Background and Charges
According to the Bylaws of the American Association of Colleges of Pharmacy (AACP), the Academic Affairs Committee shall consider
“…the intellectual, social, and personal aspects of pharmaceutical education. It is expected to identify practices, procedures, and guidelines that will aid faculties in developing students to their maximum potential. It will also be concerned with curriculum analysis, development, and evaluation beginning with the pre-professional level and extending through professional and graduate education. The Committee shall seek to identify issues and problems affecting the administrative and financial aspects of member institutions. The Academic Affairs Committee shall extend its attention beyond intra-institutional matters of colleges of pharmacy to include interdisciplinary concerns with the communities of higher education and especially with those elements concerned with health education.”
Consistent with identifying issues and problems affecting the administrative and financial aspects of member institutions, President Patricia Chase charged the 2014-15 Academic Affairs Standing Committee to examine access, affordability, and accountability in health professions education, specifically implications and expected outcomes for academic pharmacy from the perspective of the learner and faculty.
One must take on a systems approach when discussing the three pressures on college education: affordability; access and accountability. Coined the “Iron Triangle” by John Immerwahr et al., these pressures must be kept in balance as an intervention in one area affects one or both of the other areas.1 For example, a drop in the numbers of applicants and intense competition from increasing numbers of pharmacy programs over recent years has forced colleges of pharmacy to consider a broader and more varied applicant pool. For some colleges, efforts to market to and recruit this wider audience has resulted in increased costs. Additional programming is often needed to better prepare the diverse matriculating student population for the challenges of professional graduate education. Finally, greater demands for accountability and assessment of the diverse student population from Accreditation Council for Pharmacy Education (ACPE) will also require reallocation of funds to staff assessment activities. Given all these factors influencing the “Iron Triangle”, it can be a difficult balance to achieve in pharmacy education.
The purpose of this report is to examine affordability, accessibility, and accountability from both higher education and pharmacy education perspectives and propose considerations for the key stakeholders, mainly colleges/schools, students, and faculty to deliver a pharmacy education that is desirable, attainable and of high quality. The balance between affordability, accessibility, and accountability will also be considered along with considerations of what may be perceived as the inevitable arrival of disruptive innovation to higher education that creates a simpler, more affordable educational product for a new group of students who, in most cases, were not buying (or succeeding in) the current system of higher education.2
Affordability
Higher education may have become too expensive and too cumbersome to maintain balance of the “Iron Triangle” and to successfully achieve its academic mission. The increased price of higher education with a much slower increase in family incomes has led to increased indebtedness; and, for some students, pressures to work while in school or even to defer school entry.3 Is higher education unaffordable? Affordability has been defined as “…the degree to which an institution or program provides a combination of tuition, fees, grants, loans, and time-to-completion that make worthwhile a student’s investment in his/her education.”4 Before the financial crisis of 2008, enrollments increased rather than declined despite increases in tuition over the years. However, 5 forces have impacted the higher education business model and economic viability after 2008: 1) weaker post-recession personal financial situations; 2) dwindling state funding; 3) diminishing numbers of full-paying students; 4) unbundled alternatives at a lower price being made available via online education and non-credential means of showing learning such as badge systems; and, 5) a growing value gap, i.e., college graduates questioning the value of their education given the economy and student-loan debt burden.5
In examining affordability this section will explore: 1) a model of factors that affect costs of higher (pharmacy) education; 2) trends in higher education costs in general and in pharmacy schools specifically; 3) understanding the perceived value of pharmacy education; and 4) and evaluation of: “is this where we want to be?”
1) A model of factors that affect costs of higher (pharmacy) education. Given the complex nature of the higher education business model, a two-part higher education cost model is used to examine cost associated with pharmacy education. The model was originally created to help policy makers understand the cost structure of public research universities.6 In this model, university costs are divided into two parts: 1) centers that generate their own revenue such as research, clinical services, residence halls, dining facilities, athletics, bookstore and other retail outlets (these centers are expected to be self-sustaining or revenue generating), and 2) the cost centers of student education that is paid for by a combination of state appropriations, tuition and philanthropy. 6 Both of these areas contribute to the overall cost of running an institution of higher education, whether or not they generate revenue.
The two-part model appears to be relevant to pharmacy education based on financial survey data collected by AACP.7 Between 1998 and 2013 the average cost (adjusted for inflation) per public school increased 71% while average revenues increased 128%. Increases in operational costs and compensation expenses accounted for most of the change. This would seem to be a favorable position, however, tuition increases accounted for 21% of the increased revenue, and increases in state funding accounted for 7%. Thus, the remaining bulk of the increased revenues came from enterprises other than tuition, state funds and gifts. After adjusting for inflation, the average increase in expenses per private school was 12% and the average revenue increase was 15%. Increased compensation expenses accounted for most of the increased expenditures.
2) Trends in higher education costs in general and in pharmacy schools specifically. In higher education the relationship between cost and price is not so clear because the higher education revenue streams can be comprised of tuition, government support, sales of goods and services, and indirect research support. The composition of the revenue stream may vary widely between public non-profit, private non-profit, and public for-profit organizations. The average pharmacy tuition for public institutions has increased.7
Between 1998 and 2013 the proportion of pharmacy school revenue generated by tuition increased from 4.6% to 14% at public intuitions and dropped from 72.5% to 67% at private institutions. Assuming that rising tuition is a result of rising costs is reasonable since the price charged (i.e. tuition) must cover the cost of production plus a nominal profit. However, the observed tuition increases may actually result from a change in the composition of the revenue stream rather than simply increased costs.6 As an example, state governments have used the power of the public purse in an attempt to force greater operational efficiencies in public institutions; however, tuitions have increased as state appropriations have decreased. The contribution of state appropriation as a percent of total revenue for public research institutions dropped from 54% to 46% between 1987 and 2006. During this same period tuition increased 132%. The tuition increase generated slightly more revenue than that lost by state cutbacks.6 In contrast, state allocations comprised 42% of pharmacy school revenue in 1997-98 compared to 22% in 2012-13.
