Abstract
Purpose:
To examine the impact of a Continuum of Care Resident Pharmacist on (1) heart failure 30-day hospital readmissions and (2) compliance with Joint Commission Heart Failure core measure 1 at a community hospital.
Methods:
The Continuum of Care Network led by a Continuum of Care Resident Pharmacist was established in August 2011. The Continuum of Care Resident Pharmacist followed Continuum of Care Network patients and retrospectively collected data from August 2011 to December 2012. Thirty-day readmission rates for Continuum of Care Network heart failure patients versus non-Continuum of Care Network heart failure patients were compared and analyzed. Joint Commission Heart Failure core measure 1 compliance rates were retrospectively collected from January 2011 and compared to data after establishment of the Continuum of Care Network.
Results:
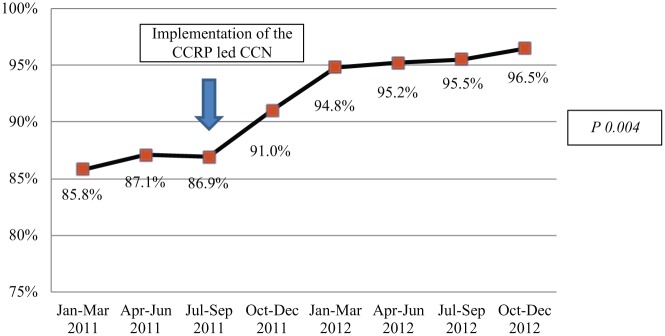
In all, 162 Continuum of Care Network patients and 470 non-Continuum of Care Network patients were discharged with a diagnosis of heart failure from August 2011 to December 2012. Continuum of Care Network heart failure patients had a lower 30-day all-cause readmission rate compared to non-Continuum of Care Network heart failure patients (12% versus 24%, respectively; p = 0.005). In addition, Heart Failure core measure 1 compliance rates improved from the 80th percentile to the 90th percentile after implementation of the Continuum of Care Network (p = 0.004). The top three interventions performed by the Continuum of Care Resident Pharmacist were discharge counseling (74.1%), providing a MedActionPlan™ (68.5%), and resolving medication reconciliation discrepancies (64.8%).
Conclusion:
The study findings suggest that a Continuum of Care Resident Pharmacist contributed to lowered heart failure readmission rates and improved Heart Failure core measure 1 compliance rates. Future randomized, controlled trials are needed to confirm these findings.
Keywords: Hospital readmissions, transitions of care, discharge instructions, heart failure
Background
With the enactment of the Patient Protection and Affordable Care Act in 2010, the Centers for Medicare and Medicaid Services (CMS) was directed to implement two programs that would affect hospitals nationwide. The first initiative was the Hospital Readmissions Reduction Program (HRRP), which required CMS to reduce payments to hospitals with excess readmissions beginning on 1 October 2012.1 The second was the Hospital Value-Based Purchasing (HVBP) program, which rewarded acute care hospitals with incentive payments for quality of care.2
Recognizing the opportunity for the expansion of the non-traditional pharmacist role in light of the impending financial incentives to improve patient quality of care, the visionaries at Sharp HealthCare and Touro University California College of Pharmacy collaborated to establish a postgraduate year 2 pharmacy residency in Continuum of Care. With the support of the leadership team at Sharp HealthCare, the inaugural Continuum of Care Resident Pharmacist (CCRP) established the Continuum of Care Network (CCN) in August 2011. The CCN is a patient-centered transitional care model based at Sharp Memorial Hospital (SMH) and includes hospitalists, specialists, case managers, social workers, bedside nurses, heart failure (HF) navigators, diabetic educators, dietitians, physical therapists, respiratory therapists, and financial counselors. The CCRP leads the CCN to ensure that care is coordinated between the various healthcare providers upon hospital admission through discharge to home.
The American Geriatrics Society defines transitions of care as a set of actions designed to ensure the coordination and continuity of healthcare as patients transfer between locations or different levels of care within the same location.3 At SMH, patients who enter the CCN are followed by the CCRP from hospital admission to post-discharge. During the inaugural year of the CCN, the CCRP focused on HF patients who were discharged from hospital to home.
