Abstract
Objectives:
To determine the effectiveness of balance exercises in the acute post-operative phase following total hip arthroplasty or total knee arthroplasty.
Methods:
Patients who had total hip arthroplasty (n = 30) or total knee arthroplasty (n = 33) were seen in their residence 1–2 times per week for 5 weeks. At the first post-operative home visit, patients were randomly assigned to either typical (TE, n = 33) or typical plus balance (TE + B, n = 30) exercise groups. The TE group completed seven typical surgery-specific joint range-of-motion and muscle strengthening exercises, while the TE + B group completed the typical exercises plus three balance exercises. Patients were assessed before and 5 weeks after administering the rehabilitation program using four outcome measures: (1) the Berg Balance Scale, (2) the Timed Up and Go test, (3) the Western Ontario McMaster Universities Osteoarthritis Index, and (4) the Activities-specific Balance Confidence Scale.
Results:
Post-intervention scores for all four outcome measures were significantly improved (p < 0.01) over baseline scores. Patients who participated in the TE + B group demonstrated significantly greater improvement on the Berg Balance Scale and the Timed Up and Go tests (p < 0.01).
Conclusion:
Balance exercises added to a typical rehabilitation program resulted in significantly greater improvements in balance and functional mobility compared to typical exercises alone.
Keywords: Total hip arthroplasty, total knee arthroplasty, balance exercises, Berg Balance Scale, Timed Up and Go test
Introduction
Balance is an important aspect of mobility and physical function.1–3 While the effect of hip osteoarthritis (OA) on balance is unclear, knee OA has been reported to significantly reduce standing balance in the elderly.4 Impairment in balance subsequently limits an individual’s mobility and physical function, including activities of daily living such as self-care and transfers,5 and is also associated with an increased incidence of falls.4,6,7 Patients with severe hip and knee OA who are awaiting total hip arthroplasty (THA) or total knee arthroplasty (TKA) are reported to have a higher incidence of falls compared to the general population.8 Also, one in four patients is reported to have a fall within 2 years following THA or TKA surgery.8 The cost of falling is high, both to the individual (physical and psychological trauma)5 and the health-care system (financial burden related to surgery and rehabilitation).6 At the same time, costs related to the patient’s inability to care for themselves and/or to be discharged to their home environment present additional burdens for the patient, their family, and the health-care system.
Studies examining balance following THA or TKA have produced conflicting results. Whereas Wykman and Goldie9 reported significant improvement in balance in 21 patients at 6 and 12 months following THA compared to pre-surgery measures; Nallegowda et al.10 reported no significant improvement in balance in patients following THA compared to age- and gender-matched subjects. Similarly, McChesney and Woollacott11 reported no significant difference in balance in 22 elderly subjects who were divided into age- and gender-matched groups; one group had undergone TKA and the other was a healthy control group. Furthermore, Gage et al.12 reported a decline in balance in 8 patients after 6 months of TKA compared to age-matched control subjects. Also, these studies did not report any rehabilitation measures that were used by the patients following surgery.
Following THA or TKA, a key criterion for hospital discharge, as well as post-operative rehabilitation, is optimization of the patient’s independence in self-care, transfer ability, functional mobility, and safety. When patients go home and return to the community after hospital discharge, they face physically demanding challenges such as negotiating curbs, stairs of various heights, and uneven walking surfaces. The functional challenges that patients face require good balance skills to prevent falls. Although post-operative exercise programs following THA or TKA may vary across various rehabilitation settings, these exercise programs typically emphasize joint range-of-motion (ROM) and muscle strengthening exercises for patients following TKA13–17 or THA.18,19 Balance component of mobility and physical function is not adequately addressed in these exercise programs. As a result, strategies to improve balance in patients who have undergone THA or TKA merit further study. Because balance is considered to be important for safe mobility and physical function,19 Gage et al.12 and Cavanaugh and Moy20 suggested incorporating balance-specific exercises to improve balance after TKA. However, Gage et al.12 and Cavanaugh and Moy20 did not use balance exercises in their studies.
The purpose of this study was to determine the effectiveness of balance exercises in the acute post-operative phase following THA or TKA.
Methods
A randomized controlled trial design with two groups was used for the study. Potential participants for the study were recruited between April 2006 and April 2009 from a large outpatient home physical therapy provider. At their first post-operative home visit and before any assessments, qualified participants were randomly assigned by their physical therapist to a typical exercise (TE) group or a typical exercise plus balance exercise (TE + B) group using a coin toss method of randomization. Heads was allocated to the TE group, and tails was allocated to the TE + B group to determine the group assignment of each participant. The participants flipped the coin and were assigned to the exercise group based on the outcome. The participants were blinded to their group allocation; however, the physical therapists were not blinded to the group allocation of the participants. Participants in the TE group completed joint ROM and muscle strengthening exercises, and participants in the TE + B group completed joint ROM, muscle strengthening, and additional balance exercises. All participants were assessed before (baseline) and after (follow-up) the intervention period. Assessments of participants at baseline were completed at the participant’s home by their attending physical therapist, who was one of the two participating physical therapists, having 3–4 years of experience in working with patients with THA and/or TKA. The physical therapists started administering intervention to the participants on the same day immediately after the baseline assessments were completed. The intervention program was administered for a period of 5 weeks. At the end of 5 weeks, follow-up assessments were completed by the primary investigator (one of the two participating physical therapists) within 3–6 days in a biomechanics laboratory at an academic center. At the beginning of the study, the two physical therapists visited one patient together for the first as well as the follow-up visits to ensure that similar information was conveyed to all participants with respect to instructions during assessment on outcome measures and also during implementation of the intervention. Ethics approval for the study was received from the University Research Ethics Board for Health Sciences Research Involving Human Subjects, and all participants provided written consent prior to participation.
