Abstract
Objective:
Outcome measures are rarely available for surveillance and system performance monitoring for mental disorders and addictions. Our study aims to demonstrate the feasibility and face validity of routinely measuring the mortality gap in the Canadian context at the provincial and regional levels using the methods and data available to the Canadian Chronic Disease Surveillance System (CCDSS) of the Public Health Agency of Canada.
Methods:
We used longitudinal data from the Quebec Integrated Chronic Disease Surveillance System, which also provides aggregated data to the CCDSS. This includes data from the health insurance registry physician claims and the hospital discharge abstract for all mental disorder diagnoses (International Classification of Diseases [ICD]-9 290–319 or ICD-10 F00–F99). Patients were defined as having had received a mental disorder diagnosis at least once during the year. Life expectancy was measured using Chiang’s method for abridged life tables, complemented by the Hsieh method for adjustment of the last age interval.
Results:
We found a lower life expectancy among psychiatric patients of 8 years for men and 5 years for women. For patients with schizophrenia, life expectancy was lowered by 12 years for men and 8 years for women. Cardiovascular disease and cancer were the most common causes of premature death. Findings were consistent across time and regions of the province. Lower estimates of the mortality gap, compared with literature, could be explained by the inclusion of primary care patients and methods.
Conclusions:
Our study demonstrates the feasibility of using administrative data to measure the impact of current and future mental health plans in Canada provided the techniques can be replicated in other Canadian provinces.
Keywords: mortality, mentally ill people, surveillance and system performance indicators
Abstract
Objectif :
Les mesures des résultats sont rarement disponibles pour le rendement de la surveillance et du système contrôlant les maladies mentales et les dépendances. Notre étude vise à démontrer la faisabilité et la validité apparente de mesurer couramment les disparités de mortalité dans le contexte canadien à l’échelle provinciale et régionale, à l’aide des méthodes et des données offertes par le Système national de surveillance des maladies chroniques (SNSMC) de l’Agence de la santé publique du Canada.
Méthodes :
Nous avons utilisé des données longitudinales du Système intégré de surveillance des maladies chroniques du Québec, qui fournit aussi des données cumulatives au SNSMC. Ceci comprend des données de facturation des médecins du registre de l’assurance maladie et des sommaires des congés d’hôpitaux pour tous les diagnostics de trouble mental (Classification internationale des maladies [CIM]-9 290–319 ou CIM-10 F00–F99). Les patients ont été définis comme ayant reçu un diagnostic de trouble mental au moins une fois durant l’année. L’espérance de vie a été mesurée à l’aide de la méthode de Chiang pour les tables de mortalité abrégées, complétée par la méthode de Hsieh pour ajustement du dernier intervalle d’âge.
Résultats :
Nous avons constaté chez les patients psychiatriques une espérance de vie moins élevée de 8 ans pour les hommes et de 5 ans pour les femmes. Pour les patients souffrant de schizophrénie, l’espérance de vie était moins élevée de 12 ans pour les hommes et de 8 ans pour les femmes. La maladie cardiovasculaire et le cancer étaient les causes les plus communes de décès prématuré. Les résultats étaient cohérents à travers le temps et les régions de la province. Les estimations moins élevées des disparités de mortalité, comparativement à la littérature, pourraient s’expliquer par l’inclusion des patients et des méthodes des soins primaires.
Conclusions :
Notre étude démontre la faisabilité d’utiliser des données administratives pour mesurer l’impact des plans de santé mentale présents et futurs au Canada, si les techniques peuvent être reproduites dans d’autres provinces canadiennes
Although first identified 20 years ago, the excess mortality observed in people with mental illness has not abated. If anything, the mortality gap has increased in the past decade, especially for CVDs.1–3 The difference is greatest for patients in contact with specialist care and for those with organic brain syndromes, substance disorders, or psychoses,2 the latter group dying about 20 years earlier than their mentally well counterparts.4 Chronic physical disorders, such as CVD and cancer, are the main causes, accounting for 85% of preventable mortality, compared with 15% accounted for by suicide, yet chronic physical disorders receive far less attention.5 Reasons for increased chronic disorders and unfavourable consequences include socioeconomic disadvantages, medication side effects, health habits (for example, smoking), and reduced access to physical health care.6 Psychiatric patients have not benefited from preventive measures that have reduced the impact of chronic disorders, such as CVD, in the general population. As a result, while mortality rates from ischemic heart disease have fallen in the last 20 years, they have increased in psychiatric patients, leading to a growing disparity in outcomes.2,7 The latter may also be related to diagnostic overshadowing; that is, symptoms and signs of urgent medical attention being overlooked as part of illness behaviour or owing to time pressure in primary and specialist medical care toward people with chronic diseases and mental disorders.8
Clinical Implications
Our results confirm the substantial impact of mental illness on mortality.