The decision to focus on HF patients was financially justified by the HRRP and HVBP. In fiscal year 2013, the HRRP only applied to patients with a diagnosis of HF, acute myocardial infarction, or pneumonia. At SMH, the readmission rate (RR) for HF patients was approximately 22% at the time, which was no different from the national average.4 The HVBP program is based on eight patient experience of care measures and 12 clinical process of care measures with the latter accounting for 70% of the total performance score. At SMH, the process of care measure with the lowest score was HF discharge instructions. CMS and Joint Commission have similar national hospital performance measures and thus shared common documentation for this HF core measure, discharge instructions (Heart Failure core measure 1 (HF-1)). While the national achievement threshold was 90.8%,5 SMH’s HF-1 was 83.5% at baseline (1 July 2009 to 31 March 2010). Therefore, decreasing the HF RR and improving compliance with HF-1 became the CCN’s primary outcome goals.
While the role of pharmacists in transitions of care has been previously described,6,7 their impact on hospital readmissions is unclear.8–13 Although some hospitals have successfully incorporated pharmacists in the patient discharge process and subsequently demonstrated fewer 30-day emergency department (ED) visits and/or readmissions compared to usual care,8,9 others have shown no difference in healthcare utilization after discharge.10–13 In addition, all these studies were conducted at large academic teaching hospitals with results that may not be generalizable to community hospitals.
Finally, there is a scarcity of research on the role of pharmacists in improving compliance to HF core measures. A single study found that a multidisciplinary team that included pharmacists may improve Joint Commission core measures for hospitalized patients with HF.14 Due to documentation issues related to medication reconciliation, the percentage of discharge instructions remained lower than anticipated.14 Warden et al.15 found that pharmacist involvement in medication reconciliation and discharge counseling for HF patients was associated with a significant increase in adherence to Joint Commission discharge instructions (83% vs 100%, p = 0.007). However, both these studies were done at teaching hospitals in which pharmacists collaborated with multidisciplinary teams. To our knowledge, there are no published studies that have examined the impact of a single pharmacist on HF 30-day RRs and compliance to HF-1 at a community hospital. The purpose of this study was to examine the impact of a CCRP on (1) HF 30-day all-cause hospital readmissions and (2) compliance with HF-1 at a single community hospital.
Methods
Study setting
Sharp HealthCare is an integrated regional healthcare delivery system in San Diego, CA, USA. It includes four acute care hospitals, three specialty hospitals, two affiliated medical groups, a health plan, home healthcare, and three skilled nursing facilities.
This study was conducted at one of the four acute care hospitals, SMH. SMH is a not-for-profit community hospital with 368 beds. The pharmacy department utilizes decentralized pharmacists who are actively involved in direct patient care activities including pain management, anticoagulation services, antibiotic stewardship, and pharmacokinetic dosing. Prior to the implementation of the CCN, pharmacists were not involved in transitions of care processes.
Study participants
Patients were eligible for this study if they were admitted for suspected HF exacerbation at SMH between August 2011 and December 2012, discharged to home, and at least 18 years old. Patients who were discharged with hospice or to a skilled nursing facility, transferred to another acute care hospital, or left against medical advice were excluded. Only patients with a final billing code for HF were included in the analysis. CCN patients were retrospectively defined as patients who had been discharged with a billable code for HF and had been seen by the CCRP, while non-CCN patients had a similarly verifiable HF discharge diagnosis but were not seen by the CCRP. The study was approved by the Sharp HealthCare Institutional Review Board.
CCRP role
Each morning, Monday through Friday, the HF Clinical Nurse Specialist provided the CCRP a list of patients who were admitted for suspected HF. The CCRP reviewed each patient’s electronic chart and performed the following:
- Admission medication review
- The CCRP reviewed the documented medication history and compared it to the list of medications in the history and physical as dictated by the hospitalist.
- Upon finding discrepancies, the CCRP interviewed the patient, patient’s family, and/or called the patient’s pharmacy and/or primary care provider to verify the patient’s medication history.
- The CCRP updated the medication history in the electronic health chart and communicated discrepancies to the hospitalist.
- Daily monitoring
- The CCRP reviewed and assessed pertinent laboratories (e.g. comprehensive metabolic panel, microbiology reports, toxicology, and complete blood count), echocardiograms, medication regimens, and provided clinical recommendations to the hospitalist and/or specialist when appropriate.
- Discharge medication review
- Prior to the patient’s discharge, the CCRP reviewed the list of anticipated discharge medications and assessed the clinical appropriateness, dosing, and accessibility.
- The CCRP worked with the social worker, case manager, and hospitalist to secure appropriate medications for the patient.
- For a suspected non-adherent patient, the CCRP faxed the discharge medication prescriptions to the adjacent community pharmacy for delivery of medications to the patient at bedside.