It is plausible that increases in state funding were not sufficient to offset increases in faculty salary and operational expenses to support the education mission of pharmacy schools. Here too, tuition increases made up for the short-fall. Furthermore, a 2010 report by the Goldwater Institute found that inflation-adjusted spending on higher education administration increased 61% over a 14-year period ending 2007 compared to a 39% increase in instructional spending over the same time period.8
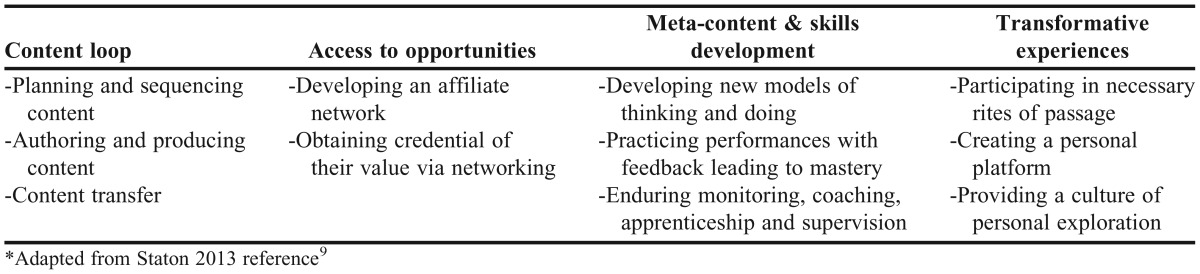
3) The perceived value of pharmacy education. A taxonomy of educational experience, created by Michael Staton to describe the educational component part of higher education that shapes students’ education, provides a useful framework to examine the implications of student expectations on process and costs of delivering a quality education.9 Table 1 highlights the 4 main components of the model. Traditionally, we concern ourselves only with curricular content and mechanisms of delivery (further described in the accessibility section), but students see the whole package.
Table 1.
The Educational Component from the Learner’s Perspective*
Cain et al. have suggested students have certain expectations in exchange for the tuition paid, namely 1) the opportunity to learn; 2) access to dedicated, expert faculty; 3) a curriculum designed to prepare them for practice; and 4) access to the necessary human and physical resources to succeed.10 The extent to which a school can effectively craft and deliver the four components of the educational experience is the extent to which graduates will perceive value for their tuition dollars. Data from the AACP Graduating Student Survey indicate an increasing trend in the percent of pharmacy graduates who do not value their pharmacy education experience.7,11 The proportion of pharmacy graduates who indicate that they would not study pharmacy if they were to choose a career again has increased from 8.0 % in 2008 to 14% in 2014 (p<0.05). While this clearly represents a minority of students, the trend is worth investigating and alleviating.
4) Is this where we want to be? In 1997 the AACP Janus Commission believed that a production model (consistent with the two-part model described above) was necessary for successful pharmacy education institutions. Using this model, the Commission recommended that schools “secure and expand pharmacy schools’ financial base beyond student tuition and state support” and identified “restructuring education to make use of the resources that are allocated” to be a challenge for the future. Furthermore, they correlated the success of the profession with the success of the pharmacy education enterprise, yet recognized that pharmacy education does little in the area of marketing and sales of its product, the pharmacist.
Based on this, the Commission urged schools/colleges of pharmacy to transform “the product and process of pharmaceutical education NOW, not eventually”.12 Looking back over the 17 intervening years since the Janus Commission report, what have we achieved? According to those data presented above, tuition dollars have funded increases in hierarchical hiring (sometimes called administrative bloat) until funds had to be diverted to cover falling state support for compensating those that are doing the teaching. There is little evidence that institutions have taken on the challenge to restructure education with bold changes to how pharmacy education is presented. At this point it seems reasonable to declare the current model of pharmacy education to be financially unsustainable and increasingly not meeting the needs of our students.
Suggestion: Colleges and schools of pharmacy must look at costs, revenue, and output from a production framework in order to be able to assess efficiencies and identify strategies for achieving economies of scope and scale to address the call of the Janus Commission to move beyond tuition or state dependence.
The healthcare environment continues to change, and curricular models that meet the dual success of the product and education process is as important today as it was in 1997. The subsequent sections of this report will address changes to the accessibility and accountability sides of the “Iron Triangle” as well as the student perspective on affordability.
Accessibility
The types of higher education institutions and the delivery mechanisms have changed over the past 50 years. Community colleges (i.e. 2-year institutions) accounted for 24% of higher education enrollment in 1963 and 48% in 2009.13 With the current proposal of free community college for everyone proposed by President Obama during the January 2015 State of the Union address, one can envision these enrollment figures to soar. Historically higher education was provided by public non-profit or private non-profit institutions. By 2001 private for-profit organizations had entered the market, accounting for 6% of the enrollment. Their market share increased to 12% by 2011. While only accounting for 12% of enrollment, for-profit institutions account for 21% of Pell Grants.14
Yet, the typical pharmacy school experience appears to remain unchanged with the Accreditation Standards focusing on curriculum length and structure with 2 years foundational, pre-pharmacy-type coursework, followed by 2 or 3 years didactic professional coursework followed by one year of experiential education. And, as with most traditional classroom education, seat time and examinations determine progress towards achievement of the program credential, ie, the Pharm.D. degree. Students who are not successful in a prerequisite course in the sequence are held back from continuing on with the original cohort. Students must attend full-time to remain on track rather than progress at their own pace as when instruction is individualized.
