A nationally representative, cross-sectional survey of women aged 30–59 years in Bangladesh showed that 81.6% of women had heard of cervical cancer (CCa) but only 48.6% were aware of CCa screening. Only 8.3% had ever been screened. Lack of CCa awareness and of understanding of the concept of screening are the key barriers to screening uptake in this cohort.
Keywords: Awareness, Barriers, Cervical cancer, Screening, Bangladesh
Abstract
Background.
Cervical cancer (CCa) is the second most common cancer among women in Bangladesh. The uptake of CCa screening was less than 10% in areas where screening has been offered, so we investigated the awareness of CCa and CCa screening, and factors associated with women’s preparedness to be screened.
Methods.
A nationally representative, cross-sectional survey of women aged 30–59 years was conducted in 7 districts of the 7 divisions in Bangladesh, using a multistage cluster sampling technique. Factors associated with the awareness of CCa and screening uptake were investigated separately, using multivariable logistic regression.
Results.
On systematic questioning, 81.3% and 48.6% of the 1,590 participants, whose mean age was 42.3 (±8.0) years, had ever heard of CCa and CCa screening, respectively. Having heard of CCa was associated with living in a rural area (adjusted odds ratio [OR]: 0.42; 95% confidence interval [CI]: 0.26–0.67), being 40–49 years old (OR: 1.59; 95% CI: 1.15–2.0), having no education (OR: 0.25; 95% CI: 0.16–0.38), and being obese (OR: 2.04; 95% CI: 1.23–3.36). Of the 773 women who had ever heard of CCa screening, 86% reported that they had not been screened because they had no symptoms and 37% did not know screening was needed. Only 8.3% had ever been screened. Having been screened was associated with being 40–49 years old (OR: 2.17; 95% CI: 1.19–3.94) and employed outside the home (OR: 3.83; 95% CI: 1.65–8.9), and inversely associated with rural dwelling (OR: 0.54; 95% CI: 0.30–0.98) and having no education (OR: 0.29; 95% CI: 0.10–0.85).
Conclusion.
Lack of awareness of CCa and of understanding of the concept of screening are the key barriers to screening uptake in women at midlife in Bangladesh. Targeted educational health programs are needed to increase screening in Bangladesh with the view to reducing mortality.
Implications for Practice:
This is the first nationwide and population-based study in Bangladesh to collect detailed information pertaining to the awareness of cervical cancer and cervical cancer screening, and factors associated with women’s preparedness to undergo screening. Rather than cultural and religious barriers, lack of awareness and knowledge of cervical cancer and screening present the primary barriers to screening uptake. The results highlight the urgent need for health education programs that have the potential to increase cervical cancer awareness and screening uptake, and reduce cervical cancer mortality.
Introduction
Cervical cancer (CCa), a highly preventable disease, is the second most common cancer in women in Bangladesh, with approximately 54.4 million women aged 15 years and older potentially at risk [1]. Current estimates reveal that 17,686 Bangladeshi women are diagnosed and 10,364 women in the country die of CCa each year [2]. The annual crude incidence rate of invasive CCa in Bangladesh is lower (15.9 per 100,000) than the annual overall incidence rate in South Asia (17.1 per 100,000); however, it is higher than the global annual crude incidence rate of 15.1 per 100,000 [1, 3].
To reduce the burden of this disease, Bangladesh launched in 2004 a national, opportunistic CCa screening program of visual inspection after application of acetic acid for women over the age of 29 years. This is now available at 252 facilities, from tertiary to primary care levels [4]. The screening uptake among women aged 30–59 years has been low (8.6%), resulting in low coverage of the target population [5]. Furthermore, poor compliance with colposcopy, when indicated, has been reported [4, 5].
The Bangladesh Midlife Women’s Health Study (BMWHS) was a population-based survey undertaken between September 2013 and March 2014 to determine women’s awareness of CCa and uptake of CCa screening, and to identify socioeconomic, cultural, and religious barriers to screening uptake.
Materials and Methods
Study Setting and Participants
We used a multistage cluster sampling method to obtain a representative sample of women, aged 30–59 years, living in each of the 7 major administrative divisions that comprise the 64 administrative districts of Bangladesh. The 7 selected districts (Barisal, Tangail, Comilla, Sathkhira, Rajshahi, Rangpur, and Habigonj) were randomly selected from the 32 districts offering opportunistic CCa screening, as described in detail elsewhere [6]. The number of women recruited in each of the 7 districts was determined by the distribution of the 3.24 million women of the target age group in these districts in the 2011 population and housing census, taking into account the ratio of urban to rural women in each district [7]. Within each district, there are enumeration areas (EAs) that are the smallest units with a defined area that include, on average, 120 households [8].
When the total sample size of 1,590 women was distributed across the rural and urban areas of the 7 districts, the smallest number of women required in any single EA was 36 [6]. Thus, the household selection was an unequal probability systematic selection with 36 households per EA. The EAs within each district were selected randomly, and within each EA, the first household was selected at random. Subsequent households (whether second, third, or fourth) were selected by using systematic sampling. Only one eligible woman was recruited from each household. If an index woman was not found in a selected household, the adjacent household was approached. In line with the multistage cluster design, sampling weight ensured representativeness of the sample at all stages. The calculation details and description of sample weight are provided in the supplemental online Appendix.
