Abstract
Objective
This study examined the role of three distinct beliefs about risk (risks associated with screening, construal of the function of screening as health-affirming or illness-detecting, and perceived susceptibility to breast cancer) in moderating women's responses to framed messages that promote mammography.
Design
Three hundred fifty-five women recruited from an inner city hospital, nonadherent to guidelines for receiving annual screening mammograms,were randomly assigned to view a gain- or loss-framed video message about the importance of mammography.
Main Outcome Measure
Mammography screening was self-reported at a 3-month follow-up.
Results
Only perceived susceptibility to breast cancer significantly moderated the effect of message framing on screening. Women with average and higher levels of perceived susceptibility for breast cancer were significantly more likely to report screening after viewing a loss-framed message compared to a gain-framed message. No effects of framing on reported screening were observed for women with lower levels of perceived susceptibility.
Conclusion
The study identifies a key role for perceived susceptibility in shaping responses to framed messages that promote cancer screenings.
Keywords: perceived risk, message framing, mammography, health behavior, persuasive communication
Nearly 1 in 8 women will be diagnosed with some form of breast cancer over the course of her life (Horner et al., 2006). Treatment of breast cancer is most successful when the cancer is discovered early, and although some recent debate exists about the effectiveness of mammography in reducing mortality from breast cancer (U.S. Preventive Services Task Force, 2009), mammography remains the most effective method of early detection (Humphrey, Helfand, Chan, & Woolf, 2002). Consequently, many public health agencies (i.e., American Cancer Society, National Cancer Institute, U.S. Preventive Services Task Force) encourage women to obtain regular mammography screenings.
More women than ever before are reporting having had at least one mammogram (Blackman, Bennett, & Miller, 1999), but effective early detection and treatment of breast cancer require following guidelines for routine screenings, and many women are still nonadherent to these recommendations (Clark, Rakowski, & Bonacore, 2003; Rakowski et al., 2004). A recent population survey found that more than half (51%) of American women aged 55 and over were, in fact, nonadherent to recommendations for annual screenings, and more than one third (36%) were nonadherent to recommendations for biennial screenings (Rakowski et al., 2004).
In this article, we examine how health message framing (cf. Rothman & Salovey, 1997) can be used to promote the use of screening mammography. The approach to message framing that we examine in this study is novel, in that it focuses on the question of for whom are loss- and gain-framed messages likely to be most effective in promoting cancer screening? In particular, we examine the influence of three distinct beliefs about the risks associated with breast cancer screening and breast cancer in general in shaping women's behavioral responses to framed messages that promote mammography screening.
Health Message Framing
The theoretical basis for most work on health message framing is prospect theory (Kahneman & Tversky, 1979). Kahneman and Tversky showed that people's choices are sensitive to how consequences of decisions are framed. In particular, people are generally loss averse in that anticipated losses of any type (money, goods, health) have more of a subjective psychological impact than equivalent gains. Thus, to avoid losses, people are more willing to gamble (i.e., make choices that involve risk and uncertainty) when the consequences of the choices are framed as losses (e.g., losing $20) than when the consequences are framed as gains (e.g., gaining $20). In contrast, people are less willing to make choices that involve risk and uncertainty when consequences of choices are framed as gains.
Rothman and Salovey (1997) used prospect theory as a guide to recommend how messages that advocate health behaviors should be framed, depending on the perceived riskiness of engaging in the behavior. Loss-framed health messages focus on the costs of not performing a health behavior, such as “When you do not get regular mammograms, you are increasing your chances of dying from breast cancer.” Gain-framed messages focus on the benefits of performing a health behavior, such as “When you get regular mammograms, you are increasing your chances of surviving breast cancer.”
To obtain or not to obtain a cancer screening such as a mammogram is a choice that involves the consideration of a number of risks and uncertainties. Often, the most salient risk is the immediate possibility that a serious disease could be discovered. As getting an illness detection test such as mammography is likely to be perceived as a risky decision in the short term, Rothman and Salovey (1997) suggested that loss-framed messages should be more likely to motivate people to make such a decision. Indeed, loss-framed messages can be more effective in promoting illness detection behaviors than gain-framed messages (see Edwards, Elwyn, Covey, Matthews, & Pill, 2001; and Rothman, Kelly, Hertel, & Salovey, 1993, for reviews), however the magnitude of the effects have varied across studies and have generally been small (see Edwards et al., 2001; O'Keefe & Jensen, 2009). These generally small effects of message framing in promoting illness detection behaviors have led some to conclude that message framing has limited, if any, role in the promotion of screening behaviors (O'Keefe & Jensen, 2009).