- Discharge counseling
- The CCRP utilized the MedActionPlan™, a proprietary web-based tool to provide a patient-friendly medication schedule.
- Medication education was provided to the patient and/or care partner with emphasis on newly prescribed medications.
- This medication education supplemented the usual discharge education provided by the bedside nurse.
- Post-discharge follow-up
- The CCRP contacted the patient within 5 working days post-discharge to identify medication access issues, assess for medication side effects, and evaluate medication adherence.
- Based on clinical judgment, the CCRP offered home visits to patients who did not appear to understand their medication lists at discharge. These patients were often elderly, lived alone, and expressed confusion about their medications upon discharge.
Outcome measures
The data for HF 30-day RRs were collected from August 2011 to December 2012. At SMH, a readmission was defined as a second admission to one of four Sharp HealthCare hospitals within 30 days following a confirmed HF discharge from SMH. RRs were calculated by dividing the total number of patients readmitted within 30 days of discharge by the total number of hospital discharges for HF.
HF-1 states that
heart failure patients discharged home with written instructions or educational material given to patient or caregiver at discharge or during the hospital stay addresses all of the following: discharge medications, activity level, diet, follow-up appointment, weight monitoring, and what to do if symptoms worsen.16
HF-1 compliance rates were retrospectively collected from January 2011 to June 2011 and compared to data after establishment of the CCN from August 2011 to December 2012.
Additional data were collected including age, gender, ethnicity or race, payer information, length of stay, number of days between discharge and readmission, and readmission length of stay. Interventions including frequency and type were also collected.
Statistical analysis
All data were analyzed using Excel, version 14.3.2. Continuous variables were compared using the Student’s t-test, and categorical data were compared using the chi-square test. Data analyses included descriptive analyses of patient demographics and interventions by the CCRP. Comparative analyses, using the chi-square test were performed on patients who entered the CCN compared to patients who did not enter the CCN. A p value of 0.05 was used to determine statistical significance.
Results
Six hundred thirty-two patients were discharged from SMH with a diagnosis of HF during the study period. Of those, 162 patients entered the CCN and were seen by the CCRP. CCN patients had a 12.3% while non-CCN patients had a 23.8% all-cause 30-day RR (0.52, confidence interval (CI) 0.33–0.81, p = 0.005). As shown in Table 1, the majority of CCN patients were male, younger than non-CCN patients, and insured by Medicare Advantage, a private company contracted Medicare health plan to provide all Part A and B benefits (p < 0.0001, p < 0.001, and p < 0.001, respectively). No other statistically significant differences were noted.
Table 1.
Characteristics of patients.
| Characteristic | CCN patients (n = 162) | Non-CCN patients (n = 470) | p value |
|---|---|---|---|
| Age, mean (SD; range) | 67.8 (16.5; 23–100) | 82.1 (8.6; 65–104) | <0.001 |
| Sex, male, no. (%) | 99 (61.1) | 230 (48.9) | <0.001 |
| Race | |||
| White, n (%) | 95 (58.6) | 292 (62.1) | 0.731 |
| Asian, n. (%) | 23 (14.2) | 58 (12.3) | |
| African American, n (%) | 11 (6.8) | 26 (5.5) | |
| Other, n (%) | 31 (19.1) | 82 (17.4) | |
| Declined, n (%) | 2 (1.2) | 12 (2.6) | |
| Ethnicity | |||
| Not Hispanic or Latino, n (%) | 132 (81.5) | 395 (84.0) | 0.382 |
| Hispanic or Latino, n (%) | 28 (17.3) | 64 (13.6) | |
| Declined, n (%) | 2 (1.2) | 11 (2.3) | |
| Insurance | |||
| Medicare Advantage, n (%) | 47 (29.0) | 154 (32.8) | <0.001 |
| Health Maintenance Organization, n (%) | 38 (23.5) | 38 (8.1) | |
| Medicare Fee-For-Service, n (%) | 31 (19.1) | 270 (57.4) | |
| Other, n (%) | 18 (11.1) | 4 (0.9) | |
| Unfunded, n (%) | 14 (8.6) | 0 | |
| County Medical Services, n (%) | 8 (4.9) | 0 | |
| MediCal | 6 (3.7) | 4 (0.9) | |
CCN: Continuum of Care Network; SD: standard deviation.
HF-1 compliance rates increased to the 90th percentile upon implementation of the CCN as shown in Figure 1 (p = 0.004).
Figure 1.
Joint Commission Heart Failure 1 core measure compliance rate.