Sample Size
The sample size calculation was based on the estimated prevalence of CCa screening uptake (8.6%) [4], with a margin of error of ±2%, among women at midlife, resulting in a minimum sample size of 755. This was then multiplied by the design effect of 2, as the urban and rural EAs were considered independently. The sample size was further increased by 5% to allow for nonsampling error, particularly nonresponse error. Thus, the final estimated sample size was 1,590 women.
Data Collection
Literacy in Bangladesh is low; thus, participation involved a structured interview during which the interviewer completed the study questionnaire. Interviews were conducted by 4 female university graduates who underwent a 2-week intensive training program that included mock interviews and field practice to ensure interview consistency. A verbal explanation of the objectives, general content, and time commitment involved in participation was provided, as was assurance of confidentiality. Verbal consent was then obtained. Completed questionnaires were reviewed daily and, if necessary, households were revisited the next day to resolve any ambiguities or to collect missing data.
The study questionnaire captured personal, sociodemographic and household characteristics, and knowledge and awareness of CCa and CCa screening. The latter were assessed by five questions: have you ever heard of CCa; have you or a member of your family had cervical cancer; can you please tell me any symptoms that would indicate a woman has CCa; have you ever heard about women having screening to find cervical cancer, and do you know of any methods of cervical cancer screening? The questionnaire also included a series of questions about potential barriers to screening. Based on the Bangladesh Demographic and Health Survey, each household’s “wealth index” was derived from variables such as housing materials, furniture and other assets, sources of water, and sanitation [9]. The questionnaire was first developed in English and translated into Bengali. Translation accuracy was verified by an independent bilingual translator and further verified by back-translation. The questionnaire was finally piloted in 16 women, after which minor refinements were made.
The BMWHS was approved by the Monash University Human Research Ethics Committee, Melbourne, Australia, and the Bangladesh Medical Research Council, Dhaka, Bangladesh.
Statistical Analysis
CCa awareness (ever heard of CCa) and CCa screening uptake were considered as two outcome variables. CCa awareness was investigated for all study participants, whereas CCa screening uptake was investigated only for those who ever heard of CCa screening. Univariate and multivariable logistic regressions were used to evaluate the association between each of the outcomes and participants’ socioeconomic and demographic characteristics. Each household’s wealth index was ascertained using a principal component analysis and was presented as wealth quintiles [9, 10]. We considered 11 variables as potential predictors for both outcomes; however, husband’s education and wealth quintiles were excluded from the multivariable logistic regression models because of multicolinearity with women’s education and place of residence, respectively. A variable with a p value of less than or equal to 0.05 was considered significant. The area under the receiver operating characteristics curve (ROC) and the Hosmer and Lemeshow (H-L) p value were used to assess the model’s discrimination and calibration performances. The first-degree interaction effect between independent variables was also investigated. All analyses were performed using statistical software packages Stata version 12.0 (StataCorp, College Station, TX, http://www.stata.com) and SPSS version 20.0 (IBM Corp., Chicago, IL, http://www-01.ibm.com).
Results
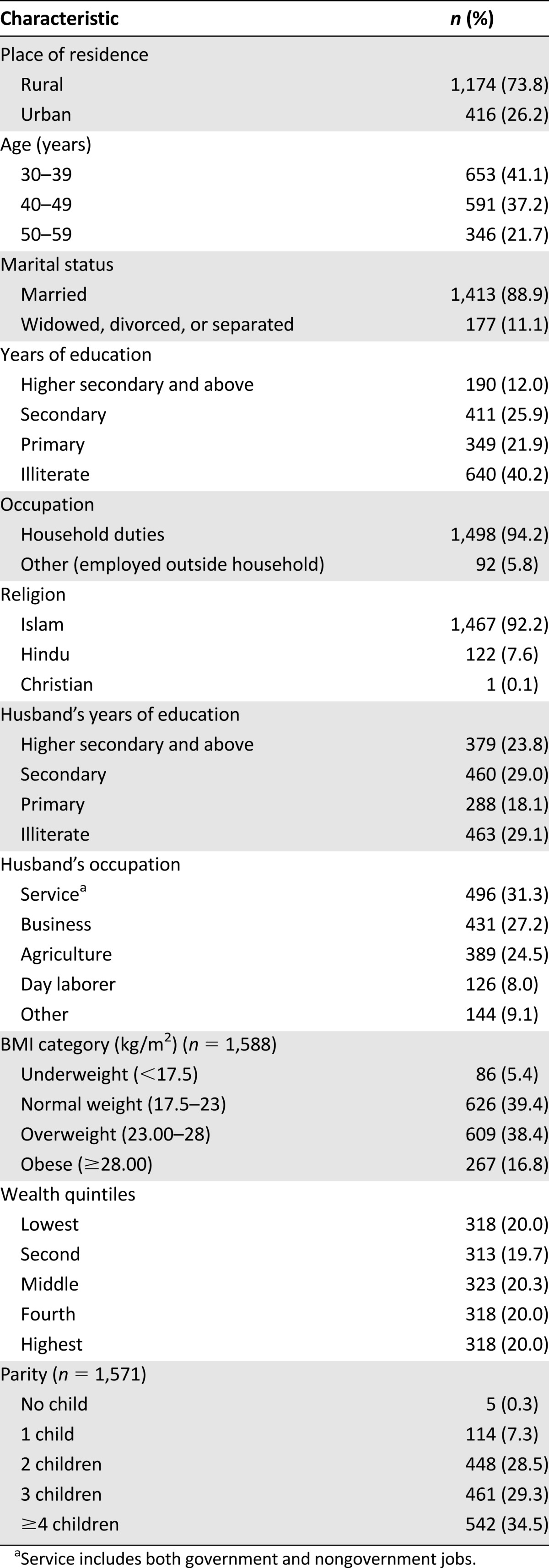
We approached 1,700 households and 1,590 women agreed to be interviewed in the study. The mean age of the participants was 42.3 (±8.0) years (Table 1). Of the 1,590 participants, 73.8% resided in rural areas. The majority (94.2%) were not employed outside the home, 88.9% were married, and 92.2% reported their religion as Islam. Having had no formal education was reported by 40.2% of the women and 12.0% had more than 10 years of education; 29.1% of the women reported that their husband had no education, and 32.5% of the women’s husbands worked in agriculture or as day laborers. Findings also showed that 16.8% of participants were obese and 5.4% were underweight, and 34.5% of the women had 4 or more children and 0.3% were nulliparous.
