Abstract
Objective. To reflect on selection policies and procedures for programs at pharmacy schools that are members of an international alliance of universities (Universitas 21).
Methods. A questionnaire on selection policies and procedures was distributed to admissions directors at participating schools.
Results. Completed questionnaires were received from 7 schools in 6 countries. Although marked differences were noted in the programs in different countries, there were commonalities in the selection processes. There was an emphasis on previous academic performance, especially in science subjects. With one exception, all schools had some form of interview, with several having moved to multiple mini-interviews in recent years.
Conclusion. The majority of pharmacy schools in this survey relied on traditional selection processes. While there was increasing use of multiple mini-interviews, the authors suggest that additional new approaches may be required in light of the changing nature of the profession.
Keywords: admissions, interviews, pharmacy students, selection
INTRODUCTION
Worldwide, the profession of pharmacy is changing its focus from being a product-oriented to a patient-centered approach.1 Governments and funders increasingly recognize the role of pharmacists as medication/drug experts being pivotal to successful health care delivery.2 Medications continue to be the most common intervention offered to patients and represent a major component of health care budgets in most countries.3 Furthermore, it is acknowledged that in many instances medications are used less than optimally, resulting in both poor health outcomes and unnecessary costs.4 Notwithstanding the important contribution of other health professionals, pharmacists, with their unique focus on all aspects of medicines, are ideally placed to provide medicines optimization in both hospital and community settings; indeed, this is increasingly recognized as their societal purpose.5
The drivers of new pharmacist roles include the increasing complexity and costs of pharmacotherapy, the growing burden of chronic illness, and shortages of health professionals in many countries. In moving from the traditional distributive functions of dispensing and selling medications to more clinical and public health roles, pharmacists will require new or enhanced skills in areas such as consultation, diagnosis, physical assessment, clinical decision-making, prescribing, communication, and moral reasoning.2,6 In addition, generic skills and attributes such as leadership and vision are required so pharmacists can take full advantage of new opportunities in health care delivery. 7,8 These elements are already addressed to varying degrees in pharmacy education programs, but there is much variability. Major change is required to ensure that pharmacy education will produce graduates with the necessary balance of skills and knowledge required for future practice.9,10
There are several possible explanations for a disconnect between pharmacy education and future practice, including the relative lack of clinical, experiential opportunities compared with other health disciplines such as medicine and nursing. Internationally, many schools have evolved from a science rather than a medical base and this has resulted in an emphasis on chemistry and pharmaceutical sciences within pharmacy curricula, often at the expense of more clinical or practice-based material. While scientific foundations are important, programs may need to increase their focus on clinical skills and generic skills such as critical thinking, leadership and innovation.6, 9-11 There has been a recent trend for pharmacy schools to be located in, or closely associated with, faculties (schools) of health sciences including medicine, dentistry, and nursing. The value of interaction with other health professions students and of interprofessional education underlines the need for further emphasis in pharmacy programs on skills such as communication, leadership, and teamwork.12,13
Svennson and fellow deans of pharmacy schools suggested that changes in pharmacy education in the United States may have inadvertently encouraged the production of “change resisters and followers” rather than “innovators and leaders,” and that one cause was the way in which students are selected for admission to pharmacy programs.14 The main qualification for entry into the profession differs internationally—a bachelor’s degree (BPharm) in Australasia, a master’s (MPharm) in the United Kingdom, and a doctorate (PharmD) in the United States. Despite these qualification differences, student selection is still based on academic performance, particularly in science subjects.