Participants
Participants in the study were a sample of convenience of consecutive patients that were referred for outpatient home physical therapy following either THA or TKA. Patients’ charts were reviewed to determine their eligibility with respect to the operated joint, any surgery-related complications, any contraindications to exercise, and other health conditions, for participation in the study. The inclusion criteria were patients who had primary unilateral THA or TKA as a result of hip or knee joint OA and had been advised by their surgeon to weight-bear as tolerated following their surgery. Patients with revision THA or TKA, or those who had been advised by their surgeon to remain nonweight-bearing or partial weight-bearing on either the operated or nonoperated leg, were excluded. Patients with neurological conditions, such as hemiplegia, peripheral neuropathy, Parkinson’s disease, multiple sclerosis or spinal cord compression, and vestibular disorders that might affect balance, and those who were considered unable to communicate or follow instructions were also excluded from the study. A total of 63 patients (22 males, 41 females) with a mean age of 66 ± 10 years were included in the study. As advised by the surgeons, all patients were taking blood thinners for prevention of blood clots, and pain medication as needed following surgery. Some patients had other health problems such as high blood pressure and high cholesterol level which did not affect their balance or participation in the study and were taking medication for these health problems as advised by their family physicians.
Intervention
After completion of assessment by the physical therapist at the first post-operative home visit, qualified patients performed their home exercise program. Participants in the TE group completed joint ROM and muscle strengthening exercises, and those in the TE + B group completed joint ROM, muscle strengthening, and additional balance exercises (Appendix 1). Patients were seen individually at their place of residence by the physical therapist on the first or second day after hospital discharge, typically 7–10 days following their surgery. Thereafter, the patients were visited by their physical therapist once or twice per week until 5 weeks. Overall, patients received 4–6 home visits during the 5 weeks that they were seen for home visits. All patients received routine education about safety, transfers, and limb positioning, as well as typical exercises relative to their surgery. Those assigned to the TE + B group were also instructed in three balance exercises that they were to complete in addition to the typical exercises. The total duration of home exercise program for the TE + B group was expected to be slightly longer than that of the TE group. All patients were provided with exercise sheets that included written and photographed instructions for each prescribed exercise, an exercise compliance table, and a contact phone number for their physical therapist.
Patients were advised to complete 10 repetitions of each exercise three times a day and to keep a record on the compliance table. Typical joint ROM and muscle strengthening exercises were completed only on the operated leg. Each patient was taught the exercises in a sequence that the physical therapists considered most advisable—beginning with the simpler and progressing to more demanding exercises. Exercise execution and repetitions were reviewed by the physical therapist at each home visit. All participants were able to perform all exercises by the second visit. Also, all patients completed the 5-week intervention period.
Typical joint ROM and muscle strengthening exercises were chosen from therapeutic exercise literature for specifically targeting one of either hip or knee joint and muscles following THA or TKA.13–18 The three balance exercises were selected by the two physical therapists based on their experience with working with patients with THA and/or TKA with an objective to keep the balance exercises simple, safe, and easy to perform by the study participants.
Outcome measurers
Prior to the intervention, the patients were evaluated during their first home visit by their physical therapist using four outcome measures: two self-report questionnaires—the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and the Activities-specific Balance Confidence (ABC) Scale—and two performance tests, the Berg Balance Scale (BBS) and the Timed Up and Go (TUG) test. Following the 5-week intervention, all patients were evaluated by the primary investigator using the same outcome measures in a biomechanics laboratory at an academic center. Although assessment sites for the baseline (home setting) and follow-up (laboratory setting) were different, all attempts were made by the therapists to standardize the equipment and the space needed to perform the tests.