Table 1.
Characteristics of women in the Bangladesh Midlife Women’s Health Study (n = 1,590)
Knowledge and Awareness of Cervical Cancer and Screening
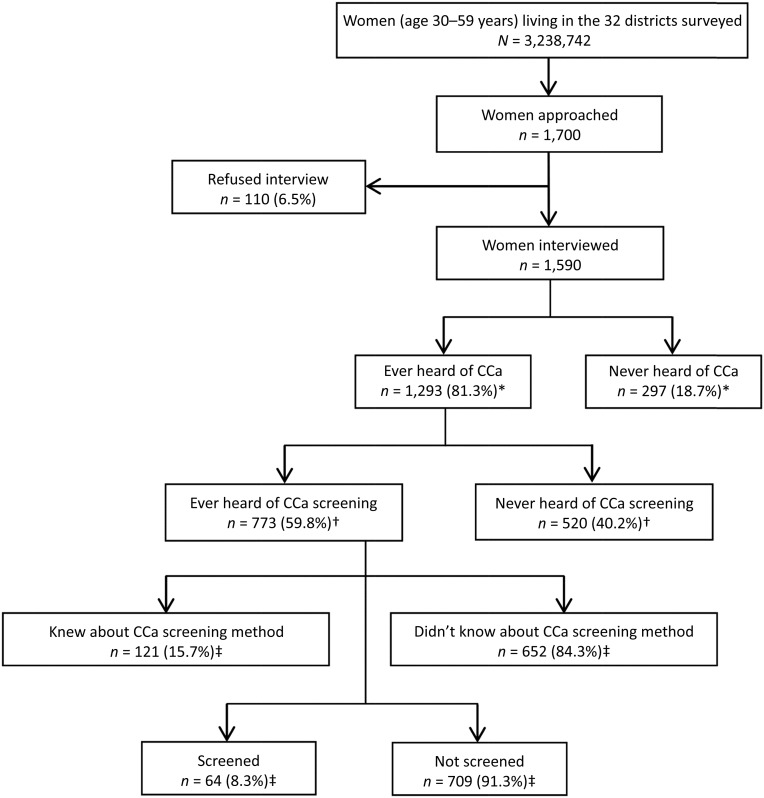
Systematic questioning revealed that 81.3% of the women had ever heard of CCa (Fig. 1). Of these, 59.8% had heard of CCa screening. Of the 773 women who had ever heard of CCa screening, 15.7% were able to report at least 1 method of CCa screening, 8.3% had been screened, 2.9% reported that a member of their family had had CCa, and 21.7% identified at least 1 correct CCa symptom from a list of symptoms provided (data not shown).
Figure 1.
Flowchart of women who had ever heard of cervical cancer and cervical cancer screening in the Bangladesh Midlife Women’s Health Study population. ∗, percentage of those interviewed; †, percentage of those who had ever heard of CCa; ‡, percentage of those who had ever heard of CCa screening.
Abbreviation: CCa, cervical cancer.