The most common causes of death mirror those in the general population: CVDs, respiratory diseases, and cancers.
Because of the complex, multi-factorial nature of these conditions, multi-pronged approaches, both individual- and population-based, will be required to address these inequalities.
Limitations
The cross-sectional method was used to calculate life expectancy.
Administrative data may also be subject to recording bias, especially for diagnosis.
The CCDSS psychiatric case definition differs from those for other disorders by stipulating that a person must attend for treatment in the current year to be considered a prevalent case in that year.
In the United Kingdom, Thornicroft9 highlighted the need for a public health approach to this problem, using the mortality gap as an easy-to-grasp indicator of system improvement. The MHCC called for similar performance indicators across provinces.10 One approach is the use of administrative data in the surveillance of changes in the mortality gap and the effect of interventions at clinical, programmatic, and system levels.11
Surveillance refers to the ongoing, systematic use of such data to identify associations and predictors of health outcomes. Surveillance was originally applied to communicable diseases but is increasingly being extended to mental illness, diabetes, arthritis, cancer, as well as circulatory and other diseases. For instance, standard case definitions for the surveillance of diabetes have been adopted by the CCDSS, a collaborative network of provincial and territorial surveillance systems supported by the PHAC.12 It produces indicators, including mortality indicators. This system is being extended to psychiatric disorders, with the first national report recently published,13 based on feasibility studies conducted in some provinces.14,15 In Quebec, the INSPQ has applied the diagnostic definitions from these feasibility studies for the surveillance of mental disorders, excess mortality, and service use.16,17
An advantage of the CCDSS is the inclusion of primary care where most people with chronic diseases, such as diabetes and mental disorders, are treated. Studies that have used administrative data from elsewhere, such as Italy, Sweden, and the United States, have been restricted to patients attending psychiatric services and thus may not reflect the mortality experience of most people with psychiatric problems.18–20 Therefore, the absolute figures of the mortality gap may vary because of the population covered, but also the very methods that are applied.
Our study aims to demonstrate the feasibility and face validity of routinely measuring the mortality gap for mental disorders in the Canadian context at the provincial and regional levels, using the methods and data available to the CCDSS of the PHAC and building on the surveillance activities of the INSPQ and its integrated chronic disease surveillance system.
Methods
Data Sources
We used the resources of the public health agency of Quebec (INSPQ).17 Estimates were produced using linked administrative databases from the physician billing agency (Régie de l’assurance maladie du Québec) and the Quebec Ministry of Health and Social Services, which together make up the QICDSS. About 99% of Quebec’s 7.5 million residents were registered with health insurance in 2006. We used the following databases: the Health Insurance Registry, the physician billing database, the hospitalization database, and the Vital Statistics Death Database. Causes of death for the mortality study were extracted from the death database. The ninth or tenth revisions of the ICD were used for coding diagnoses.
Case Definition and Measure of Prevalence
We used the case definition for psychiatric disorders chosen by the CCDSS for use in administrative databases and for which there are validated case definitions14,15,21; that is, any contact with a health service with an ICD-9 diagnosis of 290–319 or ICD-10 equivalent. Within this group, we defined 2 further categories: mood and anxiety disorders (296, 300, 311 in ICD-9 and F30–F48 and F68 in ICD-10) and schizophrenic disorders (295 in ICD-9 and F20, F21, F23.2, and F25 in ICD-10). The former also represents common mental disorders, while the latter epitomizes SMDs.
We were interested in measuring treated prevalence, which meant that a person had to meet the case definition in a given year to be considered as a prevalent case for that specific year. Each disease category was analyzed separately, which meant that a person, who, for example, had received a diagnosis of both a mood disorder and schizophrenia was counted in both categories.
Period Covered, Temporal and Regional Comparisons
Estimates were obtained through population-based longitudinal follow-up. The analysis period began on April 1, 1999, and ended on March 31, 2012. Comparisons over time and between regions were made using age-adjusted measures. These were directly standardized to the age structure of the population of Quebec in 2001.
Definition of Excess Mortality and Measure of Life Expectancy
Abridged life tables using Chiang’s method were used to calculate the life expectancies of people with mental disorders by 5-year age groups: 1 to 4 years, 5 to 9 years, and so on to 80 to 84 years and 85 years and older.22 An abridged life table is a compilation of the death rate for each age interval and, for people who died during the age interval, the average fraction of life in the interval. The Hsieh method was used to adjust the average fraction of life in the last interval of the table.23 From these 2 measurements, we calculated the probability of death in the interval by comparing the number of people living at the beginning of the interval with the number of people living at the end of the interval. From this, we derived a life expectancy, which was calculated during an 11-year period for a more robust estimate of mortality.
