Abstract
Objective
To explore factors associated with discharge placement (DP) and need for skilled assistance after patients are discharged to home following lumbar Laminectomy
Methods
A retrospective analysis of 339 patients who underwent lumbar laminectomy was conducted. We used multivariable logistic regression analysis to identify significant covariates and to construct two regression models: a primary model to predict DP, home versus inpatient rehabilitation/skilled nursing facility (IR/SNF), and a secondary model to predict the need for skilled assistance once patients are discharged to home.
Results
Sample included 48.7% females, 68.2% married, 56.3% independent in daily activities, and 85.2% discharged to home. Subjects were 56.06±12.75 years old and had 31.35±6.2 BMI. Of those discharged to home, 17.7% needed skilled assistance. Patients stayed 4.41±3.55 days in the hospital and walked 203.38±144.87 feet during hospital stay. Age, distance walked during hospital stay, and length of hospital stay (LOS) were significant positive predictors for discharge to home versus IR/SNF, whereas single living status, diminished prior level of function, and longer LOS were predictors of need for skilled assistance after discharge to home.
Conclusion
Age, mobility, marital status, prior level of function and LOS are key variables in determining healthcare needs following lumbar Laminectomy.
Keywords: Laminectomy, discharge placement, skilled care, physical therapy, functional status, length of stay
INTRODUCTION
In the United States, there has been an increase in the prevalence of lumbar spine surgeries (LSS), with a similar increase in surgery costs and related post-surgical care.1–3 The prevalence of these surgeries in the US is approximately 0.2% of the population, which is at least 40% higher than other countries and five times higher than England and Scotland.4–6 This rise in LSS in the last decade has increased the demands for optimizing surgical outcomes, and need to establish evidence-based guidelines for patient’s health care needs during their hospital stay and after hospital discharge.7–10
Lumbar laminectomy is a common surgical procedure, primarily for the treatment of lumbar stenosis in elderly patients.11 Current randomized controlled trials support lumbar laminectomy over conservative management.12 Patients who received spine surgery reported significant improvement in pain, function, and quality of life which was maintained for 4-years.13 However, the results of spinal surgeries are not always consistent and present significant variation in short and long term outcomes.14 Implementation of post-surgical interventions such as rehabilitation and post-surgical care may optimize surgical outcomes.14
Studies have investigated possible pre- and post-surgical factors to predict short- and long-term outcomes.10, 15–21 Patient-related factors such as age, gender, work status, comorbidities, preoperative pain intensity and duration, work status, and emotional and psychological factors (e.g. fear of movement, anxiety, and depression), were found to be associated with post-surgical outcomes.15, 17–19, 21–23
Intraoperative factors have also been shown to influence postsurgical outcomes. Intraoperative fluid infusion, American Society of Anesthesia (ASA) score, physical status, type of surgical procedure, and total intraoperative platelet administration were significant predictors of length of stay (LOS) in an intensive care unit.24 In another study, the number of levels fused, postoperative hemoglobin and hematocrit values, total volume of blood resuscitation, and duration of operation were also significantly correlated with LOS.25 However, these variables have not been investigated for hospital discharge planning and health care needs following hospital discharge.
Inpatient physical therapy (PT) assessment plays an important role in discharge planning. However, PT assessment and functional status are rarely studied as possible predictors of short- or long-term outcomes after LSS. Sharma and colleagues26 showed that LOS was significantly correlated with the number of inpatient PT encounters and pre- and post-surgical functional levels. LOS was significantly higher for patients discharged to a health care facility compared to home. Therefore, the aforementioned factors could also be associated with discharge placement (DP) after LSS and should be explored.
The process of discharge planning starts soon after surgery and is determined by interdisciplinary team members. Discharge planning is targeted to ensure efficient hospitalization and to determine appropriate DP, e.g. home versus health care facility, to bridge the gap between hospital and community care after discharge.27–29 Recently, there has been an increased demand to shorten LOS and to provide safe and appropriate DP for continuous community care. 27–29 In early discharge and short hospital stays, patients are usually medically stable but might not have reached the optimal functional and independence level after discharge.30 Upon discharge, patients receive education and medication to manage their symptoms. However, some patients following discharge may also need longer recovery time and more assistance with daily activities, provisional to their functional and medical status.
Predictors of DP have been determined in several orthopedic surgeries such as vertebroplasty31 and total hip or knee replacement.32–34 Prediction models were built with age, body mass index, ability to walk,33 pre-admission living status,31, 33 and functional status upon discharge32 as significant predictors of DP. However, predictors of DP following laminectomy have not been investigated. The primary aim of this retrospective study was to explore factors associated with DP (home versus health care facility) following lumbar laminectomy. The secondary aim was to investigate the factors defining the need for skilled assistance after patients are discharged to home. The role of PT assessment was also incorporated in prediction models, which has not been considered before. Understanding these factors could assist clinicians in discharge planning and the level of care needed following hospital discharge, as well as assist patients, family members and caregivers in having realistic expectations after the surgery.
METHOD
We reviewed de-identified medical records of patients who underwent lumbar laminectomy at the [BLINED] between November 2007 and July 2011. The medical informatics division at the [BLINED] has developed the Healthcare Enterprise Repository for Ontological Narration (HERON),35 an integrated data repository that provides researchers an access to de-identified electronic medical records from the hospital and clinics (Epic Corporation). HERON also provides access to other administrative, research, and public sources, such as the clinics’ billing system (GE IDX), the University Health Consortium (UHC) (https://www.uhc.edu), tumor registries, and the Social Security Death Index. HERON’s incorporation of multidisciplinary flowsheets from the electronic medical record allowed this study to evaluate vital signs and PT assessment rarely included in prior studies. We selected our cohort of interest from HERON using the i2b2 query and analysis tool,36 and created our query to find the data of interest in LSS patients’ medical records.