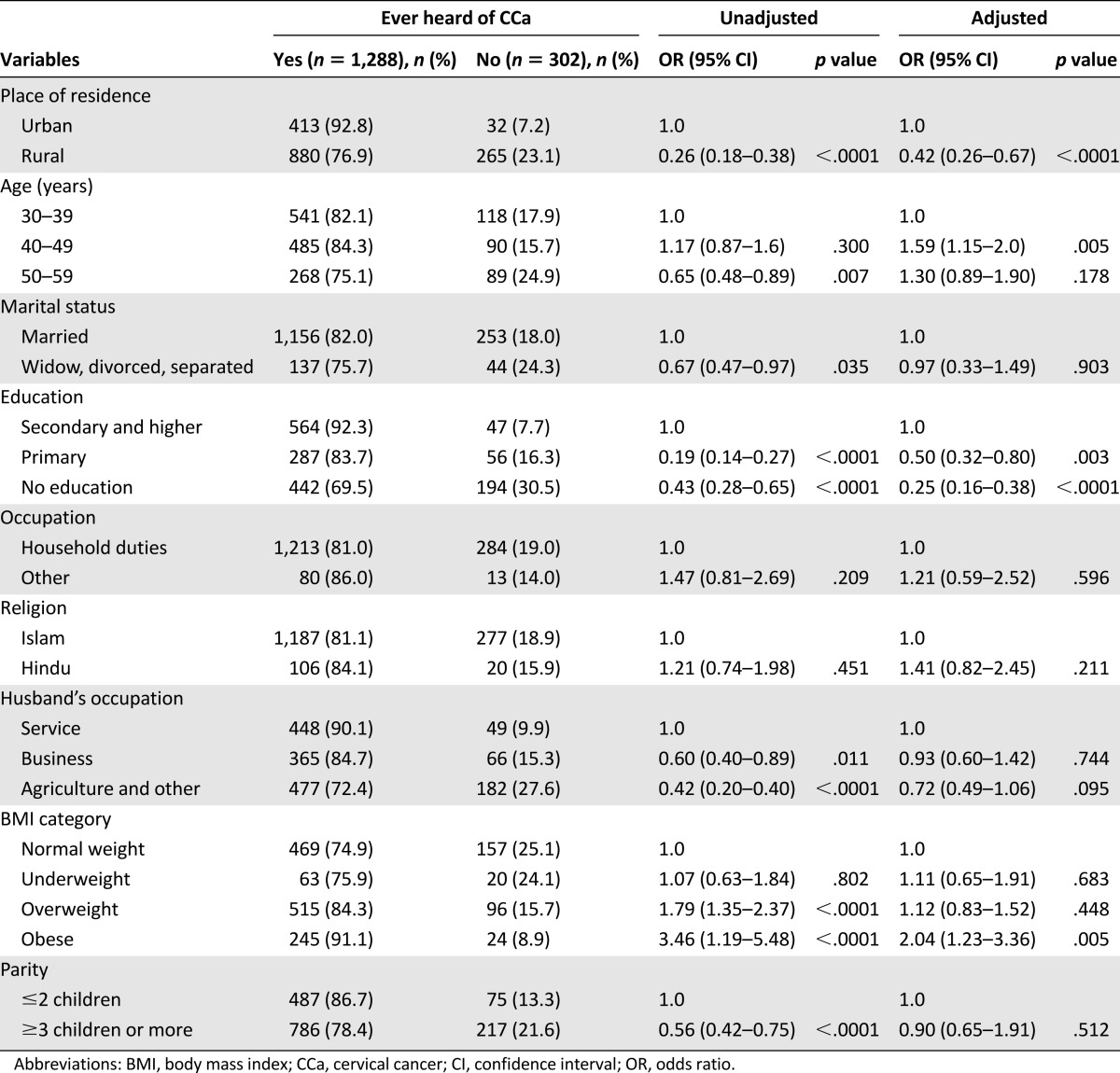
We recorded 11 potential predictors of CCa awareness, of which 9 were retained in the multivariable logistic regression model (Table 2). Women were less likely to have heard of CCa if they were living in a rural area (adjusted odds ratio [OR]: 0.42; 95% confidence interval [CI]: 0.26–0.67), and had primary (OR: 0.50; 95% CI: 0.32–0.80) or no education (OR: 0.25; 95% CI: 0.16–0.38). Women aged 40–49 years were more likely to know about CCa compared with women aged 30–39 years (OR: 1.59; 95% CI: 1.15–2.0), and obese women were more likely to be aware of CCa compared with women of normal body mass index (OR: 2.04; 95% CI: 1.23–3.36). The ROC and H-L p values for the model were .736 and .085, respectively.
Table 2.
