Abstract
Objective:
To estimate the lifetime prevalence of trauma exposure and posttraumatic stress disorder (PTSD) among a representative, active military sample, and to identify demographic and military variables that modulate rates of trauma exposure as well as PTSD rates and duration.
Method:
A cross-sectional weighted sample of 5155 regular members and 3957 reservists (n = 8441) of the Canadian Armed Forces (CAF) was face-to-face interviewed using a lay-administered structured interview that generates Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, psychiatric diagnoses.
Results:
Within this sample, 85.6% reported 1 or more trauma exposure, with a median number of 3 or more exposures. Compared with males, females were less likely (P < 0.05) to be exposed to warlike trauma (adjusted odds ratio [AOR] 0.40), disasters (AOR 0.43), assaultive violence (AOR 0.52), and witnessing trauma (AOR 0.75). However, they were more likely to report sexual assault (AOR 7.36). The lifetime prevalence of PTSD was 6.6% and the conditional rate was 7.7%. Both lifetime and conditional PTSD rates were higher among female soldiers, but lower among the reserve forces, both male and female. Finally, the median duration of PTSD was negatively influenced by younger age of onset, but not influenced by whether the event occurred during deployment.
Conclusions:
Active members of the CAF report a high degree of trauma exposure but a moderate rate of lifetime PTSD.
Keywords: posttraumatic stress disorder, military, Canadians, epidemiology
Abstract
Objectif :
Estimer la prévalence de durée de vie de l’exposition aux traumatismes et du trouble de stress post-traumatique (TSPT) dans un échantillon représentatif de militaires actifs, et identifier les variables démographiques et militaires qui modulent les taux d’exposition aux traumatismes ainsi que les taux et la durée des TSPT.
Méthode :
Un échantillon transversal pondéré de 5155 membres réguliers et de 3957 réservistes (n = 8441) des Forces armées canadiennes (FAC) ont été interrogés en personne à l’aide d’une entrevue structurée administrée par des non-spécialistes qui permet de déceler des diagnostics psychiatriques du Manuel diagnostique et statistique des troubles mentaux, 4e édition.
Résultats :
Dans cet échantillon, 85,6 % ont déclaré une ou plusieurs expositions aux traumatismes, le nombre moyen étant 3 expositions ou plus. Comparé aux hommes, les femmes étaient moins susceptibles (P < 0,05) d’être exposées à des traumatismes de guerre (rapport de cotes corrigé [RCC] 0,40), à des désastres (RCC 0,43), à des agressions violentes (RCC 0,52), et à être témoins de traumatismes (RCC 0,75). Toutefois, elles étaient plus susceptibles de déclarer des agressions sexuelles (RCC 7,36). La prévalence de durée de vie du TSPT était de 6,6 % et le taux conditionnel était de 7,7 %. Les taux de TSPT de durée de vie et conditionnels étaient plus élevés chez les femmes militaires, mais plus faibles chez les réservistes, tant masculins que féminins. Enfin, la durée moyenne du TSPT était influencée négativement par le jeune âge à l’apparition du trouble, mais n’était pas influencée par le fait que l’événement soit survenu durant la mission ou pas.
Conclusions :
Les membres actifs des FAC déclarent un degré élevé d’exposition aux traumatismes mais un taux modéré de TSPT de durée de vie.
Posttraumatic stress disorder is an exposure-based disorder characterized by a constellation of symptoms that include re-experiencing, avoidance, negative cognitions and mood, and hyperarousal.1,2 The lifetime rates of trauma exposure have ranged from 55% in older research3 to 75% to 90% in more recent studies.4,5 The PTSD lifetime prevalence rates have ranged from 1% to 14% in community-based studies,1 and from 7% to 9% in large-scale epidemiologic surveys.3,5 Such variations can be attributed to differences in the populations studied, the type of methodology used, and the changes brought to the diagnostic criteria over the years. Despite such variations, PTSD consistently emerges as one of the most important public health problems in the field of mental health.2
According to some observers, the rates of trauma exposure and the lifetime prevalence of PTSD are expected to be higher in various at-risk populations, such as active military members.1 By the very nature of their profession, military members are at a greater risk of exposure to highly traumatogenic events, such as international peace-keeping missions or combat.6 Conversely, some studies, in particular in the United Kingdom, have argued for lower rates of PTSD within the military, compared with the general population,7,8 possibly owing to the effects of personnel selection, training, and postdeployment prophylactic interventions.
Within Canadian society, as in many others, much debate still exists9 as to whether there is more or less PTSD in the military, compared with civilian populations. Despite the existence of some large-scale studies examining trauma exposure and PTSD in veterans (for example, see Kulka et al10), and in specific cohorts of active military members,7,11 rates of trauma exposure and of PTSD within active armies of the world remain unknown. To our knowledge, the CCHS-CF, developed by Statistics Canada,12 is the first and only epidemiologic survey published so far of mental health conducted in a fully representative, active military sample. The existence of this data set in the public domain allowed us to estimate the lifetime prevalence of trauma exposure and PTSD among the Canadian military; to identify demographic and military variables that modulate those rates; and to identify factors that increase or decrease the duration of PTSD once it has developed.