Study Cohort
Current Procedural Terminology (CPT) codes for posterior lumbar laminectomy, laminotomy, or decompression were used to identify the cohort of interest in the i2b2 query and analysis tool. Medical records from patients 18 years or older only were included in the study. Medical records were excluded for patients with neoplasm or intraspinal abscess, spinal deformity (scoliosis, kyphoscoliosis), spine fractures, surgery for vertebroplasty or congenital deformities, osteomyelitis, history of spine fractures, and cauda equina syndrome. Based on these criteria, 352 records were identified.
Data Selection
In the HERON data system, covariates were selected based on relative research and clinical experience.10, 15–23, 25, 26, 31–34 The covariates obtained from the system are summarized in Table 1.
Table 1.
Summary of all covariates
| Characteristics | Mean (SD) | Percentage (%) | Number of valid cases |
|---|---|---|---|
| Age | 56.06 (12.75) | - | 317 |
| Body mass index (BMI) | 31.35 (6.23) | - | 352 |
| Gender | - | 352 | |
| • Male | 51.3 | ||
| • Female | 48.7 | ||
| Housing | - | 348 | |
| • House | 88.5 | ||
| • Apartment | 11.4 | ||
| Marital status | - | 348 | |
| • Married | 68.2 | ||
| • Single/divorced/widowed | 31.8 | ||
| Living status | - | 351 | |
| • Living with family or significant other | 84.7 | ||
| • Not living with family | 15.3 | ||
| Number of comorbidities | 1.39 (1.78) | - | 352 |
| Change in hemoglobin level (gm/dl) | −1.77 (1.28) | - | 331 |
| Change in hematocrit level (%) | −2.19 (5.86) | - | 335 |
| Total fluid transfusion (ml) | 2280.98 (1038.89) | - | 352 |
| Prior level of function (PLOF) | - | 352 | |
| • Dependent | 3.8 | ||
| • Partially dependent | 39.9 | ||
| • Independent | 56.3 | ||
| Inpatient back pain on numeric pain rating scale | 4.50 (1.14) | - | 322 |
| Radiculopathy continued after surgery | - | 283 | |
| • Yes | 38.1 | ||
| • No | 61.9 | ||
| Functional dependency score | 352 | ||
| • Independent | 22.0 | ||
| • Partially dependent | 48.5 | ||
| • Maximally independent | 29.5 | ||
| Sitting and standing balance combined score | 6.24 (1.83) | - | 314 |
| Gait distance (feet) | 203.38 (144.87) | - | 352 |
| Use of assistive device during inpatient ambulation | - | ||
| • Yes | 62.6 | ||
| • No | 37.5 | ||
| Length of hospital stay | 4.41 (3.55) | 352 |
The DP was obtained from the discharge summary note signed by the attending physician, determining the discharge destination. The discharge destination included: home, home with family assistance, home setting with outpatient PT, home with home health, inpatient rehabilitation, or skilled nursing facility.
We defined comorbidities as diagnosis of any of these conditions: Cerebrovascular disease, Chronic pulmonary disease, Congestive heart failure, Connective tissue disease, Dementia, Hemiplegia, Leukemia, Malignant lymphoma, Myocardial infarction, Peripheral vascular disease, Ulcer disease, Diabetes Mellitus, Liver disease, Renal Disease, and Malignant solid tumor. We calculated the changes (post-pre surgery) in both hemoglobin and hematocrit. The sum of the volume of crystalloids, colloid was used to refer as total intraoperative fluid infusion. Patient’s self-reported prior level of function (PLOF) was determined based on the level of assistance needed in mobility and activities of daily livings (independent, partially dependent, and maximally dependent). During the hospital stay, the functional independence measure (FIM) scale37 was used to assess the level of dependency in 3 functional activities: bed mobility, transfer, and gait. The combined score of FIM was then classified as independent, partially dependent, or maximally independent. Sitting and standing balance scores during inpatient stay were measured with an 11-point balance scale.38 LOS was calculated as the number of days spent from the day of admission to the day of discharge.
Data Processing and Statistical Analysis
Data Processing
Categorical variables were converted to coded variables. For DP, ordinal data were reduced to two categories: home versus inpatient rehabilitation/skilled nursing facility (IR/SNF). Those discharged to home were further classified into two additional categories: 1) home with skilled assistance (patients who needed more than family assistance such as home health, and outpatient PT), and 2) home without skilled assistance (Figure 1).
Figure 1.
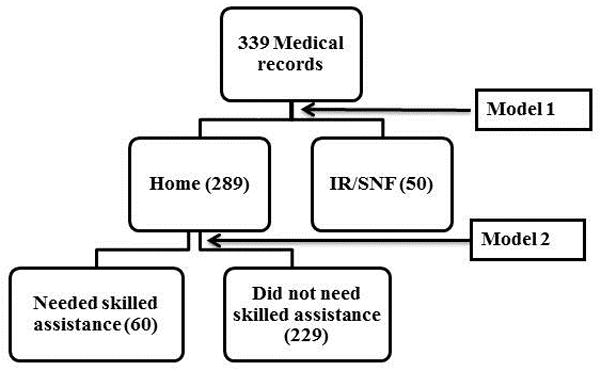
Allocation of cases to groups and subgroups
We tested the normality of the continuous variables and performed transformation on variables whenever necessary [natural log transformation of the LOS (ln (LOS)) and square root transformation of gait distance (sqrt (gait)].