Univariate and multivariable analyses of factors associated with having ever heard of cervical cancer (n = 1,590)
Barriers and Screening Uptake
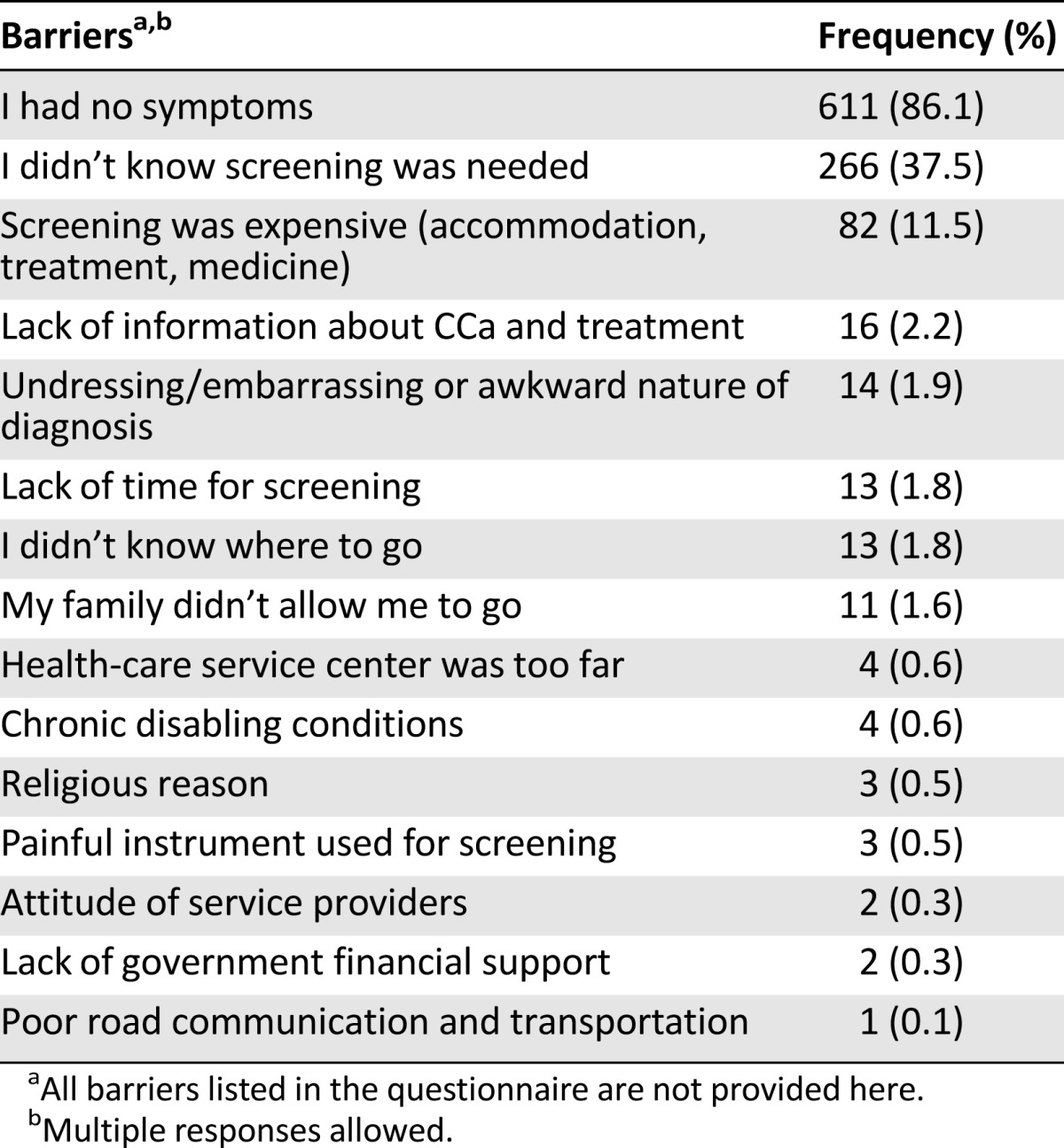
Of the 709 women who had ever heard of CCa screening but had not been screened, the reasons given for not undergoing screening included having no symptoms (86.1%), not knowing screening was needed (37.5%), and possible expense associated with screening (11.5%) (Table 3). Modesty issues and religious barriers were reported by 1.9% and 0.5% of women, respectively.
Table 3.
Women’s reasons for not being screened for cervical cancer (n = 709)
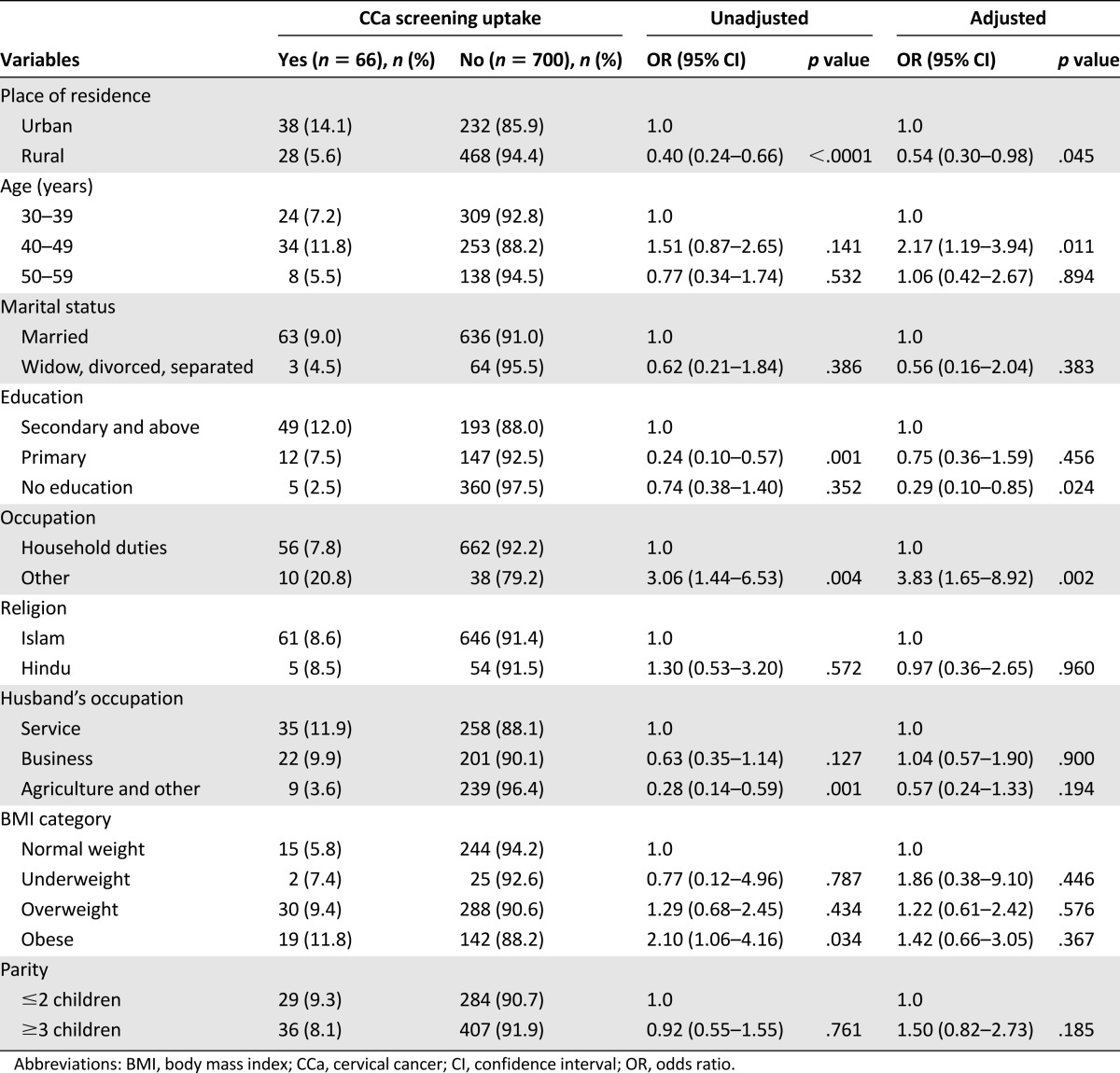
In the multivariable logistic regression model of potential predictors of uptake of CCa screening, being employed outside the home was strongly associated with screening (OR: 3.83; 95% CI: 1.65–8.92) (Table 4). Women aged 40–49 years were more likely to have been screened than women aged 30–39 years (OR: 2.17; 95% CI: 1.19–3.94). Women were less likely to have been screened if they lived in a rural area (OR: 0.54; 95% CI: 0.30–0.98) and had no education (OR: 0.29; 95% CI: 0.10–0.85). The ROC and H-L p values for the model were .744 and .241, respectively.
Table 4.
Univariate and multivariable analyses of factors associated with cervical cancer screening among women who had ever heard of screening (n = 773)
Discussion
In this representative sample of Bangladeshi women aged 30–59 years, the primary barrier to CCa screening was lack of knowledge. Although greater than 80% of women reported they had heard of CCa, nearly 40% of these women said they were unaware of a screening test for this condition, despite residing in areas where opportunistic screening had been offered. Similar findings have been reported in a recent study in Tanzania [11]. Furthermore, greater than 90% of the women who said they were aware of screening did not take up screening because they reported that either they had no symptoms or did not know screening was needed, or both. Contrary to our expectations, few women offered cultural or religious beliefs as barriers to screening. Accurate knowledge of symptoms of CCa was