BBS
The original 14-item BBS was designed to assess balance in the elderly and has been demonstrated to be valid, reliable, and responsive.21 It includes 14 simple balance tasks, which are scored on a 5-point ordinal scale (0, 1, 2, 3, and 4), with a maximum total score of 56. Higher scores on the BBS indicate better balance. The BBS is a commonly used clinical test of balance in which all 14 performance tasks focus on balance21,22 and has been previously used to assess balance in patients following hip fracture23,24 and knee OA.25
TUG
The TUG is a test of functional mobility completed using a single chair and a 3-m walkway. It combines standing up, walking, turning around, and sitting down. The TUG test has been reported to be reliable, valid, and responsive for assessing functional mobility in a frail elderly population.26 The subject is timed while he/she rises from an armchair, walks 3 m, turns around, walks back to the chair, and sits back down. The faster the time, the better is the subject’s physical function. Additional information on whether the subject used any assistive devices such as cane, used any footwear, or required any other assistance is recorded. The test is simple, quick, and requires no special equipment and has been used to assess balance in the elderly27 and in the middle-aged women following interventions to improve balance.28
WOMAC
The WOMAC is a self-administered, disease-specific questionnaire used to assess patients having OA of the hip and/or knee and has been demonstrated to be valid, reliable, and responsive.29 It consists of 24 questions distributed among three subscales: (1) a pain subscale with 5 questions, (2) a stiffness subscale with 2 questions, and (3) a physical function subscale with 17 questions. The WOMAC allows patients to make their responses using 5-point scales (0, 1, 2, 3, 4) with the total possible score being 96. Higher scores on the WOMAC indicate greater pain and stiffness, and greater difficulty in performing selected functional activities. While the WOMAC requests information from patients about their physical function rather than balance per se, it is very commonly used to assess patients with THA or TKA.15,17,19,29 Although typically reported as a total score, the strong relationship between the pain and functional subscales of the WOMAC reported by Stratford et al.30 suggests the use of function subscale score of the WOMAC in place of the total score. Subsequently, the WOMAC-function subscale scores were used in all analyses in this study.
ABC
The ABC was developed by Powell and Myers31 and was demonstrated to be valid, reliable, and responsive to assess the level of patient’s balance confidence in performing specific activities. The ABC has 16 items and is scored on a 0%–100% response scale. An average of scores for all items is calculated as patient’s total ABC score. The ABC is simple and easy to understand and takes 5–10 min to complete and score. The ABC has been used to assess fall-related self-efficacy in elderly patients after hip fracture.32
Statistical analyses
Mann-Whitney U tests were used to compare subjects who completed testing on the baseline assessment but not on the follow-up assessment (drop-outs) with the subjects who completed testing on both test occasions (completers). Subsequent analysis was confined to subjects who completed testing on both occasions. A two-way analysis of variance (ANOVA; two surgical groups (TKA, THA) by two exercise groups (TE, TE + B)) was used to compare the surgical and exercise groups’ age, height, and mass, and the baseline outcome scores.
Three-way ANOVA tests with a repeated measure were used to examine each of the four outcome measures (two surgical groups (THA, TKA) by two exercise groups (TE, TE + B) by two occasions (baseline, follow-up)). These ANOVAs were preceded by Levine’s test to examine the homogeneity of variance assumption. All statistical tests were completed using STATISTICA33 and used the 0.05 level to denote statistical significance. Statistically significant F ratios were explored further using Bonferroni post hoc tests. For the WOMAC, only scores on the WOMAC-function subscale were used for analyses.
A priori power analysis using data from a previous study with subjects with TKA34 indicated that a sample of 20 participants in each group would have a power of 0.80 to detect a difference of five standard deviations between groups on the BBS at a significance level of 0.05. Patients with THA and TKA were pooled together to provide an adequate sample size in this study.
Results
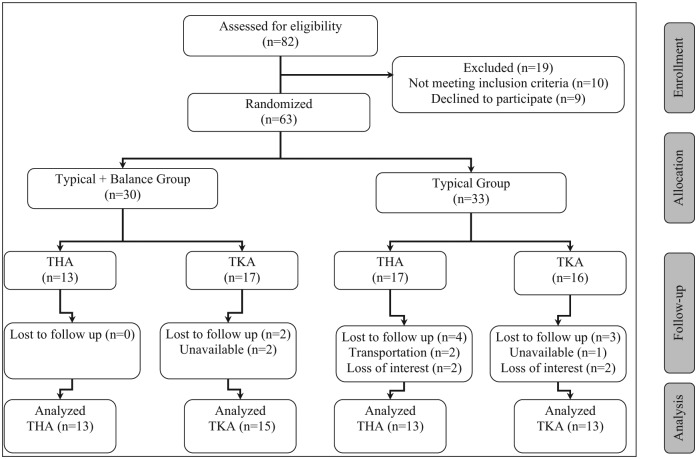
A total of 63 patients recruited for the study were randomly assigned to the TE or the TE + B group. Of these, 30 patients with THA and 33 patients with TKA belonged to the TE group (n = 33) or the TE + B group (n = 30). A total of 54 patients completed the four outcome measures on both occasions and were included in the statistical analysis (Figure 1). Demographic information for patients who completed testing on both occasions is presented in Table 1. No statistically significant differences in age, height, or body mass were observed between the surgical (THA, TKA) and exercise (TE, TE + B) groups on the baseline scores (p > 0.05).
Figure 1.
Flow diagram of participants’ progress through the phases of randomized trial.
Table 1.
Baseline demographic information of participants in the two surgical and the two exercise groups (n = 54).
| THA | TKA | TE | TE + B | |
|---|---|---|---|---|
| Sample size (n) | 26 | 28 | 26 | 28 |
| Age (years) | 68 ± 8 | 64 ± 10 | 67 ± 9 | 66 ± 10 |
| Height (cm) | 165 ± 8 | 166 ± 12 | 165 ± 12 | 166 ± 8 |
| Mass (kg) | 78 ± 19 | 87 ± 20 | 83 ± 20 | 82 ± 20 |
| Visits | 4 | 6 | 5 ± 1 | 5 ± 1 |
THA: total hip arthroplasty; TKA: total knee arthroplasty; TE: typical exercise group; TE + B: typical plus balance exercise group.