Excess mortality rates, overall and stratified by leading causes of death, were calculated using risk ratios of age-standardized mortality rates. Patients were defined based on current status in a given year.
Results
Prevalence of Mental Disorders
On average, mental disorders were diagnosed among 12% of the population annually. This represented a total of 903 000 people from 2009 to 2010.16 The age-standardized treated prevalence and the number of patients by sex in Quebec from 2009 to 2010 for all mental disorders were as follows: women: 518 624 (12.7%), men: 381 902 (9.9%); for anxiodepressive disorders: women: 369 261 (9.1%), men: 211 165 (5.4%); for schizophrenic disorders: women: 14 242 (0.35%), men: 19 418 (0.50%).
The prevalence of diagnosed mood and anxiety disorders and schizophrenic disorders varied little from 1999–2000 to 2009–2010.16 More than 70% of patients with mood and anxiety disorders were only identified and seen by GPs, while 75% of patients with schizophrenic disorders were in contact with specialist services, as well as GPs.16
Mortality Associated With Mental Disorders
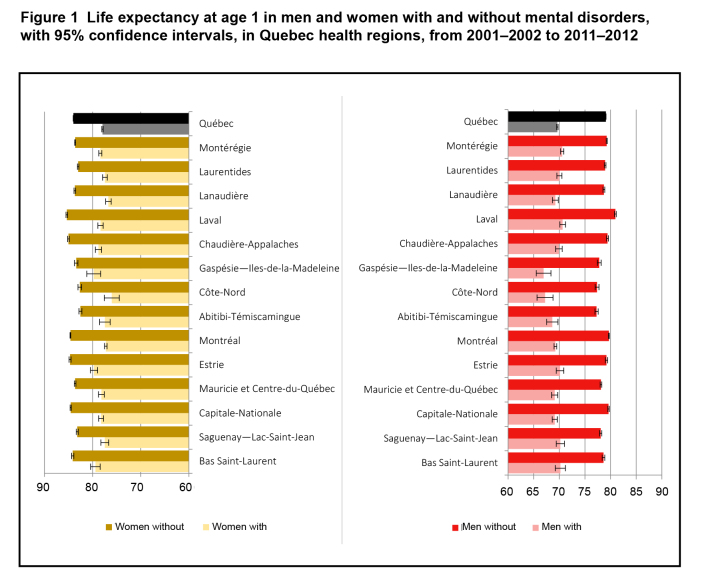
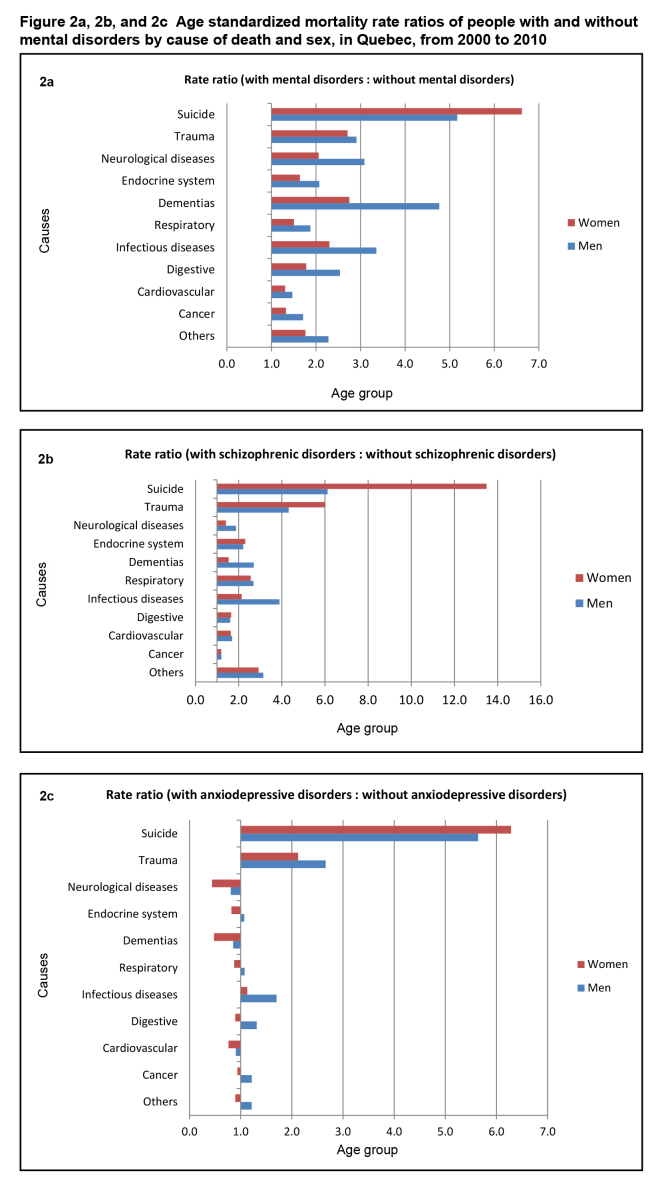
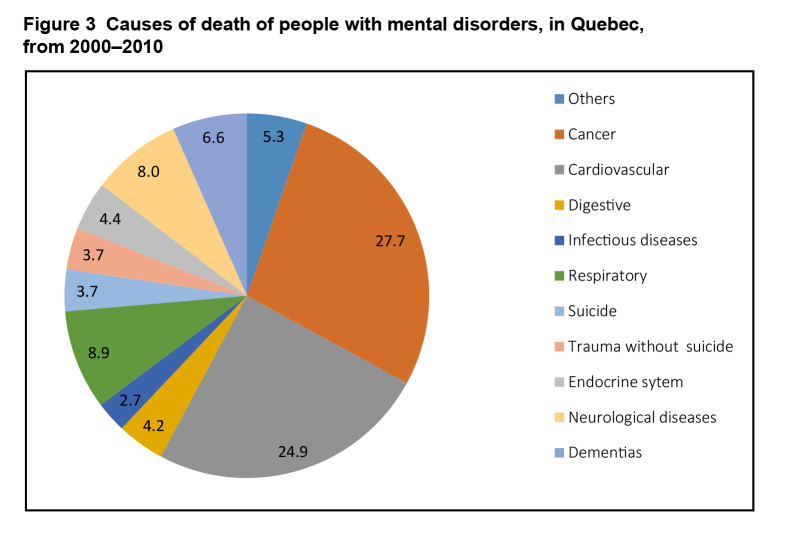
Figure 1 compares the various regions of Quebec. Life expectancy was lowest for people with mental illnesses, although the exact extent varied by region. This included small regions of less than 100 000 inhabitants, where 95% confidence intervals were widest. Differences in life expectancy between the general population of Quebec and people with mental disorders were calculated by sex (Table 1). For men with mental disorders, life expectancy was 8 years lower than for the general population (70 and 78 years, respectively). The difference was 4 years for men with mood and anxiety disorders (life expectancy = 74 years), and 12 years for those with schizophrenic disorders (life expectancy = 66 years). The life expectancy of women with mental health disorders was 5 years lower than for the general