limited, consistent with the findings of a previous qualitative study of community perceptions of CCa and screening in Bangladesh [12]. The lower level of awareness of CCa in rural communities most likely reflects low media exposure, poor literacy, poverty, and women not undertaking employment outside the home. Also associated with awareness of CCa were age, level of education, and obesity. That middle-aged women were more likely than younger women to have ever heard of CCa might be because of their greater exposure to maternal and child health services implemented in Bangladesh after the country’s independence in 1971 [13]. Studies in India have reported that prior exposure to reproductive health services was influential in creating awareness of CCa screening [14, 15]. In addition to older women having had greater exposure to health services, younger women may well have the perception that, being in good health, they are not at risk. The association between education and knowledge of CCa is not surprising. In our study, obesity was associated with urban living and high socioeconomic status, which may explain why obese women were more likely to have ever heard of CCa.
We hypothesized that cultural and religious beliefs, as well as access to screening facilities, might be operating as barriers to CCa screening uptake, as reported in other countries [16–23]. To address this issue, we asked a separate question about possible reasons for not attending for CCa screening. The minimal influence of cultural and religious beliefs on the decision to be screened is a positive finding because these factors can be challenging to modify. Our most important finding was that the majority of women who had heard of CCa screening did not understand the concept of “screening” but rather thought this should only be undertaken if symptoms were present. The variables positively associated with CCa screening in our study—namely, level of education, urban living, employment outside the home, and age—are all indices of opportunity for knowledge acquisition. The impact of age is in agreement with studies undertaken in rural Malaysia, Tanzania, and New Zealand [24–26].