It is important to recognize that any advantage of loss-framed messages in promoting illness detection rests on the assumption that people generally view screening tests to be risky. Only recently has the role of people's unique construals of screening tests in shaping their responses to framed messages been investigated. For example, Bartels, Kelly, and Rothman (2009) showed that when a fictitious screening behavior was described as something that could detect the presence of a health benefit, and thus should not be construed as risky, people were more interested in the test when information was gain-framed than loss-framed. In contrast, only when the test was described as one that could detect the presence of a health problem were participants more interested when the consequences were loss-framed. Thus, people's responses to framed messages may not always be a simple reflection of the presumed risky nature of screening behaviors but rather shaped by their individual beliefs about risk.
Message Framing and Breast Cancer Screening
Breast cancer screenings have frequently been used as a domain for testing the theoretical assumptions laid out by prospect theory (i.e., Banks et al., 1995; Lalor & Hailey, 1990; Meyerowitz & Chaiken, 1987; Schneider et al., 2001; Williams, Clarke, & Borland, 2001). However, as empirical tests of the framing postulates of prospect theory have been typically carried out in hypothetical decisions where risk is operationalized as probabilistic uncertainty in the outcome of a decision (cf. Tversky & Kahneman, 1981), it remains unclear what specific beliefs about risk and uncertainty shape people's responses about real decisions to obtain or not to obtain a cancer screening.
The risks associated with screening tests such as mammography could take a number of forms. One form represents a woman's unique beliefs about the risks of negative consequences and uncertainties associated with the screening test itself. These involve the possibility of pain, uncertainty in the effectiveness of mammography, as well as the potential for cancer to be found. These beliefs are often correlated with each other, and they are also associated with women's readiness to obtain a mammogram (Rakowski et al., 1997). Furthermore, it is these kinds of beliefs about the more immediate negative consequences of the screening test that have been hypothesized to moderate people's responses to framed messages (Rothman & Salovey, 1997).
A second form that a woman's belief about the risk implications of mammography could take is her construal of the underlying function of obtaining a mammogram—for example, to affirm that she is healthy or to find out if she has a problem. Most women may view obtaining a mammogram from the latter perspective (cf. Cioffi, 1991). However any variability in a woman's construal of the purpose of obtaining a mammogram may also shape how she responds to framed messages (Rothman, Kelly, Hertel, & Salovey, 2003). For example, Rothman et al. (2003) have argued that for women who view a mammogram as something will serve to affirm that they are healthy, gain-framed messages may be more effective. However, for women who view a mammogram as something that serves to detect a problem, loss-framed messages may be more effective. This prediction would be consistent with Bartels et al.'s (2009) findings that it was only when a screening test was construed as one that would detect a problem that a loss-framed advantage was found.
Prospect theory would suggest that these aforementioned beliefs about the risks and uncertainties of the screening test itself would be the most relevant beliefs that shape a woman's responses to framed messages that promote screening. However, it is possible that for people who do not have much experience with the behavior, beliefs about the screening test may not be particularly salient. Instead, more general beliefs about their perceived susceptibility to the health condition may be more relevant. Perceived susceptibility for breast cancer is a relatively stable belief that women hold about their chances of getting breast cancer (Han et al., 2007) and is known to be associated with decisions to get screened (Katapodi, Lee, Facione & Dodd, 2004). It may be that women with greater perceived susceptibility to breast cancer may view the prospect of obtaining a mammography as a more risky decision and loss-framed information may be more persuasive. In contrast, women with a lower perceived susceptibility to breast cancer may be less likely to view obtaining a mammogram as risky, and any advantage of loss-framed information may be reduced.