Statistical Analysis
PASW Statistics 20 (SPSS, Inc., 2009, Chicago, IL) was used for statistical analysis. To test the differences between two main groups (home vs. IR/SNF) and two subgroups (home with skilled assistance and home without skilled assistance), we used independent sample student’s t-test for normally distributed continuous variables, Mann-Whitney’s test for skewed continuous variables, and chi square rest for categorical variables (p<0.05). We performed univariable logistic regression to explore important covariates (p<0.1) to be entered in multivariable logistic regression models. In multivariable logistic regression models, possible predictors were removed from the model if they did not contribute significantly to the model (p<0.05) using the enter selection method. Also, we used backward and forward selection methods to confirm our results. Significant variables were then used to build the final two models, home vs. IR/SNF and home with or without skilled assistance. We then used receiver operating characteristics (ROC) curve to evaluate the classification accuracy of the final models. The multivariable model was built using complete cases considering small proportions of missing values among potential predictor candidates.
RESULTS
Of the entire data set, 14.8 % (52 patients) were discharged to IR/SNF, 67.3% (237 patients) were discharged to home without skilled assistance, and 17.9% (63 patients) were discharged to home with skilled assistance (Figure 1).
Model I: Home versus IR/SNF
The differences between patients discharged to home and patients discharged to IR/SNF are summarized in Table 2. Patients in the IR/SNF group were significantly older, had a higher drop in their hematocrit level after surgery, needed more fluid infusion during the surgery, had a greater number of comorbidities, and stayed longer in the hospital. PT assessment covariates showed that patients in the IR/SNF group were more likely to live alone, walked significantly shorter distance during their hospital stay, had lower balance scores, and were functionally more dependent before surgery and during their hospital stay. There were no significant differences between the two groups in other covariates, although marital and living status showed a trend toward significance between both groups.
Table 2.
Summary of patients discharged to home vs. IR/SNF
| Variable | Home mean (SD) or % | IR/SNF mean (SD) or % | p |
|---|---|---|---|
| N | 289 | 50 | |
| Age (years) | 54.96 (12.23) | 62.31 (14.01) | <0.001* |
| Gender | |||
| Female (%) | 48.7% | 54% | 0.251† |
| Male (%) | 51.3% | 46% | |
| Marital status | |||
| Married (%) | 70% | 58% | 0.052† |
| Single/Divorced/Widowed (%) | 30% | 42% | |
| BMI (kg/m^2) | 31.34 (6.15) | 31.39 (6.73) | 0.95* |
| Housing | |||
| House (%) | 91% | 84% | 0.12† |
| Other (%) | 9% | 16% | |
| Living status | |||
| Family (%) | 87% | 74% | 0.02† |
| Other (%) | 13% | 26% | |
| Prior level of function (PLOF) | |||
| Dependent (%) | 2% | 14% | <0.001† |
| Partially dependent (%) | 37.8% | 52% | |
| Independent (%) | 60.2% | 34% | |
| Change in hemoglobin level (gm/dl) | −1.73 (1.22) | −2.01 (1.60) | 0.14* |
| Change in hematocrit level (%) | −1.77 (5.79) | −4.62 (5.77) | 0.01* |
| LOS (days) | 3.91 (3.20) | 7.30 (4.10) | <0.001‡ |
| Gait distance (feet) | 223.68 (142.84) | 86.05 (91.45) | <0.001‡ |
| Balance score (Sitting and standing balance) | 6.43 (1.78) | 5.23 (1.76) | <0.001‡ |
| Dependency | |||
| Independent | 15.2% | 6% | <0.001* |
| Partially dependent | 44.9% | 24% | |
| Maximum independent | 39.9% | 70% | |
| Total fluid transfusion | 2233.12 (1002.22) | 2493.57 (1221.12) | <0.001* |
| Pain Day 0 | 4.61 (1.11) | 4.34 (1.52) | 0.12* |
| Pain Day 1 | 4.54 (1.12) | 4.29 (1.24) | 0.20* |
| Radiculopathy | |||
| Yes | 61% | 52% | 0.31† |
| No | 36% | 48 | |
| Comorbidities | 1.25 (1.68) | 2.15 (2.10) | <0.001‡ |
Independent Samples t-test,
Matt-Whitney test,
chi-square test, p<0.05 in bold
Exploratory univariable logistic regression (Table 3) showed that age, marital status, living status, prior level of function (PLOF), change in hematocrit level, ln (LOS), and sqrt (gait), balance score, number of comorbidities, and dependency score might be potential predictors for building a multivariate logistic regression model for the response variable (Home vs. IR/SNF).
Table 3.
