Abstract
A growing body of social science research has sought to conceptualize race as a multidimensional concept in which context, societal relations, and institutional dynamics are key components. Utilizing a specially designed survey, we develop and use multiple measures of race (skin color, ascribed race, and discrimination experiences) to capture race as “lived experience” and assess their impact on Latinos’ self-rated health status. We model these measures of race as a lived experience to test the explanatory power of race, both independently and as an integrated scale with categorical regression, scaling, and dimensional analyses. Our analyses show that our multiple measures of race have significant and negative effects on Latinos’ self-reported health. Skin color is a dominant factor that impacts self-reported health both directly and indirectly. We then advocate for the utilization of multiple measures of race, adding to those used in our analysis, and their application to other health and social outcomes. Our analysis provides important contributions across a wide range of health, illness, social, and political outcomes for communities of color.
Keywords: Race, Ethnicity, Self-Reported Health, Lived Experience, Skin Color, Ascribed race, Discrimination
...there are those who study race and racial dynamics, and those who routinely use the concept of race in their studies. In the case of the former…. race is seen as a profoundly social characteristic. The dynamism and fluidity of race is often used to better understand related social processes. …Racial delineations … result from historical patterns of racial hierarchy embedded in ongoing interactions…. In the case of the latter … those who use race or ethnicity in their research, as opposed to those who study race, tend to treat it as a primordial or fixed characteristic. …. as a function of fixed differences between “populations”…. race is conceptualized as a cause of myriad of social processes and distinctions.
-Angela James, “Making Sense of Race and Racial Classification,” Race and Society, (2001, p. 235–247)
INTRODUCTION
Our research places concerted attention on the conceptualization and measurement of race, developing multi-dimensional measures of race/ethnicity and then examining their impact on self-reported health status among U.S. Latinos. While our collective efforts have been directed toward a fuller understanding of the extent of racial/ethnic health disparities, we have reached the conclusion that the manner in which race and ethnicity are measured requires re-thinking and developing measures of race in a more complex manner. Thus, the breadth of research on race/ethnicity needs to reflect race as a “lived experience.” It is only recently that different and multiple measures of race/ethnicity have been utilized to assess the impact of these important factors on health status (Saperstein and Penner, 2012; Miller and Wilson, 2003). Our interest lies in examining the impact of multiple measures of race/ethnicity on the self-reported health status of U.S. Latinos. This community can pose a challenge in the discussion of race and ethnicity. In this analysis, we develop and advocate for a multi-dimensional model of race/ethnicity to examine the collective impact of race as a lived experience on the health status of U.S. Latinos. More specifically, we utilize a unique survey that included several items that capture dimensions of race as a lived experience. These dimensions of lived experience include: skin color, ascribed race, and discrimination experiences.
We see our major contribution as constructing measures of race/ethnicity and modeling these measures more comprehensively than the more limited nominal categories of racial/ethnic groups. As many social scientists would contend, race is much more complex than a single categorical variable. Using this particular array of measures constructs ‘race’ as a measurement-related endeavor, advancing the explanatory power of race in health disparities. In this analysis, we assess the process by which skin color, ascribed race, and discrimination experiences influence self-rated health among U.S. Latinos. We hypothesize that these three measures of race, interpreted as the lived experience of people of color, are negatively correlated with self-rated health status. We use two approaches to test this hypothesis. The first is a modeling approach that uses traditional categorical regression models that specify skin color, ascribed race, and discrimination experiences independently. Our next approach uses scaling and dimensional analysis to combine and scale our race measures into one multidimensional measure of race as a lived experience.
This research design allows for a discussion of how the utilization of multiple measures of race can broaden our understanding of the mechanisms by which race impacts Latino health. In addition, we highlight methodological concerns associated with more complex measures of race. Our results will be of interest to all researchers seeking to understand how race influences social, political, and health outcomes in the United States.
We begin this paper with a discussion of the literature and theory focused on racial/ethnic health disparities and the various measures of race/ethnicity employed in this area of work; next we describe our research design and methods; and then present the results of our analyses and implications for future research. We demonstrate that not only are discrimination experiences and skin color negatively associated with self-rated health status, but a scale of race/ethnicity capturing race as a lived experience for persons of color is also negatively correlated with self-rated health status. Such findings suggest that incorporating a multidimensional approach to the study of race advances our knowledge of the relationship between race/ethnicity and health outcomes.
THE STUDY OF RACE/ETHNICITY AND HEALTH
The study of racial and ethnic health disparities has taken major strides of late, both theoretically and empirically. We reviewed hundreds of studies that have confirmed the persistence of pervasive racial/ethnic inequities in the delivery of healthcare, health outcomes, and health status. There has been a relative explosion of insightful research focused on uncovering how race and ethnicity influence health in the United States (see for example; Chae et al., 2011; Woo et al., 2011; Vireull-Fuentes 2011; Sternthal 2011; James et al., 2007; Satcher et al., 2005; Smedley et al., 2003; Waidmann and Rajan, 2000; Berenson et al., 1996).
Further symbolizing the growth of this research direction, a recent volume co-edited by Nancy Lopez and Laura Gomez (2013) titled “Mapping ‘Race’: Critical Approaches to Health Disparities Research” contains a notable collection of social science research advocating for a more in-depth approach to the measurement of race by matching the measures with the complexities of this concept, an approach which is critical to health disparities research. For example, the chapters by Garcia (2013) and by Saperstein (2013) discuss and develop multi-dimensional measures of the lived experiences of racial/ethnic group members. They discuss the limitations of treating race as simply a categorical variable that does not capture the full range of individual, structural, and historical components of what race and ethnicity mean in contemporary U.S. society. In addition, the chapter by Gravlee presents developed measures that represent a fuller meaning of race (Gravlee 2013). Although the work of social scientists highlighted in this edited volume symbolizes the advancements in this area of research, we believe that there remains room for continued growth.
Early health researchers approached the study of race and health within the context of genetic and biological differences between the races, often assuming that observed differences in health conditions were due to underlying genetic or biological differences (Boyle 1970; Keil et al., 1977; Gardner et al., 1984). We do not treat race as a genetic or biological construct. We utilize a social determinants of health framework which asserts that race is a socio-cultural construct and that racial and ethnic minorities suffer from poorer health outcomes compared to non-Hispanic Whites due to their environments, social status, limited opportunities, and experiences with discrimination in the United States (Williams and Sternthal, 2010; Massey 2004; Schultz et al., 2002).
We call this perspective “lived experiences for racial/ethnic groups.” Our emphasis places greater attention on internal variation within existing racial and ethnic categories while simultaneously acknowledging the complexities associated with the concept of race/ethnicity itself. We contend that traditional distinctions between race and ethnicity are highly problematic when studying their impact on outcomes in the contemporary U.S. context. For example, for ethnicity, acculturation-based explanations for poor health outcomes among Latinos assume that as individuals lose protective cultural traits with increased time in the U.S., their health deteriorates. This conceptualization of culture not only essentializes groups but also fails to capture the fluidity of collective systems of meaning and action. The ways in which inter-subjective systems of meaning emerge and shift under specific social, historical, and political contexts is critical to understanding culture and groups (Grosofoquel 2011; Benhabib 2002; Viruell-Fuentes 2011). Furthermore, because this model locates culture within individuals, it diverts our attention away from the structural conditions that impact individual and community health status.
Our approach is consistent with the work of critical race theorists who similarly emphasize the socially constructed nature of race. Recent scholarship has applied this theoretical framework to health outcomes (Thomas et al., 2011; Ford and Airihenbuwa, 2010). Critical race theory (CRT) provides a useful framework for our analysis, as it is a trans/multi-disciplinary approach that explicitly addresses the role of individual-level discrimination and structural racism in population-and individual-level health. Ford and Airhihenbuwa (2010) have developed a CRT-based methodology specifically for public health research. Public Health Critical Race Praxis (PHCR) is an “attempt to move beyond merely documenting health inequities toward understanding and challenging the power hierarchies that undergird them” (Ford and Airhihenbuwa 2010, p. 1390). PHCR is grounded in the basic CRT tenet that posits race and racialization as central facets of health and generalized inequality (Delgado and Stefancic, 2001; Ford and Airhihenbuwa, 2010). Thomas et al. (2011) advance the foundations of CRT by advocating for a new generation of research they call health “critical race praxis,” which, among other things, calls for advanced methodological tools that can address racism and structural inequality. Our attempt to provide clarity in the measurement of race within the context of health disparities is very much in line with this overall framework.
Acknowledging that race and ethnicity are social constructions that evolve from systems of power, ideology, and stratification, we focus on the dialectical relationship between insiders and outsiders. We explore the ways in which hierarchical social relations produce poor health outcomes through the intersection of race and ethnicity. Our study builds on a growing body of ethno-racial research that documents how racialized, nativist policies adversely impact the health of Latinos and particularly Latino immigrants. This work investigates how individuals from a number of Latin American countries negotiate the tensions between constructing a sense of ethnic belonging while simultaneously confronting stigmatizing environments embedded within the current U.S. racial order (De Genova 2004; Viruell-Fuentes 2011).
For instance, Browne and Odem (2012) demonstrate that in the Southern U.S., where the old Black-White dichotomy is still dominant, local policymakers have created new dimensions of racial stratification by lumping Dominican and Guatemalan immigrants together and imposing laws which criminalize immigrants and exclude them from important resources such as health care, education, and housing. Similarly, Gomberg-Munoz (2012) elucidates how states and industries highly dependent on unauthorized Mexican workers have promoted stigmatizing rhetoric about their illegality, which facilitates the exploitation of these workers over time. This criminalization of Mexican workers depresses their wages and creates working conditions that heighten their vulnerability. Specific to health, Viruell-Fuentes (2011) demonstrates that Mexican immigrant women and second generation Mexican American women face considerable stress in negotiating ethnic identities under stigmatizing environments, and this may be a key mechanism by which living in a racialized society adversely affects health outcomes. In sum, we build on this rich qualitative literature by testing the impact of perceived Latino ethno-racial stratifications on health status by focusing on three key dimensions of these lived experiences: skin color, ascribed racial status, and experiences of discrimination. We now turn to a brief explanation of each construct.