Tangentially but related, no matter what the level of experience with which an incoming student arrives, all in the cohort must take the same courses at the same rate of completion allowing for little-to-no flexibility. A number of pharmacy schools have tried to make degree attainment more efficient and adding to perceived value by combining degrees. The joint degree options decrease the amount of time required to obtain the two degrees individually. This may save actual tuition and fees and certainly decreases the opportunity costs of being in school. What is unknown and undocumented is the costs associated with administering these programs and whether these programs are attractive to optimistic applicants and affect program selection.
As stated in the previous section, colleges and schools of pharmacy often spend their time trying to control costs rather than rethinking the transfer of content via new curricular models. However, affordability is a key component of the business models of competency based education programs, which often aim to reduce students’ costs through a variety of delivery models.”4 Furthermore, accessibility can also be enhanced by adopting curriculum models that provide individualized, flexible, competency-based programs consistent with development of professional values.
Competency based education
Porter and Reilly discuss three competency-based curricular models that have the potential to maximize resources for student success: 1) traditional course- credit-based with alternative assessments, eg, portfolios, instead of exams, 2) prior learning assessment (PLA): recognition that advances students towards degree completion (course credits or competencies), and 3) progress through mastery of competencies, taking as little or as much time as needed to master the competency. These 3 competency based curricular models center around the idea that there are multiple ways to achieve competence and honors that one size does not fit all when it comes to education.15
Competency-based education also can “make better use of technology, support new staffing patterns that utilize teacher skills and interests differently, take advantage of learning opportunities outside of school hours and walls, and help identify opportunities to target interventions to meet the specific learning needs of students. Each of these presents an opportunity to achieve greater efficiency and increase productivity.”16 Online and computer-assisted instruction, as well as, interactive internet based connections such as Skype expand access to education—no doubt making the transfer of content more efficient. With the use of technology, data are more quickly and readily available to monitor student progress. Imagine if curricula used student performance data much like the computerized adaptive testing format of many licensing examinations (testing that adapts to the ability level of the examinee, often resulting in fewer questions needing to be used to determine level of competency). This would require the development and use of a specific learning management system, such as the College for America’s CfA Learning Environment, to monitor progress and intervene as needed.17 This is not far-fetched as some school districts are already doing this with the common core curriculum.
Pharmacy education has been spurred toward competency based education with the new ACPE Standards 2016.18 These standards were developed with input from various professional sources, including the AACP CAPE Outcomes,19 the Institute of Medicine (IOM) description of competencies that all healthcare professionals should attain during their education,20 the Joint Commission of Pharmacy Practitioners’ (JCPP) Vision of Pharmacy Practice released in 2013, and “Pharmacists’ Patient Care Process”, developed by a work group from 11 national pharmacy organizations and endorsed by the Joint Commission of Pharmacy Practitioners in 2014.21
The 2011-12 Argus Commission acknowledged disruptive innovation’s potential impact on pharmacy education by recommending that technology be used “liberally” in giving credit for prerequisite and professional school requirements by “permitting a more flexible acquisition of knowledge and skills, both in the pre-pharmacy period and in the professional program” but only if individualized, technology-based assessment tools were available and used.22 The report of the 2013-2014 Academic Affairs Committee had stated that with learning analytics “the potential exists for students to move through the curriculum autonomously, self-paced, with the goal of mastery, and with faculty roles revolving more into learning facilitator rather than content provider”.23 Though disruptive to the traditional lock-step curriculum, it would promote “creativity, life-long learning and ongoing self-assessment of knowledge and skills.” “An embracing of innovation by faculty and accreditors alike, as well as students, would be essential to the implementation of such a disruptive innovation, but the benefits could be very large.”22
Flexibility in Course and Curricular Models. There has been a welcome transition in the Academy from the historical model of the lecture focusing primarily on content delivery and exams on regurgitation of that content, to a model of active engagement during the valuable time when faculty and students are together. “Flipped” models are designed to have students acquire the necessary content before class, holding students accountable for that pre-work (through “readiness assessment), using class time for immersion in application and higher order learning, and examinations focusing on a demonstration of the enhanced cognitive abilities the model promulgates.
Not all courses are amenable to a “full flip”, and faculty experimentation has led to modifications including ‘just-in-time mini-lectures’ (eg, to address concerns that arise from the readiness assessment or during the active learning exercises), having student teams address additional background material during class time (as a form of sequential disclosure during active engagement), and alternating between primarily lecture/primarily problem solving class sessions. While these are welcome advances in teaching and learning, there is still the reality that these synchronous models (e.g., lectures, flipped models) are restricted to a certain time in a certain place, limiting flexibility for students taking the course, and contributing to curriculum rigidity when juxtaposed to other, similarly confined coursework.