Univariable and multivariable logistic regression analyses for home vs. IR/SNF
| Univariable analysis | Multivariable analysis | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Factor | β | SE | p | β | SE | p |
| Age | 0.05 | 0.15 | <0.001 | 0.04 | 0.013 | 0.02 |
| Marital status | 0.61 | 0.27 | 0.05 | ‡ | ||
| Gender | −0.25 | 0.26 | 0.42 | ‡ | ||
| BMI | 0.01 | 0.02 | 0.95 | ‡ | ||
| Housing | 0.62 | 0.42 | 0.16 | ‡ | ||
| Living status | 0.84 | 0.23 | 0.02 | 0.60 | 0.45 | 0.19 |
| PLOF | −1.09 | 0.16 | <0.001 | −0.33 | 0.33 | 0.33 |
| Change in hemoglobin level | −0.17 | 0.11 | 0.16 | ‡ | ||
| Change in hematocrit level | −0.10 | 0.02 | 0.01 | −0.02 | 0.04 | 0.54 |
| ln (LOS) | 1.80 | 0.19 | <0.001 | −0.25 | 0.04 | <0.001 |
| sqrt (Gait) | −0.23 | 0.03 | <0.001 | 0.84 | 0.30 | 0.01 |
| Assistive device | 0.29 | 0.18 | 0.13 | ‡ | ||
| Balance Score | −0.35 | 0.09 | <0.01 | 0.02 | 0.12 | 0.88 |
| Intraoperative fluid infusion (mL) | 0.00 | 0.00 | 0.18 | ‡ | ||
| Pain Day 0 | −0.20 | −0.11 | 0.13 | ‡ | ||
| Pain Day 1 | −0.19 | 0.12 | 0.17 | ‡ | ||
| Radiculopathy | 0.58 | 0.53 | 0.06 | 0.04 | 0.39 | 0.93 |
| Comorbidity | 0.24 | 0.14 | <0.001 | 0.12 | 0.09 | 0.23 |
| Dependency score | −0.97 | 0.21 | <0.001 | −0.14 | 0.27 | 0.59 |
not included in multivariable analysis as they were not significant in univariable analysis, p<0.1 for univariable and p<0.05 for multivariable in bold
Multivariable logistic regression (Table 3) showed only age, sqrt (gait), and ln (LOS) were significant predictors of DP. Hosmer-Lemeshow goodness-of-fit test was non-significant (χ2 (8) = 7.77, p = 0.56), indicating good fit of model.39 The area under the ROC curve of the final model was 0.80, indicating good accuracy of the final model. A plot of odds ratios and confidence intervals suggests that the likelihood of being discharged to IR/SNF was increased by 2.42 for an every increment in natural log of LOS, and decreased by 0.83 for an increase in one square root of distance walked during the hospital stay. Although significant, the odds ratio for age was small, suggesting that the likelihood of being discharged to IR/SNF was increased by 1.04 for each one year increase in age.
Model II: Home With or Without Skilled Assistance
Of the 289 patients discharged to home, 229 did not need skilled assistance, while 60 needed skilled assistance (home health or outpatient PT). The differences between the two groups are summarized in Table 4. Patients who needed skilled assistance were significantly more likely to be single, required more fluid resuscitation during the surgery, had more comorbidities, and stayed longer in the hospital. Living status and hematocrit levels were not significantly different between both subgroups but showed a trend toward difference. PT assessment covariates showed that patients who needed skilled assistance were significantly more dependent before surgery (decreased PLOF) and during their hospital stay (decreased dependency score), walked shorter distance, and had lower balance score during their hospital stay. There was no significant difference in other covariates between the two groups.
Table 4.
Summary of the patients discharged to home with or without skilled assistance
| Variables | No skilled assistance Mean (SD) | Skilled assistance Mean (SD) | p |
|---|---|---|---|
| n | 229 | 60 | |
| Age (yr) | 54.31 (12.12) | 57.54 (12.42) | 0.07* |
| Gender | |||
| Female (%) | 46.3% | 53.3% | 0.21† |
| Male (%) | 53.7% | 46.7% | |
| Marital status | |||
| Married (%) | 74.2% | 53.3% | <0.02† |
| Single/Divorced/Widowed (%) | 25.8% | 46.7% | |
| BMI (kg/m^2) | 31.45 (6.17) | 30.91 (6.06) | 0.54* |
| Housing | |||
| House (%) | 90.1% | 85% | 0.14† |
| Other (%) | 9.9% | 15% | |
| Living status | |||
| Family (%) | 80.1% | 71.7% | 0.09† |
| Other (%) | 19.9% | 28.3% | |
| Prior level of function (PLOF) | |||
| Dependent (%) | 1.7% | 3.3% | <0.01† |
| Partially dependent (%) | 32.3% | 58.3% | |
| Independent (%) | 66% | 38.4% | |
| Change in hemoglobin level (gm/dl) | −1.70 (1.23) | −1.85 (1.19) | 0.38* |
| Change in hematocrit level (%) | −1.46 (5.87) | −2.96 (5.34) | 0.07* |
| LOS (days) | 3.32 (2.57) | 6.17 (4.23) | <0.001‡ |
| Gait distance (feet) | 234.78 (140.43) | 181.31 (143.65) | <0.01‡ |
| Balance score (Sitting and standing balance) | 6.62 (1.72) | 5.73 (1.84) | 0.01‡ |
| Functional dependency score | |||
| Independent (%) | 16.6% | 6.6% | 0.01† |
| Partially dependent (%) | 47.6% | 35.1% | |
| Maximum dependent (%) | 35.8% | 58.3% | |
| Intraoperative fluid infusion (mL) | 2176.70 (971.78) | 2482.05 (1080.54) | 0.04* |
| Pain 0 | 4.63 (1.10) | 4.58 (1.17) | 0.72* |
| Pain 1 | 4.56 (1.15) | 4.47 (0.95) | 0.57* |
| Radiculopathy | |||
| Yes | 37.5% | 40% | 0.87† |
| No | 62.5% | 60% | |
| Comorbidities | 1.14 (1.59) | 1.68 (1.94) | 0.03‡ |
Independent Samples t-test,
Matt-Whitney test,
chi-squared test, p<0.05 in bold
Exploratory univariable logistic regression (Table 5) showed that age, marital status, PLOF, change in hematocrit level, ln (LOS), sqrt (gait), use of assistive devices, balance score, total intraoperative fluid infusion, number of comorbidities, and dependency score were possible predictors (p<0.1), and were entered into the multivariable logistic regression analysis.
Table 5.
