Abstract
Background
Intraductal papillary mucinous neoplasm (IPMN) of the pancreas carries a risk of malignancy ranging from 15%-60%, depending on certain high-risk features. Diagnostic efforts often include radiographic imaging with computed tomography, magnetic resonance imaging, magnetic resonance cholangiopancreatography, and endoscopic ultrasound. Once IPMN has been diagnosed, the proposed indications for cyst resection are based primarily on size, main duct involvement, symptoms, and the presence of mural nodules. Diagnostic difficulty still remains, however, in patients with small lesions and with normal carcinoembryonic antigen levels, so alternative endoscopic modalities are needed.
Case Report
We report a case of intracystic SpyGlass Direct Visualization System (Boston Scientific) evaluation and biopsy of an IPMN in a 74-year-old male patient who presented to our surgical clinic with a history of chronic pancreatitis and significant weight loss during the last 2½ years.
Conclusion
In difficult diagnostic cases, SpyGlass pancreatoscopy can be quite useful because the device allows direct endoscopic visualization of the pancreaticobiliary ducts. Ductal pathology, including stones, strictures, and proliferative epithelial abnormalities, can be observed and even directly biopsied. Early experience in applying this technology to pancreatic cyst evaluation has indicated improved diagnostic accuracy.
Keywords: Carcinoma–pancreatic ductal, image-guided biopsy, pancreatectomy, pancreatic neoplasms, pancreatitis
INTRODUCTION
Intraductal papillary mucinous neoplasm (IPMN) of the pancreas carries a risk of malignancy ranging from 15%-60%, depending on certain high-risk features.1 Diagnostic efforts often include radiographic imaging with computed tomography (CT), magnetic resonance imaging, magnetic resonance cholangiopancreatography, and endoscopic ultrasound. Cyst fluid analysis, primarily carcinoembryonic antigen (CEA) level, can also aid in the diagnosis.2 Once IPMN has been diagnosed, the proposed indications for cyst resection are based primarily on size, main duct involvement, symptoms, and the presence of mural nodules.1 Diagnostic difficulty still remains, however, in patients with small lesions and in patients with normal CEA levels. Consequently, alternative endoscopic modalities are needed. We report a case of intracystic evaluation and biopsy of IPMN with the SpyGlass Direct Visualization System (Boston Scientific).
CASE REPORT
A 74-year-old male presented to our surgical clinic with a history of chronic pancreatitis and significant weight loss during the last 2½ years. The patient had undergone multiple endoscopic retrograde cholangiopancreatographies (ERCPs) and pancreatic stent placements for areas of ductal narrowing, with brush cytology demonstrating normal tissue. No mucin was seen extruding from the papilla. A recent CT scan revealed significant ectasia of the pancreatic duct (Figure 1), prompting the addition of SpyGlass pancreatoscopy during the most recent ERCP. The intraductal images demonstrated fronds extending throughout the main pancreatic duct consistent with IPMN (Figure 2). Intraductal SpyGlass-directed biopsies were taken, with histology demonstrating severely atypical cells.
Figure 1.
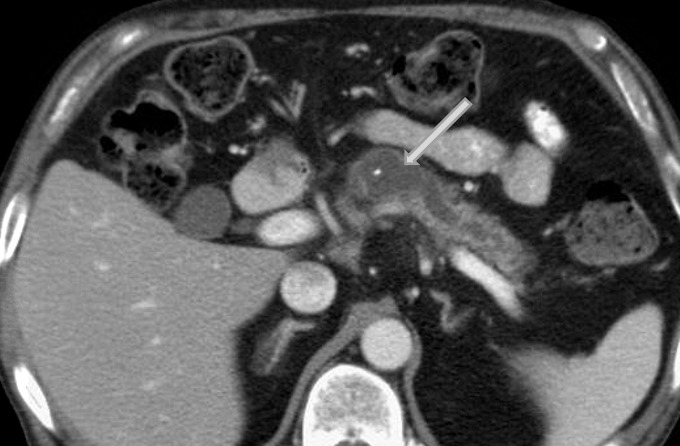
Computed tomography revealed a dilated main pancreatic duct with areas of narrowing. The pancreatic stent is seen within the duct lumen (arrow).
Figure 2.

SpyGlass pancreatoscopy of the main pancreatic duct revealed frond-like projections (arrow) from the epithelial lining, consistent with intraductal papillary mucinous neoplasm (IPMN). Endoluminal visualization allowed directed biopsies of these areas and facilitated a diagnosis of IPMN with significant atypia.
The patient was subsequently referred to the surgical oncology department for consideration of pancreatic resection. After discussion, the decision of the multidisciplinary tumor board was for the patient to undergo a total pancreatectomy in light of the diffuse nature of the disease. The patient tolerated the procedure well without complication and was discharged on postoperative day 9. The specimen was opened after resection, revealing typical IPMN ductal changes (Figure 3). Final pathology demonstrated a noninvasive IPMN with moderate and high-grade dysplasia extending the full length of the pancreatic duct. No invasive component was identified, all margins were negative for dysplasia, and all lymph nodes were negative for malignancy.