There is considerable evidence that quantitative measures such as grades in science and mathematics, prepharmacy grade point averages (GPAs), and scores in pre-admissions tests such as the Pharmacy College Admissions Test (PCAT) and the Pharmacy Education Eligibility Test (PEET), are highly predictive of success during the pharmacy program, of graduation rates, and of success in national board examinations.15-20 However, as argued by Svennson et al, “there appears to be little research on how good these measures are at predicting applicants’ future leadership potential or the likelihood of becoming change agents for the profession.”14
Additional selection processes are used by schools, such as interviews, psychometric tests, candidate profiles, and self-reflective statements, but these processes vary, even within the same country.21,22 In the case of interviews, for example, all schools in the United States must conduct an interview as a requirement of the Accreditation Council for Pharmacy Education (ACPE); however, these range from individual or group interviews to the more recent multiple-mini interviews (MMIs), which focus on generic skills and attributes and are perceived to be more objective.14,23 The suitability, experience, and training of interviewers also varies. Such variations beg the question of how we can know if we are selecting the ‘right’ students for the future practice of pharmacy. While achievement in science subjects will remain a cornerstone of selection, how do we ensure that students have the right attributes/skills for future practice (for example, patient-centred, good communication, moral reasoning, etc.)?14,24,25
The schools of pharmacy involved in the current study belong to an international network of research-intensive universities known as Universitas 21 (U21).26 The purpose of U21 is to foster international best practices in research and education through collaboration. This network currently has 27 member universities and the U21 Health Sciences Group includes 10 schools of pharmacy. These schools interact regularly through teleconferences, staff and student exchanges, and an annual conference. The selection of future students was debated at the 2012 U21 Pharmacy Discipline Conference held at the University of Auckland (UoA), New Zealand, and it was agreed that staff from UoA would lead a study on current selection policies.
The aim of the current study was to document and critically evaluate the selection policies and procedures for the entry-level programs at U21 schools of pharmacy and to reflect on whether the commonalities and differences in approach could be used to help inform the development of “best practice” models in the future selection of pharmacy students.
METHODS