Univariable and multivariable logistic regression analyses for discharge to home with or without skilled assistance
| Univariable analysis | Multivariable analysis | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Factor | β | SE | p | β | SE | p |
| Age | 0.02 | 0.02 | 0.07 | 0.03 | 0.02 | 0.84 |
| Marital status|| | 0.93 | 0.81 | <0.001 | 0.85 | 0.412 | 0.04 |
| Gender | −0.28 | 0.123 | 0.33 | ‡ | ||
| BMI | −0.02 | 0.03 | 0.54 | ‡ | ||
| Housing | 0.56 | 0.59 | 0.19 | ‡ | ||
| Living status | 0.51 | 0.29 | 0.13 | ‡ | ||
| PLOF¶ | −0.97 | 0.21 | <0.001 | −0.47 | 0.22 | 0.04 |
| Change in hemoglobin level | −0.11 | 0.12 | 0.38 | ‡ | ||
| Change in hematocrit level | −0.05 | 0.03 | 0.07 | −0.02 | 0.03 | 0.58 |
| ln (LOS) | 1.74 | 0.32 | <0.001 | 1.46 | 0.34 | <0.001 |
| sqrt (Gait) | −0.09 | 0.03 | <0.001 | 0.03 | 0.04 | 0.59 |
| Assistive device | 0.50 | 0.19 | 0.001 | −0.37 | 0.28 | 0.19 |
| Balance Score | −0.30 | 0.09 | <0.001 | −0.09 | 0.13 | 0.48 |
| Total fluid volume | 0.01 | 0.00 | 0.04 | 0.01 | 0.01 | 0.57 |
| Pain Day 0 | −0.01 | 0.14 | 0.92 | ‡ | ||
| Pain Day 1 | −0.05 | 0.13 | 0.95 | ‡ | ||
| Radiculopathy | −0.12 | 0.30 | 0.69 | ‡ | ||
| Comorbidity | 0.17 | 0.08 | 0.03 | −0.06 | 0.11 | 0.61 |
| Dependency score | 0.74 | 0.10 | 0.01 | 0.66 | 0.35 | 0.06 |
Not included in multivariable analysis as they were not significant in univariable analysis, p<0.1 for univariable and p<0.05 for multivariable in bold,
(0: married, 1: single (reference category)),
(0: dependent, 1: modified dependent, 2: independent (reference category)).
Multivariable logistic regression (Table 5) showed that marital status, PLOF, and ln (LOS) were the only significant predictors showing which patients would need skilled assistance and which patients would not after hospital discharge. Hosmer-Lemeshow goodness-of-fit test was non-significant (χ2 (8) = 2.90, p = 0.89), indicating good fit of model.39 The area under the ROC curve of the final model was 0.84, indicating good accuracy of the final model. A plot of odds ratios and confidence intervals (Figure 3) indicates that the likelihood of needing assistance is increased by 2.33 times for single patients as compared to married patients, and by 4.3 times for an increase in one natural log of LOS, and decreased by 0.63 times in more independent patients.
Figure 3.

Forest plot of odds ratios and confidence intervals (CI) of significant factors from multivariable analysis, predicting discharged to home with or without skilled assistance
DISCUSSION
In this retrospective study, we used multivariable logistic regression to build prediction models describing which patients might be discharged to home or to IR/SNF, and which patients are likely to require skilled assistance once discharged to home. Of the factors associated with discharge destination, only age, distance walked during hospital stay and LOS were significant predictors of DP. The ROC analysis suggests that our model is useful in determining which patients will need IR/SNF. For the patients who required skilled assistance at home, only marital status, PLOF, and LOS were significant predictors for health care need beyond the hospital stay. The ROC analysis suggests that our model is accurate in predicting level of assistance needed following discharge to home—with or without skilled assistance. Missing data points is a limitation of retrospective studies. We experienced less than 10% missing data points. Our analyses with and without imputation resulted in similar findings.
Home versus IR/SNF
Our results are consistent with those of previous studies involving orthopedic surgeries of other joints, where older age has been associated with discharge to IR/SNF.33, 40–42 Elderly patients are more likely to be discharged to IR/SNF, because age is often accompanied by a higher rate of complications and comorbidities, as well as a longer recovery time after surgery.25, 33 In fact, declining physical function is consistent with older age. The ability to walk a longer distance during the hospital stay is considered an important positive indicator of patients’ functional status and level of independence. With primary and revised total hip replacements, the patients’ inability to walk at the time of hospital discharge was shown to be a significant predictor for discharge to a rehabilitation facility.33 Our results are in agreement with these findings and suggest that patients should be walking more during their hospital stay post-LSS. At present, patients’ mobility is limited to the number of PT visits they receive during their hospital stay. Increasing walking distance, especially for elderly patients, may be beneficial. In our study, the LOS was also strongly correlated with the number of PT encounters (Spearman r=0.91, p<0.001), suggesting that patients who stayed longer in the hospital needed more PT assistance and therefore were anticipated to benefit from IR/SNF services. Financial factors and health insurance coverage are also important determinants for DP,43, 44 and should be considered in future studies.
Social factors such as marital and living status, pre- and post-surgical functional status, and change in hematocrit level were associated (although were not significant predictors) with DP, and should be considered in discharge planning. Although higher BMI and female gender were associated with discharge to IR/SNF in other orthopedic studies,32, 33 they were not significantly associated with DP in our study. However, in a previous study, only female gender, but not BMI, was significantly correlated with longer LOS after LSS.26 Other socio-demographic factors, such as education level, income, and race, should be investigated as possible predictors for DP in future studies, as they were associated with DP in total hip or knee replacement surgeries.32, 33
Home With or Without Skilled Assistance
The amount of social support available to patients is often considered a criterion upon discharge to home with or without skilled assistance. As expected, our results suggested that unmarried patients are likely to need skilled care at home. Secondly, the PLOF was a significant predictor for skilled assistance at home. Patients with poor PLOF before surgery are not expected to show immediate improvement after surgery, and further deterioration in the functional level is expected after surgery due to the operation and hospital admission. Therefore, those patients are more likely to need assistance at home after discharge. These results are relatively similar to Harvey and Kallames’s study31 in which the PLOF and living status prior to surgery guided the discharge planning after vertebroplasty. Attempts to improve PLOF before spinal surgeries might result in less skilled care after hospital discharge. LOS was also a significant predictor for patients needing skilled care after being discharged to home. Longer LOS indicates a longer period of recovery and a greater need for health care services after surgery, either through IR/SNF placement or home–based skilled care, as the patients’ health and functional status may not be adequate for independent function. Neither our results nor those of Harvey and Kallames’31 found an association between pain intensity and DP, or need for skilled care at home. Pain intensity is influenced by medication use and does not seem to be a sensitive measure; rather, physical and functional status are better guides for discharge planning.