Figure 3.

Gross evaluation of the surgical specimen showed ductal changes consistent with intraductal papillary mucinous neoplasm. Final pathology showed only noninvasive disease.
DISCUSSION
Autopsy studies indicate approximately 2.6% of the population and 8% of elderly patients have a pancreatic cyst.3 We now know that a subgroup of pancreatic cysts, namely the mucinous cysts (IPMNs and mucinous cystic neoplasms), has malignant potential. Numerous case series report malignancy rates for IPMN ranging from 10% to >70% depending on whether the main duct is involved and other high-risk criteria, including mural nodules, are present.1,4
These cysts can present significant diagnostic difficulty. Small lesions can resemble nonmalignant serous cysts, and main duct dilation can resemble changes seen with chronic pancreatitis. Furthermore, although a cyst fluid CEA level >192 ng/mL is 73% sensitive and 84% specific for a mucinous cyst, this test cannot differentiate benign from malignant cysts.2 Our patient had had multiple episodes of pancreatitis, had a dilated main pancreatic duct with areas of narrowing, and did not have mucin extruding from the papilla. Not until pancreatoscopy was added to the evaluation process to assess an area of ductal narrowing for malignancy was the diagnosis made.
In difficult diagnostic cases, SpyGlass pancreatoscopy can be quite useful because the device allows direct endoscopic visualization of the pancreaticobiliary ducts.5 Ductal pathology, including stones, strictures, and proliferative epithelial abnormalities, can be observed and even directly biopsied. Early experience in applying this technology to pancreatic cyst evaluation has indicated improved diagnostic accuracy.6 In our case, the pancreatoscopy, performed in a community hospital, allowed the diagnosis to be made before progression to invasive cancer. While we have not seen drastic improvement in the treatment of pancreatic cancer during the past 3 decades,7 diagnosis and management of premalignant IPMN are an area of significant achievement. Patients with these lesions, especially those with main duct involvement, have a significant malignancy risk,4 and removal of the lesion is likely curing a future pancreatic cancer. Pancreatoscopy facilitated by advancements in white light endoscopy and smaller endoscopic catheters will continue to facilitate the diagnosis and treatment of IPMN and other pancreatic pathology.8
CONCLUSION
SpyGlass pancreatoscopy is a useful tool for difficult diagnostic cases, and early experience with using this technology to evaluate pancreatic cysts has indicated improved diagnostic accuracy.
ACKNOWLEDGMENTS
The authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care and Medical Knowledge.
REFERENCES
- 1.Tanaka M, Fernández-del Castillo C, Adsay V, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012 May-Jun;12(3):183–197. doi: 10.1016/j.pan.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 2.Brugge WR, Lewandrowski K, Lee-Lewandrowski E, et al. Diagnosis of pancreatic cystic neoplasms: a report of the cooperative pancreatic cyst study. Gastroenterology. 2004 May;126(5):1330–1336. doi: 10.1053/j.gastro.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 3.Laffan TA, Horton KM, Klein AP, et al. Prevalence of unsuspected pancreatic cysts on MDCT. AJR Am J Roentgenol. 2008 Sep;191(3):802–807. doi: 10.2214/AJR.07.3340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marchegiani G, Mino-Kenudson M, Sahora K, et al. IPMN involving the main pancreatic duct: biology, epidemiology, and long-term outcomes following resection. Ann Surg. 2014 Jun 27; doi: 10.1097/SLA.0000000000000813. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen YK, Pleskow DK. SpyGlass single-operator peroral cholangiopancreatoscopy system for the diagnosis and therapy of bile-duct disorders: a clinical feasibility study (with video) Gastrointest Endosc. 2007 May;65(6):832–841. doi: 10.1016/j.gie.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 6.Arnelo U, Siiki A, Swahn F, et al. Single-operator pancreatoscopy is helpful in the evaluation of suspected intraductal papillary mucinous neoplasms (IPMN) Pancreatology. 2014 Nov-Dec;14(6):510–514. doi: 10.1016/j.pan.2014.08.007. [DOI] [PubMed] [Google Scholar]
- 7.Oettle H, Post S, Neuhaus P, et al. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA. 2007 Jan 17;297(3):267–277. doi: 10.1001/jama.297.3.267. [DOI] [PubMed] [Google Scholar]
- 8.Coté GA, Smith J, Sherman S, et al. Technologies for imaging the normal and diseased pancreas. Gastroenterology. 2013 May;144(6):1262–1271.e1. doi: 10.1053/j.gastro.2013.01.076. [DOI] [PubMed] [Google Scholar]


