor P, Ostendorf T, Floege J. Renal fibrosis: Novel insights into mechanisms and therapeutic targets. Nat Rev Nephrol. 2010;6:643–56. doi: 10.1038/nrneph.2010.120. [DOI] [PubMed] [Google Scholar]
- 12.Donadelli R, Abbate M, Zanchi C, Corna D, Tomasoni S, Benigni A, et al. Protein traffic activates NF-κB gene signaling and promotes MCP-1-dependent interstitial inflammation. Am J Kidney Dis. 2000;36:1226–41. doi: 10.1053/ajkd.2000.19838. [DOI] [PubMed] [Google Scholar]
- 13.Sanz AB, Sanchez-Nino MD, Ramos AM, Moreno JA, Santamaria B, Ruiz-Ortega M, et al. NF-κB in renal inflammation. J Am Soc Nephrol. 2010;21:1254–62. doi: 10.1681/ASN.2010020218. [DOI] [PubMed] [Google Scholar]
- 14.Lin H, Hou CC, Cheng CF, Chiu TH, Hsu YH, Sue YM, et al. Peroxisomal proliferator-activated receptor-alpha protects renal tubular cells from doxorubicin-induced apoptosis. Mol Pharmacol. 2007;72:1238–45. doi: 10.1124/mol.107.037523. [DOI] [PubMed] [Google Scholar]
- 15.Esteban V, Lorenzo O, Ruperez M, Suzuki Y, Mezzano S, Blanco J, et al. Angiotensin II, via AT1 and AT2 receptors and NF-kappaB pathway, regulates the inflammatory response in unilateral ureteral obstruction. J Am Soc Nephrol. 2004;15:1514–29. doi: 10.1097/01.ASN.0000130564.75008.F5. [DOI] [PubMed] [Google Scholar]
- 16.Vielhauer V, Mayadas TN. Functions of TNF and its receptors in renal disease: Distinct roles in inflammatory tissue injury and immune regulation. Semin Nephrol. 2007;27:286–308. doi: 10.1016/j.semnephrol.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 17.Remuzzi G, Perico N, Macia M, Ruggenenti P. The role of renin-angiotensin-aldosterone system in the progression of chronic kidney disease. Kidney Int Suppl. 2005;99:S57–65. doi: 10.1111/j.1523-1755.2005.09911.x. [DOI] [PubMed] [Google Scholar]
- 18.Fantuzzi L, Spadaro F, Purificato C, Cecchetti S, Podo F, Belardelli F, et al. Phosphatidylcholine-specific phospholipase C activation is required for CCR5-dependent, NF-kB-driven CCL2 secretion elicited in response to HIV-1 gp120 in human primary macrophages. Blood. 2008;111:3355–63. doi: 10.1182/blood-2007-08-104901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu X, Shah A, Gangwani MR, Silverstein PS, Fu M, Kumar A, et al. HIV-1 Nef induces CCL5 production in astrocytes through p38-MAPK and PI3K/Akt pathway and utilizes NF-kB, CEBP and AP-1 transcription factors. Sci Rep. 2014;4:4450. doi: 10.1038/srep04450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rollins BJ. MCP-1, −2, −3, −4, −5. Cytokine Reference. Oppenheim JJ, Feldman S, Durum S, Hirano T, Vilcek J, Nicola N, eds. London: Academic Press; 2000. p. 1145–1160.
