Recent decades have not been kind to those in the middle and bottom of the income distribution. From 1999 to 2013, real (inflation adjusted) per capita gross domestic product in the United States grew by 16%. During the same period, median real income for households headed by a high school graduate dropped by 19%. Despite this widening economic inequality and the additional stress of the 2007–2009 Great Recession, the continued improvement in United States life expectancy throughout this period—an increase of 2.1 y—along with better health among the elderly (1), provided at least some modicum of comfort that health was improving, even if economic standards were not. Case and Deaton, in their PNAS article “Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century” (2), have dashed even this cautiously optimistic view of the past several decades.
Using cause-of-death statistics from 1999 to 2013, Case and Deaton (2) demonstrate that death rates for white non-Hispanics at midlife, age 45–54 y, were rising, rather than falling as they had in the decades before 1999. Furthermore, the increased mortality from poisoning (drugs and alcohol), suicides, and related external causes (32.8 per 100,000 people) appears to fully explain the entire rise in mortality during this period (33.9 per 100,000).
The study has far-reaching implications for the financial health of the federal Medicare, Medicaid, and disability insurance programs. To the extent that this generation of baby-boomers and postbaby-boomers are approaching retirement with a higher prevalence of chronic diseases, we might expect a more rapid rise in expenditures for those newly covered by disability insurance and Medicare, and a sooner-than-expected date at which the Social Security Disability Insurance and Medicare trust funds run dry (3).
This rise in mortality rates is surprising for at least four reasons. First, it is remarkable that it took more than a decade to bring this reversal to the attention of the scientific community. There is an increasing realization that disability rates among the near-elderly are stagnant or rising (4). We are aware of only one other study that focused on rising mortality from poisoning in the context of aggregate mortality, but this work focused only on the how poisoning deaths narrowed black-white gaps in life expectancy, presenting no information on all-cause mortality by race (5). Second, within this group, mortality rates grew by a stunning 134 per 100,000 among individuals with a high school degree or less education. It is difficult to find modern settings with survival losses of this magnitude, although Russian males experienced a well-known and larger rise in mortality rates during a similar time span straddling the collapse of the Soviet Union (6).
Third, the trend is observed only for white non-Hispanics, and not for the black or Hispanic populations, who experienced a continued decline in mortality during the same period. One possible explanation is a differentially rapid decline in HIV/AIDS-related deaths among minority populations. The death rate for HIV/AIDs did indeed decline for blacks by 45.8 per 100,000, and for Hispanics by 8.2 per 100,000 more than for non-Hispanic whites (7). However, this cannot explain more than a small fraction of the total gap.
Another possibility is that racial differences in prescription opioids dispensed and misuse of prescription opioids could explain the differential mortality path. The share of Social Security Disability Insurance Medicare beneficiaries age 21–64 y who fill six or more prescriptions annually is 30% higher for whites than for blacks (8), and rates of prescription opioid use disorders are also somewhat lower for blacks (9). These differences seem too modest to explain the reversal in mortality rates, because one would require changes over time in the ratio of black-white opioid use to explain the large differential growth in black-white mortality rates.
However, another potential explanation is a rise in white non-Hispanic households without insurance during the period of analysis. From 2002 to 2013, the proportion of white non-Hispanics without insurance coverage remained steady at just under 10%. For both blacks and Hispanics, lack of coverage fell by 2.8 and 5.4 percentage points, respectively (10). Again, this seems unlikely to be a big enough change to explain steady mortality declines for blacks and Hispanics and the dramatic reversal of mortality for white non-Hispanics.