The current study revealed an association between change in hematocrit level and DP, and between volume of blood transfusion and level of assistance needed at home; however, these factors were not significant predictors in our two models. Zheng et al.25 found no correlation between blood loss and transfusion with LOS in patients who underwent lumbar spine fusion revision. Previous studies have shown correlation between intraoperative factors and LOS, but not with DP following LSS. Factors such as type of surgical procedure, ASA, and volume of intraoperative fluid infusion were predictors of LOS in an intensive care unit after mixed (cervical, thoracic, and lumbar) spine surgeries.24 In a similar study, the surgery type was associated with, but not a significant predictor of LOS.26 Surgery type did not show an association with DP in our cohort, most likely due to a fewer number of fusion surgeries.
Role of Physical Therapy Assessment
Previous studies have shown the importance of social and clinical factors as predictors of LSS outcomes, but our study highlighted the importance of factors determined by PT assessment as possible predictors of DP and the need for skilled care at home. PLOF, distance walked, balance, and functional dependency status are standard measures of PT assessment. PLOF is usually collected soon after hospital admission or surgery, and is used as indicator of possible rehabilitation needs. PLOF is also used to monitor patients’ progress or decline in function due to hospitalization, especially in older adults.45 The present study showed that patients who needed assistance with activities of daily livings prior to surgery were more likely to require skilled assistance after discharge, emphasizing the need to assess patients’ functional status prior to surgery. Secondly, walking distance is often measured and recorded during each PT visit starting with the first post-operative day, and whenever patients receive PT services. The length of distance walked indicates the patients’ ability to balance and their level of independence and endurance. Finally, dependency score measured during the PT assessment has also been considered a predictor for LOS after LSS in the Sharma et al.26 study; in the present study, it was associated with DP but was not a significant predictor. De Pablo et al.33 concluded that patients who had poor functional status after total hip replacement were discharged to IR/SNF. Our results also show that patients with a poor dependency score stayed longer in the hospital and were more likely to be discharged to IR/SNF.
CONCLUSION
Age, distance walked during the hospital stay, and LOS were significant predictors of DP, whereas single living status, PLOF, and LOS were significant predictors of skilled assistance upon discharge to home. Of the myriad of factors considered for DP following lumbar laminectomy, these variables appeared to be the most important. Age and the stability of patients’ medical status after surgery seem to be key factors in determining DP; the LOS required to reach this level and the functional measures to assess this level are important variables. Patients’ pre- and post-surgical functional status was also a significant predictor in both models. This study also suggests the importance of social support from a spouse. Incorporating the spouse and other family members in patients’ management may reduce the cost and demands on health care. This study also highlights the significance of PT assessment in determining health care services following LSS, although the DP and level of assistance needed at home after discharge are decisions of the multidisciplinary team. The value of social support and PT assessment variables suggests future health service research studies may benefit from supplementing analysis that usually incorporates administrative, laboratory, and physician documentation with the increasingly rich social history and multidisciplinary assessment data available now in electronic medical record flowsheets.
Figure 2.
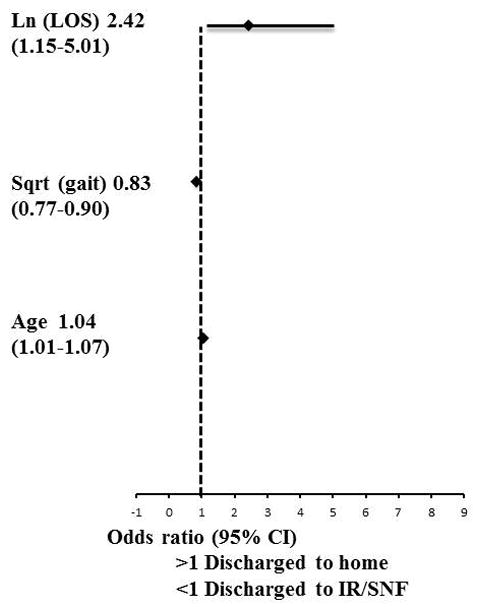
Forest plot of odds ratios and confidence intervals (CI) of significant factors from multivariable analysis, predicting discharge to home vs. IR/SNF
Acknowledgments
This work was supported by a CTSA grant from NCRR and NCATS awarded to the University of Kansas Medical Center for Frontiers: The Heartland Institute for Clinical and Translational Research # UL1TR000001 (formerly #UL1RR033179). The authors would like to thank Krista Sanchez for assistance in data processing and Dr. Lisa VanHoose for reviewing the manuscript.
Footnotes
Disclosure/Conflict of Interest
No duality of interest to declare.
The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH, NCRR, or NCATS.