Clinical Implications
This is the first epidemiologic study of trauma exposure and PTSD in a nationally representative and active military sample.
Our study may help determine service needs in the military.
Limitations
The cross-sectional nature of our study precludes drawing any conclusions on causality.
As is the case with all epidemiologic surveys conducted at the workplace, underestimation of lifetime prevalence rates cannot be ruled out, as it is possible that people with the most symptomatic PTSD have already left the CAF.
Methods
Participants and Procedure
The project for this paper was peer-reviewed by the Social Sciences and Humanities Research Council of Canada and by the Ethics committee of the Douglas Mental Health University Institute. Each participant’s written informed consent was obtained. Details of Cycle 1.2 of the CCHS-CF survey have been described elsewhere.12 The target population included all full-time regular CAF members (n = 57 000) and reservists (n = 24 000) at the time of the survey stratified by sex and rank. Within each stratum, the units were sorted by geographic region and CAF element (land, air, or sea), and the final sample was obtained using a systematic sampling scheme. Eighteen months later, after replacing out-of-scope units (that is, 713 regular members and 363 reservists no longer in the CAF), 6487 regular members and 3957 reservists were selected for a face-to-face interview between May 2002 and December 2002. A response was obtained for 5155 regular members (80%) and 3286 reservists (83%), resulting in a final sample of 8441. Demographic data for the full sample (regular and reserve forces combined) are shown in Table 1.
Table 1.
Demographic characteristics of CCHS-CF survey participants
| Variable | % | CV | 95% CI |
|---|---|---|---|
| Force | |||
| Regular | 70.9 | 0.1 | 70.7 to 71.1 |
| Reserve | 29.1 | 0.3 | 28.9 to 29.3 |
| Sex | |||
| Male | 85.3 | 0.1 | 85.1 to 85.5 |
| Female | 14.7 | 0.6 | 14.5 to 14.9 |
| Ethnicity | |||
| Caucasian | 93.5 | 0.3 | 92.9 to 94.1 |
| Non-Caucasian | 6.5 | 4.8 | 5.9 to 7.1 |
| Education | |||
| <Secondary | 8.3 | 4.5 | 7.6 to 9.0 |
| Secondary graduate | 29.3 | 1.9 | 28.2 to 30.4 |
| Some post-secondary | 40.9 | 1.5 | 39.8 to 42.1 |
| University certificate or bachelor | 16.8 | 2.0 | 16.1 to 17.4 |
| University master or doctorate | 4.6 | 3.7 | 4.3 to 5.0 |
| Marital status | |||
| Married or common law | 62.9 | 0.9 | 61.9 to 64.0 |
| Widowed, separated, or divorced | 7.4 | 4.3 | 6.8 to 8.0 |
| Single | 29.6 | 1.8 | 28.6 to 30.6 |
| Family income, Can$ | |||
| 0 to 19 999 | 2.9 | 8.0 | 2.4 to 3.3 |
| 20 000 to 39 999 | 8.2 | 4.5 | 7.5 to 8.9 |
| 40 000 to 59 999 | 25.6 | 2.2 | 24.5 to 26.7 |
| ≥60 000 | 61.5 | 1.0 | 60.3 to 62.6 |
| Age, years | |||
| 16 to 24 | 19.3 | 2.4 | 18.3 to 20.2 |
| 25 to 34 | 30.7 | 1.9 | 29.5 to 31.8 |
| 35 to 44 | 37.5 | 1.5 | 36.4 to 38.6 |
| ≥45 | 12.6 | 2.6 | 11.9 to 13.2 |
CV = coefficient of variation
Survey Instruments
The diagnostic assessment section of the CCHS-CF is based on the CIDI,13 a lay-administered psychiatric interview that generates diagnoses according to the DSMIV.1 The section included a screener for mental disorders and 7 additional sections: alcohol dependence, major depressive disorder, dysthymia, panic disorder, social phobia, generalized anxiety disorder, and PTSD. Interviews were conducted, face-to-face, by trained Statistics Canada interviewers in private on-base rooms. In a recent large-scale, epidemiologic survey, blind clinical re-interviews with the clinician-administered Structured Clinical Interview for DSM-IV14 were in good concordance with CIDI diagnoses for anxiety and mood diagnoses.15 For the PTSD section (lifetime diagnosis), respondents were given a booklet listing 28 potentially traumatic experiences and asked whether they had experienced any of them during their lifetime (an Appendix including these questions is available from the author). Respondents reporting several events were asked to pick the one that had caused the most reactions. Subsequent questions on trauma characteristics were assessed only for this index event. Based on data considerations and past research,16,17 we reduced the number of index event categories for some analyses. The nondiagnostic sections were based on sources used in other epidemiologic surveys conducted by Statistics Canada.