Present Study
The aim of this study was to examine the role of these three distinct beliefs about risk in shaping the effectiveness of gain- and loss-framed messages in motivating uptake of mammography screening. Given that no prior studies have systematically examined how risk beliefs shape people's responses to framed messages that promote cancer screenings, we made the general prediction that higher beliefs about risk and uncertainty would be associated with a greater advantage of loss-framed messages over gain-framed messages in motivating screening. We tested this prediction in an intervention study conducted in the medical center of an innercity hospital. Unlike many previous studies that have used relatively homogenous samples (Banks et al., 1995; Lalor & Hailey, 1990; Lerman et al., 1992; Meyerowitz & Chaiken, 1987; but see Schneider et al., 2001), we recruited a large ethnically diverse sample of women, all of whom were nonadherent to existing guidelines for mammography screening. Women were then randomly assigned to view either a loss-framed or gain-framed video about mammography, and self-reported screening behavior was assessed 3 months later.
Method
Participants
A convenience sample of 355 women participated in the study in exchange for monetary compensation. Women were asked to participate in the study while awaiting their regular clinic appointments in the waiting area of an inner city, Midwestern hospital internal medicine center. To be eligible for the study, women had to be 40 years of age or older and without a personal history of breast cancer. During the time of data collection, the prevailing recommendation was that women aged 50 and over obtain annual mammograms, and women aged 40–49 obtain at least biennial mammograms with some guidelines that recommend annual mammograms (cf. American Cancer Society, 2007). The mean age of participants was 51 years, with ages ranging from 40 to 85 years. Women were primarily African American (48.9%) and Caucasian (48.3%). The majority of women had health insurance that would cover a mammogram (67.9%), had received at least one mammogram in the past (69.0%), and did not have a family history of breast cancer (82.2%). Descriptive statistics on the sample are presented in Table 1.
Table 1.
Descriptive Results by Message Frame Condition
| Variable | Loss framea | Gain frameb | p |
|---|---|---|---|
| Ethnicity | |||
| Caucasian | 44.8% | 51.7% | .19 |
| African American | 51.9% | 45.4% | .22 |
| Age | 51.2 (9.4) | 51.9 (9.8) | .48 |
| Prior mammograms | 1.1 (0.8) | 1.13 (0.8) | .72 |
| Family history | 17.7% | 17.2% | .95 |
| Physician recommendation | 57.5% | 59.8% | .66 |
| Risks of mammography | 2.4 (0.9) | 2.5 (0.9) | .30 |
| Health affirming construal | 42.5% | 40.2% | .63 |
| Perceived susceptibility | 2.4 (1.0) | 2.4 (0.9) | .69 |
| Involvement in breast cancer | 4.4 (1.3) | 4.6 (1.3) | .13 |
| Screening at 3 months | 37.0% | 23.6% | <.01 |
N = 181.
N = 174.
Procedure
Women were greeted in the hospital waiting room where the study was described and eligibility criteria were verified. Those who were eligible and provided informed consent completed measures individually through paper-and-pencil packets in a private counseling room. Next, women were randomly assigned to watch one of two versions of a breast cancer and mammography educational video. On completion of the video and questionnaires, women were given an appropriately framed flyer with a list of local agencies that provide free and low-cost mammography screening. Women were then compensated $15 for participating in the initial session. Three months later, women were contacted by telephone or postal mail and asked whether or not they had obtained a mammogram in the past 3 months.
Pre-Message Questionnaire Measures
Perceived risks associated with mammography screening
Perceived risks associated with mammography screening was assessed with Rakowski et al.'s (1997) scale of the cons of mammography (α = .73). Items from the cons scale ask women to rate their agreement on a 5-point scale to statements about a number of unpleasant consequences of mammography, such as risks of unnecessary surgery, worry/anxiety, cost, conflicting recommendations, and discomfort.
Construal of the function of mammography
One item, developed for this study, assessed women's illness-detecting versus health-affirming construal of mammography. The item was modeled specifically to address the unique construal of the function of mammography as proposed by Rothman et al. (2003). It asked women to choose between the statements, “If I got a mammogram, I would get it to detect any problems with my breasts” or “If I got a mammogram, I would get it to affirm that my breasts are healthy.” Pilot testing of this item with a sample of women recruited from the same clinic (N = 35) indicated that they understood the distinction between the two statements.
Perceived susceptibility to breast cancer
Perceived susceptibility to breast cancer was assessed with a three-item perceived susceptibility scale designed specifically for breast cancer (Champion, 1999). Statements included “I feel I will get breast cancer sometime during my life,” “My chances of getting breast cancer in the next few years are great,” and “It is likely that I will get breast cancer.” Women rated their agreement using a Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). This scale is known to have discriminant validity against other beliefs, such as perceived benefits and barriers to mammography (Champion, 1999). The internal consistency of the measure in our sample was strong (α = .85).