- 21.Ruster M, Sperschneider H, Funfstuck R, Stein G, Grone HJ. Differential expression of beta chemokines MCP-1 and RANTES and their receptors CCR1, CCR2, CCR5 in acute rejection and chronic allograft nephropathy of human renal allografts. Clin Nephrol. 2004;61:30–9. doi: 10.5414/CNP61030. [DOI] [PubMed] [Google Scholar]
- 22.Tamura M, Aizawa R, Hori M, Ozaki H. Progressive renal dysfunction and macrophage infiltration in interstitial fibrosis in an adenine-induced tubulointerstitial nephritis mouse model. Histochem Cell Biol. 2009;131:483–90. doi: 10.1007/s00418-009-0557-5. [DOI] [PubMed] [Google Scholar]
- 23.Gong R, Rifai A, Tolbert EM, Biswas P, Centracchio JN, Dworkin LD, et al. Hepatocyte growth factor ameliorates renal interstitial inflammation in rat remnant kidney by modulating tubular expression of macrophage chemoattractant protein-1 and RANTES. J Am Soc Nephrol. 2004;15:2868–81. doi: 10.1097/01.ASN.0000141962.44300.3A. [DOI] [PubMed] [Google Scholar]
- 24.Vielhauer V, Berning E, Eis V, Kretzler M, Segerer S, Strutz F, et al. CCR1 blockade reduces interstitial fibrosis in mice with glomerulosclerosis and nephrotic syndrome. Kidney Int. 2004;66:2264–78. doi: 10.1111/j.1523-1755.2004.66038.x. [DOI] [PubMed] [Google Scholar]
- 25.Bedke J, Kiss E, Schaefer L, Behnes CL, Bonrouhi M, Gretz N, et al. Beneficial effects of CCR1 blockade on the progression of chronic renal allograft damage. Am J Transplant. 2007;7:527–37. doi: 10.1111/j.1600-6143.2006.01654.x. [DOI] [PubMed] [Google Scholar]
- 26.Tesch GH. MCP-1/CCL2: A new diagnostic marker and therapeutic target for progressive renal injury in diabetic nephropathy. Am J Physiol Renal Physiol. 2008;294:F697–701. doi: 10.1152/ajprenal.00016.2008. [DOI] [PubMed] [Google Scholar]
- 27.Ho J, Rush DN, Gibson IW, Karpinski M, Storsley L, Bestland J, et al. Early urinary CCL2 is associated with the later development of interstitial fibrosis and tubular atrophy in renal allografts. Transplantation. 2010;90:394–400. doi: 10.1097/TP.0b013e3181e6424d. [DOI] [PubMed] [Google Scholar]
- 28.Ho J, Wiebe C, Gibson IW, Hombach-Klonisch S, Gao A, Rigatto C, et al. Elevated urinary CCL2: Cr at 6 months is associated with renal allograft interstitial fibrosis and inflammation at 24 months. Transplantation. 2014;98:39–46. doi: 10.1097/01.TP.0000442776.40295.73. [DOI] [PubMed] [Google Scholar]
- 29.Jiang J, Chuang DY, Zong Y, Patel J, Brownstein K, Lei W, et al. Sutherlandia frutescens ethanol extracts inhibit oxidative stress and inflammatory responses in neurons and microglial cells. PLoS ONE. 2014;9:e89748. doi: 10.1371/journal.pone.0089748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.van Wyk BE, Albrecht C. A review of the taxonomy, ethnobotany, chemistry and pharmacology of Sutherlandia frutescens (Fabaceae) J Ethnopharmacol. 2008;119:620–9. doi: 10.1016/j.jep.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 31.Vlachojannis JE, Cameron M, Chrubasik S. A systematic review on the sambuci fructus effect and efficacy profiles. Phytother Res. 2010;24:1–8. doi: 10.1002/ptr.2729. [DOI] [PubMed] [Google Scholar]
- 32.Curtis PJ, Kroon PA, Hollands WJ, Walls R, Jenkins G, Kay CD, et al. Cardiovascular disease risk biomarkers and liver and kidney function are not altered in postmenopausal women after ingesting an elderberry extract rich in anthocyanins for 12 weeks. J Nutr. 2009;139:2266–71. doi: 10.3945/jn.109.113126. [DOI] [PubMed] [Google Scholar]