References
- 1.Deyo RA. Trends and variations in the use of spine surgery. Orthop Related Research. 2006;443:139–146. doi: 10.1097/01.blo.0000198726.62514.75. [DOI] [PubMed] [Google Scholar]
- 2.Weinstein JN, Lurie JD, Olson PR, et al. United States’ trends and regional variations in lumbar spine surgery: 1992–2003. Spine (Phila Pa 1976) 2006;31(23):2707–2714. doi: 10.1097/01.brs.0000248132.15231.fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schiller J, Lucas J, Ward B, Peregoy J. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. National Center for Health Statistics. Vital Health Stat. 2012;252(10) [PubMed] [Google Scholar]
- 4.Ostelo RW, de Vet HC, Waddell G, et al. Rehabilitation following first-time lumbar disc surgery: a systematic review within the framework of the cochrane collaboration. Spine (Phila Pa 1976) 2003;28(3):209–218. doi: 10.1097/01.BRS.0000042520.62951.28. [DOI] [PubMed] [Google Scholar]
- 5.Cherkin DC, Deyo RA, Loeser JD, et al. An international comparison of back surgery rates. Spine (Phila Pa 1976) 1994;19(11):1201–1206. doi: 10.1097/00007632-199405310-00001. [DOI] [PubMed] [Google Scholar]
- 6.Gray DT, Deyo RA, Kreuter W, et al. Population-based trends in volumes and rates of ambulatory lumbar spine surgery. Spine (Phila Pa 1976) 2006;31(17):1957–1963. doi: 10.1097/01.brs.0000229148.63418.c1. discussion 1964. [DOI] [PubMed] [Google Scholar]
- 7.Archer KR, Wegener ST, Seebach C, et al. The effect of fear of movement beliefs on pain and disability after surgery for lumbar and cervical degenerative conditions. Spine (Phila Pa 1976) 2011;36(19):1554–1562. doi: 10.1097/BRS.0b013e3181f8c6f4. [DOI] [PubMed] [Google Scholar]
- 8.Chou R, Baisden J, Carragee EJ, Resnick DK, Shaffer WO, Loeser JD. Surgery for low back pain: a review of the evidence for an American Pain Society Clinical Practice Guideline. Spine (Phila Pa 1976) 2009;34(10):1094–1109. doi: 10.1097/BRS.0b013e3181a105fc. [DOI] [PubMed] [Google Scholar]
- 9.Mannion AF, Elfering A. Predictors of surgical outcome and their assessment. Eur Spine J. 2006;15(Suppl 1):S93–108. doi: 10.1007/s00586-005-1045-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mannion AF, Elfering A, Staerkle R, et al. Predictors of multidimensional outcome after spinal surgery. Eur Spine J. 2007;16(6):777–786. doi: 10.1007/s00586-006-0255-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gibson JN, Waddell G. Surgery for degenerative lumbar spondylosis: updated Cochrane Review. Spine (Phila Pa 1976) 2005;30(20):2312–2320. doi: 10.1097/01.brs.0000182315.88558.9c. [DOI] [PubMed] [Google Scholar]
- 12.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 2009;91(6):1295–1304. doi: 10.2106/JBJS.H.00913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT) Spine (Phila Pa 1976) 2008;33(25):2789–2800. doi: 10.1097/BRS.0b013e31818ed8f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Desai A, Bekelis K, Ball PA, et al. Variation in outcomes across centers after surgery for lumbar stenosis and degenerative spondylolisthesis in the spine patient outcomes research trial. Spine (Phila Pa 1976) 2013;38(8):678–691. doi: 10.1097/BRS.0b013e318278e571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carragee EJ, Han MY, Suen PW, et al. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am. 2003;85-A(1):102–108. [PubMed] [Google Scholar]
- 16.DeBerard MS, LaCaille RA, Spielmans G, et al. Outcomes and presurgery correlates of lumbar discectomy in Utah Workers’ Compensation patients. Spine J. 2009;9(3):193–203. doi: 10.1016/j.spinee.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 17.den Boer JJ, Oostendorp RA, Beems T, et al. Continued disability and pain after lumbar disc surgery: the role of cognitive-behavioral factors. Pain. 2006;123(1–2):45–52. doi: 10.1016/j.pain.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 18.den Boer JJ, Oostendorp RA, Beems T, et al. A systematic review of bio-psychosocial risk factors for an unfavourable outcome after lumbar disc surgery. Eur Spine J. 2006;15(5):527–536. doi: 10.1007/s00586-005-0910-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.LaCaille RA, DeBerard MS, Masters KS, et al. Presurgical biopsychosocial factors predict multidimensional patient: outcomes of interbody cage lumbar fusion. Spine J. 2005;5(1):71–78. doi: 10.1016/j.spinee.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 20.Nygaard OP, Kloster R, Solberg T. Duration of leg pain as a predictor of outcome after surgery for lumbar disc herniation: a prospective cohort study with 1-year follow up. J Neurosurg. 2000;92(2 Suppl):131–134. doi: 10.3171/spi.2000.92.2.0131. [DOI] [PubMed] [Google Scholar]
- 21.Trief PM, Ploutz-Snyder R, Fredrickson BE. Emotional health predicts pain and function after fusion: a prospective multicenter study. Spine (Phila Pa 1976) 2006;31(7):823–830. doi: 10.1097/01.brs.0000206362.03950.5b. [DOI] [PubMed] [Google Scholar]
- 22.Gaetani P, Aimar E, Panella L, et al. Surgery for herniated lumbar disc disease: factors influencing outcome measures. An analysis of 403 cases. Funct Neurol. 2004;19(1):43–49. [PubMed] [Google Scholar]
- 23.Trief PM. A prospective study of psychological predictors of lumbar surgery outcome. Spine (Philadelphia, Pa 1976) 2000;25(20):2616–2621. doi: 10.1097/00007632-200010150-00012. [DOI] [PubMed] [Google Scholar]