Skin Color
A primary measure associated with the lived experiences of people of color is skin color.ii Social scientists have found that phenotype, in this case skin color, impacts many social outcomes for African Americans. Darker skinned African Americans on average make less money (Keith and Herring, 1991; Bowman et al., 2004; Hersch 2006), live in more highly segregated areas (Massey et al., 2003), and even have a more difficult time garnering votes when running for office than African Americans with lighter skin color (Terkildsen 1993). In short, skin color serves to pattern significant marginalization among African Americans (Cohen 1999).
Lesser developed is a research literature focusing on the role of skin color on social outcomes for Latinos. For example, Telles and Murguia (1990) find that darker skinned Mexican Americans receive lower earnings than their lighter skin co-ethnics. Similarly, Morales (2008) finds that skin color can lead to Latinos being segmented within labor markets, with darker skin Latinos being stratified into lower-waged sectors of the labor market. Taking a more in-depth examination of the impact of skin color on occupational prestige, Espino and Franz (2002) find that skin color magnifies lower prestige for Latinos of Mexican and Cuban origin but not for Puerto Ricans. Specific to political equality, Tafoya (2004) finds that a U.S.-born Latino’s whiteness is clearly and consistently associated with higher social status, higher levels of civic participation, and a stronger sense of social acceptance. Finally, scholars have compared the impact of phenotype across countries (Uhlmann et al., 2012; Telles and Steele, 2012; Perreira and Telles, 2014).
Many early health researchers approached the study of the impact of skin color on health with the assumption that they were testing the impact of genetics on health outcomes. The vast majority of this early work was on the relationship between skin color and hypertension among African Americans (Boyle 1970; Harburg et al., 1978; Keil et al., 1977, 1 1992; Klag et al., 1991). One study found an association between skin color and cancer deaths among African Americans (Knapp 1995), and another found an association between skin color and diabetes among Mexican Americans (Gardner et al., 1984). For the most part, early skin color/health studies were not conceptualizing skin color as a marker for racism or discrimination but rather as a marker for genetics and/or biology. In the last two decades, research has moved toward a more social construction interpretation of the relationship between skin color (or colorism) and health outcomes (see Krieger 1998; Klonoff 2000). This research has found that individuals with darker skin tend to have poorer health (Gravlee et al., 2005; Klonoff and Landrine, 2000).
A more recent development in work exploring the relationship between skin color on health, as well as discrimination and privilege, is to extend this examination beyond African Americans. Studies over the last decade have placed greater emphasis on the continuing significance of skin color as marker of status, stratification, and racial distinctions across many different minority populations (i.e. Latinos, Asian Americans, and Native Americans) (Gomez 2000; Harris 2002; Hochschild 2011). For example, Sanchez and Ybarra (2013) find that skin color is negatively correlated with self-reported health status among Latinos, such that darker skin Latinos report worse health status than their lighter skin counterparts.
The inclusion of skin color as an indicator of race produces measurement challenges that have been addressed in several different ways. Most commonly, the respondent is placed in a skin tone category (ranging from lighter to darker skin ratings) based on her/his self-report or the report of an external observer. It seems clear that a respondent’s basis for such self-assignment (as well as the third party’s) will be based on the individual’s experiences, self-concept, social identity/ies, social networks, and other external influences. For our part, we have operationalized the skin color measure based upon a self-reported five-point scale on a continuum from very light to very dark.
Social meaning and value in U.S. society place more a positive value on being lighter so that the full range of the scale is seldom utilized; instead, a skewed distribution toward the “lighter” side of the scale is common (Garcia 1991). A related approach has been the interviewer’s placement of the respondent on the skin color scale. This has resulted in “race-of-interviewer effect” in which interviewers perceive greater variations in the skin tones of same race respondents than among different race respondents (for example, Black interviewers categorized White respondents as lighter than their White interviewer counterparts and vice versa) (Hill 2002). More recently, Chan et al. (2005) have included both self-reported skin “phenotype” as well as readings from a narrow band reflectance spectrometer. The primary purpose of this approach was to make “precise” measures of skin color to be used in the evaluation of patients and expand the clinical information collected (Chan et al., 2005). The accuracy and precision of a reflectance spectrometer fails to capture the social meaning, status, and context from which skin color and race as a social construction are interconnected.
Social science scholars of health outcomes, such as Gravlee (2005), find that ascribed skin color (rather than a specific racial category) is more important in predicting health outcomes than the more “objective” clinical measure of reflectometer-determined skin color.iii These findings have potential implications for skin color measurement and begin to move towards the more structural/societal aspects of racism that Dressler et al. (2005) and others (Gee and Ford, 2011; Williams and Mohammed, 2009) note as having greater impact on health outcomes. This interconnection is taken into account in our model for our three measures of race. It is not skin color as a clinical measure that we are interested in; rather it is the contribution of skin color to the social construction of race.
Ascribed Race/Ethnicity
Perceptions of others’ racial classifications represent the socio-political and structural underpinnings of the complexity and multi-dimensionality of race. While some researchers (Prewitt 2005; Hochschild et al., 2011) have proposed the supplanting of skin color over the traditional categories of race, there is greater consensus that a broader conceptualization of race needs to include the phenotypic measure of skin tone/color (LaVeist 1994; Williams 1997; Woo et al., 2011). The measurement challenges of two “sources” of skin color “categorization” do complement our notion of the complexity of race. Building upon our discussion of the multidimensional construction of race, the relational nature of race clearly indicates that categorization and identification of race extends beyond the individual. That is, factors affecting a person’s racial identification and lived experiences are shaped by social structures, common perceptions/stereotypes, norms and beliefs, and treatment by others (Frank et al., 2010).
Our second dimension of race deals with racial “categorization” of individuals by others. While it can be related to skin color, racial classification maintains extant notions about racial groupings in society. Many surveys ask interviewers to place their respondents into racial categories (Telles and Lim, 1998), or respondents’ perceptions of their racial identification by others are part of the many dimensions of race (Tashiro 2002). We can call this aspect of race “externally ascribed race” or “perceived race.”
Externally ascribed race is an interesting and yet relatively understudied dimension in the study of race. Social identities indicate who we are, who other people are, and, receptively, who other people think we are (Helms 1990). As a result, race as lived experiences includes the implications of being “categorized racially” by others. For example, psychologists have begun to differentiate between imposed ascribed identities and those chosen by individuals. Imposed ascribed identities were those assumed by White counselors and psychologists about their clients of color rather than characteristics of self-identity that are measured. For the most part, inferences were being made solely on physical appearance (Hogg and Terry, 2002). Martinez (2002, 67–73) tells the story of person of color growing up in a predominantly White, upper-middle class community and first coming to the realization that others saw her as non-White.
To our knowledge, Jones et al. (2008) are the only scholars who directly measure ascribed race, or “socially assigned race,” iv as we have done here to examine impacts on health status. They find that for Blacks, Hispanics, and Native Americans discordance between their self-identified race/ethnicity and their socially assigned race (i.e. being socially assigned as White) is most predictive of better health status regardless of self-identified race. A more recent study by Saperstein (2009) finds that perceived race more strongly predicts differences in screening outcomes than self-identified race. From this finding, Saperstein argues that “the results are more consistent with recent attention to the role of discrimination and implicit prejudice in clinical encounters.”
Discrimination Experiences
When focusing on race, experiences of interpersonal racial discrimination are a prominent measure, thus we cannot talk about race without talking about discrimination and racism.v Social science scholars have found that experiences of interpersonal racial discrimination foster group identity among racial and ethnic groups (Bernal and Martinelli, 1993; Masuoka 2006). In the African American politics literature, linked fate is an appropriate connection to our discussion. For example, Michael Dawson’s (1995) theory of the Black utility heuristic posits that the historic and continued role of racial discrimination in the United States is the basis for linked fate for Blacks. Continuous exposure to racial discrimination makes African Americans more aware of their racial identity, and therefore heightens a sense of linked fate.
Similarly, Latinos have been subject to a long history of discriminatory and exclusionary practices by non-Latinos (see Cobas et al., 2009; and Garcia 2008 for a review of this literature). For example, the Latino population has endured the challenges historically associated with forced segregation, including having separate and unequal facilities like schools, theaters, swimming pools, and even cemeteries (Kawasaki 1998; Massey and Denton, 1989a, 1989b). Latinos, particularly Mexican Americans in the Southwest, were subjected to lynching and violence in response to their movements to acquire political power and equal representation (Nelson and Lavariega Monforti, 2006).
Experiences of interpersonal racial discrimination have a prominent role in the racial and ethnic health disparities literature. Scholars have speculated as to the biological mechanisms by which experiences of interpersonal racism and discrimination might be translated into poorer health outcomes. Many studies reflect a general assumption that the stress response mechanism due to discrimination plays the major role (Williams 2009; Paradies 2006; Dressler et al., 2005; Krieger 1999; Flores et al., 2012). In addition, scholars have detailed other specific potential biological mechanisms including the “allostatic load,” or accumulated biological adversity over the life course (Geronimus 2005; Mays et al., 2007) and “epigenetics,” or the biologic changes in the proteins surrounding the genome that can affect how the genes are expressed and can be passed from one generation to another (Kuzawa 2009). Furthermore, Myers (2009) suggests numerous and interacting complex biological mechanisms by which psychological stressors of the lived experience of race are translated into physical health status. Similarly, Harrell et al. (2011) provide a detailed typology of the potential neuro-psycho-biological channels by which personal experiences with racism may impact health.
The commonality among these is that psychological stress associated with frequent experiences of interpersonal racism and discrimination are sufficient to produce physiological and biological changes observed as poorer health status. Although scholars have explored the relationship between African American experiences of interpersonal racial discrimination and health, there is relatively limited work exploring this relationship among Latinos (but see Finch et al., 2001 and Williams and Mohammed, 2009; Choi et al., 2013; Hicken et al., 2014; Kreiger et al., 2011; and Shippee et al., 2013.) For example, Choi et al. (2013) find that experiences of interpersonal racial discrimination are negatively correlated with self-reported health status among Latinos. In addition, Finch et al. (2001) found that when Mexican-Americans as a national origin group is isolated in their analysis, these respondents reported poorer self-rated health. These strands of research strongly suggest that interpersonal racial discrimination is not only a major component of the “lived experiences” of racial and ethnic minorities, but it also highly correlated with health outcomes.