Involvement in breast cancer issues
Three items from Finney and Iannotti's (2001) scale of involvement with the issue of breast cancer were used to measure involvement in breast cancer issues. Women rated on a 7-point Likert scale how much of a concern breast cancer was to them, how much they read articles about breast cancer, and how much they paid attention to media about breast cancer (α = .71).
Family history of breast cancer
Women reported the number of first-degree relatives that had been diagnosed with breast cancer. This measure was collapsed to reflect whether the women had at least one first-degree relative with breast cancer (0 = no, 1 = yes).
Number of prior mammograms
All women were asked whether they had any prior mammograms, and if so, they were asked to provide the approximate dates of the last two prior mammograms. On the basis of this information, an index was created of the number of prior mammograms received (0, 1, or 2 or more).
Physician recommendation
Women were asked whether, in the last year, a doctor or nurse had recommended they get a mammogram (0 = no, 1 = yes).
Behavioral Follow-Up
Self-reported follow-up of mammography
Mammography usage was assessed with a single item, “Have you obtained a mammogram within the past 3 months?” (0 = no, 1 = yes). Self-reports of mammography screening are known to be highly correlated with reports taken from medical records (i.e., Howard, Agarwal, & Lytwyn, 2009; Rauscher, Johnson, Cho, & Walk, 2008).
Materials
The gain- and loss-framed videos presented equivalent information concerning breast cancer risk factors, detection procedures, the importance of early detection, facts about mammography, and guidelines for obtaining regular mammograms. The videos were approximately 10 minutes in length and included a series of 70 photographs, drawings, and graphics that are matched to audio narration that have been used in previous research (see Schneider et al., 2001, for more details). The gain-framed video, titled “The Benefits of Mammography,” emphasized the benefits of getting a mammogram, whereas the loss-framed video, titled “The Risks of Neglecting Mammography,” emphasized the costs of not getting a mammogram. In each of the videos, approximately 9% of the visuals and 40% of the narrative content were framed.
An example of gain-framed video content was “Breast cancer is the most common cancer found in women … detecting breast cancer early can save a woman's life” and “When a woman gets regular mammograms, she is doing her best to detect breast cancer early. And, detecting breast cancer early can save her life.” An example of loss-framed video content was “Breast cancer is the most common cancer found in women … failing to detect breast cancer early can cost a woman her life” and “When a woman does not get regular mammograms, she is not doing her best to detect breast cancer early. And, failing to detect breast cancer early can cost her life.”
Analytic Strategy
The goal of the present study was to examine the interactions between message frame and risk beliefs on the likelihood of obtaining a mammography at follow-up by using moderated multiple logistic regression. All variables with the exception of message frame were mean-centered prior to inclusion in the model so that the conditional effect of message frame on screening would be estimated at the mean levels of all other variables (Jaccard, 2001). The experimental condition, message frame, was coded as 0 (gain-frame) and 1 (lossframe).
Results
Follow-Up and Attrition
At the 3-month follow-up, 30.4% of women reported that they had obtained a mammogram since the initial study session. The remaining 69.6% of women were made up of those who either reported that they had not obtained a mammogram (208 women) or who were unable to be contacted after repeated attempts (39 women). The women available for follow-up did not differ from those unavailable in age, ethnicity, education, marital status, mammography history, and family history of breast cancer (all ps >.16). However, women who could not be contacted were less likely to have health insurance that would cover a mammogram (p = .08). For this reason, the women who were unable to be contacted at follow-up were assumed to have not obtained a mammogram in all subsequent analyses.
Correlates among risk beliefs
As Table 2 shows, the three risk-related beliefs represented generally distinct constructs in our sample. Greater perceived risks of mammography screening was not significantly associated with construal of the function of mammography (r = .09, p = .09), but it was associated with greater perceived susceptibility to breast cancer (r = .11, p < .05). Perceived susceptibility to breast cancer was not significantly associated with construal of the function of mammography (r = −.02, ns).
Table 2.