Four hundred eighty-two interventions were performed in 162 CCN patients as summarized in Table 2. The top five interventions performed by the CCRP were discharge counseling (74.1%), providing a MedActionPlan (68.5%), resolving problems with medication reconciliation (64.8%), communicating with the community pharmacy (19.1%), and clarifying and correcting a discharge medication prescription (18.5%).
Table 2.
Type of intervention among CCN patients (n = 162).
| Intervention | n (%) |
|---|---|
| Provided discharge counseling, n (%) | 120 (74.1) |
| Created MedActionPlan™, n (%) | 111 (68.5) |
| Medication reconciliation problem, n (%) | 105 (64.8) |
| Admission medication reconciliation, n (%) | 69 (42.6) |
| Discharge medication reconciliation, n (%) | 36 (22.2) |
| Communicated with community pharmacy, n (%) | 31 (19.1) |
| Discharge medication prescription problem, n (%) | 30 (18.5) |
| At least one clinical recommendation to inpatient prescriber, n (%) | 29 (17.9) |
| Communicate information to primary care provider | 18 (11.1) |
| Non-formulary or expensive medication(s), n (%) | 14 (8.6) |
| Lack of patient access to community pharmacy, n (%) | 7 (4.3) |
| Referral to diabetic educator, n (%) | 7 (4.3) |
| Referral to PAP, n (%) | 7 (4.3) |
| Referral to heart failure clinical nurse specialist, n (%) | 3 (1.9) |
CCN: Continuum of Care Network; PAP: patient assistance program.
Of the 162 CCN patients, 30 patients received home visits while 132 received telephonic follow-up, as depicted in Tables 3 and 4, respectively. Twenty-three (76.7%) patients who received a home visit by the CCRP required at least one home intervention. The top three home interventions were provision of a pillbox (76.7%), patient taking incorrect medication(s) (52.2%), and patient taking an incomplete medication regimen (26.1%). Of the 132 patients who received a telephone follow-up call, 10 (7.6%) patients received an intervention with additional patient education needed as the most frequent intervention.
Table 3.
Post-discharge home visit in CCN patients (n = 30).
| Variable | N (%) |
|---|---|
| At least one home intervention, n (%) | 23 of 30 (76.7) |
| Provided pillbox, n (%) | 12 of 23 (52.2) |
| Taking incorrect medication(s), n (%) | 10 of 23 (26.1) |
| Taking incomplete medication regimen, n (%) | 6 of 23 (26) |
| Taking discontinued medication(s), n (%) | 3 of 23 (13.0) |
| Taking expired medication(s), n (%) | 1 of 23 (4.3) |
| Had issues with access to medications, n (%) | 1 of 23 (4.3) |
| Provision of co-pay card, n (%) | 1 of 23 (4.3) |
| Number of days between discharge and home visit, mean (SD; range) | 2.5 (1.6; 1–7) |
| Number of minutes spent on home visit, mean (SD; range) | 50.7 (22.7; 15–120) |
CCN: Continuum of Care Network; SD: standard deviation.
Table 4.
Post-discharge follow-up phone call in CCN patients (n = 132).
| Variable | No. (%) |
|---|---|
| At least one phone intervention, n (%) | 10 (7.6) |
| Needed additional education, n (%) | 7 of 10 (70.0) |
| Needed follow-up appointment, n (%) | 2 of 10 (20.0) |
| Lack of insurance coverage, n (%) | 1 of 10 (10.0) |
| Number of days between discharge and phone call, mean (SD; range) | 3.8 (3.2; 1–22) |
| Number of minutes spent on phone call, mean (SD; range) | 6.8 (4.0; 5–15) |
CCN: Continuum of Care Network; SD: standard deviation.
Discussion
This study is the first to evaluate the impact of a single pharmacist on HF 30-day RRs along with adherence to discharge instructions in a community hospital. Interventions by the CCRP resulted in fewer all-cause 30-day readmissions, a prolonged improvement in HF-1 rates, and approximately four interventions per patient prior to hospital discharge. This was significant for CCN patients who were male, younger (than non-CCN patients), and insured by Medicare Advantage. Although these discrepancies were significant, this study was not randomized or designed to benefit a certain patient population. Randomized control studies are needed to confirm whether these attributes (i.e. gender, age, and payer group) may affect hospital readmissions.