population (78 and 83 years, respectively). Among women with schizophrenic disorders, the life expectancy was reduced by 10 years (life expectancy = 73 years). As some disorders, such as schizophrenia, occur in young adults, analyses were repeated for life expectancy at age 20, with similar findings for mental disorders in general, for anxiety and depression and for schizophrenia. A separate analysis for people who had been psychiatric inpatients indicated a greater mortality gap, with a life expectancy of 65 years for females (95% CI 63 to 67 years) and 59 for males, (95% CI 57 to 60 years), a gap of 18 and 19 years, respectively. Compared with the general population, mortality rate ratios for mental disorders were higher for all causes of death, with suicide and dementia having the greatest differences. The pattern was similar when the analyses were restricted to patients with SMDs, such as schizophrenia (Figures 2a and 2b). People with mood and anxiety disorders had similar increases in suicide and trauma, but a more ambiguous pattern for other causes of death (Figure 2c). However, in absolute terms, CVDs and cancers were the main causes of death for people with mental disorders (Figure 3).
Figure 1. Life expectancy at age 1 in men and women with and without mental disorders, with 95% confidence intervals, in Quebec health regions, from 2001–2002 to 2011–2012.
Table 1.
Life expectancy at age 1 in the general population and in people with mental disorders by sex, in Quebec, from 2001–2002 to 2011–2012
| Population and disease status | Life expectancy, years | |
|---|---|---|
|
| ||
| Women | Men | |
| General population | 82.8 | 77.7 |
| Mental disorders | 77.9 | 69.6 |
| Mood and anxiety disorders | 83.8 | 73.5 |
| Schizophrenic disorders | 72.6 | 65.5 |
Figure 2a, 2b, and 2c. Age standardized mortality rate ratios of people with and without mental disorders by cause of death and sex, in Quebec, from 2000 to 2010.
Figure 3. Causes of death of people with mental disorders, in Quebec, from 2000–2010.