- 24.Nahtomi-Shick O. Does intraoperative fluid management in spine surgery predict intensive care unit length of stay? J Clin Anesth. 2001;13(3):208–212. doi: 10.1016/s0952-8180(01)00244-6. [DOI] [PubMed] [Google Scholar]
- 25.Zheng F, Cammisa FP, Jr, Sandhu HS, et al. Factors predicting hospital stay, operative time, blood loss, and transfusion in patients undergoing revision posterior lumbar spine decompression, fusion, and segmental instrumentation. Spine (Phila Pa 1976) 2002;27(8):818–824. doi: 10.1097/00007632-200204150-00008. [DOI] [PubMed] [Google Scholar]
- 26.Sharma NK, Arnold PM, McMahon JK, et al. Acute Physical Therapy and Length of Hospital Stay Following Lumbar Discectomy and Lumbar Fusion: A Retrospective Analysis. Journal of Acute Care Physical Therapy:JACPT. 2012;3(1):157–163. [Google Scholar]
- 27.Shepperd S, Parkes J, McClaren J, et al. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2004;(1):CD000313. doi: 10.1002/14651858.CD000313.pub2. [DOI] [PubMed] [Google Scholar]
- 28.Shepperd S, Doll H, Broad J, et al. Early discharge hospital at home. Cochrane Database Syst Rev. 2009;(1):CD000356. doi: 10.1002/14651858.CD000356.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shepperd S, McClaran J, Phillips CO, et al. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2010;2010(1):CD000313. doi: 10.1002/14651858.CD000313.pub3. [DOI] [PubMed] [Google Scholar]
- 30.Mauerhan DR. Relationship between length of stay and dislocation rate after total hip arthroplasty. J Arthroplasty. 2003;18(8):963–967. doi: 10.1016/s0883-5403(03)00334-6. [DOI] [PubMed] [Google Scholar]
- 31.Harvey RE. Discharge disposition following vertebroplasty. AJNR Am J Neuroradiol. 2011;32(9):1614–1616. doi: 10.3174/ajnr.A2580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.DeJong G. Physical therapy activities in stroke, knee arthroplasty, and traumatic brain injury rehabilitation: their variation, similarities, and association with functional outcomes. Phys Ther. 2011;91(12):1826–1837. doi: 10.2522/ptj.20100424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de Pablo P. Determinants of discharge destination following elective total hip replacement. Arthriti Rheum. 2004;51(6):1009–1017. doi: 10.1002/art.20818. [DOI] [PubMed] [Google Scholar]
- 34.Mallinson TR. A comparison of discharge functional status after rehabilitation in skilled nursing, home health, and medical rehabilitation settings for patients after lower-extremity joint replacement surgery. Arch of Phys Med Rehabil. 2011;92(5):712–720. doi: 10.1016/j.apmr.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 35.Waitman LR, Warren JJ, Manos EL, et al. Expressing observations from electronic medical record flowsheets in an i2b2 based clinical data repository to support research and quality improvement. AMIA Annu Symp Proc. 2011;2011:1454–1463. [PMC free article] [PubMed] [Google Scholar]
- 36.Murphy SN, Weber G, Mendis M, et al. Serving the enterprise and beyond with informatics for integrating biology and the bedside (i2b2) J Am Med Inform Assoc. 2010;17(2):124–130. doi: 10.1136/jamia.2009.000893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hamilton BGC, Sherwin F, Zielezny M, et al. uniform national data system for medical rehabilitation. In: Fuhrer MJ, editor. Rehabilitation outcomes: analysis and measurement. 1. Baltimore: Paul H. Brookes; 1987. [Google Scholar]
- 38.Kluding P, Swafford B, Cagle P, et al. Reliability, responsiveness, and validity of the Kansas University Standing Balance Scale. J Geriatr Phys Ther (2001) 2006;29(3):93–99. doi: 10.1519/00139143-200612000-00003. [DOI] [PubMed] [Google Scholar]
- 39.Peng C-YJ, Lee KL, Ingersoll GM. An Introduction to Logistic Regression Analysis and Reporting. J Educ Res. 2002;96(1) [Google Scholar]
- 40.Forrest G, Fuchs M, Gutierrez A, et al. Factors affecting length of stay and need for rehabilitation after hip and knee arthroplasty. J Arthroplasty. 1998;13(2):186–190. doi: 10.1016/s0883-5403(98)90097-3. [DOI] [PubMed] [Google Scholar]
- 41.Jones CA, Voaklander DC, Johnston DW, et al. The effect of age on pain, function, and quality of life after total hip and knee arthroplasty. Arch Intern Med. 2001;161(3):454–460. doi: 10.1001/archinte.161.3.454. [DOI] [PubMed] [Google Scholar]
- 42.Munin MC, Kwoh CK, Glynn N, et al. Predicting discharge outcome after elective hip and knee arthroplasty. Am J Phys Med Rehabil. 1995;74(4):294–301. doi: 10.1097/00002060-199507000-00006. [DOI] [PubMed] [Google Scholar]
- 43.FitzGerald JD, Boscardin WJ, Hahn BH, et al. Impact of the Medicare Short Stay Transfer Policy on patients undergoing major orthopedic surgery. Health Serv Res. 2007;42(1):25–44. doi: 10.1111/j.1475-6773.2006.00606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lim HJ, Hoffmann R, Brasel K. Factors influencing discharge location after hospitalization resulting from a traumatic fall among older persons. J Trauma. 2007;63(4):902–907. doi: 10.1097/01.ta.0000240110.14909.71. [DOI] [PubMed] [Google Scholar]
- 45.Kuisma R. A randomized, controlled comparison of home versus institutional rehabilitation of patients with hip fracture. Clin Rehabil. 2002;16(5):553–561. doi: 10.1191/0269215502cr525oa. [DOI] [PubMed] [Google Scholar]


