Developing effective communication strategies to increase vaccine uptake is crucial in times of increasing vaccine hesitancy and repeated outbreaks of vaccine-preventable diseases. Horne et al. (1) conclude from their study that a combination of warnings, an anecdote about a sick child, and pictures thereof are suitable to counter antivaccination attitudes; however, correcting vaccination myths proved unsuccessful. Yet, the study is somewhat fuzzy about what “antivaccination” actually means. It further summarizes different constructs in a single-attitude variable that we believe deserve separate attention. These two considerations led us to reanalyze the study’s data, resulting in the additional, important conclusions outlined below.
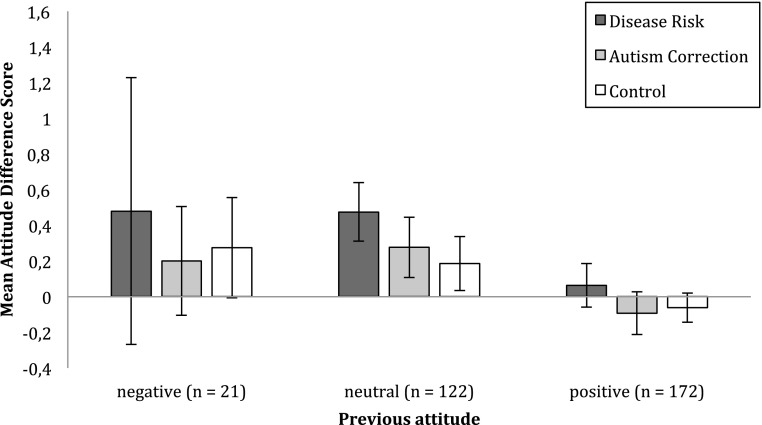
The sample in Horne et al.’s study is generally provaccination (figure 3 in ref. 1). The authors divide the sample according to the terciles of the distribution. This results in a bottom category—suggesting these are the antivaccinators—that comprises participants with attitude scores ranging from 1 to 4.4 on a scale from 1 to 6, with M = 3.60, SD = 0.89 (middle category: 4.6–5.4; top category: 5.6–6). In a reanalysis, we used the scale values for categorization (details below Fig. 1). The results reveal that the effect reported in Horne et al.’s report was actually caused by the fence-sitters: that is, those individuals who are neither for nor against vaccination (Fig. 1). Additionally, both the disease risk and the autism correction intervention improved the fence-sitters’ attitudes. It also becomes evident that the antivaccinators’ attitudes did not change as a result of the interventions.
Fig. 1.
Mean attitude difference scores (posttest minus pretest) as a function of communication strategies and prior attitude. Data from ref. 1. Prior attitude scores (PAS) were classified based on the scale values: negative attitude: PAS < 3, neutral: 3 ≥ PAS < 5, positive: PAS ≥ 5. n = 315. Error bars are 95% confidence intervals.
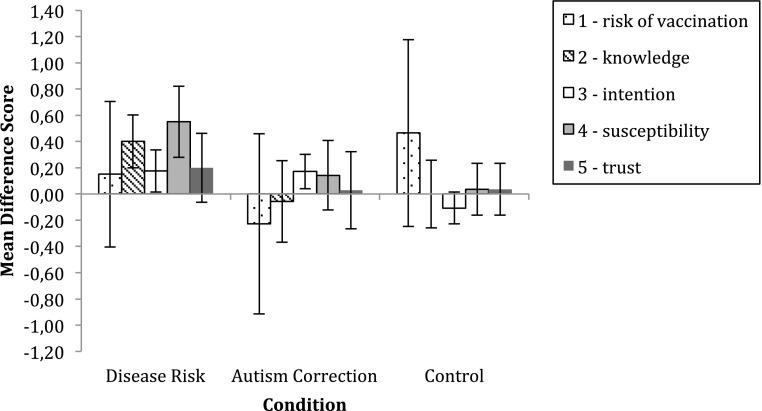
Additionally, we would like to challenge the way in which the attitude toward vaccination is operationalized. Generally, attitudes are “a psychological tendency that is expressed by evaluating a particular entity with some degree of favor or disfavor” (2). Horne et al. (1) operationalize attitude as a mean of five different variables that resemble constructs, such as perceived risk of vaccination and the intention to vaccinate (Fig. 2). These are theoretically very different constructs (3), and interventions might influence these constructs in a different manner (4). It is therefore important to identify the interventions’ effects on these constructs. Moreover, the interventions are directed toward parents and three of five items are related to childhood vaccinations. Thus, a closer look at parents is advisable. A reanalysis of parents’ data (n = 103) shows that one of the major barriers to vaccination behavior, perceived risk of vaccination, was not at all affected by either intervention (Fig. 2). The intention to vaccinate, however, increased both as a result of the disease risk as well as autism correction intervention.
Fig. 2.
Mean difference scores of the dependent variables (posttest minus pretest) as a function of communication strategies. Data from ref. 1. The sample consists of parents with children ≤18 years (n = 103). The attitude construct was decomposed in its original variables, resembling the following constructs: 1) risk of vaccination (“The risk of side effects outweighs any protective benefits of vaccines”); 2) knowledge (“Vaccinating healthy children helps protect others by stopping the spread of disease”); 3) intention (“I plan to vaccinate my children”); 4) susceptibility (“Children do not need vaccines for diseases that are not common anymore”); 5) trust (“Doctors would not recommend vaccines if they were unsafe”). Error bars are 95% confidence intervals.
In summary, we would like to extend Horne et al.’s (1) conclusion and stress the importance of both increasing the awareness of disease risks and correcting vaccination myths. Both strategies will change the utility of vaccination and may increase intentions to vaccinate. The data show that countering antivaccination attitudes is difficult. Rather than attempting to convert a small number of antivaccinators, it seems more promising to target the larger group of fence-sitters (4, 5) because they may be more responsive to interventions.
Acknowledgments
We thank Zachary Horne and his co-authors for providing us with the original data and detailed descriptions of all variables.
Footnotes
The authors declare no conflict of interest.
References
- 1.Horne Z, Powell D, Hummel JE, Holyoak KJ. Countering antivaccination attitudes. Proc Natl Acad Sci USA. 2015;112(33):10321–10324. doi: 10.1073/pnas.1504019112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eagly AH, Chaiken S. The Psychology of Attitudes. Harcourt Brace Jovanovich; Fort Worth, TX: 1993. [Google Scholar]
- 3.Ajzen I. The theory of planned behavior. In: Lange PAM, Kruglanski AW, Higgins ET, editors. Handbook of Theories of Social Psychology. Sage; London, UK: 2012. pp. 438–459. [Google Scholar]
- 4.Betsch C, Böhm R, Chapman GB. Using behavioral insights to increase vaccination policy effectiveness. Policy Insights from Behav Brain Sci. 2015;2:61–73. [Google Scholar]
- 5.Leask J. Target the fence-sitters. Nature. 2011;473(7348):443–445. doi: 10.1038/473443a. [DOI] [PubMed] [Google Scholar]