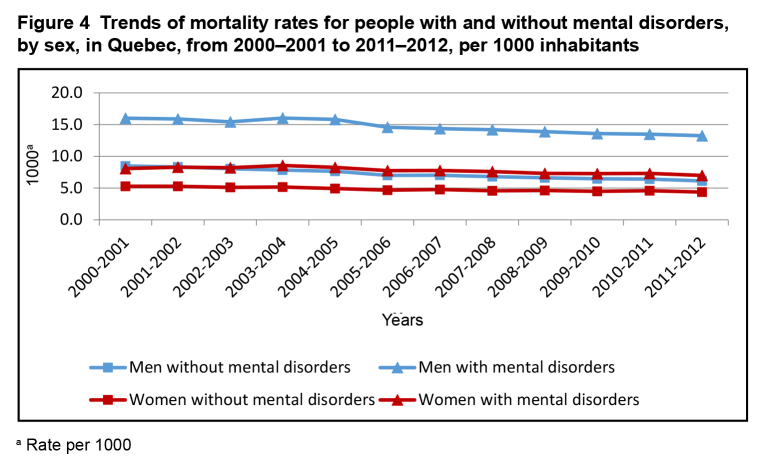
An analysis of age standardized mortality rates by sex during the past decade showed little variation by sex over time, suggesting that our estimates of mortality in psychiatric patients were stable (Figure 4).
Figure 4. Trends of mortality rates for people with and without mental disorders, by sex, in Quebec, from 2000–2001 to 2011–2012, per 1000 inhabitants.
a Rate per 1000
Interpretation
Our study demonstrates the feasibility of using health administrative data for the surveillance of excess mortality in patients with severe and common mental disorders in the Canadian context. The methods seem robust across mental disorders, across regions, and over time.
Our findings emphasize that chronic medical illnesses, such as CVDs and cancer, are the most common causes of preventable deaths and reduced life expectancy in psychiatric patients. Unlike other work from the United Kingdom, Sweden, and the United States, our study is not restricted to patients of specialist psychiatric services but includes all people with a treated psychiatric disorder, irrespective of setting, including primary care. This reduces referral or selection bias, as most patients receive psychiatric treatment from GPs. The only other work that included primary care was a 2005 cross-sectional study from Nova Scotia.24 However, this work did not use the CCDSS definition of mental disorders and did not report life expectancy, a metric better understood by decision makers and the public. The study also did not include data covering a period of 10 years.
Our results confirm the excess mortality of people with mental disorders, especially those with the most SMDs, such as schizophrenia. However, the reduction in life expectancy in our study is less marked than in patients of specialist mental health services in the United States, Sweden, or Australia.5,18,20,25 One explanation, mentioned previously, is that we included all patients receiving psychiatric care, such as those of family physicians and specialists, outside the formal psychiatric care system. This explanation is consistent with our own finding that the life expectancy of people who had required inpatient treatment was significantly worse. Another explanation is that the Canada Health Act ensures greater equity than exists in other countries, even though discrimination can still occur.26
Similar to some other studies of mood and anxiety disorders, we did not find an increased mortality risk for CVD and cancer disorders in women.27 This may again be related to the inclusion of primary care attenders or to greater help seeking behaviour by women with mood and anxiety disorders in general, thus enabling earlier detection and treatment of comorbid common chronic diseases. Nevertheless, considering the association between depression and diabetes or other chronic diseases in primary care in both sexes, one would expect some reduction in life expectancy.28,29 Longer-term and larger-cohort studies may reveal significant decreases in life expectancy among women, even though this is lower than in men.
Methodological Limitations
The QICDSS databases only cover people in treatment, and one-off surveys have shown that only 40% of Canadians with a self-reported mental disorder seek services for their mental health.30 However, given that the QICDSS covers 97% of all insured people, who in turn represent 99% of the Quebec population, and that our study extends over 10 years, this would minimize the likelihood of missing any person in the population who received a mental disorder diagnosis.17 In addition, one-off surveys can underestimate the treated prevalence by one-half. For example, 1 study that used the equivalent of the QICDSS databases but also took into account procedure codes for talk therapies estimated that, each year, 75% of the expected 1-in-5 people with a mental disorder was identified by GPs.31 In the case of schizophrenia, the QICDSS yearly prevalence was comparable with the median found in the meta-analysis of Saha et al.32
The cross-sectional method was used to calculate life expectancy. This is the life expectancy we would obtain if a person aged 1 was subjected throughout their life to the same age-specific mortalities prevailing in the study period. For the subcategory we refer to as having a mental disorder, we assume that its life course mortality is equivalent to that of mortality levels observed for each age group during our study period. Therefore, caution is needed when interpreting it as a life expectancy at age 1 for people identified with mental disorders. In fact, the measure represents the mean number of years left to live beyond the age of 1 for people subjected to the mortality conditions of active treated cases of mental disorders during the study period.