Multi-Dimensionality of Race/Ethnicity
Studies by Campbell (2009), Saperstein (2006) and Telles and Lim (1998) have found that different approaches to measuring race do in fact portray different pictures of the extent of racial inequality. In varying degrees, depending on the context and the outcome under scrutiny, the nature of the relationship differs. For example, Saperstein (2006) used measures of observed and self-reported race in the General Social Survey and found that the different measures “yield substantively different results when used to explain income inequality in the United States.” In an educational context, Campbell (2009), using four measures of race-parent and self-report for self-identification and interviewer report of race and color, found that a number of educational outcomes are associated with the observed race measures for Latinos and single race groups but not for multiracial groups.
Our multiple measures incorporate skin color, ascribed race, and experiences of discrimination. Our interests lie in establishing the effects of different measures of race on health indicators so that research findings are more accurate and useful. For example, ascribed race might be best suited for studies of discrimination or access to goods and services, while self-reported race might be more useful for studies of attitudes and motivations (Burch and Loveman, 2011). Our effort builds upon other researchers’ efforts to “re-conceptualize” race in order to capture the “lived experiences” of race and the use of multi-dimensional measures.
We anticipate that we will find poorer self-reported health among Latinos who are of a darker skin color, who are identified as being Latino by others, and who report experiences of discrimination, even after controlling for a range of covariates (such as income, education, and access to health insurance). We refer to our primary theory as the Lived Experience Hypothesis. Our inquiry into re-conceptualizing race also includes the development of multi-dimensional measures of race and how they interact with each other to influence health outcomes as well as other outcomes. We test this theory through principle component analysis in which we scale the three measures in a two-dimensional space.
DATA AND METHODS
We take advantage of a 2011 Latino Decisions/impreMedia survey that was designed in collaboration with the Robert Wood Johnson Foundation (RWJF) Center for Health Policy at the University of New Mexico (UNM) for our analysis. Latino Decisions conducted the field work for the survey and worked in conjunction with the RWJF Center for Health Policy at UNM to design the survey instrument. This survey was therefore designed by a community of scholars with a strong background in the methodological issues in the quantitative study of race and ethnicity. The authors were able to create several measures utilized in our analysis with a specific focus on testing the relationship between race measured from a multidimensional perspective and self-reported health status. This is therefore an ideal data-set for our research question.
A total of 1,200 Latinos were interviewed over the phone through two samples: 600 Latino registered voters and 600 non-registered Latinos. The non-voter sample was added for the specific purpose of ensuring that our ability to explore the relationship between multiple measures of race and health included non-citizen Latinos, who are excluded from registered voter samples.
All phone calls were administered by Pacific Market Research in Renton, Washington. The survey has an overall margin of error of +/−4%, with an AAPOR response rate of 29%. Latino Decisions selected the 21 states with the highest number of Latino residents and that collectively account for 91% percent of the overall Latino adult population in the United States. The voter sample was drawn from registered voters using the official statewide databases of registered voters maintained by elections officials in each of the 21 states. A separate list of Hispanic households was used to identify respondents for the non-voter sample, which was designed to be proportionate to the overall population in those states. Probability sampling methods were employed in both samples based on the respective lists used to identify the universe of potential participants. Respondents were interviewed by telephone, and they could choose to be interviewed in either English or Spanish. A mix of cell phone only and landline households were included in the sample design, and both samples are weighted to match the 2010 Current Population Survey universe estimate of Latinos and Latino voters respectively for the 21 states with respect to age, place of birth, gender, and state. The survey was approximately 22 minutes long and was fielded from September 27, 2011 to October 9, 2011.
The primary outcome variable of interest is self-reported health status using a single health status question within the Latino Decisions dataset. The self-reported health status question included in the Latino Decisions survey is very close in wording to the item included in the Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System (BRFSS) for many years.vi Both questions utilize a 1 to 5 Likert scale, with respondents rating their health status from excellent to poor. The specific survey question we utilize is “How would you rate your overall physical health--excellent, very good, good, fair, or poor?” which is nearly identical to the CDC BRFSS question of “Would you say that in general your health is--excellent, very good, good, fair, or poor?”
Numerous studies have found the overall BRFSS questionnaire to produce reliable and valid resultsvii (Nelson et al., 2001). Self-reported health status, as measured by the CDC BRFSS, has been especially well studied in relation to mortality (Idler and Benyamini, 1997). Self-reported health status has also been found to be associated with a variety of health behaviors and health status indicators including physician-rated health status, smoking behavior, alcohol use, healthy eating, physical activity, healthy days, diabetes-related complications, and cardiovascular disease (Mossey and Shapiro, 1982; Tsai et al., 2010a, Tsai et al., 2010b; Zullig and Hendryx, 2010; Rubin and Peyrot, 1999).
A number of health scholars have recently identified challenges in using self-rated health status to examine variation in health across diverse racial/ethnic and immigrant populations. Bzostek et al. (2007) find large differences in the proportion of Hispanic immigrants, US-born Hispanics, and US-born Whites who report fair/poor health status in Los Angeles. Hispanic immigrants report the highest rates of fair/poor health status, even in the face of objective measures of better health. They further find evidence for language and acculturation differences in how the self-rated response categories are interpreted among Hispanics. Viruell-Fuentes et al. (2011) find evidence that Spanish-speaking Latino immigrants make use of the “fair” response option more frequently than other response options and more than English-speaking Latinos, even after controlling for covariates known to impact health. Similar non-English effects have been noted among foreign-born Asians (Kandula et al., 2007) and foreign-born Arabs (Abdulrahim and Baker, 2009) in the U.S. and among French-speaking Canadians (Layes et al., 2012).
While we acknowledge the limitations documented by these scholars in the use of the self-reported health status measure, we note that the primary recommendation among these studies is the use of caution when using self-rated health in comparing health status between racial/ethnic groups, or in measuring health disparities. We have noted the primary methodological recommendations of these scholars and have incorporated them into our study. First, in translating the “fair” response option category we follow the Viruell-Fuentes et al. (2011) recommendation of using “mas o menos” rather than the traditional “regular” translation. The original survey design included a split sample approach that randomly gave Spanish respondents (n=601) the “regular” response (n=302) and others the “mas o menos” response (n=299). Our analysis includes only the subset of Spanish respondents who were provided the “mas o menos” response option so that our analysis is consistent with other major studies using this measure. Secondly, we make use of two important control variables specific to immigrant experience: language and nativity (Bzostek et al., 2007; Abdulrahim and Baker, 2009). Given that our study is examining differences within the population of U.S. Hispanics, and having addressed the major methodological recommendations of scholars, we feel confident that our self-reported health is a viable measure to test our hypotheses.
Our explanatory variables are three measures of race/ethnicity that encompass our multi-dimensional approach to capturing race beyond self-identification. It is important to note that self-identification was utilized in our survey as a screener question to identify who was eligible for participation in the survey. The specific question is “The most frequently used terms to describe persons of Latin American descent living in the United States are ‘Hispanic’ and ‘Latino.’ Of the two, which do you prefer, Hispanic or Latino, or are you not of Hispanic or Latino origin?” Given that this is a sample specific to Latinos, we do not have any variation on this item, which does not allow us to include a “self-identification” variable in our models. However, this approach is consistent with our research question: are multi-dimensional approaches to measuring race beyond self-identification useful in research focused on outcomes such as health? The three measures beyond self-identification that we utilize in our analysis are self-reported skin color, ascribed race, and experiences with racial/ethnic discrimination.
We utilize the following question to measure skin color: “ We are interested in how you would describe your appearance. How would you describe your skin color with 1 being very light and 5 being very dark or somewhere in between?” The categories of the variable are very light, light, medium, dark, and very dark. We approach the concept of skin color in line with Gravlee et al. (2005), who contend that skin color may be a key cultural, not biological, variable of interest. Furthermore, we note that our approach of using self-reported skin color is consistent with the work of others (Klonoff and Landrine, 2000) who have found skin color to be correlated with health status. Our approach is different from those who have used reflectometers to assess skin color as more of a clinical measure and have found no association with health status (Araujo and Borrell, 2006; Gravlee et al., 2005; Krieger et al., 1998).
We utilize the following question to measure ascribed race: “ How do other people usually classify you in the United States? Would you say you are primarily viewed by others as…?” The response categories for this variable are Hispanic/Latino, Black/African American, White, American Indian/Native American, Mexican, and Some Other Group. We have coded this variable to create three mutually exclusive categories: Latino which is coded 0) all non-Latino, 1) defined as Latino; Mexican which is coded 0) all non-Mexican, 1) defined as Mexican and White which is coded 0) all non-White, 1) defined as White. These set of dummy variables represent the racial/ethnic categories into which most Latinos fall under the U.S. racial “classification” schema. In addition, the respondent’s perception of how others place him/her racially can be based on a number of determinants (i.e. national origin, phenotypical characteristics, accent, cultural practices, etc.).
Finally, our measure of discrimination experience utilizes the following survey question: “Have you personally experienced discrimination, or been treated unfairly because of your race or ethnicity?” The response categories for this measure are 0= No and 1= Yes. This measure is specific to racial/ethnic discrimination, making it ideal for our purposes here. This measure is also very similar to most identified in Paradies’ (2006) systematic review of the extant work focused on self-rated discrimination and health status. Summary statistics for all variables used in this analysis are listed in Table 1.
Table 1.
Summary Statistics
| Variables | N | Mean | SD | Min | Max |
|---|---|---|---|---|---|
| Self-Defined Health1 | 1150 | 3.098 | 1.175 | 1 | 5 |
| Discrimination | 1169 | 0.345 | --- | 0 | 1 |
| Skin Color2 | 1138 | 2.532 | 0.962 | 1 | 5 |
| Ascribed Mexican | 1082 | 0.389 | --- | 0 | 1 |
| Ascribed Latino | 1082 | 0.494 | --- | 0 | 1 |
| Ascribed White | 1082 | 0.117 | --- | 0 | 1 |
| L.E. Scale3 | 1017 | 3.871 | 2.126 | 1 | 8 |
| Education4 | 1150 | 3.471 | 1.547 | 1 | 6 |
| Age | 1121 | 51.623 | 17.182 | 18 | 98 |
| Income Missing | 1200 | 0.191 | --- | 0 | 1 |
| Inc. Less $40k | 1200 | 0.485 | --- | 0 | 1 |
| Inc. $40-$60 | 1200 | 0.130 | --- | 0 | 1 |
| Inc. $60-$80k | 1200 | 0.073 | --- | 0 | 1 |
| Inc. More $80k | 1200 | 0.122 | --- | 0 | 1 |
| Uninsured | 1132 | 0.212 | --- | 0 | 1 |
| Female | 1200 | 0.586 | --- | 0 | 1 |
| Nativity5 | 1200 | 0.431 | --- | 0 | 1 |
| Spanish Speaker6 | 895 | 0.334 | --- | 0 | 1 |
| Acculturation7 | 895 | 1.868 | 1.309 | 0 | 3 |
| Mexican Origin | 1200 | 0.528 | --- | 0 | 1 |
Health (1=Poor, 2=Fair, 3=Good, 4=Very Good, 5=Excellent)
Skin Color (1=Very Light, 2=Light, 3=Medium, 4=Dark, 5=Very Dark)
L.E. Scale is our lived experience scale which is outlined in Table 2.