Data Analyses
Weighting
To produce estimates that are representative of the CAF population, a survey weight was created by Statistics Canada and applied to each respondent. This weight reflects 4 adjustments: the differential probabilities of selection in each of the 5 strata (for example, male–female and private– sergeant–officer); the reduction in the target sample size in the second phase of data collection owing to higher than estimated response rates in the first phase; the removal of people who were no longer CAF members during the data collection period (out-of-scope units); and the participants who could not be reached for an interview, provided unstable data, or refused to participate. All analyses are weighted using the final survey weight.
Statistical Analyses
All rates are reported in the form of prevalence. Adjusted odds ratios were obtained from multiple logistic regressions for the probability of having been exposed to a certain category of traumatic event adjusted for age, sex, ethnicity, marital status, education, income, geographic region, military force type, rank, and element. The time to remission from PTSD symptoms for the index event was obtained using the Kaplan–Meier analysis.18
As the CCHS-CF uses a complex sampling design, using the survey weight is appropriate only for calculating the point estimates of prevalence rates and odds ratios. To produce accurate variance estimates, the results obtained for point estimates were bootstrapped.19 Bootstrapping estimates the variance by generating a random sample with replacement from within the study sample and estimating variance from 500 such iterations. We used bootstrap data files and software that were prepared by Statistics Canada. Coefficient of variation of estimates was also produced. Data with a coefficient of variation greater than 33% were suppressed owing to extreme sampling variability. The analyses for the lifetime prevalence of trauma exposure and PTSD were conducted using SAS, version 9.0 (SAS Institute Inc, Cary, NC). Missing data were minimal (0.0% to 1.9%) and thus not imputed but rather removed. To create the Kaplan–Meier curves for the remission of PTSD, the method of balanced repeated replication implemented in SUDAAN was used. This method can produce bootstrap variance estimates when bootstrap weights are provided and designated to be balanced repeated replication weights. The log-rank test was used to test the homogeneity of survival curves for subgroups. As no software is available for applying weights in this test, the results for the log-rank test do not take into account the sample weights. To correct for this problem, we used a 2-sided P value of 0.01 to judge statistical significance for this test. Otherwise the P value was set at 0.05 (2-sided test).
Results
Lifetime Exposure to Traumatic Events
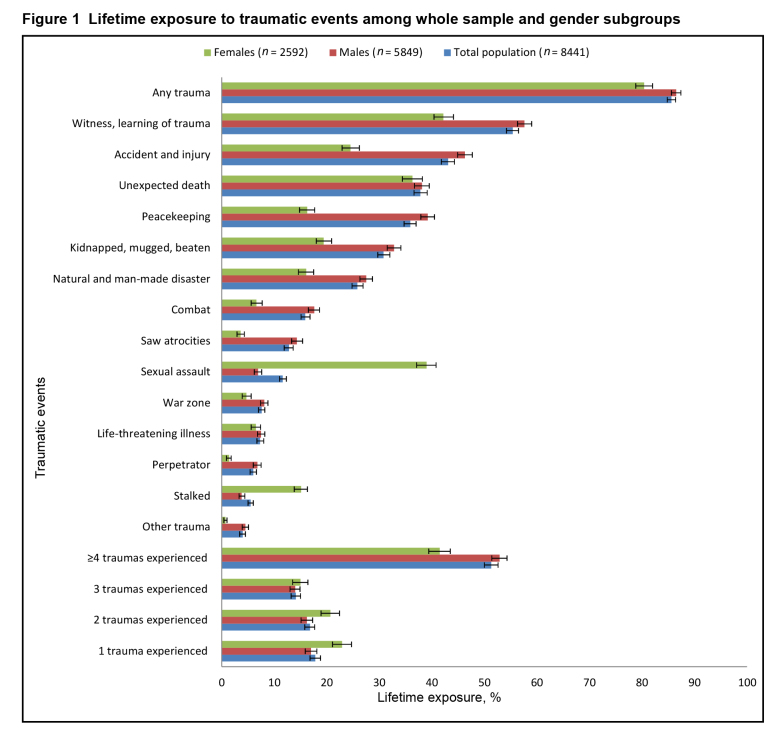
Among the whole sample, 85.6% (86.5% of the men and 80.4% of the women) reported exposure to at least one trauma exposure in their lifetime (Figure 1). The median number of exposures was 3 or more of such events. Collapsing the 28 trauma categories into the following 5 (not shown in Table 1), compared with men, women were significantly less likely (P < 0.05) to be exposed to warlike trauma (AOR 0.40, 95% CI 0.35 to 0.45), man-made or natural disasters (AOR 0.43, 95% CI 0.39 to 0.48), assaultive violence (AOR 0.52, 95% CI 0.46 to 0.59), and witnessing trauma (AOR 0.75, 95% CI 0.67 to 0.84). However, women were much more likely to be exposed to sexual assault (AOR 7.36, 95% CI 6.48 to 8.35).