Ethics approval to conduct the study was obtained from the University of Auckland Human Ethics Committee. A condition of approval was to maintain the anonymity of participating schools. For this reason university and country names are not disclosed here. An open questionnaire, designed to take about 15 to 20 minutes to complete, was developed with the following items: nature of entry-level degree; number of students admitted; number of applicants; categories of applicants; affirmative action or preferential entry schemes; academic selection criteria; prerequisite subjects; use of additional tests [eg, Pharmacy College Admissions Test (PCAT)]; use of interviews; format of interviews; weightings for selection criteria; nature of postgraduation training; any other comments.
The questionnaire was sent to the directors of admissions at 9 of the schools (one school is not a currently active member). Completed questionnaires were returned electronically to the research team. Because of the relatively small sample size, results are presented as individual “case-studies,” using a tabular presentation to highlight both commonalities and differences in selection policies and procedures.
RESULTS
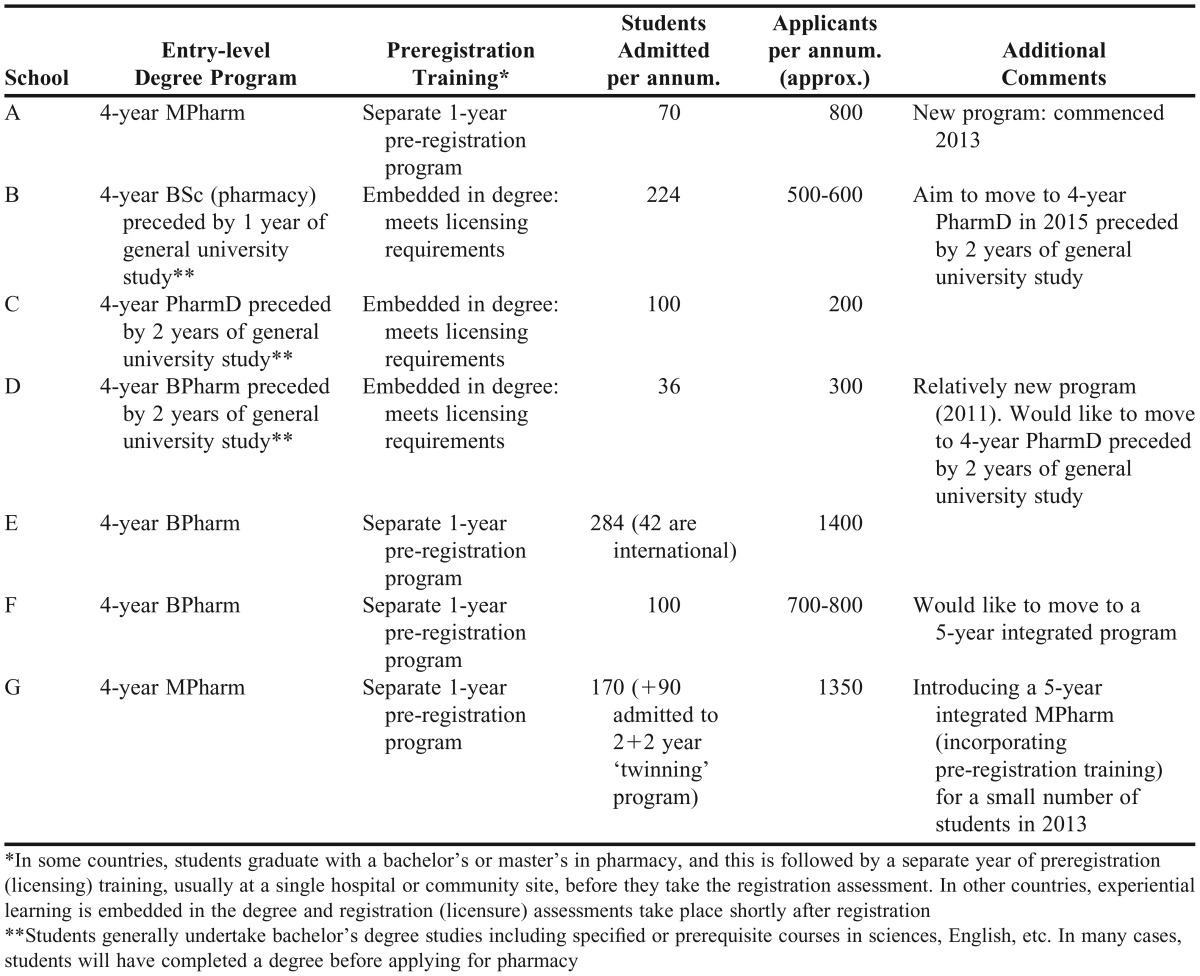
Of the 9 schools contacted, 7 returned the questionnaire (6 countries represented). As shown in Table 1, only one school (C) offers the PharmD as the entry-level qualification. However, one other school (B) was planning on introducing the PharmD in 2015, and another school (D) reported wanting to move to this model in the future. The other 4 schools (A,E,F, G) offered a 4-year BPharm or MPharm followed by a separate 1-year preregistration (licensing) program (“internship”) leading to licensure, although several were exploring a 5-year program that would integrate the prelicensing training into the degree. The number of students admitted ranged from 36 (school D) to 284 (school E), and the number of applicants ranged from 200 (school C) to 1400 (school E). The programs at schools A and D were newer than the others, having been established in 2013 and 2011, respectively.
Table 1.
Degree Type, Number of Applicants, and Students Admitted Per Year
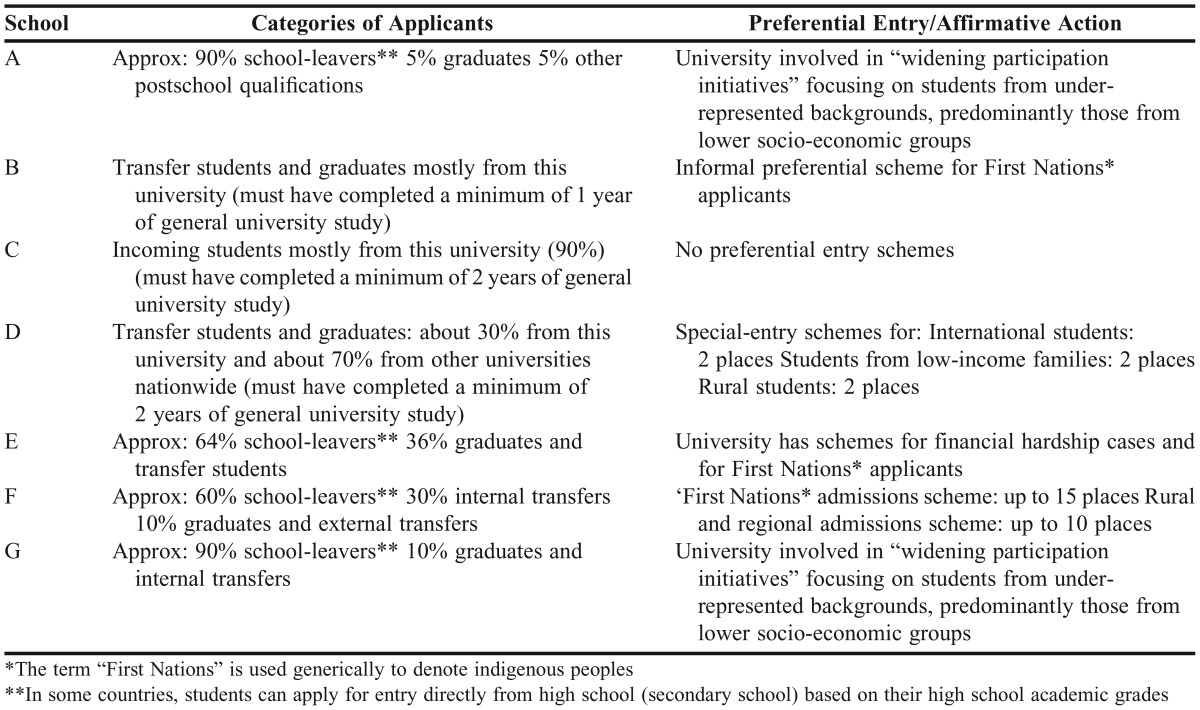
Categories of applicants and the existence of preferential entry/affirmative action schemes are shown in Table 2. Schools for which the majority of applicants had completed high school (“school-leavers”) are in those countries with a separate prelicensing year following the pharmacy degree, while those with such training embedded in the degree select from applicants with prior tertiary study. The majority of schools had some sort of preferential entry/affirmative action scheme, with the exception of school C. These schemes tended to focus on indigenous students, rural students, and those from lower socio-economic groups. In some instances (eg, school F), these schemes involved quite a high proportion of applicants.