Several studies have demonstrated the role of pharmacists in reducing hospital readmissions in HF patients.7,17–23 In a recent study, Warden et al. examined the effects of pharmacist-led HF medication education and discharge instruction program on 30-day RRs and Joint Commission HF core measures. Interventions included clinical recommendations, corrections to medication reconciliation, discharge education, provision of a complete discharge medication list, and telephonic post-discharge follow-up. After 3 months, authors noted a reduction in 30-day all-cause RRs in the intervention group, a finding similar to our study. While our study included both post-discharge telephonic follow-up and home visits, it can be assumed that the impact of both studies is similar and significant. The data further strengthen the benefit of including pharmacists in the effort to reduce hospital readmissions.
Prior to the implementation of the CCRP-led CCN, SMH’s discharge instruction compliance rates were consistently in the 80th percentile. This was likely due to the lack of pharmacist involvement at the discharge process, which stems from the budgetary limitations on pharmacy services experienced at many community hospitals. The CCRP’s involvement from the time of admission to discharge may have directly impacted discharge instructions as the CCRP closely monitored the patient’s medication regimen. This allowed the CCRP to compare any medications from prior to admission to those ordered during the hospitalization and to identify and correct any missing or duplicative medications upon discharge. These efforts led to an increase in HF-1 adherence rates and are consistent with previous studies and reinforce the importance of incorporating a pharmacist in the discharge process.14,15
Finally, previous studies have reported the type, frequency, and benefit of pharmacist interventions.6,11–13,15 Our data show similar findings and also include uncommon interventions such as the provision of MedActionPlan, communication with the community pharmacy, and correcting a discharge medication prescription. Although a proprietary tool was utilized in this study, the provision of a patient-friendly medication schedule and list is vital during patient education. The CCRP noted that patients had a better understanding of their regimen compared to the hospital’s printed discharge medication list. Among 31 patients, the CCRP called the community pharmacy to clarify patient’s home medications, inquire co-pay or out-of-pocket medication costs, obtain an order for a missing discharge medication, change a discharge medication, and/or hand off pertinent patient information to an outpatient provider. The CCRP made every effort to ensure that patients were able to access and afford their discharge medications. This also included having to contact the inpatient prescriber to correct the physical prescription for discharge medications. Corrections such as missing quantity, dosing direction, and/or missing signature delayed the patient from obtaining their discharge medications and placed unneeded pressure on the community pharmacies to reach the prescriber. These interventions along with increased discharge instruction compliance may have contributed to hospital readmission reductions.
Limitations
This was a non-randomized, single-site study that utilized a historical control group, thus negating the ability to conclude a direct relationship between the CCRP and study outcomes. Hospital admissions or discharges may have occurred during CCRP’s off hours, possibly resulting in fewer interventions than anticipated. In addition, the CCRP was unable to identify readmissions that could have occurred to non-Sharp hospitals. Finally, the CCRP saw 3.43 times more patients than were ultimately coded as having had an HF admission which may have limited the CCRP’s ability to evaluate more suspected HF patients. Despite these limitations, this study illustrates the impact of a single pharmacist. These effects may be magnified if multiple pharmacists are involved. The results from this study provide support for the participation of pharmacists in efforts to reduce HF readmissions and improve core measures, especially in a community hospital setting. However, a randomized, controlled study is necessary to further evaluate the impact of a resident pharmacist or pharmacist on HF 30-day all-cause RRs and Joint Commission core measures.
Conclusion
The implementation of a CCRP-led intervention was associated with a significant reduction in RRs among HF patients and sustainable improvement in discharge instruction compliance in a community hospital.
Acknowledgments
The authors thank Albert Rizos, Pharm.D., BCPS, for guidance and support throughout this project. A.C.B. was the inaugural PGY-2 Continuum of Care Resident Pharmacist (2011–2012) and J.T.T. was the following PGY-2 Continuum of Care Resident Pharmacist (2012–2013) at Sharp Memorial Hospital, San Diego, CA, USA.
Footnotes
Declaration of conflicting interests: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1. Centers for Medicare and Medicaid Services. Readmissions reduction program overview, https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html (accessed 1 October 2013).
- 2. Centers for Medicare and Medicaid Services. Hospital Value-Based Purchasing, https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/hospital-value-based-purchasing/index.html (accessed 1 October 2013).
- 3. Coleman EA, Boult C; American Geriatrics Society Health Care Systems Committee. Improving the quality of transitional care for persons with complex care needs. J Am Geriatr Soc 2003; 51: 556–557. [DOI] [PubMed] [Google Scholar]
- 4. Medicare. Hospital compare, http://www.medicare.gov/hospitalcompare/profile.html#profTab=3&ID=050100&loc=SAN%20DIEGO%2C%20CA&lat=32.7153292&lng=117.1572551&name=SHARP%20MEMORIAL%20HOSPITAL&Distn=7.3 (accessed 1 April 2014).