The more fully hybrid and online courses introduce asynchronous possibilities that can allow students to take courses they may not otherwise be able to take, progress more quickly, and/or allow for individualized progression. With properly-designed coursework, this also increases the possibilities for individualized approaches based on learning preferences (in contrast to content-delivery lecture-based models). CAPE outcomes 4.1.1, 4.1.2, and 4.1.3 call for the student to develop a personalized understanding of their own learning (metacognition) as an important component for growth and professional development.19
There is also a need for increased flexibility as student demographics continue to change over time. Colleges of pharmacy traditionally have relied on and recruited from the immediate post-undergraduate cohort which is diminishing in many parts of the country resulting in a need and efforts to accommodate diverse markets/populations, e.g., recruiting from working adults with previous degrees who wish a career change. Typically, there are four barriers to further education for working adults: the lack of time to pursue education; family responsibilities; scheduling of course time and place; and the cost of educational courses.24
Flexible learning can be defined in terms of offering students choice in the pace, place and mode of learning.25 “Pace” includes accelerated and decelerated programs, part-time learning, recognition of prior learning, and the associated use of credit frameworks. “Place” is the primary domain of learning which is Colleges/schools of pharmacy but can include work-based learning and private or consortium-based providers of coursework. Technology-enhanced learning enables flexibility of learning across geographical boundaries. Finally, “mode” focuses on the role of learning technologies in enhancing flexibility, e.g., distance learning, blended learning, synchronous and a-synchronous modes of learning.
Programs that can easily address some of these issues will open up opportunities to this group, thus promoting some level of access and affordability. New curricular/program models are evolving to become more accessible, cost-efficient, and for some, accountable. Recent micro-disruptions to the traditional process in pharmacy education include the use of accelerated and distance, i.e., online, programs. To date, there are 14 accelerated programs in the United States, meaning professional students attend school year-round to complete the 4-year curriculum in three, comprising a burden of carrying heavier course loads with minimal breaks.7 In addition, several post-baccalaureate non-traditional Pharm.D. programs provide students with flexible online curricula.
With too little flexibility, programs may lack the capacities to adequately respond to a changing enrollment market environment and market make up. Programs with too much flexibility may run the risk of increasing costs, lacking integrity and a lowering of standards. The inclusion of competency-based education would provide some assurance of integrity with the use of common competencies advocated by ACPE. Accreditation goals are to assure minimum competencies and some level of standardization among schools/colleges of pharmacy.
Considerations before committing: Faculty Development and Support. Faculty quickly learn that creating an online course is considerably more challenging than a standard course, in terms of initial design, interaction during the course, and course upkeep. While the same fundamental elements of good course design apply (defining outcomes, defining assessment, and identifying the learning activities), one must also carefully consider the elements of delivery and engagement as well. For example, an asynchronous course expecting collaboration among teams will need to define technologies available (and expected) for all students, levels of accountability including peer assessment of contributions, and assessment of both collaborative and individual outcomes. As another example, students in a self-paced asynchronous course frequently benefit from thoughtfully identified time-dependent milestones (i.e., structured self-paced) rather than an open-ended “move at your own pace” which frequently leads to procrastination.
Since it is not intuitive for a faculty member to know how to move from a classically trained lecturer to teaching online and related coursework, faculty must be provided the appropriate academic development for teaching in these alternate educational modalities. Faculty must also have the appropriate resources (fiscal, physical, financial) to support these efforts as well. While these transformations don’t necessarily need to be expensive, the support needs to be there to provide the components and approaches that the faculty member has deemed essential for the course. Most universities will have a centralized teaching center (or equivalent) that is well-equipped to support faculty in learning new teaching methods, including these.
Many colleges/schools of pharmacy have internal programs of technical support to facilitate faculty efforts in terms of the technology to be employed and the appropriate utilization of course management systems (eg, Canvas®, BlackBoard®), freeing the faculty member to focus on the essential educational aspect of the course. Course transformation provides an excellent opportunity for faculty to develop scholarship of teaching and learning in the development, execution, and assessment of these newer course approaches. The 2011-12 Academic Affairs Report provided an excellent overview of the necessity for scholarly teaching in the Academy, and details on the essential components that define scholarly teaching.26
Whereas the 2013-14 Academic Affairs Committee Report addressed scholarship issues pertaining to emerging technologies, and called for a broader dialog across the academy and sharing of educational resources in innovative education.23 We applaud the recommendation relating to educational (course) materials and extend it to include enhanced dialog on the experimentation in hybrid/online course design to facilitate student access, flexibility, and personalized learning.
Lastly, it is also essential to gauge the culture of the school/college as to whether this type of transformation will truly be supported. Faculty become frustrated with a bait-and-switch model when they are led to believe their efforts will recognized and rewarded, only to find that is not the case. The college/school administration, as well as (if not more importantly) the executive committee/budget council making raise and promotion decisions, need to provide a consistent message of recognition for the considerable efforts required in course redesign.
Suggestion: Colleges/schools of pharmacy should engage in thinking about new ways to manage curricula to provide increased flexibility to meet the changing needs of leaners.
Demonstration Projects
For competency based education to be effective and transparent, programs must articulate what constitutes the Pharm.D. credential and explore the curricular architecture frameworks that communicates what graduates will be able to do upon graduation with the degree. In 2015, the American Medical Association (AMA) started an $11 million grant program titled “Accelerating Change in Medical Education” that is aimed at closing the gap between how physicians are educated and future health care needs.27
One area of funding examined the development of new methods for teaching and assessing competencies to create more flexible and individualized learning plans. Through these demonstration projects, colleges/schools of medicine are being allowed to explore flexible curricular delivery. Currently in pharmacy education we do not have the ability to engage in these types of demonstration projects not only due to funding issues but mainly because of the accreditation standards. For example, the curriculum must be 4 years long or equivalent which is not true competency based education where achievement of competence is not tied to a specific amount of time.