Table 2.
Categories of Applicants and Preferential Entry/Affirmative Action Schemes
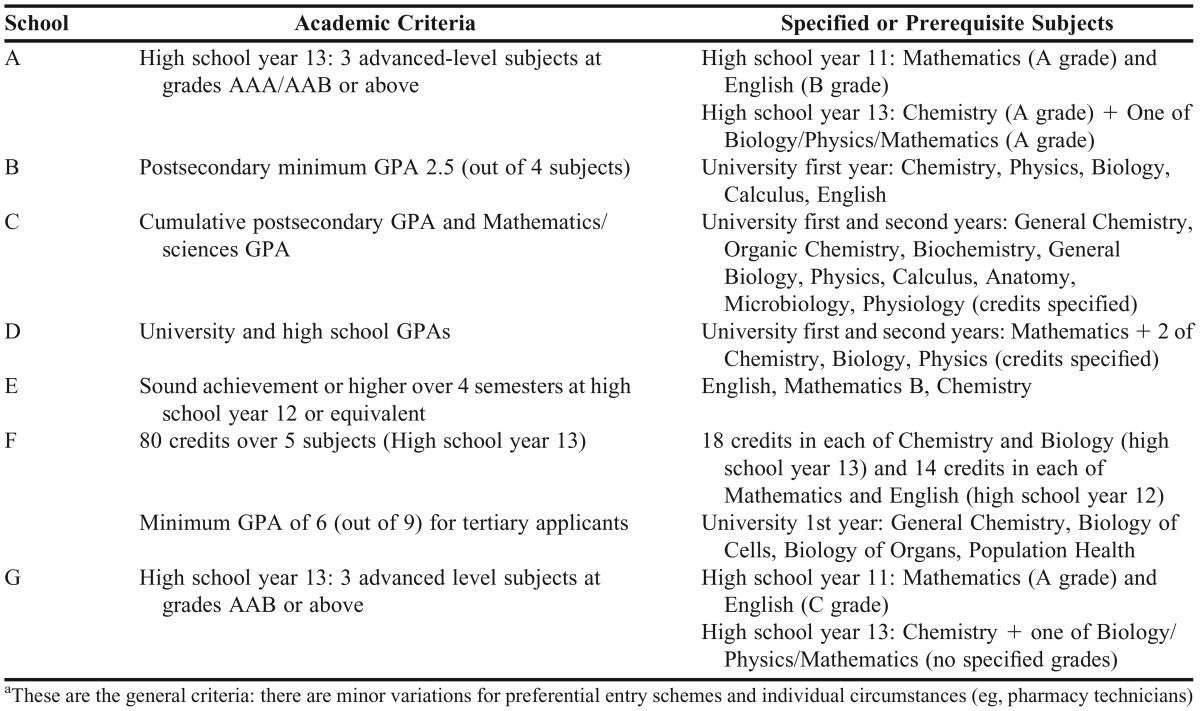
The general academic criteria and specified/prerequisite subjects for admittance to the programs are shown in Table 3. Although academic criteria initially appeared diverse because of the different frameworks, there were some commonalities. All schools sought applicants with average or above average academic grades, whether at school-leaver or tertiary level, particularly in science subjects. The only specified subject in all cases was chemistry and a mix of mathematics/biology/physics was required by most. English was an important criterion in most cases, although the particular requirements varied from country to country.