Figure 1. Lifetime exposure to traumatic events among whole sample and gender subgroups.
Sociodemographic and Military Factors Associated With Lifetime Trauma Exposure
We explored the contribution of the sociodemographic and military factors listed in Table 1 on the odds of being exposed to trauma. Compared with Caucasians, non-Caucasians were more likely to be exposed to assaultive violence (AOR 1.30, 95% CI 1.03 to 1.65) and sexual assault (AOR 1.53, 95% CI 1.14 to 2.07). Compared with the regular forces, the reserve forces were less likely to be exposed to warlike trauma (AOR 0.33, 95% CI 0.28 to 0.38), man-made or natural disasters (AOR 0.75, 95% CI 0.67 to 0.85), assaultive violence (AOR 0.83, 95% CI 0.71 to 0.95), and witnessing trauma (AOR 0.62, 95% CI 0.54 to 0.70).
Compared with people serving in the Land forces, those serving in the Air or the Sea were less likely to be exposed to warlike trauma (AOR 0.31, 95% CI 0.26 to 0.36 and AOR 0.39, 95% CI 0.33 to 0.46, respectively), man-made or natural disasters (AOR 0.73, 95% CI 0.64 to 0.83 and AOR 0.72, 95% CI 0.63 to 0.83, respectively), assaultive violence (AOR 0.59, 95% CI 0.51 to 0.68 and AOR 0.76, 95% CI 0.64 to 0.89, respectively), and witnessing trauma (AOR 0.58, 95% CI 0.50 to 0.67 and AOR 0.61, 95% CI 0.52 to 0.70, respectively). Compared with officers, people within the lower ranks (for example, rank of private) were more likely to be exposed to warlike trauma (AOR 1.26, 95% CI 1.05 to 1.51), man-made or natural disasters (AOR 1.24, 95% CI 1.04 to 1.48), and assaultive violence (AOR 1.44, 95% CI 1.19 to 1.74).
Lifetime Prevalence of PTSD
As shown in Table 2, the lifetime prevalence of PTSD for the total sample was 6.6% (SE 0.3%). Once exposed to trauma, the conditional risk (that is, among people reporting trauma exposure) for PTSD for the total sample was 7.7% (SE 0.4%). The lifetime prevalence of PTSD was about twice as high for women than for men (11.6% and 5.7%). Women were also more than twice as likely as men to develop PTSD once exposed to trauma (14.5% and 6.6%). Also shown in Table 2, both the lifetime prevalence of PTSD and the conditional risk for PTSD were higher for regular than for reserve forces (7.3%, compared with 4.8% and 8.2%, compared with 6.2%, respectively).
Table 2.
Lifetime PTSD prevalence among the whole sample
| Variable | Total sample (N = 8347) | Trauma exposed (n = 7064) | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| % | CV | 95% CI | % | CV | 95% CI | |
| Lifetime PTSD | 6.6 | 4.7 | 6.0 to 7.2 | 7.7 | 4.7 | 7.0 to 8.4 |
| Force | ||||||
| Regular | 7.3 | 5.5 | 6.5 to 8.1 | 8.2 | 5.5 | 7.3 to 9.1 |
| Reserve | 4.8 | 8.4 | 4.0 to 5.6 | 6.2 | 8.3 | 5.2 to 7.2 |
| Sex | ||||||