Scores on the BBS, TUG, WOMAC-function, and ABC for the TE and TE + B groups are presented in Table 2. Only the TUG scores were characterized by a significant Levine’s test (p < 0.05). Subsequently, variance stabilization transformation (natural logarithmic)35 was used for the TUG scores to meet the necessary assumption of homogeneity of variances. The three-way ANOVAs for the four outcome measures produced several statistically significant F ratios (Table 3), summarized as follows. First, the differences between the groups, the TE + B group demonstrated significantly greater improvement from the baseline to follow-up than did the TE group on the BBS (p < 0.01; Figure 2) and the TUG (p < 0.01; Figure 3). Second, differences between the groups with respect to occasion, the follow-up scores on the BBS, TUG, WOMAC-function, and ABC were significantly improved over the baseline scores on all four ANOVAs (p < 0.01).
Table 2.
Summary of scores for the Typical Exercise and Typical plus Balance Exercise groups on the outcome measures at baseline and follow-up.
| Occasion | Baseline |
Follow-up |
||
|---|---|---|---|---|
| Exercise group | TE | TE + B | TE | TE + B |
| BBS (0–56) | 37 ± 10 | 34 ± 7 | 48 ± 6 | 53 ± 6 |
| TUG (s) | 32 ± 17 | 48 ± 26 | 15 ± 5 | 13 ± 4 |
| WOMAC-function (0–68) | 36 ± 11 | 37 ± 11 | 16 ± 10 | 14 ± 13 |
| ABC (0–100) | 37 ± 19 | 36 ± 24 | 69 ± 23 | 74 ± 23 |
TE: typical exercise group; TE + B: typical plus balance exercise group; BBS: Berg Balance Scale; TUG: Timed Up and Go test; WOMAC-function: Western Ontario and McMaster Universities Osteoarthritis Index physical function subscale; ABC: Activities-specific Balance Confidence Scale.
Table 3.
Summary of the F ratios and p values produced by the three-way ANOVA tests for the four outcome measures.
| Outcome measure | Effect | F ratio | p value |
|---|---|---|---|
| BBS | Surgerya | 0.36 | 0.54 |
| Exercise groupb | 1.12 | 0.29 | |
| Occasionc | 221.42 | 0.000* | |
| Surgery × exercise group | 1.27 | 0.26 | |
| Surgery × occasion | 0.45 | 0.50 | |
| Exercise group × occasion | 7.19 | 0.009* | |
| Surgery × exercise group × occasion | 1.86 | 0.17 | |
| TUG | Surgerya | 0.11 | 0.73 |
| Exercise groupb | 0.28 | 0.59 | |
| Occasionc | 219.58 | 0.000* | |
| Surgery × exercise group | 0.87 | 0.35 | |
| Surgery × occasion | 0.00 | 0.98 | |
| Exercise group × occasion | 8.76 | 0.004* | |
| Surgery × exercise group × occasion | 0.49 | 0.48 | |
| WOMAC-function | Surgerya | 3.90 | 0.053 |
| Exercise groupb | 0.11 | 0.73 | |
| Occasionc | 165.41 | 0.000* | |
| Surgery × exercise group | 0.03 | 0.85 | |
| Surgery × occasion | 0.22 | 0.64 | |
| Exercise group × occasion | 0.71 | 0.40 | |
| Surgery × exercise group × occasion | 1.31 | 0.25 | |
| ABC | Surgerya | 2.37 | 0.12 |
| Exercise groupb | 0.49 | 0.48 | |
| Occasionc | 137.27 | 0.000* | |
| Surgery × exercise group | 0.37 | 0.54 | |
| Surgery × occasion | 0.07 | 0.78 | |
| Exercise group × occasion | 0.47 | 0.49 | |
| Surgery × exercise group × occasion | 0.64 | 0.42 |
BBS: Berg Balance Scale; TUG: Timed Up and Go test; WOMAC-function: Western Ontario and McMaster Universities Osteoarthritis Index physical function subscale; ABC: Activities-specific Balance Confidence Scale.
Surgery effect: total hip arthroplasty versus total knee arthroplasty.
Exercise group effect: typical exercise group versus typical plus balance exercise group.
Occasion effect: baseline versus follow-up.
p < 0.01.
Figure 2.
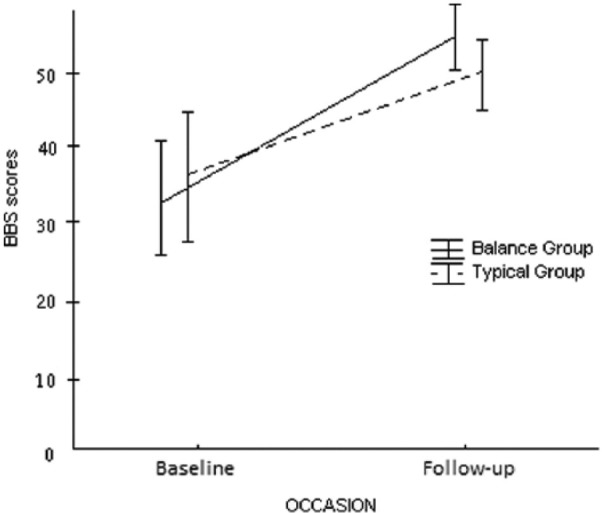
Exercise group by occasion interaction for the exercise groups on the Berg Balance Scale (BBS).