- 33.Das K, Samanta TT, Samanta P, Nandi DK. Effect of extract of Withania Somnifera on dehydration-induced oxidative stress-related uremia in male rats. Saudi J Kidney Dis Transpl. 2010;21(1):75–80. [PubMed] [Google Scholar]
- 34.Jeyanthi T, Subramanian P. Protective effect of Withania somnifera root powder on lipid peroxidation and antioxidant status in gentamicin-induced nephrotoxic rats. J Basic Clin Physiol Pharmacol. 2010;21(1):61–78. doi: 10.1515/JBCPP.2010.21.1.61. [DOI] [PubMed] [Google Scholar]
- 35.Vedi M, Rasool M, Sabina EP. Protective effect of administrationo of Withania somifera against bromobenzene induced nephrotoxicity and oxidative stress in rats. Ren Fail. 2014;21:1–9. doi: 10.3109/0886022X.2014.918812. [DOI] [PubMed] [Google Scholar]
- 36.Minhas U, Minz R, Das P, Bhatnagar A. Therapeutic effect of Withania somnifera on pristane-induced model of SLE. Inflammopharmacology. 2012;20:195–205. doi: 10.1007/s10787-011-0102-8. [DOI] [PubMed] [Google Scholar]
- 37.Mossine VV, Waters JK, Hannink M, Mawhinney TP. piggyBac Transposon plus insulators overcome epigenetic silencing to provide for stable signaling pathway reporter cell lines. PLoS ONE. 2013;8:e85494. doi: 10.1371/journal.pone.0085494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fernandes AC, Cromarty AD, Albrecht C, van Rensburg CE. The antioxidant potential of Sutherlandia frutescens. J Ethnopharmacol. 2014;95:1–5. doi: 10.1016/j.jep.2004.05.024. [DOI] [PubMed] [Google Scholar]
- 39.Avula B, Wang YH, Smillie TJ, Fu X, Li XC, Mabusela W, et al. Quantitative determination of flavonoids and cycloartanol glycosides from aerial parts of Sutherlandia frutescens (L.) R. BR. by using LC-UV/ELSD methods and confirmation by using LC-MS method. J Pharm Biomed Anal. 2010;52:173–80. doi: 10.1016/j.jpba.2010.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fu X, Li XC, Smiillie TJ, Carvalho P, Mabusela W, Syce J, et al. Cycloartane glycosides from Sutherlandia frutescens. J Nat Prod. 2008;71:1749–53. doi: 10.1021/np800328r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Byers PL, Thomas AL, Millican M. “Wyldewood’ elderberry. Hort Science. 2010;45:312–3. [Google Scholar]
- 42.Pfaffl MW. A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res. 2001;29:e45. doi: 10.1093/nar/29.9.e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nakajima S, Kato H, Takahashi S, Johno H, Kitamura M. Inhibition of NF-κB by MG132 through ER stress-mediated induction of LAP and LIP. FEBS Lett. 2011;585:2249–54. doi: 10.1016/j.febslet.2011.05.047. [DOI] [PubMed] [Google Scholar]
- 44.Kadomatsu M, Nakajima S, Kato H, Gu L, Chi Y, Yao J, et al. Cordycepin as a sensitizer to tumour necrosis factor (TNF)-α-induced apoptosis through eukaryotic translation initiation factor 2α (eIF2α)- and mammalian target of rapamycin complex 1 (mTORC1)-mediated inhibition of nuclear factor (NF)-κB. Clin Exp Immunol. 2012;168:325–32. doi: 10.1111/j.1365-2249.2012.04580.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hei Z, Zhang A, Wei J, Gan X, Wang Y, Luo G, et al. Lipopolysaccharide effects on the proliferation of NRK52E cells via alternations in gap-junction function. J Trauma Acute Care Surg. 2012;73:67–72. doi: 10.1097/TA.0b013e318256a0fe. [DOI] [PubMed] [Google Scholar]