The issue of meeting accreditation standards is not new to the Academy. In 2012, Svensson, et al, stated: “Colleges and schools of pharmacy seem to be encouraged to concentrate on meeting a prescribed list of competencies and not continuing our past practices of experimenting with novel ways to educate our students”.28
Recommendation: AACP should work with ACPE to advocate for more flexibility in how curricular are structured and allow for demonstration projects in this area to make curricula competency versus hours based.
Accountability
Role of Accreditation. Self-regulation through the process and outcomes involved in accreditation are important in demonstrating accountability to stakeholders.29 Accreditation supports accountability to students, families, government agencies, and the public. The process of Self-Study and accreditation in pharmacy education is a single measure of accountability. Individual colleges/schools expend great effort in a 12-18 month time period of Self-Study, evaluating how their program measures up against the standards for the professional degree program. Peer review teams assess and validate the self-study, determining to what degree the program is compliant with the standards and extensive monitoring and follow-up is typically required.
So, is this enough to demonstrate accountability? How much is enough? When do we stop and say “it’s good enough”? Is the Self-Study process, associated with such a visit, embarked upon to ensure the necessary changes are being made to meet accreditation standards (perhaps, one could argue, for the sake of change) or is it done to ensure that the best pharmacy graduate who can meet the needs of a changing healthcare environment is being produced? Extensive resources are expended in the process of Self-Study, onsite accreditation visit, and monitoring. As an additional measure of accountability ACPE recently established a policy requiring colleges/school make specific outcomes of their program (e.g. on-time graduation rate, NAPLEX results) publicly available.30
Historically, the accreditation cycle for pharmacy education was 6 years and institutions could approach it as “one and done” endeavor. Although full accreditation has been extended to 8 years, the standards now require an ongoing, systematic approach to self-assessment with continuous program improvement at the forefront; this has yielded a marathon versus sprint approach to self-evaluation and enhancement. If colleges/schools of pharmacy are not being held accountable through a broad, all-encompassing, continuous accreditation process, then the question should be asked, why are we doing it? Are we not measuring the quality of education Vis a Vis our accreditation process?
Accountability beyond accreditation. Alternatively, or perhaps in addition to the above, one could propose that the ultimate measure of quality pharmacy education would occur when evaluating the impact of future pharmacists on healthcare inclusive of the savings in healthcare dollars and impact on improving the healthcare quality. For example, SB493 in California very specifically authorizes the pharmacist to take on an expanding role in healthcare; one that includes, among other things, ordering and interpreting tests for the purposes of managing efficacy and toxicity of drugs.31
How is it ensured that pharmacists are, indeed, being trained to meet these needs? Is it the Academy that should be held accountable for such outcomes? Or are there organizations beyond ACPE that should also be employed in this measure of accountability? Per the letter written to the people of Purdue University by its President, Mitchell E. Daniels Jr., in January of 2014, it is suggested that “higher education has been immune from close examination of its results, as reflected in value compared with price”. In other words, does the price of a pharmacy education “pay off” in its subsequent impact on society?32
Accountability to the Healthcare Environment. The Institute of Medicine report, Health Professions Education: A Bridge to Quality, highlighted that the education of health professionals including pharmacists was not adequately preparing clinicians to provide high quality care.20 The IOM challenged colleges and accreditors to develop healthcare professionals who were able to: provide patient-centered care, work as part of an interprofessional team, practice evidence-based medicine, focus on quality improvement, and use information technology. While advances in some of these areas may have been made, it’s been a decade since this report and, one could argue, substantial progress in linking education with practice and developing all graduates who are competent in these areas has not been realized.
Pharmacy education in the United States is regulated by the Accreditation Council for Pharmacy Education and ultimately, the U.S. Department of Education. In most countries, governments are responsible for the quality of health professions education either through a department or ministry of education or health. Infrequently, responsibility for the quality of education for health professionals lies with a national pharmacy organization.33
For example, in 2009 the Ministry of Health and Social Welfare (MOHSW) in Tanzania identified the pharmacy workforce was insufficient to provide care to the country’s population. The MOHSW recommended changes in how pharmacists were trained so they could expand their scope of practice and provide services beyond drug distribution. Moreover, they recommended additional training for pharmacy faculty and development of additional pharmacy schools to increase capacity.34
In a commissioned report regarding educating health professionals for the 21st century, it was identified that education is crucial to transforming the healthcare system.35 Certainly, the healthcare system has become increasingly costly and complex. Accordingly, the professional education system must keep pace by offering instructional approaches that adequately prepare each of our graduates to not only function in this environment but to transform it through continuous quality improvement.
Although pharmacy education has been attempting to address the 5 core areas outlined in the IOM report from a decade ago, and the standards for pharmacy accreditation have become increasingly complex and rigid, the question becomes, Are we where we want to be in terms of preparing our graduates to work in and transform the current health care system? Do our students see the connection between their education and practice? Do they feel accountable to their patients and understand the responsibility of being a pharmacist?
A strong connection between pharmacy education and patient care is critical for students to see the connection and feel accountable to their patients, their families, and their healthcare colleagues. We want to educate and train individuals who are able to maximize the healthcare of their patients as pharmacists. In order to practice at the top of their license and transform practice, we need to leverage pharmacy education to do so.