Table 3.
General Academic Criteria and Specified/Prerequisite Subjects for Admittance to Pharmacy Programsa
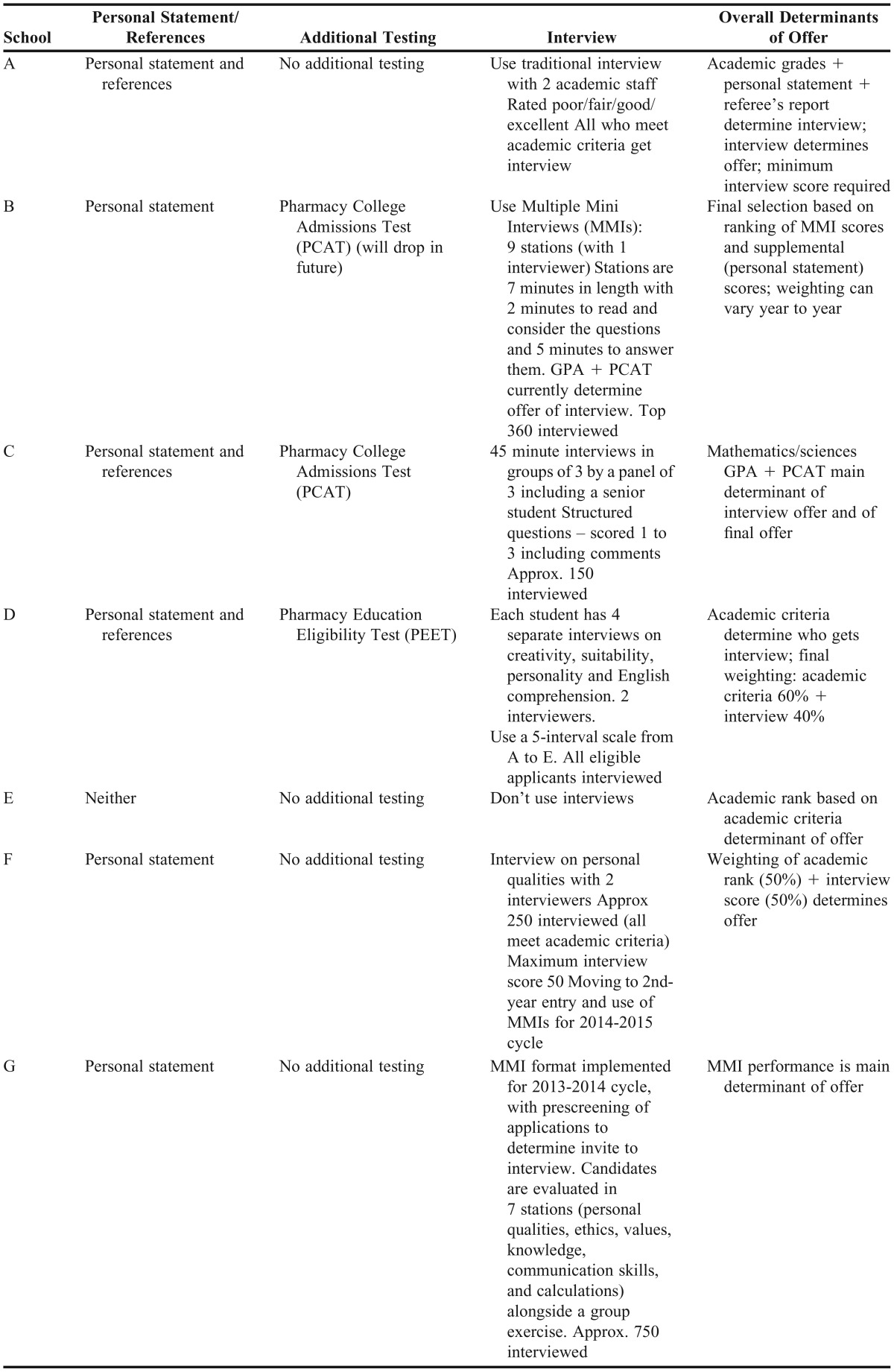
Additional criteria are shown in Table 4. All but one school (E) used interviews as part of the selection process. Two schools (B, G) introduced MMIs to replace the traditional interview, and another school (F) will introduce MMIs in the next admissions round. Three schools use an additional psychometric test (schools B, C, D), although one school (B) is intending to drop this in the near future. In 2 cases (schools A, B), a personal profile/statement was also considered. In most cases, the final determination of an offer was based on a combination of the academic rank and interview performance, although the weightings varied from school to school.