- 5. Joint Commission. Improving America’s hospitals. The Joint Commission’s annual report on quality and safety, 2011, http://www.jointcommission.org/assets/1/6/TJC_Annual_Report_2011_9_13_11_.pdf (accessed 1 April 2014).
- 6. Bayley BK, Savitz LA, Maddalone T, et al. Evaluation of patient care interventions and recommendations by a transitional care pharmacist. Ther Clin Risk Manag 2007; 3: 695–703. [PMC free article] [PubMed] [Google Scholar]
- 7. Novak CJ, Hastanan S, Moradi M, et al. Reducing unnecessary hospital readmissions: the pharmacist’s role in care transitions. Consult Pharm 2012; 27(3): 174–179. [DOI] [PubMed] [Google Scholar]
- 8. Dudas V, Bookwalter T, Kerr KM, et al. The impact of follow-up telephone calls to patients after hospitalization. Am J Med 2001; 111(9B): 26S–30S. [DOI] [PubMed] [Google Scholar]
- 9. Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med 2009; 150: 178–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Anderegg SV, Demik DE, Carter BL, et al. Acceptance of recommendations by inpatient pharmacy case managers: unintended consequences of hospitalist and specialist care. Pharmacotherapy 2013; 33(1): 11–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med 2006; 166(5): 565–571. [DOI] [PubMed] [Google Scholar]
- 12. Sarangarm P, London MS, Snowden SS, et al. Impact of pharmacist discharge medication therapy counseling and disease state education: Pharmacist Assisting at Routine Medical Discharge (project PhARMD). Am J Med Qual 2013; 28(4): 292–300. [DOI] [PubMed] [Google Scholar]
- 13. Walker PC, Bernstein SJ, Jones JN, et al. Impact of a pharmacist-facilitated hospital discharge program: a quasi-experimental study. Arch Intern Med 2009; 169(21): 2003–2010. [DOI] [PubMed] [Google Scholar]
- 14. Coons JC, Fera T. Multidisciplinary team for enhancing care for patients with acute myocardial infarction or heart failure. Am J Health Syst Pharm 2007; 64(12): 1274–1278. [DOI] [PubMed] [Google Scholar]
- 15. Warden BA, Freels JP, Furuno JP, et al. Pharmacy-managed program for providing education and discharge instructions for patients with heart failure. Am J Health Syst Pharm 2014; 71(2): 134–139. [DOI] [PubMed] [Google Scholar]
- 16. Joint Commission. Specifications manual for Joint Commission national quality core measures (2010A1), https://manual.jointcommission.org/releases/archive/TJC2010B/MIF0028.html (accessed 1 April 2014).
- 17. Rainville EC. Impact of pharmacist interventions on hospital readmissions for heart failure. Am J Health Syst Pharm 1999; 56: 1339–1342. [PubMed] [Google Scholar]
- 18. Lopez-Cabezas C, Salvador CF, Quadrada DC, et al. Randomized clinical trial of a postdischarge pharmaceutical care program vs. regular follow-up in patients with heart failure. Farm Hosp 2006; 30: 328–342. [DOI] [PubMed] [Google Scholar]
- 19. Stewart S, Pearson S, Horowitz JD. Effects of a home based intervention among patients with congestive heart failure discharged from acute hospital care. Arch Intern Med 1998; 158: 1067–1072. [DOI] [PubMed] [Google Scholar]
- 20. Varma S, McElnay JC, Hughes CM, et al. Pharmaceutical care of patients with congestive heart failure: interventions and outcomes. Pharmacotherapy 1999; 19: 860–869. [DOI] [PubMed] [Google Scholar]
- 21. Murray MD, Young J, Hoke S, et al. Pharmacist intervention to improve medication adherence in heart failure: a randomized trial. Ann Intern Med 2007; 146: 714–725. [DOI] [PubMed] [Google Scholar]
- 22. Roughead EE, Barratt JD, Ramsay E, et al. The effectiveness of collaborative medicine reviews in delaying time to next hospitalization for patients with heart failure in the practice setting: results of a cohort study. Circ Heart Fail 2009; 2: 424–428. [DOI] [PubMed] [Google Scholar]
- 23. Thompson CA. Integrated pharmacy practice helps reduce heart failure readmission rate. Am J Health Syst Pharm 2012; 69: 1540–1541 (News). [DOI] [PubMed] [Google Scholar]