Would a better connection between education and practice facilitate this? The Department of Health and Human Services has no responsibility or impact on health professions education. Similar to the relationship between the Ministry of Health and the Department of Education, Training and Employment in some countries, collaboration between the DHHS and the Department of Education conceivably could better support the vision of connecting students with practice in an education system that is focused on clinical practice and the service of patients.
It is recognized that a strong relationship between the health and science sectors of society and the government and pharmacy education is of extreme importance in maximizing pharmacy’s contributions to the delivery of quality, cost-effective healthcare.33 And it has been determined that improved healthcare (quality and cost) must include a focus on individuals and families; a redesign of primary care services and structures; population health management; a cost control platform; and system integration and execution.36 Preparedness of this through pharmacy education cannot be understated.
Recommendation: AACP should work with ACPE, the Department of Education, and the Department of Health and Human Services to explore a collaborative approach to measures of accountability for pharmacy education to the healthcare environment and improvement of patient care.
Affordability and accountability from the student perspective
The preceding sections have reviewed the three sides of the “Iron Triangle” from the institutions perspective. Since it was discovered in the previous affordability section that the students were bearing the brunt of the increases in higher education cost through tuition and finding decreasing value for their money, we revisit the affordability and accountability but this time from the student perspective.
Affordability for students. Making education more affordable to students in these modern times is a dynamic challenge. Students have a number of aid options including federal, state and institutional grants; guaranteed and non-guaranteed student loan programs; and work-study programs.37 States have also increased their need-based and non-need-based grant programs. Roughly 30% of all state grants and 55% of institutional grants are not based on need. Students in middle upper and upper income groups often take on non-secured debt from private lenders.37 While the average Pell Grant award increased to $4,500 in 2011, the actual purchasing power of the award decreased to 32% from 33% of public 4 year tuition in 1976-77 (adjusted for inflation).38
Between 1979-80 and 2008-09 total federal grant expenditures increased 28% (to $24.8 billion) while student loan borrowing increased 577% (to $84.0 billion/year) adjusted to 2008 dollars.37 The total student loan debt crossed the $800 billion mark in 2010.39 Forty-one percent of students in private 4-year universities and 54% of students in private nonprofit 4-year universities accumulated student debt in 2007-08.
While the average debt load for undergraduates is about $25,000, students in private schools, graduate school and professional programs accumulate more debt.38 Some have questioned if students are taking loans to finance a life-style rather than financing their education. The three potential problems with large student debt load are that 1) it may direct students to high-paying jobs at the expense of lower-paying career-development opportunities; 2) if students don’t understand the loan repayment terms it can compromise the financial solvency of graduates and impede future investments and economic growth; 3) the value of the college education may not be worth the long-term cost.39
Research on student aid programs over the past 59 years has revealed the following: that aid programs increase access to education; the complexity of the application process can be a deterrent for some to access aid; adding academic incentives to aid, increases average GPAs and may improve persistence; and, students/families may not understand the long-term implications of loan repayment when they take out the loans.38 Therefore, a current trend in higher education is to help students learn how to handle money and debt. The Apollo Research Institute conducted a study and discovered the top psychosocial issue most frequently experienced by college students was anxiety and stress over college-related expenses.40 Recent graduates feeling overwhelmed by their student loans may benefit from taking a look at a comprehensive guide to state and federal pharmacy student loan forgiveness programs. Pharmacists currently qualify for three federal loan repayment programs.
The National Health Service Corps (NHSC) Loan Repayment Program offers up to $50,000 for providers working for 2 years in a qualified site in a health professions shortage area. Eligible sites include (Federally-Qualified Health Centers (FQHCs); and Rural Health Clinics. Qualified sites exist in all 50 states. The Faculty Loan Repayment Program offers up to $40,000 for trained health professionals from disadvantaged backgrounds who serve on faculty for two years. While the NHSC Loan Repayment program and the Faculty Loan Repayment program support individuals, the State Loan Repayment Program (SLRP) is a federally funded program that offers matching dollars for states to operate their own loan repayment programs. Roughly 30 states obtain matching funds through this program. Eligible participants must work in Health Professional Shortage Areas (HPSAs) within their state.9
Accountability to students The cohorts of students admitted to pharmacy schools today a have a diverse mixture educational and work experiences. In the digital age we have digital natives (students who have grown up with technology) and digital immigrants (students who are pre-digital age) and include our faculty. The amount of material that students need to be familiar with is growing exponentially, therefore there are too many facts for any individual to commit to memory. Competency-based curriculum requires students to have clinical knowledge, skills, and attitudes required to deliver patient care and perhaps skills that can be used in other healthcare settings such as industry, public health, drug information, and academia. Students want to use their time efficiently and have more hands on experiences to learn material. Students also value engaging with faculty in meaningful ways. Faculty are facilitators of student learning and developers of cutting edge curriculum.
Other ways to increase the perceived value of the education received by students is once enrolled, programs should encourage students to become immersed in the organizational and professional culture of the pharmacy field and learn to appreciate varying opportunities for their careers and what services the school/program provides that may facilitate their performance while in school and their preparation for life after graduation, e.g., services or programs such as opportunities to develop leadership capabilities or to prepare for next-level training/education (residencies, fellowships, MS/PhD graduate programs). The breadth of elective course and non-traditional experiential offerings, as well as, formal mentoring/advising programs and career counseling, development and placement opportunities can provide individualized assistance and result in satisfaction with the program and the choice of the pharmacy profession. Availability of honors programs and opportunities to conduct research open up students’ skill development beyond typical pharmacy education content and career opportunities.