Our data strongly support the proposal that a broad, community-based awareness program is likely to improve CCa screening uptake in Bangladesh [5]. But our findings also demonstrate that the development of an awareness program in Bangladesh must take into account both the low level of literacy and that few women work outside their homes. Therefore, to be effective, an awareness campaign would need to incorporate visual and verbal communication, and be able to reach women in their immediate domestic environment. A model piloted in Bangladesh for breast health promotion has involved the use of smartphone technology by community workers [27]. This model could be adapted to improve knowledge of CCa screening, treatment, and, ultimately, vaccination.
A major strength of the BMWHS is the robust sampling of a socioeconomically heterogeneous group of women living in regions where CCa screening has been available for some years. This unique data set has enabled us to explore the impact on CCa screening of a range of demographic variables. Careful questionnaire development, interviewer training, and quality control of interviews ensured the credibility of the results. That the level of screening uptake in our study is identical to an independent report of uptake [4] provides strong evidence of external validity. Recall and reporting bias with respect to some questions pertaining to awareness, knowledge, and barriers to screening uptake might have occurred. Although 80% of the participants in our study said they had heard of CCa, this figure may be an overestimate, as many of the women had difficulty distinguishing between CCa and cancer of other reproductive organs, or other conditions such as genital prolapse or fistula.
Conclusion
Awareness of the role of screening is the key barrier to CCa screening uptake in Bangladesh. Health education programs, appropriately adapted to the target population, particularly women confined to their homes and who are illiterate, younger, and living in rural areas, have the potential to increase CCa screening uptake and reduce CCa mortality.
See http://www.TheOncologist.com for supplemental material available online.
Supplementary Material
Acknowledgments
The study was supported by philanthropic donations to the Women’s Health Research Program, Monash University. The donors had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. We thank the Bangladesh Civil Service Administration Cadre Mohammad Alamgir Kabir, who arranged accommodation for our survey team in all study sites. We thank Dr. Roslin Botlero for verifying our study instrument. We thank Afruza Arman, Lamia Anwar, Lila-Nur Shemonto, and Tasmia Haque for their sincere efforts in data collection, and the midlife women of Bangladesh for participating in this study.
Author Contributions
Conception and Design: Rakibul M. Islam, Robin J. Bell, Susan R. Davis
Provision of study material or patients: Rakibul M. Islam, Mohammad B. Hossain
Collection and/or assembly of data: Rakibul M. Islam
Data analysis and interpretation: Rakibul M. Islam, Robin J. Bell, Baki Billah, Mohammad B. Hossain, Susan R. Davis
Manuscript writing: Rakibul M. Islam, Robin J. Bell, Susan R. Davis
Final approval of manuscript: Rakibul M. Islam, Robin J. Bell, Baki Billah, Mohammad B. Hossain, Susan R. Davis
Disclosures
Susan R. Davis: Trimel Pharmaceuticals Canada (C/A), Lawley Pharmaceuticals (RF), Abbott Australia, Pfizer Pharmaceuticals (H); Robin J. Bell: Lawley Pharmaceuticals (RF). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
References
- 1.Bruni L, Barrionuevo-Rosas L, Albero G, et al. ICO information centre on HPV and cancer (HPV information centre). Human papillomavirus and related diseases in Bangladesh. Summary Report 2015-03-20. Available at http://www.hpvcentre.net/statistics/reports/BGD.pdf. Accessed November 9, 2015.
- 2.Ferlay J, Shin HR, Bray F. GLOBOCAN 2008: Cancer incidence and mortality worldwide. IARC Cancer Base. No. 10. Lyon, France: IARC Press; 2010. [Google Scholar]
- 3.Bruni L, Barrionuevo-Rosas L, Albero G, et al. ICO information centre on HPV and cancer (HPV information centre). Human papillomavirus and related diseases in the world. Summary Report 2015-04-08. Available at http://www.hpvcentre.net/statistics/reports/XWX.pdf. Accessed November 9, 2015.
- 4.Basu P, Nessa A, Majid M, et al. Evaluation of the National Cervical Cancer Screening Programme of Bangladesh and the formulation of quality assurance guidelines. J Fam Plann Reprod Health Care. 2010;36:131–134. doi: 10.1783/147118910791749218. [DOI] [PubMed] [Google Scholar]
- 5.Nessa A, Hussain MA, Rashid MH, et al. Role of print and audiovisual media in cervical cancer prevention in Bangladesh. Asian Pac J Cancer Prev. 2013;14:3131–3137. doi: 10.7314/apjcp.2013.14.5.3131. [DOI] [PubMed] [Google Scholar]
- 6.Islam RM, Bell RJ, Hossain MB, et al. Bangladesh Midlife Women’s Health Study (BMWHS): Methods, challenges and experiences. Maturitas. 2015;80:89–94. doi: 10.1016/j.maturitas.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 7.Bangladesh Bureau of Statistics. Population and housing census 2011: Socio-economic and demographic report. Bangladesh Bureau of Statistics and Informatics Division, Ministry of Planning. Available at http://203.112.218.66/webtestapplication/userfiles/image/bbs/socio_economic.Pdf. Accessed December 10, 2014.