Correlations Among Major Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Risks of screening | — | ||||||
| 2. Construal of mammography | .09 | — | |||||
| 3. Perceived susceptibility | .11* | −.02 | — | ||||
| 4. Involvement in breast cancer issues | −.13* | −.07 | .32** | — | |||
| 5. Family history of breast cancer | .05 | .08 | −.17** | −.13* | — | ||
| 6. Number of prior mammograms | −.29** | .02 | −.08 | .14** | −.03 | — | |
| 7. Physician recommendation | −.07 | −.03 | .06 | .12* | −.11* | .37** | — |
Note. Correlations involving dichotomous variables (construal of mammography, family history, and physician recommendation) represent point biserial correlations; correlations involving two dichotomous variables represent phi coefficients.
p < .05.
p < .01.
Covariates
Predictors of screening
Previous research has found age (Burack, George, & Gurney, 2000), prior screening history (Han et al., 2007), and physician recommendation (Fox, Murata, & Stein, 1991) to strongly predict likelihood of subsequent screening. In our sample, the only associations between these variables and risk-related beliefs were older age being associated with somewhat greater perceived susceptibility (r = .10, p = .06) and fewer prior screenings being associated with elevated perceived risks of screening (r = −.29, p < .01). To account for demographic and medical influences on screening, we included these three factors as initial predictors of screening, and they accounted for approximately 7% of the variance in screening when included in a first block, likelihood ratio (LR) χ2(3) = 28.67, p < .001. However, physician recommendation was not a significant predictor of screening (p = .87) and was removed from the model.
Moderation of Message Framing by Risk Beliefs
In a second logistic regression model, message frame, risk beliefs, and their interactions were added as predictors and accounted for a significant additional portion of variance in screening, LR χ2(7) = 22.47, p < .01. Table 3 shows the results of this moderated logistic regression model. Overall, loss-framed messages led to a significantly higher rate of screening compared to gain-framed messages (odds ratio [OR] = 2.26). Among women who viewed a loss-framed message, 37% reported screening at follow-up. However, among women who viewed a gain-framed message, only 24% reported a screening at follow-up. Thus, this loss-framed advantage is consistent with results of other prior mammography studies (Banks et al., 1995; Schneider et al., 2001). This main effect of loss-frame was not significantly moderated by either women's beliefs about the risks of mammography screening or by their construals of the function of mammography. However, it was qualified by a significant interaction with perceived susceptibility to breast cancer (OR = 1.68), indicating that the effectiveness of message frame depended on a woman's perceived susceptibility to breast cancer.
Table 3.
Logistic Regression Predicting Mammography Screening at 3 Months
| Variable | OR | 95% CI |
|---|---|---|
| Age | 1.05** | 1.02–1.07 |
| Previous mammograms | 1.50* | 1.06–2.12 |
| Loss frame | 2.26** | 1.35–3.78 |
| Risks of screening | 0.54** | 0.34–0.85 |
| Frame × Risks of screening | 1.70† | 0.94–3.06 |
| Construal of mammography | 1.08 | 0.50–2.37 |
| Frame × Construal | 0.92 | 0.33–2.54 |
| Perceived susceptibility | 0.84 | 0.56–1.26 |
| Frame × Susceptibility | 1.68* | 1.01–2.80 |
Note. N = 355. OR = odds ratio; CI = confidence interval.
p = .078.
p < .05.
p < .01.