Education (1=Grade 1–8, 2=Some HS, 3=HS, 4=Some College, 5=College Grad, 6=Post-Grad)
Nativity (0=Foreign Born, 1=U.S.-Born)
Spanish Interview (Only includes Spanish respondents who were given the “Mas o Menos” option)
Acculturation Scale (Combining Language and Nativity)
Our analytic approach is focused on the exploration of various techniques intended to determine if our measures of race/ethnicity provide a more clear depiction of the relationship between race and health outcomes among the Latino population than studies using more traditional measures. While our primary focus in this paper is to determine the impact that race, as measured from this multi-dimensional approach, has on the self-rated health of Latinos in the U.S., we are also concerned with how scholars interested in more developed approaches to measuring race should approach modeling. Therefore, we conduct a number of different analyses, including principle components analysis and various interaction specifications to provide a guide as to how to best measure race as a lived experience.
Our Race/Ethnicity as Lived Experienced Scale is intended to capture the lived experience of race for Latinos in a single “scaled” measure with the goal of parsimony and sensitivity to multi-dimensionality. Race is a highly complex concept, and consequently, our effort to account for this complexity within the approach of scaling was a challenge. From a theoretical perspective, identifying the minimum and maximum values of the scale was straightforward; at the low-end of the scale are Latinos who report the lightest skin color, reported no discrimination, and who are viewed by others as White. Conversely, the high category includes dark –skinned Latinos who have experienced discrimination and who report being viewed by others as non-White.
Establishing the categories in the middle as well as assigning those who are ascribed as “Mexican” on the scale proved to be more challenging, as this required us to determine where some respondents, those who, for example, reported dark skin but who did not experience discrimination, would fall along the scale relative to light skinned Latinos who have experienced discrimination. Due to the lack of theory in this area, and for simplicity, we combined ascribed Mexican and ascribed Latino respondents. This parsimonious approach allows us to observe how being ascribed White compares to all other Latino/Hispanic categories. Among these two factors, we approached the scale from the standpoint that skin color was the more dominant dimension of race due to skin color a) being identified in the literature as a predictor of health outcomes, and more importantly (and as discussed below), b) skin color is conceived as the antecedent to both ascribed race and discrimination experiences. The Race/Ethnicity as Lived Experience Scale is presented in Table 2.
Table 2.
Race as Lived Experienced Scale
| Coded | Skin Color | Ascribed Race | Discrimination | Frequency | Percent |
|---|---|---|---|---|---|
| 1 | Very Light, Light, & Medium | White | No | 85 | 8.36 |
| 2 | Very Light & Light | Mexican/Latino | No | 244 | 23.99 |
| 3 | Medium | Mexican/Latino | No | 290 | 28.52 |
| 4 | Dark & Very Dark | Mexican/Latino | No | 51 | 5.01 |
| 5 | Very Light & Light & Medium | White | Yes | 34 | 3.34 |
| 6 | Very Light & Light | Mexican/Latino | Yes | 112 | 11.01 |
| 7 | Medium | Mexican/Latino | Yes | 160 | 15.73 |
| 8 | Dark & Very Dark | Mexican/Latino | Yes | 41 | 4.03 |
Finally, we control for a handful of measures that have been found to be correlated with Latino health status in previous research. The inclusion of these factors is intended to provide clarity as to whether or not the relationship of interest in our analysis, a multidimensional approach to race and health status, holds when other factors known to influence Latino health are accounted for in the model. Among the demographic variables we include standard measures of income, educational attainment, age, and gender. The impact of socio-economic status on Latino health outcomes is well established in the literature (Alder et al., 1994; Braveman et al., 2005; Marmot 2006). To assess income we have included several dummy variables representing different income categories: $40,000-$60,000, $60,000-$80,000, and >$80,000, with less than $40,000 serving as the reference category. We also include a variable of “unknown” income in the model which includes respondents who did not report their income as a means of saving cases. We also include a measure for whether respondents currently have health insurance, as we expect uninsured Latinos to have poorer self-rated health based on the findings from previous work exploring this relationship (CDC 2011; Carrillo et al., 2011). Finally, we control for several Latino-specific factors, including nativity, language of survey, and national origin.
Research has documented that more acculturated Latinos, again, often measured by language, nativity, and length of stay, receive higher rates of preventive services, encounter fewer barriers in obtaining care, and are more likely to have health coverage (Gamboa and Kahramanian, 2005; Wells et al., 1989). However, scholars utilizing self-rated health as their dependent variable have found that foreign-born Latinos are more likely to report better self-reported health than their U.S.-born counterparts (Massey et al., 2004; Finch et al., 2002). This debate in the literature motivates our inclusion of measures of acculturation. For the purposes of this study we construct a scaled acculturation variable incorporating both nativity and language of survey into a single measure, as these two measures are highly correlated and inclusion of both separately may lead to issues with multicollinearity. Acculturation is a scale from 0–3, with 0 representing the least acculturated (non-U.S.-born and Spanish survey administration); 1=U.S.-born and Spanish survey, 2= non-U.S.-born and English survey, 3=U.S.-born and English survey) based on the following two questions: “Do you prefer that we speak in English or Spanish?” and “Were you born in the United States, on the island of Puerto Rico, or in another country?” Puerto Ricans are counted in our acculturation variable as U.S.-born if they were born in the U.S. and foreign born if they reported being born outside the U.S. We also include a measure for whether respondents are of Mexican origin, as this population has been found to have unique health outcomes relative to Latinos from other backgrounds (CDC 2011; Mulvaney-Day et al., 2007; Zsembil and Fennell, 2005).
RESULTS
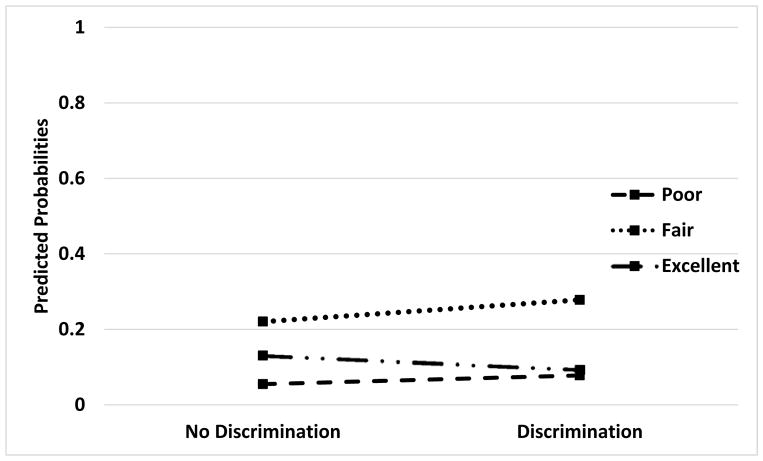
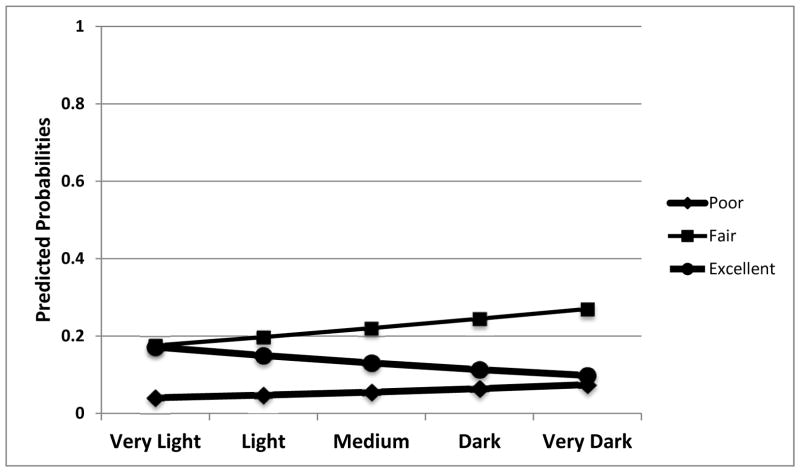
We begin our results with a discussion of our ordered-logistic model, which is intended to test the Lived Experience Hypothesis. Our multi-dimensional measures of race are negatively correlated with self-rated health among Latinos. The results of this model are depicted in Table 3. We find strong support for our primary hypothesis, as both discrimination and skin color are significantly and negatively associated with self-rated health status, indicating that Latinos who have faced discrimination and who have dark skin color report worse health status than Latinos who are lighter and who have not faced discrimination in the past year. To assess the substantive impact of these two variables on self-rated health, we also computed and plotted predicted probabilities for both skin color and discrimination (see Figures 2 and 3), allowing the values of these two variables to vary while holding the control variables at their means, medians, or modes. As we see in Figures 2 and 3, both skin color and discrimination have a marked substantive effect on Latino health, with the likelihood of reporting “excellent” health being 17.14 percent for very light skinned Latinos compared to 9.80 percent for very dark skinned Latinos. This represents a 7.34 percentage point decrease in reporting “excellent” self-rated health as one moves from light to dark skin.
Table 3.