Figure 3.
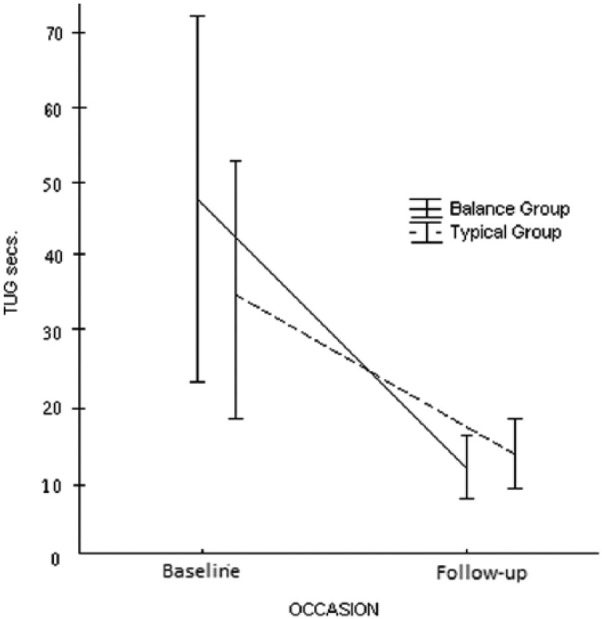
Exercise group by occasion interaction for the exercise groups on the Timed Up and Go (TUG) test.
No significant differences in age, height, body mass, or performances on the BBS, TUG, WOMAC-function, and ABC (baseline) were observed between the 9 participants who dropped out and the 54 participants who completed the study (p > 0.05).
Discussion
Following THA or TKA, patients who received home physical therapy irrespective of their exercise groups demonstrated significant improvement on all four functionally oriented tests. Although this finding supports the traditional clinical belief that balance will improve following a typical exercise program alone, this study did observe that those who performed balance exercises in addition to typical exercises demonstrated significantly greater improvement in the balance-oriented tests (BBS and TUG) than those who performed typical joint ROM and muscle strengthening exercises alone. These results suggest that should the therapist believe that balance is of key importance for their patient, the use of simple balance exercises can readily lead to improvement in this component of many functional activities as determined within a relatively short period of 5 weeks.
Similar improvement in balance has been reported by Liao et al.36 in patients with knee replacement after administering a balance exercise program. However, the study by Liao et al.36 included patients who had surgery 2 months before they started participation in the exercise program, and therefore, the patients’ TUG scores were lower at baseline assessment (12 ± 1 and 13 ± 2 for the control and experimental groups, respectively). In this study, the patients were recruited 7–10 days after the THA or TKA surgery, and therefore, the patients’ TUG scores were comparatively higher at baseline assessment. At the completion of this study, the patients’ TUG scores had significantly reduced. This study was completed before the end of 2 months’ duration following THA or TKA surgery.
Improvements in balance as observed in this study have also been reported in previous studies following balance intervention in patients with other health conditions. Diracoglu et al.37 in an 8-week study reported improvement in balance from kinesthesia and balance exercises added to strengthening exercises as compared to strengthening exercises alone in female patients with knee OA. Williams et al.38 also reported improvement in balance following a home-based balance exercise program in women with lower limb OA or rheumatoid arthritis on balance measures such as functional reach test, but no differences were observed on the WOMAC-function scores. Hiroyuki3 reported significant improvement in balance measures such as one leg stand test, functional reach test, and the TUG following balance and gait exercise in the frail elderly population. Similar improvements in balance following balance exercises have also been reported in patients with stroke39 and multiple sclerosis.40
No significant differences were observed between the exercise groups on the WOMAC-function or the ABC. This finding may reflect the lack of balance orientation of these outcome measures compared to the BBS and the TUG. The BBS is designed to assess balance while performing 14 functional tasks, and performance on the TUG relies heavily on the patient’s balance during transfers and walking. The WOMAC-function and the ABC, on the other hand, are self-report questionnaires which rely on the patient’s subjective assessment of their performance, without actually requiring the patient to perform the tasks described in the questions,41–43 not all of which include a balance-related component.
In this study, no differences were observed between the THA and the TKA patients on the outcome measures. Subsequently, data for THA or TKA patients were pooled together. Previous studies have reported no differences between patients undergoing THA and those undergoing TKA at 6-month follow-up after surgery.44,45 Whereas previous studies have used typical joint ROM and muscle strengthening exercises following THA or TKA,13–19 to our knowledge, this study is thought to be the first to assess the utility of adding balance exercises for these patients in the acute post-operative phase following THA or TKA. We chose to add balance exercises to a typical acute post-operative exercise program, rather than replacing some of the typical exercises with balance exercises. Liao et al.36 have used a similar strategy to administer balance exercise program to the patients in experimental group following TKA. Since neither the typical exercises nor the balance exercises used following THA or TKA are standardized among therapists, it was unclear which exercises would best be replaced in order to match the two exercise programs on the number of exercises to be completed. Furthermore, we believed that a treatment effect that could be confidently linked to the balance exercises alone needed to be demonstrated before attempting to replace some of the typical ROM and muscle strengthening exercises with balance exercises. As a result, the balance exercises–added option was considered to be the most practical means to initially assess the viability of balance exercises and to optimize the chances of finding a balance effect if it existed.