Table 4.
Use of Personal Statements, Additional Testing, Interviews, and Overall Determinants of Offer
DISCUSSION
The aim of our study was to analyze commonalities and differences in selection of pharmacy students among a small group of schools belonging to an international alliance and to determine if these factors could be used to help inform the development of best-practice models for the student selection process. We found that policies and procedures differed widely according to the individual context. For example, the number of students admitted per annum varied from 36 to 284. There was a notable mix of entry-level qualifications (BPharm, BSc in Pharmacy, MPharm, PharmD) and pathways to registration according to the country. Four schools had a prelicensing year after graduation—this may change in the future as schools move to programs that integrate prelicensing experience, which some schools indicated an interest in.
In line with the different models, there was a mix of entrants, ranging from approximately 90% school-leavers (school E) to 100% tertiary transfers (school C). It is beyond the scope of this paper to speculate whether one system is better than another, but we assume that programs with entry after some university study would have more mature students who are more certain about their career choice.
Despite the obvious differences, there were commonalities in the approach to selection. Of course, all schools sought candidates with good high school or tertiary academic performance. Science subjects were highlighted as prerequisites in all cases, with chemistry being stipulated by all and a mix of mathematics/biology/physics by most.16-18 English was also an important prerequisite for all, although the level of evidence required varied, with several schools stipulating grades from high school year 11, or via standardized tests of English as a second language such as the International English Language Testing System (IELTS). While adequate preparation in science subjects is important for prospective pharmacy students, and they need to be mathematically and scientifically literate, the heavy emphasis on science achievement may no longer be appropriate as the profession moves to a more clinical future. If this future requires a greater understanding of human behavior and enhanced communication and interpersonal skills, a greater emphasis on the humanities and social sciences at the selection stage may provide an alternative foundation.
Most schools required a personal profile/statement. This was used as a determination to offer an interview, as a prompt for interviewers, or as part of the overall weighting for selection. In the authors’ experience, the utility of personal statements is fairly limited and their main use is to get a sense of the applicant before interview, and provide some useful prompts for interview questions. Three schools used some form of additional psychometric screening (PCAT, PEET), although one school was planning to drop the PCAT following its introduction of MMIs. As with personal statements, these tests were used either to determine the offer of an interview or formed part of the overall weighting. Mini-interviews are designed to explore applicants’ problem-solving ability, creativity, and social awareness, and therefore raise the question of whether additional testing is redundant if MMIs are used.14,24
Six of the schools used some form of interview; mostly a traditional interview of an individual applicant with one or two interviewers. Only 1 school did not conduct interviews and relied entirely on academic ranking of applicants. In most cases, the interview (or MMI) was heavily weighted or was the main determinant of an offer. In all cases where an interview was used (both traditional and MMIs), the emphasis was on personal qualities of the applicant rather than academic ability. Two schools used MMIs, and a third school is moving to MMIs in the next admissions round.
In contrast to the traditional one-on-one interview, during which a number of topics are covered by the same interviewer, the MMI approach uses a series of stations that examine different facets of the applicant’s personal qualities. Typically, 8 to 10 stations are used, each with a different scenario concentrating on a particular attribute (e.g, social awareness, critical thinking, ethical reasoning). Students spend 5 or 6 minutes at each station and each scenario is individually scored by the interviewer(s) for that station. The scores from individual stations are aggregated to give an overall score for each applicant. Mini-interviews originated at McMaster University Medical School in the early 2000s, and there is now considerable international experience with their use and substantial evidence of their validity and utility.23,27 Well established as a selection tool for medicine, MMIs are being increasingly used by schools of pharmacy,28 MMIs benefit the selection process by helping determine personal qualities and attributes required for future practice and by providing a greater degree of objectivity through use of standardized scenarios, scoring systems, and interviewers.21-23
Another discovery was the use of preferential entry programs, with 6 of the 7 schools recruiting “first-nation,” rural, or disadvantaged students. It would be inappropriate to have a “one size fits all” approach to this issue as contexts vary so widely. In fact, a number of countries have statutory obligations to recruit indigenous populations, and the preferential entry program for the schools in this study reflected the particular circumstances of the countries in which they were based.