- 46.Simonyi A, Chen Z, Jiang J, Zong Y, Chuang DY, Gu Z, et al. Inhibition of microglial activation by elderberry extracts and its phenolic components. Life Sci. 2015;128:30–8. doi: 10.1016/j.lfs.2015.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jeyanthi T, Subramanian P. Nephroprotective effect of Withania somnifera: A dose-dependent study. Ren Fail. 2009;31:814–21. doi: 10.3109/08860220903150320. [DOI] [PubMed] [Google Scholar]
- 48.Liu H, Ning H, Men H, Hou R, Fu M, Zhang H, et al. Regulation of CCL5 expression in smooth muscle cells following arterial injury. PLoS ONE. 2012;7:e30873. doi: 10.1371/journal.pone.0030873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vanden Berghe W, Sabbe L, Kaileh M, Haegeman G, Heyninck K. Molecular insight in the multifunctional activities of Withaferin A. Biochem Pharmacol. 2012;84:1282–91. doi: 10.1016/j.bcp.2012.08.027. [DOI] [PubMed] [Google Scholar]
- 50.Yang H, Wang Y, Cheryan VT, Wu W, Cui CQ, Polin LA, et al. Withaferin A inhibits the proteasome activity in mesothelioma in vitro and in vivo. PLoS One. 2012;7:e41214. doi: 10.1371/journal.pone.0041214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mondal S, Mandal C, Sangwan R, Chandra S, Mandal C. Withanolide D induces apoptosis in leukemia by targeting the activation of neutral sphingomyelinase-ceramide cascade mediated by synergistic activation of c-Jun N-terminal kinase and p38 mitogen-activated protein kinase. Mol Cancer. 2010;9:239. doi: 10.1186/1476-4598-9-239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Singh D, Aggarwal A, Maurya R, Naik S. Withania somnifera inhibits NF-kappa B and AP-1 transcription factors in human peripheral blood and synovial fluid mononuclear cells. Phytother Res. 2007;21:905–13. doi: 10.1002/ptr.2180. [DOI] [PubMed] [Google Scholar]
- 53.Kaileh M, Vanden Berghe W, Heyerick A, Horion J, Piette J, Libert C, et al. Withaferin a strongly elicits IkappaB kinase beta hyperphosphorylation concomitant with potent inhibition of its kinase activity. J Biol Chem. 2007;282:4253–64. doi: 10.1074/jbc.M606728200. [DOI] [PubMed] [Google Scholar]
- 54.Heyninck K, Lahtela-Kakkonen M, Van der Veken P, Haegeman G, Vanden BW. Withaferin A inhibits NF-kappaB activation by targeting cysteine 179 in IKKb. Biochem Pharmacol. 2014;91:501–9. doi: 10.1016/j.bcp.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 55.Ku SK, Han MS, Bae JS. Withaferin A is an inhibitor of endothelial protein C receptor shedding in vitro and in vivo. Food Chem Toxicol. 2014;68:23–9. doi: 10.1016/j.fct.2014.03.009. [DOI] [PubMed] [Google Scholar]
- 56.Choi MJ, Park EJ, Min KJ, Park JW, Kwon TK. Endoplasmic reticulum stress mediates withaferin A-induced apoptosis in human renal carcinoma cells. Toxicol In Vitro. 2011;25:692–8. doi: 10.1016/j.tiv.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 57.Yang ES, Choi MJ, Kim JH, Choi KS, Kwon TK. Withaferin A enhances radiation-induced apoptosis in Caki cells through induction of reactive oxygen species, Bcl-2 downregulation and Akt inhibition. Chem Biol Interact. 2011;190:9–15. doi: 10.1016/j.cbi.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 58.Um HJ, Min KJ, Kim DE, Kwon TK. Withaferin A inhibits JAK/STAT3 signaling and induces apoptosis of human renal carcinoma Caki cells. Biochem Biophys Res Commun. 2012;127:24–9. doi: 10.1016/j.bbrc.2012.08.133. [DOI] [PubMed] [Google Scholar]