| Male | 5.7 | 6.0 | 5.0 to 6.4 | 6.6 | 6.0 | 5.8 to 7.4 |
| Female | 11.6 | 5.5 | 10.4 to 12.9 | 14.5 | 5.4 | 13.0 to 16.0 |
| Ethnicity | ||||||
| Caucasian | 6.5 | 4.9 | 5.9 to 7.2 | 7.6 | 4.9 | 6.9 to 8.4 |
| Non-Caucasian | 7.1 | 16.1 | 4.9 to 9.4 | 8.3 | 16.1 | 5.7 to 10.9 |
| Education | ||||||
| <Secondary | 6.8 | 17.6 | 4.4 to 9.1 | 7.9 | 17.6 | 5.2 to 10.6 |
| Secondary graduate | 6.5 | 8.7 | 5.4 to 7.6 | 7.4 | 8.7 | 6.2 to 8.7 |
| Some post-secondary | 7.3 | 7.2 | 6.3 to 8.3 | 8.5 | 7.1 | 7.3 to 9.7 |
| University certificate or bachelor | 5.3 | 10.7 | 4.2 to 6.4 | 6.4 | 10.6 | 5.1 to 7.7 |
| University master or doctorate | 5.0 | 18.4 | 3.2 to 6.7 | 6.0 | 18.2 | 3.9 to 8.1 |
| Marital status | ||||||
| Married or common law | 6.3 | 6.1 | 5.5 to 7.0 | 7.0 | 6.1 | 6.2 to 7.9 |
| Widowed, separated, or divorced | 14.0 | 11.8 | 10.7 to 17.2 | 15.3 | 11.7 | 11.8 to 18.8 |
| Single | 5.4 | 9.1 | 4.4 to 6.3 | 7.0 | 9.1 | 5.7 to 8.2 |
| Family income, Can$ | ||||||
| 0 to 19 999 | 7.2 | 23.0 | 3.9 to 10.4 | 9.8 | 22.8 | 5.4 to 14.2 |
| 20 000 to 39 999 | 5.5 | 17.9 | 3.6 to 7.4 | 6.9 | 17.6 | 4.5 to 9.3 |
| 40 000 to 59 999 | 8.8 | 8.9 | 7.2 to 10.3 | 10.1 | 8.9 | 8.4 to 11.9 |
| ≥60 000 | 5.8 | 6.0 | 5.2 to 6.5 | 6.7 | 5.9 | 5.9 to 7.5 |
| Age, years | ||||||
| 16 to 24 | 4.1 | 13.2 | 3.0 to 5.2 | 5.6 | 13.2 | 4.2 to 7.1 |
| 25 to 34 | 6.9 | 9.0 | 5.7 to 8.1 | 8.1 | 9.0 | 6.7 to 9.5 |
| 35 to 44 | 7.8 | 6.8 | 6.7 to 8.8 | 8.5 | 6.8 | 7.4 to 9.6 |
| ≥45 | 5.9 | 12.0 | 4.5 to 7.3 | 6.7 | 11.9 | 5.1 to 8.2 |
CV = coefficient of variation
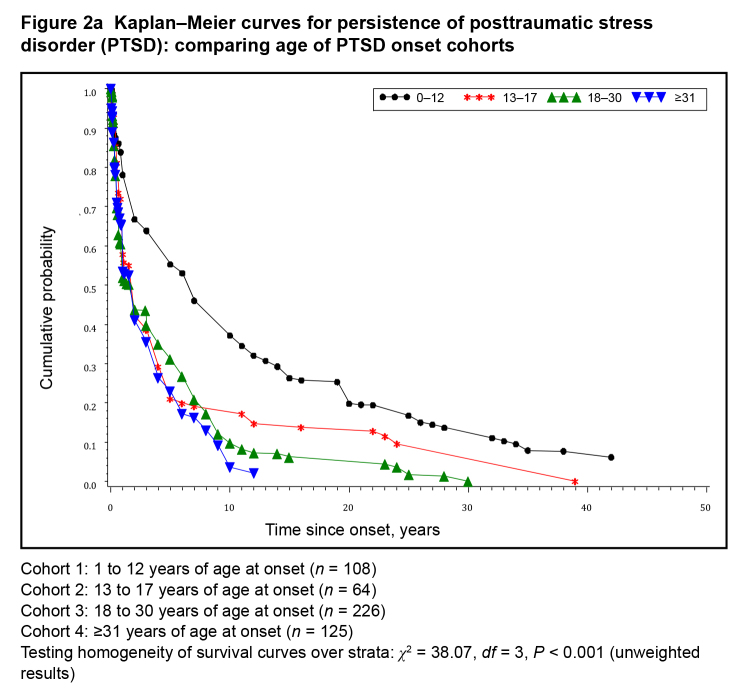
Duration of PTSD
Cumulative probability of PTSD persistence is reported in Figure 2a. The median duration for people whose symptoms started before age 13 was 6.5 years, which was much greater, compared with medians (1.5 years) for the other 3 age categories (13 to 17, 18 to 30, and 31 or older). Given that age of onset may be confounded by trauma type, we next examined the combined effects of age of onset and trauma type (during deployment, compared with not). Only CAF members whose age of onset was 18 or older were included in these analyses. The prevalence of PTSD caused by deployment-related trauma in military personnel 18 years and older was 2.33 (95% CI 1.95 to 2.72). As shown in Figure 2b, there is a visible trend whereby the shortest median durations (1.1 years) were observed for people whose symptoms were not related to deployment (regardless of age). People with deployment-related trauma whose age of onset was 18 to 30 years old, compared with 31 years and older, had a median duration of 1.7 years and 2.2 years, respectively.
Figure 2a. Kaplan–Meier curves for persistence of posttraumatic stress disorder (PTSD): comparing age of PTSD onset cohorts.