Administrative data may also be subject to recording bias, especially for diagnosis. Although 95% of billing claims made by psychiatrists in Quebec include a diagnosis,17 evidence from Ontario suggests that accuracy is lower for substance abuse and disorders other than psychoses.33 Elsewhere, a study34 from Saskatchewan comparing anxiety or mood disorder diagnoses and the prescription of antidepressants reported a sensitivity of 84% and a specificity of 90%. Therefore, we have emphasized overall psychiatric morbidity, or large categories validated in previous feasibility studies in some Canadian provinces including Quebec,14,15,21 to minimize possible bias. In terms of mortality, concordance between the vital statistics death database and the physician billings database improved from 95% to 98% between 1996 and 2009.17
The CCDSS psychiatric case definition differs from those for other disorders by stipulating that a person must attend for treatment in the current year to be considered a prevalent case in that year. In the case of diabetes and hypertension, a case is considered to be active until the end of the study period, death, or emigration.12,35 Hence deaths of people who have been diagnosed with mental disorders in the past but have had no diagnosis in the current year were classified as not having mental disorders. The impact of these people on the measurement of excess mortality is impossible to determine, as we do not know the current state of their unobserved mental health.
The lack of information in administrative data on services delivered outside the province can also be a limitation for interregional comparisons. For Quebec, these include areas bordering Ontario or New Brunswick, where part of the population receives medical care in the adjoining province.
Implications
Our results show the substantial impact of mental illness on mortality. Unlike one-off surveys, they present a longitudinal picture and thus the ability to evaluate the effect of future interventions on the excess mortality faced by psychiatric patients. The most common causes of death mirror those in the general population: CVDs, respiratory diseases, and cancers.
Because of the complex, multi-factorial nature of these conditions, multi-pronged approaches will be required to address these inequalities, in the same way that multi-pronged approaches have been used to reduce the mortality associated with these common conditions in the general population. These strategies should include both individual- and population-based components.
In terms of subcategories of psychiatric patients, the greater all-cause mortality in schizophrenia may suggest discrimination in access to the prevention and treatment of chronic diseases, and the need to integrate primary and specialist care in the case management and rehabilitation of patients who are severely mentally ill.2,26 This might include training modules for GPs concerning chronic disease comorbidities, taking into account diagnostic overshadowing and stigma.9 By contrast, the increased rates of suicide and trauma in mood disorders may suggest the need for population-based suicide prevention strategies and improved access to psychiatric treatment.36,37
We believe that mental health surveillance will help prompt action to improve outcomes at various levels. At a systems level, for instance, indicators on diabetes from the CCDSS have informed recommendations for system and practice improvement.38,39 Similar projects could easily integrate mental disorder indicators. For example, mental health indicators produced by the PHAC could inform the work of national commissions, such as the MHCC.40 This could be complemented by the introduction of peer-support workers in mental health services and the participation of families in governance and system evaluation.41 The development of mental health surveillance can be based on such examples and integrate indicators on excess mortality to provide useful information to guide decision making at program, regional, or system levels.
Conclusions
Decreasing discrimination in health and health care services for patients with mental illness also requires a public health perspective provided by the surveillance and analysis of excess mortality among patients with mental disorders,9 and those with other common chronic disorders. Our study demonstrates the feasibility of using administrative data to measure the impact of current and future mental health plans in Canada, provided the techniques can be replicated in other Canadian provinces.10,42
Abbreviations
- CCDSS
Canadian Chronic Disease Surveillance System
- CVD
cardiovascular disease
- GP
general practitioner
- ICD
International Classification of Diseases
- INSPQ
Institut national de santé publique du Québec
- MHCC
Mental Health Commission of Canada
- PHAC
Public Health Agency of Canada
- QICDSS
Quebec Integrated Chronic Disease Surveillance System
- SMD
severe mental disorder
Acknowledgments
This project was conducted and funded as part of the chronic diseases surveillance mandate of the INSPQ. Dr Lesage and Dr Kisely were also supported by their universities. A Canadian Institutes of Health Research grant on the use of administrative health databases in Canada, to measure treated mental disorders in children and youth, partly supported Dr Diallo.
