Abstract
Background
Hepatic hydatid cysts rarely invade portal veins causing portal cavernomatosis as a secondary complication.
Case Report
We report the case of a patient with direct invasion of the right portal vein by hydatid cysts causing portal cavernomatosis diagnosed via magnetic resonance imaging (MRI).
Conclusion
The presented case highlights the useful application of MRI with T2-weighted images and gadolinium-enhanced T1-weighted images in the diagnosis of hepatic hydatid lesions presenting with a rare complication of portal cavernomatosis.
Keywords: Echinococcosis–hepatic, gadolinium ethoxybenzyl DTPA, liver, magnetic resonance imaging, portal vein
INTRODUCTION
Hydatid cyst disease, or echinococcosis, is an endemic disease seen principally in the countries of the Middle and Far East and Africa. Hydatid cysts primarily affect the abdominal area of the liver and cause complications such as perforation of hollow organs of the abdomen, biliary communication, peritoneal seeding, transdiaphragmatic thoracic involvement, and hepatic or portal vein invasion.1-4 Direct portal vein invasion by cystic contents is rare, especially when caused by a hydatid lesion located in the hepatic hilum or caudate lobe.2 Obliteration of portal veins by cysts results in portal cavernous transformation, noted on magnetic resonance imaging (MRI) or computed tomography (CT) scans as tortuous veins that enhance after contrast administration. We present the case of a patient with hepatic hydatid disease with cysts obliterating the right and main portal veins, causing portal cavernomatosis around the obstructed veins.
CASE REPORT
A 52-year-old male was seen in the general surgery clinic for rectoscopy to rule out rectal malignancy as a cause of rectal bleeding. On physical examination, his vital signs were within normal limits. He reported vague abdominal pain, and his laboratory findings were unremarkable. An adenomatous polyp of the rectum was observed on rectoscopic examination. MRI of the abdomen and pelvis was performed with a 1.5T MRI unit (GE Signa Excite HD, GE Healthcare) using an 8-channel phased-array torso coil.
Single-shot fast spin echo T2-weighted MRI showed a multilocular cystic lesion centered on hepatic segment 6 and extending into the portal hilum on coronal (Figure 1, arrows) and axial (Figure 2, arrows) views (repetition time [TR]=625 ms, echo time [TE]=92 ms, slice thickness 5 mm). After intravenous administration of a gadolinium-based contrast material, no enhancement was seen in the lesion on T1-weighted axial image (Figure 3, arrows). Portal cavernous transformation was identified around the lesion on the same axial image (Figure 3, arrowheads) indicating portal cavernomatosis. When the patient was questioned, he reported that a hepatic hydatid cyst lesion had been diagnosed years ago; however, he was not aware of the portal vein invasion. The patient had no concerns caused by the hydatid cyst lesion and did not agree to surgery. He was discharged to follow-up.
Figure 1.
On coronal view, single-shot fast spin echo T2-weighted magnetic resonance image shows a multilocular cystic lesion (arrows) in hepatic segment 6 extending into the portal hilum.
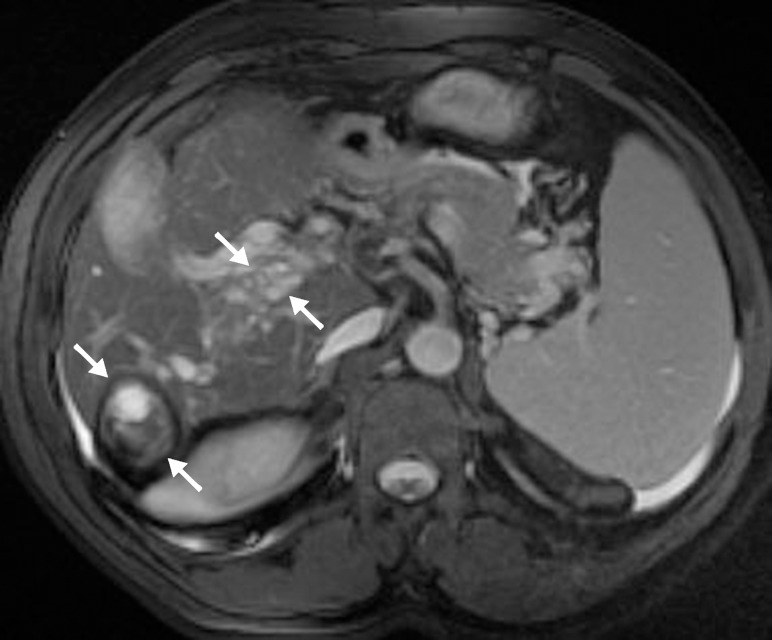
Figure 2.
On axial view, fat-saturated single-shot fast spin echo T2-weighted magnetic resonance image shows a multilocular cystic lesion (arrows) in hepatic segment 6 extending into the portal hilum.
Figure 3.
After intravenous administration of a gadolinium-based contrast material, no enhancement was seen in the lesion on T1-weighted axial image (arrows). Portal cavernous transformation was identified around the lesion on the same axial image (arrowheads) indicating portal cavernomatosis.
DISCUSSION
Reports of hydatid cyst lesions that invade portal veins, obliterate blood flow, and eventually result in portal cavernomatosis are rare.1,2 Typically, thrombosis and external compression of the portal system by hydatid cysts are the causes of cavernomatosis.2 Direct invasion of the portal vein by the cystic contents is a rare and unusual complication of hepatic hydatid disease.
Secondary portal cavernous transformation might be a sign of portal vein invasion or compression, but the much more common complication of biliary system communication with the hydatid cysts should be ruled out for correct diagnosis.
Hydatid cyst disease diagnosis is made by various radiologic methods including ultrasonography, CT, and MRI.3 Although ultrasonography and CT are the first-line and most readily available imaging methods, MRI is reported to be the best imaging method for differentiating cystic components and for showing biliary tract communication.3 Gadolinium-enhanced MRI shows venous structures and makes it possible to diagnose cavernomatosis. T2-weighted images are useful for showing cystic components, and T1-weighted images are used with gadolinium administration to differentiate venous structures.
CONCLUSION
This case highlights the useful application of MRI with T2-weighted and gadolinium-enhanced T1-weighted images in the diagnosis of hepatic hydatid lesions presenting with the rare complication of portal cavernomatosis.
ACKNOWLEDGMENTS
The authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care and Medical Knowledge.
REFERENCES
- 1.Agarwal N, Dewan P. Portal hypertension as a rare complication of hydatid cyst: diagnosis and management. Internet J Gastroenterol. 2009 9:1. http://ispub.com/IJGE/9/1/3570. Accessed September 17, 2015. [Google Scholar]
- 2.Pedrosa I, Saíz A, Arrazola J, Ferreirós J, Pedrosa CS. Hydatid disease: radiologic and pathologic features and complications. Radiographics. 2000 May-Jun;20(3):795–817. doi: 10.1148/radiographics.20.3.g00ma06795. [DOI] [PubMed] [Google Scholar]
- 3.Marrone G, Crino F, Caruso S, et al. Multidisciplinary imaging of liver hydatidosis. World J Gastroenterol. 2012 Apr 7;18(13):1438–1447. doi: 10.3748/wjg.v18.i13.1438. doi: 10.3748/wjg.v18.i13.1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Czermak BV, Akhan O, Hiemetzberger R, et al. Echinococcosis of the liver. Abdom Imaging. 2008 Mar-Apr;33(2):133–143. doi: 10.1007/s00261-007-9331-0. [DOI] [PubMed] [Google Scholar]