Ordered Logistic Regression Coefficients for Measures of Race as Lived Experienced on Latino Self-Rated Health
| Explanatory Variable | Coefficient | Standard Error | Odds Ratio |
|---|---|---|---|
| Measures of Race: | |||
| Experienced Discrimination | −0.375*** | 0.145 | 0.687*** |
| Skin Color (Light to Dark) | −0.161** | 0.074 | 0.851** |
| Viewed as White by Others (Reference Category) | |||
| Viewed as Latino by Others | −0.234 | 0.218 | 0.792 |
| Viewed as Mexican by Others | 0.375 | 0.242 | 1.455 |
| Socio-Demographic Factors: | |||
| Education | 0.242*** | −0.057 | 1.274*** |
| Income < $40K (Reference Category) | |||
| Income ($40-$60K) | 0.038 | 0.21 | 1.039 |
| Income ($60-$80K) | 0.193 | 0.249 | 1.212 |
| Income (>$80K) | 0.485** | 0.22 | 1.625** |
| Income Unspecified/Unknown | 0.178 | 0.211 | 1.194 |
| Age | −0.022*** | 0.004 | 0.979*** |
| Currently Uninsured | −0.818*** | 0.183 | 0.441*** |
| Female | −0.192 | 0.142 | 0.825 |
| Cultural Factors: | |||
| Acculturation | 0.080 | 0.059 | 1.084 |
| National Origin (Mexican) | −0.286* | 0.155 | 0.751* |
Source: Latino Decisions/UNM RWJF Survey
N =700 Pseudo R2 = .059
≤.01
p≤.05
p≤.001
Figure 2.
The Substantive Impact of Discrimination on Health Status
Note: Controlling for Skin Color, Ascribed Race Categories, Age, Education, Income, Gender, Health Insurance, Nativity, Language of Interview, and Mexican Origin.
Figure 3.
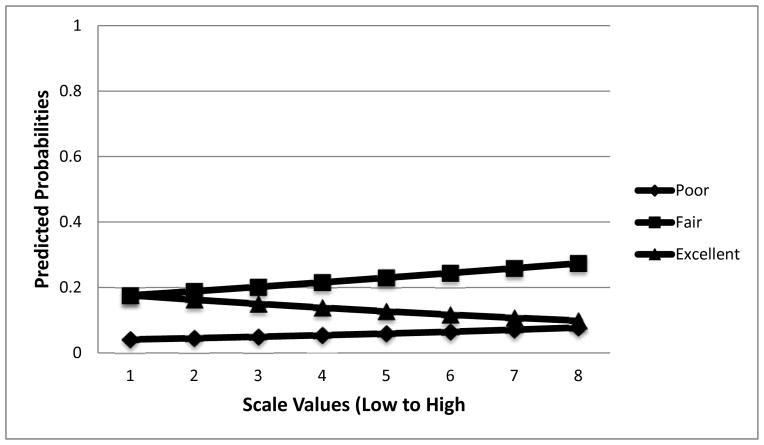
The Substantive Impact of Race as Lived Experience Scale on Health Status
Note: Controlling for Age, Education, Income, Gender, Health Insurance, Nativity, Language of Interview, and Mexican Origin.
Similarly, Latinos who have not reported experiences of discrimination have a greater likelihood of reporting “excellent” health (13.04 percent) when compared to those who do report experiences of discrimination (9.34 percent). We also find a reasonable substantive impact of both skin tone and discrimination on the probability of individuals reporting fair health status when compared to poor health. For instance, as one moves from light to dark skin there is a 9.43 percent increase in the likelihood of reporting fair health, and as one moves from no experiences of discrimination to experiences of discrimination we find an increase in the likelihood of reporting fair health.
Although ascribed race is not statistically significant when other race variables are included, the results from the first stage of our analysis strongly suggest that Latinos who have a lived experience in which race and ethnicity has a marked impact on their daily lives have worse health than those with a different lived experience where race/ethnicity is not as prominent. That said, our model suggests that, when juxtaposed with discrimination and skin color, being viewed as Latino or “Mexican” (relative to White) does not have a significant impact on self-rated health. Moreover, the results of the principle components analysis and bi-plots reveal that ascribed race and skin color are highly correlated constructs that are orthogonal with experiences of discrimination. In other words, among these three constructs, skin color and ascribed race cluster and are more closely aligned compared to experienced discrimination.
In addition to our multi-dimensional measures of race, we will briefly discuss the performance of the control variables as well. The socio-demographic factors are very meaningful, as essentially all of these controls have an impact on Latino self-rated health status. In line with the extant literature on the relationship between education and income broadly (Marmot 2006; Marmot and Wilkinson, 1999), both education and income are positively correlated with self-rated health among Latinos. However, we find that while Latinos who make more than $80,000 a year (relative to Latinos who make less than $40,000 a year) report better health, Latinos in the middle category of $60,000-$80,000 and Latinos who make between $40,000 and $60,00 are not statistically different from Latinos in the low-income category. Furthermore, and also consistent with previous research, age and not having health insurance are significantly and negatively correlated with self-rated health status. Finally, we do not find evidence that Latinas report poorer health status than Latino males after controlling for other factors. Among cultural factors, we find that Latinos who are more acculturated are no different than less acculturated Latinos. Lastly, we find that respondents of Mexican origin report worse health than non-Mexican origin Latinos, a finding that is marginally significant at the 0.10 level. The fact that our control variables are in line with the extant literature lends some confidence in the results of our race measures.
To further explore our multi-dimensional approach to measuring race, the next steps in our analysis include the specification of an interaction between skin color and discrimination. These two variables were found to be significantly correlated with self-rated health in the previous model. Now we explore whether these two specific aspects of race as an individual’s lived experience, which interacts Latinos who are darker skin and experienced discrimination, result in worse self-rated health reports than Latinos with iterations that are less “extreme.” The results from this model (not reported in this paper), however, reveal that the interaction term is not statistically correlated with Latino self-rated health. We therefore do not find evidence that these two measures of race have an interactive impact on Latino health status.
The final and arguably most ambitious component of our analysis is to test the association of a scale combining our three dimensions of race as lived experience of individuals with Latino self-rated health. Our scale ranges from a low value of Latinos with light skin tone who did not report discrimination and who are viewed as others as being White to a high value of Latinos with dark skin who did report discrimination and who are viewed by others as being Mexican or Latino. In short, this scale represents our approach to capture the effect race and ethnicity have on the lives of Latinos in the U. S. and how these lived experiences influence the health status of this population. As shown in Table 4, and in line with our Lived Experience Hypothesis, the race scale is significant and negatively correlated with Latino self-rated health. This relationship holds even when we control for other factors known to influence health outcomes, including having health insurance. Consequently, we find that when all three dimensions of race are combined in a scale, Latinos whose daily lives are more directly influenced by their race/ethnicity report poorer health than Latinos for whom race is not a central factor. As shown in Figure 3, the substantive impact of the race scale indicates that the lived experiences associated with race have meaningful implications for the reported health status of Latinos. More specifically, we see in Figure 3 that as Latinos move along the scale from the minimum to maximum value, the likelihood of reporting “excellent” health decreases from 17.6 percent to 9.86 percent, a 7.74 percentage point decrease. We conclude that the experiences associated with being a racial/ethnic minority in the U. S. do have significant consequences for the self-rated health of Latinos.
Table 4.
Ordered Logistic Regression Coefficients for the Lived Experienced Scale on Latino Self-Rated Health
| Explanatory Variable | Coefficient | Standard Error | Odds Ratio |
|---|---|---|---|
| Measures of Race: | |||
| LES Scale | −0.096*** | 0.032 | 0.909*** |
| Socio-Demographic Factors: | |||
| Education | 0.224*** | 0.056 | 1.251*** |
| Income < $40K (Reference Category) | |||
| Income ($40-$60K) | 0.006 | 0.209 | 1.006 |
| Income ($60-$80K) | 0.125 | 0.247 | 1.133 |
| Income (>$80K) | 0.454** | 0.22 | 1.574** |
| Income Unspecified/Unknown | 0.214 | 0.21 | 1.238 |
| Age | −0.021*** | 0.004 | 0.979*** |
| Currently Uninsured | −0.758*** | 0.183 | 0.469*** |
| Female | −0.209 | 0.141 | 0.811 |
| Cultural Factors: | |||
| Acculturation | 0.081 | 0.058 | 1.085 |
| National Origin (Mexican) | −0.068 | 0.14 | 0.934 |
Source: Latino Decisions/UNM RWJF Survey
N = 700 Pseudo R2 = .053
<.01
p≤.05
p≤.001
The performance of the control variables, for the most part, portrays a similar story to that described for the base model where each measure of race was specified independently. For example, younger Latinos and those with higher education levels report better health than their older and less educated counterparts. Furthermore, Latinos who lack health insurance report worse health than those who are currently insured. We note that the impact of combining our three dimensions of race into a scale generally has little impact on how the other variables in our model influence Latino self-rated health.
CONCLUSIONS AND DISCUSSION
As our nation continues to become more racially and ethnically diverse, understanding the ways in which the lives of individuals in society vary by race and ethnicity becomes more critical. We advocate for approaching the task of measuring race and ethnicity from the standpoint of capturing the lived experiences of individuals. This requires moving beyond single measures of race and/or ethnicity which are usually constructed through self-identification. We have suggested three specific measures relevant to the race and health literature that have the potential to move us in this direction: skin color, ascribed race, and discrimination experiences. By exploring the relationships between these concepts and self-reported health status, we are able to determine whether or not this multi-dimensional measurement strategy yields any significant results beyond what we might find if we relied on a single measure of race/ethnicity.
Our analysis reveals that, among these three factors, both skin color and discrimination experiences are significantly and negatively correlated with Latino self-rated health status. Therefore, Latinos who have darker skin color and who have faced discrimination in their daily lives have poorer self-rated health compared to Latinos who are of lighter skin color and who do not report any experiences with discrimination. Furthermore, when combined into a scale with ascribed race, we find that Latinos with a lived experience that includes being discriminated against, having darker skin, and being viewed as being non-White by others have poorer health than those on the other extreme of the scale. This represents solid evidence for our Lived Experience Hypothesis.
While promising at this early stage of development, we acknowledge that there are a number of unsettled issues with our analysis. Most prominently, we must conduct the path analysis component of our analysis to help determine the process by which these measures influence self-rated health status. We anticipate finding that skin color is the dominant factor which both directly and indirectly impacts health by driving ascribed race and experiences with discrimination. However, we need to test whether our theory that phenotype, in this case skin color, provides the context for the various lived experiences within racial and ethnic communities. The results from this final stage of our analysis can help improve our scaling efforts and potentially advance the theoretical foundation driving many research questions within racial and ethnic politics. Research in this area should consider protective factors such as marital status on the self-reported health of Latinos, an inquiry we could not explore due to the absence of this measure in the dataset.