The seven typical joint ROM and muscle strengthening exercises and three balance exercises were selected by two physical therapists who routinely provide physical therapy to THA or TKA patients following surgery and who both had 3–4 years of clinical experience. They were guided by the exercises utilized in previous studies,13–18 as well as their own clinical experience. In this study, the same three balance exercises were used for patients following THA or TKA surgery. These exercises were selected for their simplicity and the ability of all patients to complete them. All patients were able to perform all of the typical exercises, and patients in the typical plus balance exercise group were able to perform all of the balance exercises for the recommended 10 repetitions and frequency of three times per day by their second home visit. All patients reported completion of all exercises at the recommended frequency and number of repetitions with the exception of three patients (one in the typical plus balance exercise group and two in the typical exercise group) who did not perform exercises for a day due to a prior engagement.
Although nine patients completed testing at baseline, but not at follow-up, neither their demographic variables nor their functional scores at baseline differed significantly from those of patients who completed the study. Also, the nine patients who dropped out were not included in the final analyses. For these reasons, we believe that the patients who dropped out of the study did not affect the outcome of the study. From a clinical standpoint, patients undergoing THA or TKA tend to be elderly, have other medical conditions, and have transportation and mobility issues which may contribute to their dropping out. Previous investigators have reported similar proportions of drop-outs during the post-operative rehabilitation phases.16,17,36,43,46
Several limitations of this study need to be recognized. Participants in the study comprised a sample of convenience that was referred to home-based, outpatient physical therapy within a limited geographical area. Furthermore, all patients had been advised by their physician to weight-bear as tolerated on the operated limb; nonweight-bearing or partial weight-bearing patients were excluded. The assessor was not blinded to the patients’ exercise group assignment during assessment at follow-up, and the assessments at follow-up were carried out in a laboratory setting as opposed to the patient’s home setting at baseline. Although assessments were done by two different assessors at baseline and by one at follow-up, interrater reliability of outcome measures was not evaluated before completing the assessments. The total duration for home exercise program for patients in the typical plus balance exercise group was slightly longer than those in the typical exercise group to accommodate the additional balance exercises. In addition, this study examined the effectiveness of balance exercises after a relatively short-term intervention of 5 weeks in the acute post-operative phase following THA or TKA. Pre-surgical and longer term (12–24 weeks post-surgery) assessments were not completed. The involvement of the hip and knee joint proprioception in maintaining balance in patients was not the object and so not assessed in this study.
In conclusion, this study suggests that balance exercises in addition to typical joint ROM and muscle strengthening exercises in the acute post-operative phase following THA or TKA can result in significantly greater improvements in balance with a 5-week intervention period, compared to a typical post-operative physical therapy program alone. In clinical situations where the therapist considers improvement in balance to be important, balance exercises such as those used in this study may provide a practical means to rapidly improve balance.
Acknowledgments
The authors would like to thank all participants who took part in the study.
Appendix
Appendix 1.
Rehabilitation program (duration: 10 repetitions, 3 times a day).
| Typical exercises for THA | Typical exercises for TKA | Balance exercises for THA and TKA |
|---|---|---|
| 1. Assisted knee flexion with a strap in lying 2. Knee extension on a towel roll in lying 3. Isometric quadriceps in lying 4. Hip abduction in standing with holding a stable support 5. Hip extension in standing with holding a stable support 6. Hip flexion in standing with holding a stable support 7. Knee flexion in standing with holding a stable support |
1. Assisted knee flexion with a strap in lying 2. Knee extension on a towel roll in lying 3. Knee flexion by sliding foot on bed in lying 4. Straight leg raises in lying 5. Assisted knee extension with strap around the foot in lying 6. Knee extension in sitting 7. Knee flexion by sliding foot on the floor in sitting |
1. Rotate trunk clockwise and then in anti-clockwise direction in standing without support 2. Lunge in walk standing position without support and then repeat with the other leg forward 3. Shift weight to one side in a stride standing position without support and then repeat on the other side |
THA: total hip arthroplasty; TKA: total knee arthroplasty.
Footnotes
Declaration of conflicting interests: The authors report no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Study Registration: ClinicalTrials.gov Protocol Registration System; ClinicalTrials.gov ID: NCT01555307; Protocol ID: R-06-461.