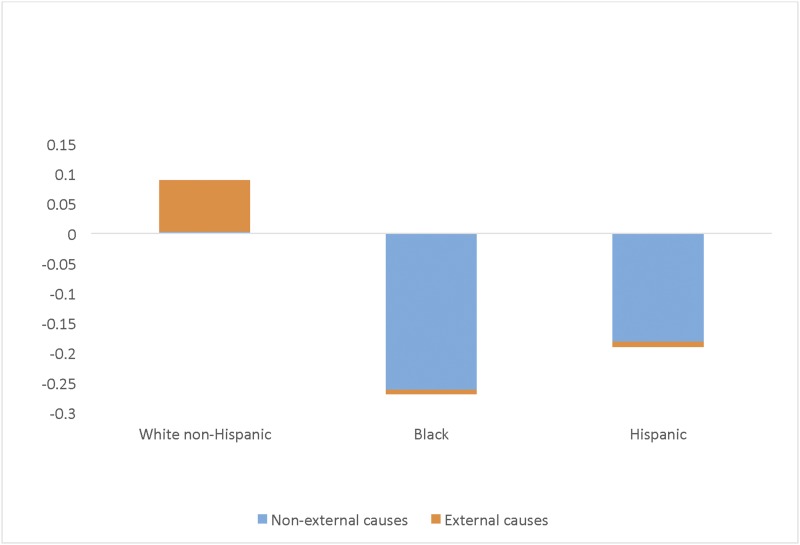
Finally, the Case and Deaton (2) result is surprising because it might appear to the casual reader that a rapidly rising rate of death as a result of external causes was the primary cause for what went wrong with this cohort of middle-aged people. In Fig. 1 we display the proportional changes in white non-Hispanic, black, and Hispanic mortality rates between 1999 and 2013, for ages 45–54, taken from table 1 in ref. 2. The mortality declines (or increase) are further split into two parts: those resulting from external causes (e.g., poisoning, self-harm, transport accidents, and cirrhosis) and those resulting from other causes. Although the external causes explain the jump up in mortality for white non-Hispanics, they cannot explain why there wasn’t a corresponding decline commensurate with the other comparison groups. Had mortality rates in this population fallen at the average rate of decline among black and Hispanic rates, we would have predicted roughly 88 fewer deaths per 100,000 population.
Fig. 1.
Proportional change in mortality 1999–2013, by race and ethnicity. Data from table 1 in ref. 2.
What accounts then for the lack of progress in white non-Hispanic mortality for those aged 45–54 y? One explanation is that drug- or alcohol-related deaths are attributed to other diseases, such as chronic lower respiratory diseases, assault, viral hepatitis, and deaths resulting from falls that are often the consequence of excess drug or alcohol use. Mortality attributed to these diseases certainly grew among white non-Hispanics even as they declined for Hispanics and blacks during the study period (7). This can’t be the entire story, however, because death rates for many other causes related to cardiovascular disease, diabetes, and to a lesser extent, cancer diverged for white non-Hispanics and Hispanics during this period.
Case and Deaton (2) consider the Great Recession and a long productivity slowdown that preceded it as one explanation driving the mortality trends they report, but note that Europe has experienced similar slowdowns without any mortality reversal. Economic conditions seem like an unlikely source of the mortality reversal if only because events like the Great Recession affected white non-Hispanics less than Hispanics or blacks (10).
However, the response to negative economic events is not even across these groups. In June of 2010, when unemployment rates
Using cause-of-death statistics from 1999 to 2013, Case and Deaton demonstrate that death rates for white non-Hispanics at midlife, age 45–54 y, were rising, rather than falling as they had in the decades before 1999.
stood at 9.7%, a Pew survey asked respondents if they thought their financial situation would improve or get worse in the coming year. Eighty-one percent of blacks thought their financial situation would improve, compared with only 57% of white non-Hispanics (11). Alongside the mortality findings, Case and Deaton (2) demonstrate significant increases in adverse physical and mental health, increased pain, risk for heavy alcohol use, and evidence of organ damage related to alcohol use. These trends in morbidity are consistent with this pessimism, and could lead to higher rates of mortality among diseases not usually associated with drug or alcohol abuse.