Finally, although our primary focus in this paper has been to determine if these alternative measures to race and ethnicity impact the self-reported health status of Latinos, there are many other applications for this approach to the measurement of outcomes in communities of color. Scholars may gain new insights into a range of health, illness, social, and political outcomes in communities of color by applying this multidimensional measurement strategy. For example, the lived experience scale that we have developed in this analysis could be applied to the group identity of Latinos as well as socio-economic status. Helping advance a fuller notion of “race” through a novel measurement approach has benefits to a wide range of scholars. As the nation continues to respond to a diversification of its population, scholars will need to re-think approaches to measuring race and ethnicity. With internal variation within groups becoming just as important as differences across them, our study provides an innovative measurement strategy for others to follow. We hope that this will spark a movement away from binary measures of race and ethnicity with the goal of improving our ability to tackle disparities in health and other outcomes.
Figure 1.
The Substantive Impact of Skin Color on Health Status
Note: Controlling for Discrimination, Ascribed Race Categories, Age, Education, Income, Gender, Health Insurance, Nativity, Language of Interview, and Mexican Origin
Footnotes
Names are listed alphabetically and do not reflect contributions made to the project
While skin color (in terms of darker vs. lighter skin tones) dominates the analytical attention, and is our focus here, it is important to note that other traits such as indigenous vs. “European” features, shape of eyes and the elliptical fold, hair texture, and skin bleaching represent different phenotypic markers that may be associated with race.
The inter-relationship between skin color and ascribed race not only reinforces our notions about the complexity of race, but also the measurement challenges of constructing multi-dimensional indicators.
Assessed by the question “How do other people usually classify you in this country?” (Jones et al., 2008)
We acknowledge that some studies have sought to move to a more direct measurement of racial subordination as power relations or institutional racism (see Gee and Ford (2011) and Harrell, et al. (2010). That is, to tap into the view that the underlying basis for the existence of racial categories lies with power, control, status, access, and inequities. While beyond the scope of this project, we support the work of those interested in measuring these dimensions.
Per CDC BRFSS Operational and User’s Guide Version 3.0, BRFSS surveys are conducted via computer-assisted telephone interviewing at the state level, with data submitted to CDC where they are compiled and analyzed.
Contributor Information
John A. Garcia, Inter-University Consortium for Political and Social Research, University of Michigan.
Gabriel R. Sanchez, Department of Political Science and RWJF Center for Health Policy, University of New Mexico
Shannon Sanchez-Youngman, Department of Political Science and RWJF Center for Health Policy, University of New Mexico.
Edward D. Vargas, Center for Women’s Health and Health Disparities Research, University of Wisconsin-Madison
Vickie D. Ybarra, Department of Political Science and RWJF Center for Health Policy, University of New Mexico
WORKS CITED
- Ahmed Ameena, Mohammed Selena, Williams David R. Racial discrimination & health: Pathways & Evidence. Indian Journal of Medical Research. 2007;126:318–327. [PubMed] [Google Scholar]
- Abdulrahim Sawsan, Baker Wayne. Differences in Self-Rated Health by Immigrant Status and Language Preference among Arab Americans in the Detroit Metropolitan Area. Social Science & Medicine. 2009;68:2097–2013. doi: 10.1016/j.socscimed.2009.04.017. [DOI] [PubMed] [Google Scholar]
- Alder Nancy, Boyce Thomas, Chesney Margaret, Cohen Sheldon, Folkman Susan, Kahn Robert, Sym Leonard. Socioeconomic Status and Health: The challenge of the Gradient. American Psychologist. 1994;49(1):15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- Alegria Margarita, Mulvaney-Day Norah, Canino Glorisa. Prevalence of Psychiatric Disorders across Latino Subgroups in the United States. American Journal of Public Health. 2007;97(1):68–71. doi: 10.2105/AJPH.2006.087205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araújo B, Borrell LN. Understanding the Link between Discrimination, Life Chances and Mental Health Outcomes among Latinos. Hispanic Journal of Behavioral Sciences. 2006;28:245–266. [Google Scholar]
- Benhabib Seyla. The Claims of Culture: Equality and Diversity in the Global Era. Princeton, NJ: Princeton University Press; 2002. [Google Scholar]
- Bernal M, Knight G, editors. Ethnic identity: Formation and transmission among Hispanics and other Minorities. Albany, NY: State University of New York Press; 1993. [Google Scholar]
- Bowman Phillip J, Muhammad Ray, Ifatunji Mosi. Skin Tone, Class and Racial Attitudes among African-Americans. In: Herring Cedric., editor. Skin Deep: How Race and Complexions Matter in the ‘Color-Blind’ Era. Chicago: University of Illinois Press; 2004. pp. 128–158. [Google Scholar]
- Boyle Edwin. Biological Patterns in Hypertension by Race, Sex, Body Weight, and Skin Color. JAMA. 1970;213(10):1637–1643. [PubMed] [Google Scholar]
- Braveman Paula, Cubbin Catherine, Egerter Susan, Chldeya Sekai, Kristen Marchi, Metzler Marilyn, Posner Samuel. Socioeconomic Status in Health Research: One Size Does not Fit All. JAMA. 2005;294(22):2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- Browne Irene, Odem Mary. Juan Crow in the Nuevo South? Racialization of Guatemalan and Dominican Immigrants in the Atlanta Metro Area. Du Bois Review: Social Science Research on Race. 2012;9(2):321–337. [Google Scholar]
- Bruch Sarah, Loveman Mara. Measuring and Modeling Race as a Multi-Dimensional Construct: Evidence from Research on Racial Disparities in Education. Paper presented at the Population Association of America annual meeting; April; Washington D.C. 2011. [Google Scholar]
- Bzostek Sharon, Goldman Noreen, Pebley Anne. Why do Hispanics in the USA Report Poor Health? Social Science & Medicine. 2007;65:990–1003. doi: 10.1016/j.socscimed.2007.04.028. [DOI] [PubMed] [Google Scholar]
- Campbell Mary E. Multiracial Groups and Educational Inequality: A Rainbow or a Divide? Social Problems. 2009;56(3):425–446. [Google Scholar]
- Carillo J Emilio, Carillo Victor, Perez Hector, Sala-Lopez Debbie, Natale-Pereira Ana, Byron Alex. Defining and Targeting Health Care Access. Journal of Health Care for the Poor and Underserved. 2011;22:562–575. doi: 10.1353/hpu.2011.0037. [DOI] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention. CDC Health Disparities and Inequalities Report-United States, 2011 in. Morbidity and Mortality Weekly Report. 2011;(Supplement 60):1–116. [Google Scholar]
- Chae David H, Nuru-Jeter Amani M, Lincoln Karen D, Francis Darlene D. Conceptualizing Racial Disparities in Health Advancement of a Socio-Psychobiological Approach. Du Bois Review: Social Science Research on Race. 2011;8(1):63–77. [Google Scholar]
- Chan Joanna, Ehrlich Allison, Lawrence Reva, Moshell Alan, Turner Maria, Kimball Alexa. Assessing the Role of Race in Quantitative Measures of Skin Pigmentation and Clinical Assessments of Photosensitivity. Journal of American Academy of Dermatology. 2005;52(4):609–615. doi: 10.1016/j.jaad.2004.03.051. [DOI] [PubMed] [Google Scholar]
- Choi Kyung-Hee, Paul Jay, Ayala George, Boylan Ross, Gregorich Steven E. Experiences of Discrimination and Their Impact on the Mental Health Among African American, Asian and Pacific Islander, and Latino Men Who Have Sex With Men. American Journal of Public Health. 2013;103(5):868–874. doi: 10.2105/AJPH.2012.301052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobas José A, Duany Jorge, Feagin Joe R. How the United States Racializes Latinos: White Hegemony and Its Consequences. Boulder: Paradigm Publishers; 2009. [Google Scholar]
- Cohen Cathy. The Boundaries of Blackness: AIDS and the Breakdown of Black Politics. Chicago: Chicago University Press; 1999. [Google Scholar]
- Curtin Philip D. The Slavery Hypothesis for Hypertension among African Americans: The Historical Evidence. American Journal of Public Health. 1992;82:1681–1686. doi: 10.2105/ajph.82.12.1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson Michael C. Behind the Mule: Race, Class and African American Politics. Princeton, NJ: Princeton University Press; 1995. [Google Scholar]
- De Genova Nicholas. The Legal Production of Mexican/Migrant ‘Illegality.’. Latino Studies. 2004;2(2):160–185. [Google Scholar]
- Dressler William W, Oths Kathryn S, Gravlee Clarence C. Race and Ethnicity in Public Health Research: Models to Explain Health Disparities. Annual Review of Anthropology. 2005;34:231–352. [Google Scholar]
- Espino Rodolfo, Franz Michael M. Latino Phenotypic Discrimination Revisited: The Impact of Skin Color on Occupational Prestige. Social Science Quarterly. 2002;83:612–623. [Google Scholar]
- Finch BK, Hummer RA, Kol B, Vega WA. The Role of Discrimination and Acculturative stress in the Physical Health of Mexican-Origin Adults. Hispanic Journal of Behavioral Sciences. 2001;23(4):399–429. [Google Scholar]
- Flores Elena, Tschann Jeanne M, Dimas Juanita M, Bachen Elizabeth A, Pasch Lauri A, de Groat Cynthia L. Perceived Discrimination, Perceived Stress, and Mental and Physical Health among Mexican-Origin Adults. Hispanic Journal of Behavioral Sciences. 2008;30(4):401–424. [Google Scholar]