- 8.Bangladesh Bureau of Statistics. Monitoring the Situation of Vital Statistics of Bangladesh (MSVSB) Project Dhaka, Bangladesh: Bangladesh Bureau of Statistics, Statistics Division, Ministry of Planning, Government of the People's Republic of Bangladesh, 2011.
- 9. National Institute of Population Research and Training (NIPORT) MaA, and ICF International. Bangladesh Demographic and Health Survey 2011. Dhaka, Bangladesh and Calverton, MD: NIPORT, Mitra and Associates, and ICF International, 2013.
- 10.Rutsein SO, Johnson K. The DHS Wealth Index. DHS comparative reports no. 6. Available at http://dhsprogram.com/publications/publication-cr6-comparative-reports.cfm. Accessed November 7, 2015.
- 11.Cunningham MS, Skrastins E, Fitzpatrick R, et al. Cervical cancer screening and HPV vaccine acceptability among rural and urban women in Kilimanjaro Region, Tanzania. BMJ Open. 2015;5:e005828. doi: 10.1136/bmjopen-2014-005828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ansink AC, Tolhurst R, Haque R, et al. Cervical cancer in Bangladesh: Community perceptions of cervical cancer and cervical cancer screening. Trans R Soc Trop Med Hyg. 2008;102:499–505. doi: 10.1016/j.trstmh.2008.01.022. [DOI] [PubMed] [Google Scholar]
- 13.Chowdhury AMR, Bhuiya A, Chowdhury ME, et al. The Bangladesh paradox: Exceptional health achievement despite economic poverty. Lancet. 2013;382:1734–1745. doi: 10.1016/S0140-6736(13)62148-0. [DOI] [PubMed] [Google Scholar]
- 14.Dhamija S, Sehgal A, Luthra UK, et al. Factors associated with awareness and knowledge of cervical cancer in a community: Implication for health education programmes in developing countries. J R Soc Health. 1993;113:184–186. doi: 10.1177/146642409311300407. [DOI] [PubMed] [Google Scholar]
- 15.Nene B, Jayant K, Arrossi S, et al. Determinants of women’s participation in cervical cancer screening trial, Maharashtra, India. Bull World Health Organ. 2007;85:264–272. doi: 10.2471/BLT.06.031195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abdullahi A, Copping J, Kessel A, et al. Cervical screening: Perceptions and barriers to uptake among Somali women in Camden. Public Health. 2009;123:680–685. doi: 10.1016/j.puhe.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 17.Fang DM, Baker DL. Barriers and facilitators of cervical cancer screening among women of Hmong origin. J Health Care Poor Underserved. 2013;24:540–555. doi: 10.1353/hpu.2013.0067. [DOI] [PubMed] [Google Scholar]
- 18.Guimond ME, Salman K. Modesty matters: Cultural sensitivity and cervical cancer prevention in Muslim women in the United States. Nurs Womens Health. 2013;17:210–216. doi: 10.1111/1751-486X.12034. [DOI] [PubMed] [Google Scholar]
- 19.Lee MC. Knowledge, barriers, and motivators related to cervical cancer screening among Korean-American women. A focus group approach. Cancer Nurs. 2000;23:168–175. doi: 10.1097/00002820-200006000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Lesjak M, Ward J, Rissel C. Cervical screening of Arabic-speaking women in Australian general practice. J Med Screen. 1997;4:107–111. doi: 10.1177/096914139700400208. [DOI] [PubMed] [Google Scholar]
- 21.Matin M, LeBaron S. Attitudes toward cervical cancer screening among Muslim women: A pilot study. Women Health. 2004;39:63–77. doi: 10.1300/J013v39n03_05. [DOI] [PubMed] [Google Scholar]
- 22.Padela AI, Peek M, Johnson-Agbakwu CE, et al. Associations between religion-related factors and cervical cancer screening among Muslims in greater Chicago. J Low Genit Tract Dis. 2014;18:326–332. doi: 10.1097/LGT.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patel S. Muslim Americans reaching for health and building alliances (MARHABA): A study of breast and cervical cancer screening barriers and facilitators among Muslim women in New York city. Paper presented at: 142nd APHA Annual Meeting and Exposition, November 15-November 19, 2014; New Orleans, LA. [Google Scholar]
- 24.Gan DEH, Dahlui M. Cervical screening uptake and its predictors among rural women in Malaysia. Singapore Med J. 2013;54:163–168. doi: 10.11622/smedj.2013047. [DOI] [PubMed] [Google Scholar]
- 25.Gao W, Paterson J, DeSouza R, et al. Demographic predictors of cervical cancer screening in Chinese women in New Zealand. N Z Med J. 2008;121:8–17. [PubMed] [Google Scholar]
- 26.Perng P, Perng W, Ngoma T, et al. Promoters of and barriers to cervical cancer screening in a rural setting in Tanzania. Int J Gynaecol Obstet. 2013;123:221–225. doi: 10.1016/j.ijgo.2013.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ginsburg OM, Chowdhury M, Wu W, et al. An mHealth model to increase clinic attendance for breast symptoms in rural Bangladesh: Can bridging the digital divide help close the cancer divide? The Oncologist. 2014;19:177–185. doi: 10.1634/theoncologist.2013-0314. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.