Cohort 1: 1 to 12 years of age at onset (n = 108)
Cohort 2: 13 to 17 years of age at onset (n = 64)
Cohort 3: 18 to 30 years of age at onset (n = 226)
Cohort 4: ≥31 years of age at onset (n = 125)
Testing homogeneity of survival curves over strata: χ2 = 38.07, df = 3, P < 0.001 (unweighted results)
Figure 2b.
Kaplan–Meier curves for posttraumatic stress disorder (PTSD) persistence according to deployment and age of PTSD onset
Cohort 1: deployment-unrelated trauma, age of onset: 18 to 30 (n = 117)
Cohort 2: deployment-unrelated trauma, age of onset: ≥31 (n = 57)
Cohort 3: deployment-related trauma, age of onset: 18 to 30 (n = 114)
Cohort 4: deployment-related trauma, age of onset: ≥31 (n = 69)
Testing homogeneity of survival curves over strata: χ2 = 6.58, df = 3, P = 0.09 (unweighted results)
Discussion
Prevalence of Trauma Exposure
The 85.6% rate of lifetime trauma exposure in this active Canadian military sample may appear high, but it is comparable with rates of 89.6% that have been reported in an American civilian sample.4 Still, it does appear somewhat higher than a rate of 76.1% recently reported in a Canadian civilian sample.6 The median number of exposures of 3 or more is in line with what others have found.4,5
Consistent with the civilian literature on sex differences in trauma exposure,3–5 we found that males had higher exposure rates for most trauma types; however, we found that females had a striking 39% exposure rate to sexual assault. This rate is higher than that reported in civilian studies.5 As questions regarding the timing and nature of the trauma experiences were limited to the worst event only in the CCHS-CF, the proportion of sexual assault experiences that took place while in military service, like any other noncombat-related trauma, cannot be determined. The finding that nearly 4 out of 10 women in this nationally representative active military sample experienced sexual assault highlights the importance of assessing this type of trauma in female military members and veterans in future studies. Future studies should explore what portion of these experiences took place after entry into military service. Note, past PTSD is an important risk factor for future PTSD.20,21
Prevalence of PTSD
Estimates of the lifetime prevalence of PTSD in this military sample, 6.6%, are, at first sight, remarkably close to the prevalence rates reported in recent civilian studies: 6.8%17 to 7.8%3 in the United States and 9.2% in Canada.5 This finding is somewhat contrary to the assumption that active military members may be at a greater risk for developing PTSD because of their professional experiences. It may be tempting to conclude that rates obtained in the CAF are not far off from those found in civilian samples and to conclude that serving in the military does not increase the lifetime risk of developing PTSD. However, doing so is not warranted for at least 2 very important reasons. First, regarding the previously reported Canadian PTSD rates,5 conditional lifetime prevalence was atypically calculated based on people who had suffered a traumatic event and had experienced symptoms of PTSD, and, as such, must be compared with other lifetime rates with caution. Therefore, the real lifetime PTSD rate in Canada remains unclear. Second, unlike civilian populations, in which those who develop the disorder remain in the sampling pool of prospective study participants, in samples of work-related trauma, those who develop a chronic and severe form of mental illness, such as PTSD, are likely to leave, or, in the case of the Canadian military’s universality of service policy, be asked to leave, their job after some time, and therefore are excluded, de facto, from the sampling pool. Thus it is likely that our study underestimates the rates of PTSD, as many of the people who developed chronic and severe mental illness were not included in this active military sample survey.22
Thus while the prevalence estimates presented are faithful representations of the lifetime PTSD rates for people in service at the time of the survey, the PTSD rate of those leaving the CAF every year remains unknown. Therefore, it is impossible with the available data to answer the question of whether CAF members report more trauma exposure and more PTSD than the Canadian population using prevalence estimates. In the future, past-year incidence estimates, rather than lifetime prevalence rates, could potentially yield a more reliable yardstick to compare civilian and military rates of mental health problems. Alternately, future studies should include active and retired military personnel to determine the lifetime PTSD rate associated with serving in the military.
Demographic Factors Affecting the Rate of PTSD
As found in other surveys,5,23 lifetime prevalence of PTSD was higher in women than in men. Rates of PTSD were higher in lower-rank military members, perhaps reflecting a higher likelihood of serving in the frontlines for military members of lower rank. Finally, the rates of PTSD were higher in the land element, compared with other military elements, likely because the land troops are more likely to be involved in direct combat, a traumatic event that has been consistently found to be highly traumatogenic.4
The Course of PTSD
Most active military members who developed PTSD in their lifetime experienced a chronic course of symptoms. The most enduring forms of the disorder were found for people whose symptoms started before they entered in the military forces, that is, in early childhood, with median symptom duration of 6, compared with 2, years for the other groups with an older onset. The figures also suggest that about one-half of the adult survivors of childhood PTSD no longer met the diagnostic criteria for the disorder when they entered the military. Because age and trauma type were confounded, we selected all the study participants whose PTSD onset was in adulthood and looked at the contribution of military deployment.