- Flores Rene, Telles Edward. Social Stratification in Mexico: Disentangling Color, Ethnicity, and Class. American Sociological Review. 2012;77:486–494. doi: 10.1177/0003122412444720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford Marvella E, Adam Kelly P. Conceptualizing and Categorizing Race and Ethnicity in Health Services Research. Health Services Research. 2005;40(5):1658–1675. doi: 10.1111/j.1475-6773.2005.00449.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford C, Airhihenbuwa C. The Public Health Critical Race Methodology: Praxis for Antiracism Research. Social Science & Medicine. 2010;71:1390–1398. doi: 10.1016/j.socscimed.2010.07.030. [DOI] [PubMed] [Google Scholar]
- Frank Reanne, Akresh Ilana Redstone, Lu Bo. Latino Immigrants and the U.S. Racial Order: How and Where Do They Fit In? American Sociological Review. 2010;75:378–401. [Google Scholar]
- Garcia Ignacio M. White But Not Equal: Mexican Americans, Jury Discrimination, and the Supreme Court. Tucson: University of Arizona Press; 2008. [Google Scholar]
- Garcia John A. Report on the Latino National Political Survey and Construction of Race (Skin color) and Cultural Items. 1991. [Google Scholar]
- Garcia John A. Toward a Holistic Conceptualization and Operationalization of Race and Health Disparities. In: Gomez Laura E, Lopez Nancy., editors. Mapping ‘Race’: Critical Approaches to Health Disparities Research. New Brunswick, NJ: Rutgers University Press; 2013. pp. 188–209. [Google Scholar]
- Gardner LI, Jr, Stern MP, Haffner SM, Gaskill SP, Hazuda HP, Relethford JH, Eifler CW. Prevalence of Diabetes in Mexican Americans. Diabetes. 1984;33:86–92. doi: 10.2337/diab.33.1.86. [DOI] [PubMed] [Google Scholar]
- Gee Gilbert C, Ford Chandra L. Structural Racism and Health Inequities: Old Issues, New Directions. Du Bois Review. 2011;8(1):115–132. doi: 10.1017/S1742058X11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J. ‘Weathering’ and Age–Patterns of Allostatic Load Scores among Blacks and Whites in the United States. American Journal of Public Health. 2006;96(5):826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomberg-Munoz Ruth. Inequality in a Post-racial Era: Race, Immigration, and Criminalization of Low-Wage Labor. Du Bois Review: Social Science Research on Race. 2012;9(2):339–353. [Google Scholar]
- Gómez Christina. The Continual Significance of Skin Color: An Exploratory Study of Latinos in the Northeast. Hispanic Journal of Behavioral Sciences. 2000;22:94. [Google Scholar]
- Gravlee Clarence C, Dressler William W, Russell Bernard H. Skin Color, Social Classification, and Blood Pressure in Southeastern Puerto Rico. American Journal of Public Health. 2005;95(12):2191–2197. doi: 10.2105/AJPH.2005.065615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravlee Clarence. Operationalizing Race in Health Research: From Mantra to Measurement. In: Gomez Laura E, Lopez Nancy., editors. Mapping ‘Race’: Critical Approaches to Health Disparities Research. New Brunswick, NJ: Rutgers University Press; 2013. [Google Scholar]
- Grosofoguel Ramon. Race and Ethnicity as Racialized Ethnicities? Identities within Global Coloniality. Ethnicities. 2004;4(3):315–336. [Google Scholar]
- Harburg E, Gleiberman L, Roeper P, Schork MA, Schull WJ. Skin Color, Ethnicity, and Blood Pressure I: Detroit Blacks. American Journal of Public Health. 1978;68:1177–1183. doi: 10.2105/ajph.68.12.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell Camara Jules P, Burford Tanisha I, Cage Brandi N, Nelson Travette McNair, Shearon Sheronda, Thompson Adrian, Green Steven. Multiple Pathways Linking Racism to Health Outcomes. Du Bois Review. 2011;8(1):143–157. doi: 10.1017/S1742058X11000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris David, Sim Jeremiah. Who is Multi-Racial? Assessing the Complexity of Lived Race. American Sociological Review. 2002;67(4):614–627. [Google Scholar]
- Helms JE. The Measurement of Black Racial Identity Attitudes. In: Helms JE, editor. Black and White Racial Identity: Theory, Research, and Practice. Westport, CT: Greenwood Press; 1990. pp. 33–48. [Google Scholar]
- Hersch Joni. Discussion Paper No. 545. Harvard Law School; Cambridge, MA 02138: 2006. Skin Tone Effects among African Americans: Perceptions and Reality. [Google Scholar]
- Hicken Margaret T, Lee Hedwig, Morenoff Jeffrey, House James S, Williams David R. Racial/Ethnic Disparities in Hypertension Prevalence: Reconsidering the Role of Chronic Stress. American Journal of Public Health. 2014;104(1):117–123. doi: 10.2105/AJPH.2013.301395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill Mark. Race of the Interviewer and Perception of Skin Color: Evidence from the Multi-City Study of Urban Inequality. American Sociological Review. 2002;66(1):99–108. [Google Scholar]
- Hochschild Jennifer. Including Oneself and Including Others: Who Belongs in My Country? The Annals of the American Academy of Political and Social Science. 2011;634:78–97. [Google Scholar]
- Hochschild Jennifer L, Weaver Vesla M, Burch Traci. Destabilizing the American Racial Order. Dædalus, the Journal of the American Academy of Arts & Sciences. 2011;140(2):151–165. [Google Scholar]
- Hogg MA, Terry DJ. Social Identity Processes in Organizational Contexts. London: Psychology Press; 2002. [Google Scholar]
- Idler EL, Benyamini Y. Self-rated Health and Mortality: A Review of Twenty-Seven Community Studies. Journal of Health and Social Behavior. 1997;38(1):21–37. [PubMed] [Google Scholar]
- James Cara, Thomas Megan, Lillie-Blanton Marsha, Garfield Rachel. Project Report. The Kaiser Family Foundation; Menlo Park, CA: 2007. Key Facts: Race, Ethnicity & Medical Care. [Google Scholar]
- Jones Camara, Truman BI, Elam-Evans LD, Jones CA, Jones CY, Jiles R, Rumisha SF, Perry GS. Using Socially Assigned Race to Probe White Advantages in Health Status. Ethnicity and Disease. 2008;18(4) Supplement:1–12. [PubMed] [Google Scholar]
- Kamasaki Charles. The Fair Housing Index: An Audit of Race and National Origin Discrimination in the Greater Washington Mortgage Lending Marketplace. Washington, DC: 1998. [Google Scholar]
- Kandula Manratha R, Lauderdale Diane S, Baker David W. Differences in Self-Reported Health among Asians, Latinos, and Non-Hispanic Whites: The Role of Language and Nativity. Annals of Epidemiology. 2007;17:191–198. doi: 10.1016/j.annepidem.2006.10.005. [DOI] [PubMed] [Google Scholar]
- Keil JE, Tyroler HA, Sandifer SH, Boyle E., Jr Hypertension: Effects of Social Class and Racial Admixture: The results of a Cohort Study of the Black Population of Charleston, South Carolina. American Journal of Public Health. 1977;67:634–639. doi: 10.2105/ajph.67.7.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keith VM, Herring C. Skin Tone and Stratification in the Black Community. American Journal of Sociology. 1991;97(3):760–778. [Google Scholar]
- Klag MJ, Whelton PK, Coresh J, Grim CE, Kuller LH. The Association of Skin Color with Blood Pressure in U.S. Blacks with Low Socioeconomic Status. JAMA. 1991;265:599–602. [PubMed] [Google Scholar]
- Klonoff Elizabeth A, Landrine Hope. Is Skin Color a Marker for Racial Discrimination? Explaining the Skin Color–Hypertension Relationship. Journal of Behavioral Medicine. 2000;23(4):329–338. doi: 10.1023/a:1005580300128. [DOI] [PubMed] [Google Scholar]
- Knapp RG, Keil JE, Sutherland SE, Rust PF, Hames C, Tyroler HA. Skin Color and Cancer Mortality among Black Men in the Charleston Heart Study. Clinical Genetics. 1995;47(4):200–206. doi: 10.1111/j.1399-0004.1995.tb03959.x. [DOI] [PubMed] [Google Scholar]
- Krieger N, Sidney S, Coakley E. Racial Discrimination and Skin Color in the CARDIA Study: Implications for Public Health Research. American Journal of Public Health. 1998;88:1308–1313. doi: 10.2105/ajph.88.9.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger Nancy. Embodying Inequality: A Review of Concepts, Measures, and Methods for Studying Health Consequences of Discrimination. International Journal of Health Services. 1999;29(2):295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- Kuzawa CW, Sweet E. Epigenetics and the Embodiment of Race: Developmental Origins of US Racial Disparities in Cardiovascular Health. American Journal of Human Biology. 2009;21(1):2–15. doi: 10.1002/ajhb.20822. [DOI] [PubMed] [Google Scholar]
- LaVeist Thomas. Beyond dummy Variables and Sample Selection: What Health Service Researchers Ought to Know about Race as a Variable. HSR: Health Services Research. 1994;29(1):1–16. [PMC free article] [PubMed] [Google Scholar]
- Layes Audrey, Asada Yukiko, Kephart George. Whiners and Deniers – What Does Self-Rated Health Measure? Social Science and Medicine. 2012;75(1):1–9. doi: 10.1016/j.socscimed.2011.10.030. [DOI] [PubMed] [Google Scholar]
- Lin SS, Kelsey JL. Use of Race and Ethnicity in Epidemiologic Research: Concepts, Methodological Issues, and Suggestions for Research. Epidemiologic Review. 2000;22(2):187–202. doi: 10.1093/oxfordjournals.epirev.a018032. [DOI] [PubMed] [Google Scholar]
- Lopez Nancy, Gomez Laura., editors. Mapping Race: Critical Approaches to Health Disparities Research. New Brunswick, NJ: Rutgers University Press; 2013. [Google Scholar]
- Marmot Michael. Status Syndrome—A Challenge to Medicine. BMJ (Clinical Research Ed) 2006;295(17):1304–1307. doi: 10.1001/jama.295.11.1304. [DOI] [PubMed] [Google Scholar]
- Martinez Jacqueline M. Learning to See What I was Never Supposed to See: Becoming Chicana in a White World. In: Martin JN, Nakayama TK, Flores LA, editors. Readings in Cultural Contexts. 2. Houston: Mayfield Publishing Company; 2002. pp. 67–73. [Google Scholar]
- Massey Douglas, Denton NA. Residential Segregation of Mexicans, Puerto Ricans, and Cubans in U.S. Metropolitan Areas. Sociology and Social Research. 1989;73:73–83. [Google Scholar]
- Massey Douglas, Denton NA. Racial Identity among Caribbean Hispanics: The Effect of Double Minority Status on Residential Segregation. American Sociological Review. 1989;54:790–808. [Google Scholar]