It would be virtually impossible to have a common selection process because of the widely different contexts in which schools of pharmacy operate. It should, however, be possible to develop key principles for selecting future practitioners who will be working in more patient-centered roles. The pharmacy program is demanding and prior academic achievement, as reflected in high school grades or pre-entry GPAs, will rightly remain an important admission determinant. However, whether it should be the sole determinant, as is the case in one of the schools in this study, is debatable. Another consideration is whether emphasis on achievement in science subjects should be broadened to include high achievement in humanities and other subjects. This would allow for a more diverse pool of applicants. In our limited experience of selecting high-achieving applicants without the full range of stipulated prerequisites for our program (for example, biology), such candidates have performed well in their studies.
If qualities such as empathy, communication, professionalism, and moral reasoning are important attributes for future practitioners, how would these be assessed objectively at the selection stage? Mini-interviews could replace the traditional interview, but students’ prior experiences in health care and community settings, or in student organizations, are also useful indicators of future leadership or innovation potential.24,25 It is important to design selection processes that consider these nontraditional factors.
The main limitation of the current study was the small sample size of 7 universities across 6 countries, which limits the findings and generalizability. Only 9 universities in the U21 group have pharmacy program, and of these 9, only 7 responded. In addition, U21 members are a particular type of university, which further limits the wider application of the findings. The authors acknowledge these limitations but would argue that the point of the study was to use the findings from this small, selected group, to stimulate further discussion and debate on the best ways to select the pharmacy students of the future.
CONCLUSION
In this study of pharmacy student selection policies and procedures at 7 schools in 6 countries, we found marked differences and similarities in approach. Differences were primarily contextual, reflecting the varying nature of the entry-level programs in different countries. Similarities were found in the high level of academic achievement required pre-entry and in emphasis on achievement in science subjects as the main determinant. While most of the schools used some form of interview, the majority used a traditional individual interview, although a few schools had begun using MMIs. Use of pre-admission tests, personal statements, and other evidence for admission also varied. Most schools operated some form of preferential entry scheme determined by the context in which the school operated. Because of contextual diversity, a best-practice model for pharmacy student selection is unlikely. However, all schools should reflect on their selection policies and procedures in light of the changes in practice and the needs of future practitioners.
ACKNOWLEDGMENTS
The authors acknowledge the assistance of Caroline Voisine, executive officer, U21 Health Sciences Group, for assistance with distribution of the questionnaires, and the admissions directors at the participating schools.
REFERENCES
- 1.Smith J, Picton C, Dayan M. Now or never: shaping pharmacy for the future. The report on the Commission on future models of care delivered through pharmacy. Royal Pharmaceutical Society of Great Britain, London, UK. 2013. http://www.rpharms.com/promoting-pharmacy-pdfs/moc-report-full.pdf. Accessed 18 October 2015.
- 2.Department of Health. Pharmacy in England: building on strengths – delivering the future. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/228858/7341.pdf 18 October 2015.
- 3. OECD. Pharmaceutical expenditure, in OECD, Health at a Glance: Europe 2012. OECD Publishing, 2012. (doi: 10.1787/9789264183896-55-en). Accessed August 12, 2014.