References
- 1. Brouwer B, Musselman K, Culham E. Physical function and health status among seniors with and without a fear of falling. Gerontology 2004; 50: 135–141. [DOI] [PubMed] [Google Scholar]
- 2. Cho BL, Scarpace D, Alexander NB. Tests of stepping as indicators of mobility, balance, and fall risk in balance-impaired older adults. J Am Geriatr Soc 2004; 52: 1168–1173. [DOI] [PubMed] [Google Scholar]
- 3. Hiroyuki S, Uchiyama Y, Kakurai S. Specific effects of balance and gait exercises on physical function among the frail elderly. Clin Rehabil 2003; 17: 472–479. [DOI] [PubMed] [Google Scholar]
- 4. Wegener L, Kisner C, Nichols D. Static and dynamic balance responses in persons with bilateral knee osteoarthritis. J Orthop Sports Phys Ther 1997; 25: 13–18. [DOI] [PubMed] [Google Scholar]
- 5. Duncan PW, Chandler J, Studenski S, et al. How do physiological components of balance affect mobility in elderly men? Arch Phys Med Rehabil 1993; 74: 1343–1349. [DOI] [PubMed] [Google Scholar]
- 6. Carroll NV, Slattum PW, Cox FM. The cost of falls among the community-dwelling elderly. J Manag Care Pharm 2005; 11: 307–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Robbins AS, Rubenstein LZ, Josephson KR, et al. Predictors of falls among elderly people: results of two population-based studies. Arch Intern Med 1989; 149: 1628–1633. [PubMed] [Google Scholar]
- 8. Mitchell SY, McCaskie AW, Francis RM, et al. P69 Falls in patients with hip and knee osteoarthritis: the impact of joint replacement surgery. J Bone Joint Surg Br 2008; 90B: 385. [Google Scholar]
- 9. Wykman A, Goldie I. Postural stability after total hip replacement. Int Orthop 1989; 13: 235–238. [DOI] [PubMed] [Google Scholar]
- 10. Nallegowda M, Singh U, Bhan S, et al. Balance and gait in total hip replacement: a pilot study. Am J Phys Med Rehabil 2003; 82: 669–677. [DOI] [PubMed] [Google Scholar]
- 11. McChesney JW, Woollacott MH. The effect of age-related declines in proprioception and total knee replacement on postural control. J Gerontol A Biol Sci Med Sci 2000; 55: M658–M666. [DOI] [PubMed] [Google Scholar]
- 12. Gage WH, Frank JS, Prentice SD, et al. Postural responses following a rotational support surface perturbation, following knee joint replacement: frontal plane rotations. Gait Posture 2008; 27: 286–293. [DOI] [PubMed] [Google Scholar]
- 13. Beaupre LA, Davies DM, Jones CA, et al. Exercise combined with continuous passive motion or slider board therapy compared with exercise only: a randomized controlled trial of patients following total knee arthroplasty. Phys Ther 2001; 81: 1029–1037. [PubMed] [Google Scholar]
- 14. Davies DM, Johnston DW, Beaupre LA, et al. Effect of adjunctive range-of-motion therapy after primary total knee arthroplasty on the use of health services after hospital discharge. Can J Surg 2003; 46: 30–36. [PMC free article] [PubMed] [Google Scholar]
- 15. Moffet H, Collet JP, Shapiro SH, et al. Effectiveness of intensive rehabilitation on functional ability and quality of life after first total knee arthroplasty: a single-blind randomized controlled trial. Arch Phys Med Rehabil 2004; 85: 546–556. [DOI] [PubMed] [Google Scholar]
- 16. Kramer JF, Speechley M, Bourne R, et al. Comparison of clinic and home based rehabilitation programs after total knee arthroplasty. Clin Orthop Relat Res 2003; 410: 225–234. [DOI] [PubMed] [Google Scholar]
- 17. Franklin PD, McLaughlin J, Boisvert CB, et al. Pilot study of methods to document quantity and variation of independent patient exercise and activity after total knee arthroplasty. J Arthoplasty 2006; 21(Suppl. 2): 157–163. [DOI] [PubMed] [Google Scholar]
- 18. Trudelle-Jackson E, Smith SS. Effects of a late-phase exercise program after total hip arthroplasty: a randomized controlled trial. Arch Phys Med Rehabil 2004; 85: 1056–1062. [DOI] [PubMed] [Google Scholar]
- 19. Sashika H, Matsuba Y, Watanabe Y. Home program of physical therapy: effect on disabilities of patients with total hip arthroplasty. Arch Phys Med Rehabil 1996; 77: 273–277. [DOI] [PubMed] [Google Scholar]
- 20. Cavanaugh JT, Moy RJ. Balance and postoperative lower extremity joint reconstruction. Orthop Phys Ther Clin N Am 2002; 11: 75–99. [Google Scholar]
- 21. Berg K, Wood-Dauphinee S, Williams JI, et al. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can 1989; 41: 304–311. [Google Scholar]
- 22. Muir SW, Berg K, Chesworth B, et al. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther 2008; 88: 449–459. [DOI] [PubMed] [Google Scholar]
- 23. Mendelsohn ME, Overend TJ, Connelly DM, et al. Improvement in aerobic fitness during rehabilitation after hip fracture. Arch Phys Med Rehabil 2008; 89: 609–617. [DOI] [PubMed] [Google Scholar]