Some support for this view comes from Russia, when there was a sharp increase in mortality during the 1980s and 1990s. There was no support for the view that the health care system, diet, or material depravation drove mortality increases. In contrast, alcohol consumption, external causes of death, and stress related to a poor outlook of the future were much more closely related to the sharp rise in mortality rates (6).
Case and Deaton (2) do not provide a complete solution to the mystery of why middle-aged people in the United States are facing rising mortality and morbidity over time; these are aggregate statistics, and as Case and Deaton have shown in their other research (12, 13), the solution is likely to be found by studying individuals and their health-related behaviors. Ironically, a new interpretation of rules by the Centers for Medicare and Medicaid Services have made it even more difficult to study addiction trends, which appear to play an important role in growing mortality over the period. In response to privacy concerns by patient advocates, the Centers for Medicare and Medicaid Services now routinely delete all hospital and physician records related to drugs or alcohol, making it impossible for researchers to document changes over time in, for example, emergency room admissions for drug overdoses (14). Case and Deaton (2) have clearly identified a serious public health problem, and we will need all of the resources of population-based epidemiology and clinical-based insights to solve it.
Footnotes
The authors declare no conflict of interest.
See companion article on page 15078.
References
- 1.Cutler DM, Ghosh K, Landrum MB. Evidence for significant compression of morbidity in the elderly U.S. population. In: Wise D, editor. Discoveries in the Economics of Aging. Univ of Chicago Press; Chicago: 2014. [Google Scholar]
- 2.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci USA. 2015;112:15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lakdawalla DN, Goldman DP, Shang B. The health and cost consequences of obesity among the future elderly. Health Aff (Millwood) 2005;24(Suppl 2):W5R30–W5R41. doi: 10.1377/hlthaff.w5.r30. [DOI] [PubMed] [Google Scholar]
- 4.Chen Y, Sloan FA. Explaining disability trends in the U.S. elderly and near-elderly population. Health Serv Res. 2015;50(5):1528–1549. doi: 10.1111/1475-6773.12284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harper S, Rushani D, Kaufman JS. Trends in the black-white life expectancy gap, 2003-2008. JAMA. 2012;307(21):2257–2259. doi: 10.1001/jama.2012.5059. [DOI] [PubMed] [Google Scholar]
- 6.Brainerd E, Cutler DM. Autopsy on an empire: Understanding mortality in Russia and the former soviet union. J Econ Perspect. 2005;19(1):107–130. [Google Scholar]
- 7.Center for Disease Control and Prevention . Compressed Mortality File 1999-2013 on CDC WONDER Online Database, released October 2014. Series 20. National Center for Health Statistics; Rockville, MD: 2014. [Google Scholar]
- 8.Morden NE, et al. Prescription opioid use among disabled Medicare beneficiaries: Intensity, trends, and regional variation. Med Care. 2014;52(9):852–859. doi: 10.1097/MLR.0000000000000183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003–2013. JAMA. 2015;314(14):1468–1478. doi: 10.1001/jama.2015.11859. [DOI] [PubMed] [Google Scholar]
- 10. US Census Bureau, Current Population Survey (CPS) Table Creator. CPS Annual Social and Economic Supplements 2003, 2007, 2010, and 2014. Available at www.census.gov/cps/data/cpstablecreator.html. Accessed October 18, 2015.
- 11.Taylor P, et al. 2010. How the Great Recession Has Changed Life in America (Pew Research Center, Washington, DC)
- 12.Case A, Deaton A. Large cash transfers to the elderly in South Africa. Econ J. 1998;108(Sept):1330–1361. [Google Scholar]
- 13.Case A, Deaton A. Health and wealth among the poor: India and South Africa compared. Am Econ Rev. 2005;95(2):229–233. doi: 10.1257/000282805774670310. [DOI] [PubMed] [Google Scholar]
- 14.Frakt AB, Bagley N. Protection or harm? Suppressing substance-use data. N Engl J Med. 2015;372(20):1879–1881. doi: 10.1056/NEJMp1501362. [DOI] [PubMed] [Google Scholar]