Suggestion: Schools or Colleges of Pharmacy should 1) continue to help students navigate the financial aid process and utilize a variety of aid other than loans; 2) provide student access to financial management programs to enable them to manage debt and newly earned salaries; and 3) consider all educational components from the student’s perspective in order to enhance the value of pharmacy education.
CONCLUSION
The academic affairs committee set out to address the affordability, accessibility and accountability of a pharmacy education. But it became quickly apparent that the rising costs of higher education was the burning platform that demanded immediate attention. So the question then became, with the “Iron Triangle”, is there a way to make education more affordable and at the same time increase access and maintain accountability? We believe that there is.
Educational models that move from the rigid lecture model to more hybrid or fully flexible coursework introduce asynchronous possibilities that expand student access while at the same time reduce cost of delivery. But this type of curricular model does demand a change in the manner in which we hold ourselves accountable. Depending on design, these approaches could allow students to take courses they may not otherwise be able to take, progress more quickly, increases the possibilities for individualized approaches based on learning, and allows for individualized costs to the institution and student based on progression. In order for faculty to move course design in this direction, the appropriate faculty development and resources need to be identified, and the rewards structure needs to recognize the considerable effort that is needed to develop and sustain new models.
Furthermore, since the reduced costs are associated with reduced faculty teaching time, faculty need assurances that their time can be used for creating new revenue streams. Although there has been a contraction in NIH funding for science faculty to obtain, we are encouraged by the recent expanding of fundable practice opportunities and provider status initiatives for pharmacy practice faculty. Lastly, in order for this type of innovation to occur in our programs, we need to rethink to whom we are accountable. As stated by the 1997 AACP Janus Commission, the success of the pharmacy education enterprise is dependent on the success of the profession.
We need to move beyond ACPE educational standards and create measures of accountability for pharmacy education to the healthcare environment.
REFERENCES
- 1.Immerwahr J, Johnson J, Gasbarra P. The Iron Triangle: College Presidents Talk about Costs, Access, and Quality. A Report from The National Center for Public Policy and Higher Education and Public Agenda, October, 2008. http://www.highereducation.org/reports/iron_triangle/IronTriangle.pdf. Accessed March 23, 2015.
- 2.Soares L. A. “Disruptive” Look at Competency-Based Education: How the Innovative Use of Technology Will Transform the College Experience. Center for American Progress; 2012. https://www.americanprogress.org/issues/higher-education/report/2012/06/07/11680/a-disruptive-look-at-competency-based-education/. Accessed March 23, 2015.
- 3. Losing Ground: A National Status Report on the Affordability of American Higher Education. San Jose, CA: National Center for Public Policy and Higher Education; 2004.
- 4.Everhart D. Clarifying competency based education terms. On American Council on Education and Blackboard blog. http://blog.blackboard.com/clarifying-competency-based-education-terms/. Accessed March 23, 2015.
- 5.Selingo JJ. College (Un) Bound. Boston, MA: Houghton Mifflin Harcourt Publishing; 2013. [Google Scholar]
- 6.McPherson P, Shulenburger D. Understanding the cost of public higher education. Planning for Higher Education. 2010:15–24. [Google Scholar]
- 7. D. Taylor, American Association of Colleges of Pharmacy, March 27, 2015.
- 8. Greene JP, Kisida B, Mills J. Administrative bloat at American universities: The real reason for high costs in higher education. Policy Report No. 239. Phoenix, AZ: The Goldwater Institute; 2010:1–19.
- 9.Staton M. Unbundling Higher Education: Taking Apart the Components of the College Experience. In: Kelly AP, Carey K, editors. Stretching the Higher Education Dollar. Cambridge, MA: Harvard Education Press; 2013. pp. 105–124. [Google Scholar]
- 10.Cain J, Noel Z, Smith KM, Romanelli F. Four rights of the pharmacy educational consumer. Am J Pharm Educ. 2014;78(6):Article 115. doi: 10.5688/ajpe786115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Association of Colleges of Pharmacy. Graduating Student Survey. 2014 National Summary Report. http://www.aacp.org/resources/research/institutionalresearch/Documents/2014_GSS_Final%20Summary%20Report_All%20Schools_117_for%20web.pdf. Accessed March 27, 2015.
- 12.Bootman JL, et al. Approaching the Millennium: The Report of the AACP Janus Commission. Am J Pharm Educ. 1997;61(4) [Google Scholar]
- 13.Baum S, Kurose C, McPherson M. An overview of American higher education. The Future of Children. 2013;23:17–39. doi: 10.1353/foc.2013.0008. [DOI] [PubMed] [Google Scholar]
- 14.Baum S, Payea K. Trends in Student Aid 2012. New York College Board. 2012 [Google Scholar]
- 15.Porter SR, Reilly K. Competency-based education as a potential strategy to increase learning and lower costs. Washington, DC. http://hcmstrategists.com/maximizingresources/images/CBE_Paper.pdf. Accessed March 23, 2015.
- 16.Competency-based learning or personalized learning. US Department of Education. http://www.ed.gov/oii-news/competency-based-learning-or-personalized-learning. Accessed March 23, 2015.
- 17.Lewis J. CfA Learning Environment (CLE). EDUCAUSE 2014. Nextgenlearning.org. Accessed March 23, 2015.