- 24. Kulmala J, Sihvonen S, Kallinen M, et al. Balance confidence and functional balance in relation to falls in older persons with hip fracture history. J Geriatr Phys Ther 2007; 30: 114–120. [DOI] [PubMed] [Google Scholar]
- 25. Sun SF, Hsu CW, Hwang CW, et al. Hyaluronate improves pain, physical function and balance in the geriatric osteoarthritic knee: a 6-month follow-up study using clinical tests. Osteoarthritis Cartilage 2006; 14: 696–701. [DOI] [PubMed] [Google Scholar]
- 26. Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991; 39: 142–148. [DOI] [PubMed] [Google Scholar]
- 27. Berger L, Klein C, Commandeur M. Evaluation of the immediate and midterm effects of mobilization in hot spa water on static and dynamic balance in elderly subjects. Ann Readapt Med Phys 2008; 51: 84–95. [DOI] [PubMed] [Google Scholar]
- 28. Bouillon LE, Sklenka DK, Driver AC. Comparison of training between 2 cycle ergometers on dynamic balance for middle-aged women. J Sport Rehabil 2009; 18: 316–326. [DOI] [PubMed] [Google Scholar]
- 29. Bellamy N, Buchanan WW, Goldsmith H, et al. Validation study of WOMAC: a health status instrument for measuring clinically-important patient-relevant outcomes following total hip or knee arthroplasty in osteoarthritis. J Orthop Rheumat 1988; 1: 95–108. [PubMed] [Google Scholar]
- 30. Stratford PW, Dogra M, Woodhouse L, et al. Validating self-report measures of pain and function in patients undergoing hip and knee arthroplasty. Physiother Can 2009; 61: 189–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) scale. J Gerontol A Biol Sci Med Sci 1995; 50: M28–M34. [DOI] [PubMed] [Google Scholar]
- 32. Petrella PJ, Payne M, Myers A, et al. Physical function and fear of falling after hip fracture rehabilitation in the elderly. Am J Phys Med Rehabil 2000; 79: 154–160. [DOI] [PubMed] [Google Scholar]
- 33. StatSoft Inc. STATISTICA 7.0. Tulsa, OK: StatSoft Inc, 2000. [Google Scholar]
- 34. Seely T. Standing balance before and after total knee arthroplasty: a pilot study. Master’s thesis, University of Western Ontario, London, ON, Canada, 2005. [Google Scholar]
- 35. Mendoza-Nunez VM, Garcia-Sanchez A, Sanchez-Rodriguez M, et al. Overweight, waist circumference, age, gender, and insulin resistance as risk factors for hyperleptinemia. Obes Res 2002; 10: 253–259. [DOI] [PubMed] [Google Scholar]
- 36. Liao CD, Liou TH, Huang YY, et al. Effects of balance training on functional outcome after total knee replacement in patients with knee osteoarthritis: a randomized controlled trial. Clin Rehabil 2013; 28: 697–709. [DOI] [PubMed] [Google Scholar]
- 37. Diracoglu D, Aydin R, Baskent A, et al. Effects of kinesthesia and balance exercises in knee osteoarthritis. J Clin Rheumatol 2005; 11: 303–310. [DOI] [PubMed] [Google Scholar]
- 38. Williams SB, Brand CA, Hill KD, et al. Feasibility and outcomes of a home-based exercise program on improving balance and gait stability in women with lower-limb osteoarthritis or rheumatoid arthritis: a pilot study. Arch Phys Med Rehabil 2010; 91: 106–114. [DOI] [PubMed] [Google Scholar]
- 39. Smania N, Picelli A, Gandolfi M, et al. Rehabilitation of sensorimotor integration deficits in balance impairment of patients with stroke hemiparesis: a before/after pilot study. Neurol Sci 2008; 29: 313–319. [DOI] [PubMed] [Google Scholar]
- 40. Cattaneo D, Jonsdottir J, Zocchi M, et al. Effects of balance exercises on people with multiple sclerosis: a pilot study. Clin Rehabil 2007; 21: 771–781. [DOI] [PubMed] [Google Scholar]
- 41. Kennedy D, Stratford PW, Pagura SM, et al. Comparison of gender and group differences in self-report and physical performance measures in total hip and knee arthroplasty candidates. J Arthroplasty 2002; 17: 70–77. [DOI] [PubMed] [Google Scholar]
- 42. Stratford PW, Kennedy D, Pagura SM, et al. The relationship between self-report and performance-related measures: questioning the content validity of timed tests. Arthritis Rheum 2003; 49: 535–540. [DOI] [PubMed] [Google Scholar]
- 43. Rejeski WJ, Ettinger WH, Jr, Schumaker S, et al. Assessing performance-related disability in patients with knee osteoarthritis. Osteoarthritis Cartilage 1995; 3: 157–167. [DOI] [PubMed] [Google Scholar]
- 44. Jones CA, Voaklander DC, Suarez-Almazon ME. The effect of age on pain, function and quality of life after total hip and knee arthroplasty. Arch Intern Med 2001; 161: 454–460. [DOI] [PubMed] [Google Scholar]
- 45. Mahomed NN, Liang MH, Cook EF, et al. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol 2002; 29: 1273–1279. [PubMed] [Google Scholar]
- 46. Galea MP, Levinger P, Lythgo N, et al. A targeted home and center based exercise program for people after total hip replacement: a randomized clinical trial. Arch Phys Med Rehabil 2008; 89: 1442–1447. [DOI] [PubMed] [Google Scholar]