- 4.Sarkar U, Lopez A, Maselli JH, Gonzales R. Adverse drug events in U.S. adult ambulatory medical care. Health Serv Res. 2011;46(5):1517–1533. doi: 10.1111/j.1475-6773.2011.01269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spinewine A, Fialova D, Byrne S. The role of the pharmacist in optimizing pharmacotherapy in older people. Drugs Aging. 2012;29(6):495–510. doi: 10.2165/11631720-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 6.DiPiro JT. Preparing our students for the many opportunities in pharmacy. Am J Pharm Educ. 2011;75(9):Article 170. doi: 10.5688/ajpe759170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Toklu HZ, Hussain A. The changing face of pharmacy practice and the need for a new model of pharmacy education. Journal of Young Pharmacists. 2013;5(2):38–40. doi: 10.1016/j.jyp.2012.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sorensen TD, Traynor AP, Janke KK. A pharmacy course on leadership and leading change. Am J Pharm Educ. 2009;73(2):23. doi: 10.5688/aj730223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Langley CA, Aheer S. Do pharmacy graduates possess the necessary professional skills? Pharm Educ. 2010;10(2):114–118. [Google Scholar]
- 10.Willis SC, Shann P, Hassell K. Who will be tomorrow’s pharmacists and why did they study pharmacy? Pharm J. 2006;277:107–108. [Google Scholar]
- 11.Keshishian F, Brenton BP. Pharmacy students’ perceptions of their curriculum and profession: implications for pharmacy education. Pharm Educ. 2011;11(1):194–200. [Google Scholar]
- 12.Jesson JK, Langley CA, Wilson KA, Hatfield K. Science or practice? UK undergraduate experiences and attitudes to the MPharm degree. Pharm World Sci. 2006;28(5):278–283. doi: 10.1007/s11096-006-9038-2. [DOI] [PubMed] [Google Scholar]
- 13.Migliore MM, Costantino RC, Campagna NA, Albers DS. Educational and career goals of pharmacy students on graduation. Am J Pharm Educ. 2013;77(9):Article 187. doi: 10.5688/ajpe779187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Svennson CK, Ascione FJ, Bauman JL, et al. Are we producing innovators and leaders or change resisters and followers? Am J Pharm Educ. 2012;76(7):Article 124. doi: 10.5688/ajpe767124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Houglum JE, Aparasu RR, Delfinis TM. Predictors of academic success and failure in a pharmacy professional program. Am J Pharm Educ. 2005;69(3):Article 43. [Google Scholar]
- 16.Kuncel NR, Credé M, Thomas LL, Klieger DM, Seler SN, Woo SE. A meta-analysis of the validity of the Pharmacy College Admissions Test (PCAT) and grade predictors of pharmacy student performance. Am J Pharm Educ. 2005;69(3):Article 51. [Google Scholar]
- 17.Bush J. Early characteristics and academic performance of students in a Master of Pharmacy degree program in the UK. Am J Pharm Educ. 2012;76(7):Article 126. doi: 10.5688/ajpe767126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schnauner SS, Hardinger KL, Graham MR, Garavalia L. Admission variables predictive of academic struggle in a PharmD program. Am J Pharm Educ. 2013;76(1):Article 8. doi: 10.5688/ajpe7718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCall KL, MacLaughlin EJ, Fike DS, Ruiz B. Preadmissions predictors of PharmD graduates’ performance on the NAPLEX. Am J Pharm Educ. 2007;71(1):Article5. doi: 10.5688/aj710105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sharif S, Bansal N, Gifford L, Morris GA, Barber J. What makes a student succeed? Pharm Educ. 2002;2(3):147–149. [Google Scholar]
- 21.Joyner PU, Cox WC, White-Harris C, Blalock SJ. The structured interview and interview training in the admissions process. Am J Pharm Educ. 2007;71(5):Article 83. doi: 10.5688/aj710583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gardner SF. Influencing admissions decisions. Am J Pharm Educ. 2008;72(4):Article 81. doi: 10.5688/aj720481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pau A, Jeevaratnam K, Chen YS, Fall AZ, Khoo C, Nadarajah VD. The multiple mini-interview (MMI) for student selection in health professions training – a systematic review. Med Teach. 2013;35(12):1027–1041. doi: 10.3109/0142159X.2013.829912. [DOI] [PubMed] [Google Scholar]
- 24.Kiersma ME, Plake KS, Mason HL. Relationship between admission data and pharmacy student involvement in extracurricular activities. Am J Pharm Educ. 2011;75(8):Article 155. doi: 10.5688/ajpe758155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Latif DA. Including the assessment of non-traditional factors in pharmacy school admissions. Ann Pharmacother. 2005;39(4):721–726. doi: 10.1345/aph.1E498. [DOI] [PubMed] [Google Scholar]
- 26. Universitas 21. The leading global network of research universities for the 21st century. http://www.universitas21.com. Accessed August 12, 2014.
- 27.Eva KW, Reiter HI, Trinh K, Wasi P, Rosenfeld J, Norman GR. Predictive validity of the multiple mini-interview for selecting medical trainees. Med Educ. 2009;43(8):767–775. doi: 10.1111/j.1365-2923.2009.03407.x. [DOI] [PubMed] [Google Scholar]
- 28.Cameron AJ, Mackeigan LD. Development and pilot testing of a multiple-mini interview for admission to a pharmacy degree program. Am J Pharm Educ. 2012;76(1):Article 10. doi: 10.5688/ajpe76110. [DOI] [PMC free article] [PubMed] [Google Scholar]