References
- 1.Amaddeo F, Tansella M. Mortality among people with mental disorders. Epidemiol Psichiatr Soc. 2010;19(1):1–3. [PubMed] [Google Scholar]
- 2.Lawrence D, Kisely S, Pais J. The epidemiology of excess mortality in people with mental illness. Can J Psychiatry. 2010;55(12):752–760. doi: 10.1177/070674371005501202. [DOI] [PubMed] [Google Scholar]
- 3.Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64(10):1123–1131. doi: 10.1001/archpsyc.64.10.1123. [DOI] [PubMed] [Google Scholar]
- 4.Tiihonen J, Lonnqvist J, Wahlbeck K, et al. 11-year follow-up of mortality in patients with schizophrenia: a population-based cohort study (FIN11 study) Lancet. 2009;374(9690):620–627. doi: 10.1016/S0140-6736(09)60742-X. [DOI] [PubMed] [Google Scholar]
- 5.Lawrence D, Hancock KJ, Kisely S. The gap in life expectancy from preventable physical illness in psychiatric patients in western Australia: retrospective analysis of population based registers. BMJ. 2013;346:f2539. doi: 10.1136/bmj.f2539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chwastiak LA, Tek C. The unchanging mortality gap for people with schizophrenia. Lancet. 2009;374(9690):590–592. doi: 10.1016/S0140-6736(09)61072-2. [DOI] [PubMed] [Google Scholar]
- 7.Lawrence DM, Holman CD, Jablensky AV, et al. Death rate from ischaemic heart disease in western Australian psychiatric patients 1980–1998. Br J Psychiatry. 2003;182:31–36. doi: 10.1192/bjp.182.1.31. [DOI] [PubMed] [Google Scholar]
- 8.Giddings G. Sense and sensitivity. CMAJ. 2013;185(18):1555. doi: 10.1503/cmaj.131617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thornicroft G. A new mental health strategy for England. BMJ. 2011;342:d1346. doi: 10.1136/bmj.d1346. [DOI] [PubMed] [Google Scholar]
- 10.Mental Health Commission of Canada (MHCC) Changing directions, changing lives: the mental health strategy for Canada. Calgary (AB): MHCC; 2012. [Google Scholar]
- 11.Tansella M, Thornicroft G. A conceptual framework for mental health services: the matrix model. Psychol Med. 1998;28(3):503–508. doi: 10.1017/s0033291796005880. [DOI] [PubMed] [Google Scholar]
- 12.Pelletier C, Dai S, Roberts KC, et al. Report summary. Diabetes in Canada: facts and figures from a public health perspective. Chronic Dis Inj Can. 2012;33(1):53–54. [PubMed] [Google Scholar]
- 13.Public Health Agency of Canada (PHAC) Report from the Canadian chronic disease surveillance system: mental illness in Canada. Ottawa (ON): PHAC; 2015. [Google Scholar]
- 14.Kisely S, Lin E, Gilbert C, et al. Use of administrative data for the surveillance of mood and anxiety disorders. Aust N Z J Psychiatry. 2009;43(12):1118–1125. doi: 10.3109/00048670903279838. [DOI] [PubMed] [Google Scholar]
- 15.Kisely S, Lin E, Lesage A, et al. Use of administrative data for the surveillance of mental disorders in 5 provinces. Can J Psychiatry. 2009;54(8):571–575. doi: 10.1177/070674370905400810. [DOI] [PubMed] [Google Scholar]
- 16.Lesage A, Émond V, Rochette L. Surveillance of mental disorders in Québec: prevalence, mortality and service utilization profile. Quebec (QC): Direction de l’analyse et de l’évaluation des systèmes de soins et services, Institut national de santé publique du Québec; 2013. [Google Scholar]
- 17.Blais C, Jean S, Sirois C, et al. Quebec Integrated Chronic Disease Surveillance System (QICDSS), an innovative approach. Chronic Dis Inj Can. 2014;34(4):226–235. [PubMed] [Google Scholar]
- 18.Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis. 2006;3(2):A42. [PMC free article] [PubMed] [Google Scholar]
- 19.Grigoletti L, Perini G, Rossi A, et al. Mortality and cause of death among psychiatric patients: a 20-year case-register study in an area with a community-based system of care. Psychol Med. 2009;39(11):1875–1884. doi: 10.1017/S0033291709005790. [DOI] [PubMed] [Google Scholar]
- 20.Wahlbeck K, Westman J, Nordentoft M, et al. Outcomes of Nordic mental health systems: life expectancy of patients with mental disorders. Br J Psychiatry. 2011;199(6):453–458. doi: 10.1192/bjp.bp.110.085100. [DOI] [PubMed] [Google Scholar]
- 21.Vanasse A, Courteau J, Fleury MJ, et al. Treatment prevalence and incidence of schizophrenia in Quebec using a population health services perspective: different algorithms, different estimates. Soc Psychiatry Psychiatr Epidemiol. 2012;47(4):533–543. doi: 10.1007/s00127-011-0371-y. [DOI] [PubMed] [Google Scholar]
- 22.Chiang CL. The life table and its applications. Original ed. Malabar (FL): RE Krieger; 1984. [Google Scholar]
- 23.Hsieh JJ. A general theory of life table construction and a precise abridged life table method. Biom J. 1991;33(2):143–162. doi: 10.1002/bimj.4710330204. [DOI] [PubMed] [Google Scholar]