- Massey Doug, Durand Jorge, Malone Nolan J. Beyond Smoke and Mirrors: Mexican Immigration in an Era of Economic Integration. New York: Russell Sage Foundation; 2003. [Google Scholar]
- Massey Doug. Segregation and Stratification: A Biosocial Perspective. Du Bois Review: Social Science Research on Race. 2004;1:7–25. [Google Scholar]
- Masuoka Natalie. Together they Become One: Examining the Predictors of Pan-ethnic Group Consciousness among Asian Americans and Latinos. Social Science Quarterly. 2006;87(5):993–1011. [Google Scholar]
- Mays Vickie M, Ponce Ninez A, Washington Donna L, Cochran Susan D. Classification of Race and Ethnicity: Implications for Public Health. Annual Review of Public Health. 2003;24:83–110. doi: 10.1146/annurev.publhealth.24.100901.140927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays Vickie, Cochran Susan, Barnes Namdi W. Race, Race Based Discrimination, and Health Outcomes Among African Americans. Annual Review of Psychology. 2007;58:201–225. doi: 10.1146/annurev.psych.57.102904.190212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller Kristen, Wilson Stephanie. Asking About Race: Survey Question Design for Respondents with Multiple Race Identities. Paper presented at the Annual Meeting of the American Sociological Association; Atlanta, GA. August 16.2003. [Google Scholar]
- Montalvo Frank F, Edward Codina G. Skin Color and Latinos in the United States. Ethnicities. 2001;1(September):321–341. [Google Scholar]
- Morales Maria Christina. The Ethnic Niche as an Economic Pathway for the Dark Skinned Labor Market Incorporation of Latina/o Workers. Hispanic Journal of Behavioral Sciences. 2008;30(3):280–298. [Google Scholar]
- Mossey JM, Shapiro E. Self-rated Health: A Predictor of Mortality among the Elderly. American Journal of Public Health. 1982;72:800–808. doi: 10.2105/ajph.72.8.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers Hector F. Ethnicity-and Socio-economic Status-related Stresses in Context: An Integrative Review and Conceptual Model. Journal of Behavioral Medicine. 2009;32:9–19. doi: 10.1007/s10865-008-9181-4. [DOI] [PubMed] [Google Scholar]
- Nelson William E, Jr, Monforti Jessica Lavariega., editors. Black and Latino/a Politics: Issues in Political Development in the United States. Miami: Barnhardt and Ashe Publishing; 2006. [Google Scholar]
- Paradies Yin. A Systematic Review of Empirical Research on Self-reported Racism and Health. International Journal of Epidemiology. 2006;35(4):888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- Paradies Yin, Cunningham Joan. The DRUID Study: Racism and Self-Assessed Health Status in an Indigenous Population. BMC Public Health. 2012;12:131. doi: 10.1186/1471-2458-12-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perreira Krista, Telles Edward E. The Color of Health: Skin Color, Ethnoracial Classification, and Discrimination in the Health of Latin Americans. Social Science & Medicine. 2014;116:241–250. doi: 10.1016/j.socscimed.2014.05.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prewitt Kenneth. Racial Classification in America: Where Do We Go from Here? Dædalus. 2005 Winter;:4–17. [Google Scholar]
- Rubin RR, Peyrot M. Quality of Life and Diabetes. Diabetes/Metabolism Research and Reviews. 1999;15(3):205–18. doi: 10.1002/(sici)1520-7560(199905/06)15:3<205::aid-dmrr29>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Sanchez Gabriel R, Ybarra Vickie D. New Approaches to the Study of Racial and Ethnic Health Disparities: Advocating Better Measures and Exploration of Internal Variation within Diverse Groups. In: Gomez Laura E, Lopez Nancy., editors. Mapping ‘Race’: Critical Approaches to Health Disparities Research. Piscataway, NJ: Rutgers University Press; 2013. [Google Scholar]
- Saperstein Aliya. Double Checking the Race Box: Examining Inconsistency between Survey Measures of Observed Race and Self-Reported Race. Social Forces. 2006;85(1):57–74. [Google Scholar]
- Saperstein Aliya. Different Measures, Different Mechanisms: A New Perspective on Racial Disparities in Health Care.) Research in the Sociology of Health Care. 2009;27:21–45. [Google Scholar]
- Saperstein Aliya, Penner Andrew. Racial Fluidity and Inequality in the United States. American Journal of Sociology. 2012;118(3):676–727. [Google Scholar]
- Saperstein Aliya. Representing the Multi-dimensionality of Race in Survey Research. In: Gomez Laura E, Lopez Nancy., editors. Mapping ‘Race’: Critical Approaches to Health Disparities Research. New Brunswick, NJ: Rutgers University Press; 2013. pp. 167–187. [Google Scholar]
- Satcher David, Fryer George E, Jr, McCann Jessica, Troutman Adewale, Woolf Steven H, Rust George. What If We Were Equal? A Comparison of the Black-White Mortality Gap in 1960 and 2000. Health Affairs. 2005;24(2):459–464. doi: 10.1377/hlthaff.24.2.459. [DOI] [PubMed] [Google Scholar]
- Schulz Amy J, Williams David R, Israel Barbara, Lempert Lora B. Racial and Spatial Relations as Fundamental Determinants of Health in Detroit. The Milbank Quarterly. 2002;80:677. doi: 10.1111/1468-0009.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shippee Tetyana, Henning-Smith Carrie, Shippee Nathan, Kemmick Jessie Pintor, Call Kathleen T, McAlpine Donna, Johnson Pamela Jo. Discrimination in Medical Settings and Attitudes toward Complementary and Alternative Medicine: The Role of Distrust in Conventional Providers. Journal of Health Disparities Research and Practice. 2013;6(1):30–45. [Google Scholar]
- Smedley Brian D, Stith Adrienne Y, Nelson Alan R. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, D.C: National Academies Press; 2003. [PubMed] [Google Scholar]
- Sternthal Michelle J, Slopen Natalie, Williams David R. Racial Disparities in Health – How Much Does Stress Really Matter? Du Bois Review. 2011;8(1):95–113. doi: 10.1017/S1742058X11000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tafoya Sonya. Shades of Belonging. Pew Hispanic Center; 2004. Dec 6, [accessed July 12, 2013]. http://www.pewhispanic.org/files/reports/35.pdf. [Google Scholar]
- Tashiro CJ. Considering the Significance of Ancestry through the Prism of Mixed-Race Identity. Advances in Nursing Science. 2002;25(2):1–21. doi: 10.1097/00012272-200212000-00002. [DOI] [PubMed] [Google Scholar]
- Telles Edward E, Murguia Edward. Phenotypic Discrimination and Income Differences among Mexican Americans. Social Science Quarterly. 1990;71(4):682–96. [Google Scholar]
- Telles Edward E, Lim Nelson. Does it Matter Who Answers the Race Question? Racial Classification and Income Inequality in Brazil. Demography. 1998;35(4):465–474. [PubMed] [Google Scholar]
- Telles Edward E, Steele Liza. Pigmentocracy in the Americas: How is Educational Attainment Related to Skin Color? Americas Barometer Insights. 2012;73:1–8. [Google Scholar]
- Terkildsen Nayda. When White Voters Evaluate Black Candidates: The Processing Implications of Candidate Skin Color, Prejudice and Self-Monitoring. American Journal of Political Science. 1993;37(4):1032–1053. [Google Scholar]
- Tsai James, Ford Earl S, Li Chaoyang, Zhao Guixiang, Pearson William S, Balluz Lina S. Multiple Healthy Behaviors and Self-Rated Health: Findings from the 2007 Behavioral Rick Factor Surveillance System Survey. Preventive Medicine. 2010;51(3–4):268–274. doi: 10.1016/j.ypmed.2010.07.010. [DOI] [PubMed] [Google Scholar]
- Tsai James, Ford Earl S, Zhao Chaoyang, Balluz Lina S. Physical Activity and Optimal Self-Rated Health of Adults with and Without Diabetes. BMC Public Health. 2010;10:65. doi: 10.1186/1471-2458-10-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhlmann Eric, Dasgupta Nilanjana, Elgueta Angelica, Greenwald Andrew, Swanson Jane. Subgroup Prejudice Based on Skin Color among Hispanics in the United States and Latin America. Social Cognition. 2002;20(3):198–225. [Google Scholar]
- Viruell-Fuentes Edna A. ‘It’s A Lot of Work’ – Racialization Processes, Ethnic Identity Formations, and their Health Implications. Du Bois Review. 2011;8(1):37–52. [Google Scholar]
- Viruell-Fuentes Edna A, Morenoff Jeffrey D, Williams David R, House James S. Language of Interview, Self-Rated Health, and the Other Latino Health Puzzle. AJPH. 2011;101:1306–1313. doi: 10.2105/AJPH.2009.175455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waidmann Timothy A, Rajan Shruti. Race and Ethnic Disparities in Health Care Access and Utilization: An Examination of State Variation. Medical Care Research and Review. 2000;57(4):55–84. doi: 10.1177/1077558700057001S04. [DOI] [PubMed] [Google Scholar]
- Williams David. Race and Health: Basic Questions, Emerging Directions. Annals of Epidemiology. 1997;7(5):322–333. doi: 10.1016/s1047-2797(97)00051-3. [DOI] [PubMed] [Google Scholar]
- Williams David R, Mohammed Selina A. Discrimination and Racial Disparities in Health: Evidence and Needed Research. Journal of Behavioral Medicine. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams David R, Sternthal Michelle. Understanding Racial-ethnic Disparities in Health: Sociological Contributions. Journal of Health and Social Behavior. 2010;51(S):S15–S27. doi: 10.1177/0022146510383838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo Meghan, Bryn Austin S, Williams David R, Bennett Gary G. Reconceptualizing the Measurement of Multiracial Status for Health Research in the United States. Du Bois Review. 2011;8(1):25–36. [Google Scholar]
- Zsembik Barbara, Fennell Dana. Ethnic Variation in Health and the Determinants of Health among Latinos. Social Science and Medicine. 2005;61(1):53–63. doi: 10.1016/j.socscimed.2004.11.040. [DOI] [PubMed] [Google Scholar]
- Zullig Keith J, Hendryx Michael. Comparative Analysis of Health Related Quality of Life (HRQOL) for Residents of US Counties with and without Coal Mining. Public Health Reports. 2010;125(4):548–555. doi: 10.1177/003335491012500410. [DOI] [PMC free article] [PubMed] [Google Scholar]