Among people exposed to a traumatic event in adulthood, there still was a trend for a younger age of PTSD onset to be associated with longer symptom duration. However, the most striking finding was that, in more than one-half of the military members with a lifetime PTSD diagnosis, the index trauma was not related to a military deployment. Further, deployment-related, compared with -unrelated, trauma exposure did not have different median PTSD symptom duration, suggesting a similar course and, by extension, a similar level of severity for both types of trauma. Although the CAF have been mostly involved in peace-building or -keeping missions since World War II, note that, according to a recent study, the level of trauma exposure among a sample of Canadian veterans seeking treatment for PTSD, compared with that of their American counterparts, peacekeepers’ have similar PTSD rates than soldiers and suffer from the same social functioning problems.24,25 In peacekeepers, the rates of PTSD vary from 3% to 20%.26–29
Strengths, Limitations, and Future Directions
To our knowledge, the CCHS-CF is the first epidemiologic study of trauma exposure and PTSD in a nationally representative, active military sample. Past research on trauma exposure and PTSD in the military have been limited to select troops that have served in specific military operations,30 limiting generalizability of findings to other troops that may have served in vastly different military operations. The CCHS-CF used methodology that is similar to that used in epidemiologic surveys of trauma exposure and PTSD in civilians (for examples, see Kessler et al3,17). Despite that, for reasons explained above, the findings should not be directly compared with those from civilian studies.
Future analyses of the CCHS-CF 2012 data will include post-Afghanistan war experiences that will require similar research attention, as a higher exposure to military operations and combat may elicit additional aspects of the impact on mental health of the CAF members.31 Future research should also consider comorbidity of other mental disorders, such as alcohol abuse, anxiety disorders, and depression, which may factor into the duration and sex differences demonstrated in these findings.
The CCHS-CF also had numerous limitations that should be considered in interpreting the results. First, the cross-sectional nature of the survey precludes drawing any conclusions on causality. Longitudinal studies are needed to determine whether the associations observed between demographic and military factors and likelihood of exposure to specific types of traumatic events are causal. Finally, as has been discussed elsewhere,17 age at interview and age-related failure to recall the exact timing of symptoms may have limited the accuracy of the age of onset data, which were used in analyses examining the chronicity of symptoms.
Conclusion
Findings from our epidemiologic survey of mental health conducted in a fully representative, active military sample found that active members of the CAF report a high degree of trauma exposure but a moderate rate of lifetime PTSD. Rates of PTSD were higher in women, in lower-rank military members, and in the land element, compared with other military elements. Chronicity of PTSD symptomology was associated with younger age of PTSD onset, even among people exposed to a traumatic event in adulthood.
The rate of sexual trauma among female military members was very high. Echoing other studies, the index trauma was not related to a military deployment in more than one-half of female and male military members with lifetime PTSD diagnosis and deployment-related trauma demonstrated a similar course to unrelated trauma exposure.
Acknowledgments
This work was supported in part by Veterans Affairs Canada, by the Social Sciences and Humanities Research Council, and by Statistics Canada. Dr Fikretoglu acknowledges a post-doctoral salary award from the Canadian Institute of Health Research while working on this manuscript. Dr Brunet acknowledges a salary award from the Fonds de recherche en santé du Québec while working on this manuscript. The authors thank Mark Zamorski for his consultation during the editing phase for the manuscript.