- 24.Kisely S, Smith M, Lawrence D, et al. Mortality in individuals who have had psychiatric treatment: population-based study in Nova Scotia. Br J Psychiatry. 2005;187:552–558. doi: 10.1192/bjp.187.6.552. [DOI] [PubMed] [Google Scholar]
- 25.Bjorkenstam E, Ljung R, Burstrom B, et al. Quality of medical care and excess mortality in psychiatric patients—a nationwide register-based study in Sweden. BMJ Open. 2012;2:e000778. doi: 10.1136/bmjopen-2011-000778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kisely S, Smith M, Lawrence D, et al. Inequitable access for mentally ill patients to some medically necessary procedures. CMAJ. 2007;176(6):779–784. doi: 10.1503/cmaj.060482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murphy JM, Gilman SE, Lesage A, et al. Time trends in mortality associated with depression: findings from the Stirling County study. Can J Psychiatry. 2010;55(12):776–783. doi: 10.1177/070674371005501205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schmitz N, Messier L, Nitka D, et al. Factors associated with disability and depressive symptoms among individuals with diabetes: a community study in Quebec. Psychosomatics. 2011;52(2):167–177. doi: 10.1016/j.psym.2010.11.020. [DOI] [PubMed] [Google Scholar]
- 29.Schmitz N, Wang J, Malla A, et al. Joint effect of depression and chronic conditions on disability: results from a population-based study. Psychosom Med. 2007;69(4):332–338. doi: 10.1097/PSY.0b013e31804259e0. [DOI] [PubMed] [Google Scholar]
- 30.Lesage A, Vasiliadis H, Gagné M, et al. Prevelance of mental illnesses and related service utilization in Canada: an analysis of the Canadian Community Health Survey. Mississauga. (ON): Canadian Collaborative Mental Health Initiative; 2006. [Google Scholar]
- 31.Ouadahi Y, Lesage A, Rodrigue J, et al. [Can mental health problems be diagnosed by general physicians? Perspectives of family physicians according to administrative standards] Sante Ment Que. 2009;34(1):161–172. doi: 10.7202/029764ar. French. [DOI] [PubMed] [Google Scholar]
- 32.Saha S, Chant D, Welham J, et al. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2(5):e141. doi: 10.1371/journal.pmed.0020141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tu K, Wang M, Ivers N, et al. Case definition validation study for mental health surveillance in Canada. Toronto (ON): Institute of Clinical Evaluative Sciences; 2012. [Google Scholar]
- 34.West SL, Richter A, Melfi CA, et al. Assessing the Saskatchewan database for outcomes research studies of depression and its treatment. J Clinical Epidemiol. 2000;53(8):823–831. doi: 10.1016/s0895-4356(99)00237-1. [DOI] [PubMed] [Google Scholar]
- 35.Public Health Agency of Canada (PHAC) Report from the Canadian Chronic Disease Surveillance System: hypertension in Canada. Ottawa (ON): PHAC; 2010. [PubMed] [Google Scholar]
- 36.Lesage A, St-Laurent D, Gagne M, et al. [Suicide prevention from a public health perspective] Sante Ment Que. 2012;37(2):239–255. doi: 10.7202/1014954ar. French. [DOI] [PubMed] [Google Scholar]
- 37.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294(16):2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 38.Public Health Agency of Canada (PHAC) Report from the National Diabetes Surveillance System: diabetes in Canada, 2009 [Internet] Ottawa (ON): Chronic Disease Surveillance Division Centre for Chronic Disease Prevention and Control; 2009. [cited 2015 Nov 6]. Available from: http://www.phac-aspc.gc.ca/publicat/2009/ndssdic-snsddac-09/index-eng.php. [Google Scholar]
- 39.Canadian Diabetes Association (CDA) An economic tsunami the cost of diabetes in Canada [Internet] Toronto (ON): CDA; 2009. [cited 2015 Nov 6]. Available from: http://www.diabetes.ca/publications-newsletters/advocacy-reports/economic-tsunami-the-cost-of-diabetes-in-canada. [Google Scholar]
- 40.Rosenberg S, Rosen A. Can mental health commissions really drive reform? Towards better resourcing, services, accountability and stakeholder engagement. Australas Psychiatry. 2012;20(3):193–198. doi: 10.1177/1039856212447860. [DOI] [PubMed] [Google Scholar]
- 41.Institute of Health Economics (IHE) Consensus statement on improving mental health transitions [Internet] Edmonton (AB): IHE; 2014. [cited year 2015 Nov 6]. Available from: http://www.ihe.ca/advanced-search/consensus-statement-on-improving-mental-health-transitions. [Google Scholar]
- 42.Kirby MJL, Keon WJ. Out of the shadows at last. Transforming mental health, mental illness and addiction services in Canada [Internet] Ottawa (ON): The Standing Senate Committee on Social Affairs, Science and Technology, Parliament of Canada; 2006. [cited 2015 Nov 6]. Available from: http://www.parl.gc.ca/content/sen/committee/391/soci/rep/rep02may06-e.htm. [Google Scholar]