- 18.Accreditation Council for Pharmacy Education. Accreditation Standards and Key Elements for the Professional Program Leading to the Doctor of Pharmacy Degree (“Standards 2016”) https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf. Accessed May 18, 2015.
- 19.Medina MS, Plaza CM, Stowe CD, et al. Center for the advancement of pharmacy education 2013 educational outcomes. Am J Pharm Ed. 2013;77(8):Article 162. doi: 10.5688/ajpe778162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Institute of Medicine Committee on the Health Professions Education Summit. Greiner AC, Knebel E, editors. Health Professions Education: A Bridge to Quality. Washington (DC): National Academies Press (US); 2003. http://www.ncbi.nlm.nih.gov/books/NBK221528. Accessed January 19, 2015.
- 21.Joint Commission of Pharmacy Practitioners. Pharmacists’ Patient Care Process May 29, 2014. https://www.accp.com/docs/positions/misc/JCPP_Pharmacists_Patient_Care_Process.pdf. Accessed May 18, 2015.
- 22.Speedie MK, Baldwin JN, Carter RA, Raehl CL, Yanchick VA, Maine LL. Cultivating ‘habits of mind’ in the scholarly pharmacy clinician: Report of the 2011-12 Argus Commission. Am J Pharm Educ. 2012;76(6) doi: 10.5688/ajpe766S3. Article S3;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cain J, Conway JM, DiVall MV, et al. Report of the 2012-13 academic affairs committee. Am J Pharm Educ. 2013;78(10):Article S23. doi: 10.5688/ajpe7810S23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cahalan M., Lacireno-Paquet N., Silva T. 1998. Adult education participation decisions and barriers: review of conceptual frameworks and empirical studies. Washington, DC: US Department of Education, Office of Education Research and Development, National Center for Education Statistics.
- 25.The Higher Education Academy. Flexible Learning Summit Report. https://www.heacademy.ac.uk/sites/default/files/resources/FL_summit_report_final.pdf. Accessed May 18, 2015.
- 26.Mason HL, Assemi M, Brown B, et al. Report of the 2011-12 academic affairs standing committee. Am J Pharm Educ. 2012;75(10):Article S12. doi: 10.5688/ajpe7510S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.American Medical Association. Accelerating Change in Medical Education. http://www.ama-assn.org/sub/accelerating-change/overview.shtml. Accessed April 22 2015.
- 28.Svensson CK, Ascione FJ, Bauman JL, et al. Are We Producing Innovators and Leaders or Change Resisters and Followers? Am J Pharm Educ. 2012;76(7):Article 124. doi: 10.5688/ajpe767124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Accreditation and accountability. looking back and looking ahead, Council for Higher Education Accreditation. http://www.chea.org/pdf/accred_account.pdf. Accessed January 5, 2015.
- 30.Policies and procedures for ACPE accreditation of professional degree programs. Accreditation Council for Pharmacy Education. https://acpe-accredit.org/pdf/PoliciesProceduresJuly2014.pdf. Accessed December 12, 2014.
- 31.Bill No Senate. 493, Chapter 469. An act to amend Sections 733, 4040, 4050, 4051, 4052, 4052.3, 4060, 4076, 4111, and 4174 of, and to add Sections 4016.5, 4052.6, 4052.8, 4052.9, 4210, and 4233 to, the Business and Professions Code, relating to pharmacy. http://leginfo.legislature.ca.gov/faces/billStatusClient.xhtml Accessed March 8, 2015.
- 32.An open letter to the people of Purdue. http://www.purdue.edu/president/email/2014/1401-med-openletter.html . Accessed February 3, 2015.
- 33.A global framework for quality assurance of pharmacy education. FIP Pharmacy Education Task Force, International Pharmaceutical Federation. http://www.fip.org/files/fip/PharmacyEducation/QA%20Booklet.pdf. Accessed Jan 5, 2015.
- 34.Youmans S, Ngassapa O, Chambuso M. Clinical pharmacy to meet the health needs of Tanzanians: education reform through partnership across continents (2008-2011) J Public Health Policy. 2012;33(Suppl 1):S110–S125. doi: 10.1057/jphp.2012.44. [DOI] [PubMed] [Google Scholar]
- 35.Frenk J, Chen L, Bhutta ZA, et al. Health professional for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376:1923–58. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 36.IHI Triple Aim Initiative. The Institute for Healthcare Improvement. http://www.ihi.org/engage/initiatives/TripleAim/Pages/default.aspx. Accessed February 2, 2015.
- 37.Heller DE. The Financial Aid Picture: Realism, Surrealism, or Cubism? In: Weidman JC, editor. Economics and Finance of Higher Education. Boston, MA: Pearson Learning Solutions; 2014. pp. 137–163. [Google Scholar]
- 38.Dynarski S, Scott-Clayton J. Financial Aid Policy: Lessons from Research. In: Weidman JC, editor. Economics and Finance of Higher Education. Boston, MA: Pearson Learning Solutions; 2014. pp. 99–117. [Google Scholar]
- 39.Avery C, Turner S. Student Loans: Do College Students Borrow Too Much – or Not Enough? In: Weidman JC, editor. Economics and Finance of Higher Education. Boston, MA: Pearson Learning Solutions; 2014. pp. 321–341. [Google Scholar]
- 40.Shepp D. Top 6 Reasons Adult College Students Drop Out. jobs.aol.com. http://jobs.aol.com/articles/2012/08/13/top-6-reasons-older-college-students-drop-out/. Accessed March 23, 2015.