Abbreviations
- CCHS-CF
Canadian Community Health Survey—Canadian Forces Supplement
- CAF
Canadian Armed Forces
- CIDI
Composite International Diagnostic Interview
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- PTSD
posttraumatic stress disorder
References
- 1.American Psychological Association (APA) Diagnostic and statistical manual of mental disorders. 4th ed. Washington (DC): APA; 2000. Text revision. [Google Scholar]
- 2.American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders. 5th ed. Arlington (VA): APA; 2013. [Google Scholar]
- 3.Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 4.Breslau N, Kessler RC, Chilcoat HD, et al. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55(7):626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- 5.Van Ameringen M, Mancini C, Patterson B, et al. Post-traumatic stress disorder in Canada. CNS Neurosci Ther. 2008;14(3):171–181. doi: 10.1111/j.1755-5949.2008.00049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Breslau N, Davis GC, Andreski P, et al. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry. 1991;48(3):216–222. doi: 10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- 7.Fear NT, Jones M, Murphy D, et al. What are the consequences of deployment to Iraq and Afghanistan on the mental health of the UK armed forces? A cohort study. Lancet. 2010;375(9728):1783–1797. doi: 10.1016/S0140-6736(10)60672-1. [DOI] [PubMed] [Google Scholar]
- 8.Rona RJ, Hooper R, Jones M, et al. Mental health screening in armed forces before the Iraq war and prevention of subsequent psychological morbidity: follow-up study. BMJ. 2006;333(7576):991. doi: 10.1136/bmj.38985.610949.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bernier M. Ottawa (ON):: Standing Committee on National Defence, House of Commons Canada; 2009. Doing well and doing better: health services provided to Canadian Forces personnel with an emphasis on post-traumatic stress disorder [Internet] [cited 2013 Oct 25]. Available from: http://veteranvoice.info/ARCHIVE/info_09JunDND%20PTSD%20Report%20_eng.pdf. [Google Scholar]
- 10.Kulka RA, Schlenger WE, Fairbank JA, et al., editors. Trauma and the Vietnam War generation: report of findings from the National Vietnam Veterans Readjustment Study. New York (NY): Brunner– Mazel; 1990. [Google Scholar]
- 11.Gray GC, Chesbrough KB, Ryan MA, et al. The Millennium Cohort Study: a 21-year prospective cohort study of 140,000 military personnel. Mil Med. 2002;167(6):483–488. [PubMed] [Google Scholar]
- 12.Statistics Canada . Statistics Canada; 2003. Canadian Community Health Survey—mental health and well-being—Canadian Forces (CCHS-CF) [Internet] [cited 2013 Oct 25]. Available from: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SurvId=27305&SurvVer=1&SDDS=5084&InstaId=27306&InstaVer=1&lang=en&db=imdb&adm=8&dis=2#a3. [Google Scholar]
- 13.World Health Organization (WHO) Composite International Diagnostic Interview. Version 2.1. Geneva (CH): WHO; 1997. [Google Scholar]
- 14.First M, Spitzer R, Gibbon M, et al. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition (SCID-I/NP) New York (NY): Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 15.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 16.Breslau N, Kessler RC, Chilcoat HD, et al. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55(7):626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- 17.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 18.Kaplan PMEL. Nonparametric estimation from incomplete observations. J Am Statist Assoc. 1958;53(282):457–481. [Google Scholar]
- 19.Efron B, Tibshirani RJ. An introduction to the bootstrap. New York (NY): Chapman & Hall; 1994. [Google Scholar]
- 20.Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68(5):748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- 21.Ozer EJ, Best SR, Lipsey TL, et al. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull. 2003;129(1):52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- 22.Brunet A, Monson E. Suicide risk among active and retired Canadian soldiers: the role of posttraumatic stress disorder. Can J Psychiatry. 2014;59(9):457–459. doi: 10.1177/070674371405900901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sareen J. Posttraumatic stress disorder in adults: impact, comorbidity, risk factors, and treatment. Can J Psychiatry. 2014;59(9):460–467. doi: 10.1177/070674371405900902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Richardson JD, Elhai JD, Pedlar DJ. Association of PTSD and depression with medical and specialist care utilization in modern peacekeeping veterans in Canada with health-related disabilities. J Clin Psychiatry. 2006;67(8):1240–1245. doi: 10.4088/jcp.v67n0810. [DOI] [PubMed] [Google Scholar]
- 25.Fikretoglu D, Brunet A, Poundja J, et al. Validation of the deployment risk and resilience inventory in French-Canadian veterans: findings on the relation between deployment experiences and postdeployment health. Can J Psychiatry. 2006;51(12):755–763. doi: 10.1177/070674370605101205. [DOI] [PubMed] [Google Scholar]
- 26.Deahl M, Srinivasan M, Jones N, et al. Preventing psychological trauma in soldiers: the role of operational stress training and psychological debriefing. Br J Med Psychol. 2000;73(1):77–85. doi: 10.1348/000711200160318. [DOI] [PubMed] [Google Scholar]
- 27.Gibson RM. [Calgary (AB)]: University of Calgary; 1997. The development of the Canadian Deployment Impact Scale for assessing PTSD: a psychometric study. [dissertation] [Google Scholar]
- 28.Litz BT, Orsillo SM, Friedman M, et al. Posttraumatic stress disorder associated with peacekeeping duty in Somalia for US military personnel. Am J Psychiatry. 1997;154(2):178–184. doi: 10.1176/ajp.154.2.178. [DOI] [PubMed] [Google Scholar]
- 29.MacDonald C, Chamberlain K, Long N, et al. Mental health, physical health, and stressors reported by New Zealand Defense Force peacekeepers: a longitudinal study. Mil Med. 1998;163(7):477–481. [PubMed] [Google Scholar]
- 30.Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 31.Hines LA, Sundin J, Rona RJ, et al. Posttraumatic stress disorder post Iraq and Afghanistan: prevalence among military subgroups. Can J Psychiatry. 2014;59(9):468–479. doi: 10.1177/070674371405900903. [DOI] [PMC free article] [PubMed] [Google Scholar]