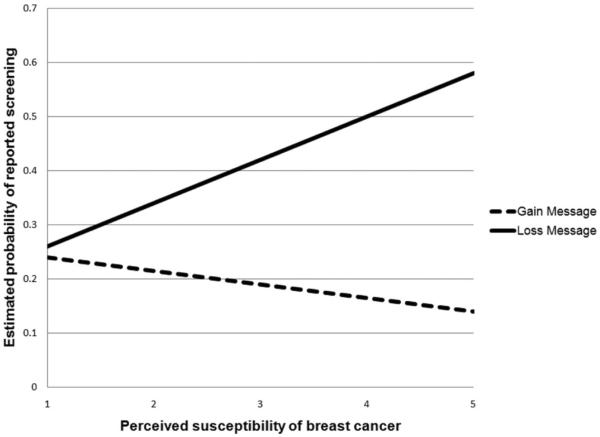
Figure 1 displays the estimated probability of reported screening at 3 months for both the gain- and loss-framed message conditions across levels of perceived susceptibility to breast cancer. To decompose this interaction, we followed the recommendations of Jaccard (2001) and estimated the conditional effect of message framing on reported screening at three levels of perceived susceptibility (−1 SD, average, +1 SD). Among women with average and higher (+1 SD) perceived susceptibility to breast cancer (Ms = 2.41 and 3.39 in perceived susceptibility, respectively), there was a significant advantage of the loss-framed message (Ms = 0.36, 0.44; SEs = 0.03) over the gain-framed message (Ms = 0.20, 0.17; SEs = 0.03, 0.02), respectively (ps = .03 and <.001). However, no loss-frame advantage was found among women with lower perceived susceptibility (−1 SD, M = 1.42) to breast cancer. For these women, those who viewed a loss-framed message (M = 0.28, SE = 0.03) reported statistically similar rates of screening as those who viewed a gain-framed message (M = 0.22, SE = 0.03, p = .48). An analysis of the simple slopes revealed that this interaction was driven by the loss-framed message leading to higher rates of screening at increasing levels of perceived susceptibility (OR = 1.40, SE = .22, p = .04). Among those who viewed the gain-framed message, there was no association between perceived susceptibility and screening (OR = .85, SE = .17, p = .41).
Figure 1.
Probability of screening at 3 months as a function of perceived susceptibility to breast cancer (1 = low perceived susceptibility; 5 = high perceived susceptibility) and message frame.
Although the interaction between perceived risks associated with screening and message framing was only marginally significant (p = .08), the pattern of the interaction was similar to that found for perceived susceptibility. Among women with average (M = 2.41) and higher (+1 SD, M = 3.30) perceived risks associated with mammography, there was a significant advantage of the loss-framed message (Ms = 0.36, 0.34; SEs = 0.03) over the gain-framed message (Ms = 0.20, 0.12; SEs = 0.03, 0.02), respectively(both ps = <.01). However, no loss-frame advantage was found among women with lower (−1 SD, M = 1.52) perceived risks associated with mammography. For these women, those who viewed a loss-framed message (M = 0.38, SE = 0.03) reported statistically similar rates of screening as those who viewed a gain-framed message (M = 0.30, SE = 0.03, p = .31).
Ethnic Differences
The diversity of our sample allowed us to examine whether the effects of message framing and risk beliefs on screening were consistent across ethnic groups. We conducted a logistic regression similar to Table 2 but added terms that represent all two-way and three-way interactions between message frame, risk beliefs, and ethnicity (1 = Black, 0 = White/other). In this analysis, all three-way interactions between message frame, risk beliefs, and ethnicity were not significant, including the Message Frame × Perceived Susceptibility × Ethnicity interaction (OR = .94, p = .91). Thus, there was no indication that any of the Message Frame × Risk Beliefs interactions varied by ethnicity.
Moderation of Message Framing by Family History and Involvement
We also examined whether other constructs related to perceived susceptibility significantly moderated women's behavioral responses to framed messages. Neither family history nor involvement in breast cancer issues significantly moderated the effect of message framing on screening (all ps > .72), suggesting that neither the Message Frame × Perceived Susceptibility or the Message Frame × Perceived Risks of Mammography interactions were attributable to any of these related factors.
Discussion
Prospect theory identifies beliefs about risk and uncertainty as factors that shape people's responses to framed information, and it has been used as a basis for recommending how health messages should be framed to motivate adherence (Rothman & Salovey, 1997). This study provides the first direct test of the relationship between risk beliefs and health message framing in the promotion of cancer screening behavior, assessed in our study by self-report at a 3-month follow-up. We found perceived susceptibility to breast cancer determined the extent to which loss-framed messages encouraged women to obtain a mammogram. Women who perceived a higher susceptibility to breast cancer were significantly more persuaded to obtain a mammogram by the loss-framed message than the gain-framed message. This finding is of particular importance given research that shows higher perceptions of susceptibility to be associated with reduced screening rates (Han et al., 2007; Lerman & Schwartz, 1993). Thus, our findings support the usefulness of loss-framed messages in the promotion of mammography, particularly among women who perceive a high susceptibility to breast cancer. In contrast, women who perceived a lower susceptibility to breast cancer were equally persuaded by the gain-framed and loss-framed messages. Given that message framing did not have an effect on screening among women with lower perceived susceptibility, more research is needed to clarify how to best motivate such women to obtain screenings.
Our findings join studies in other domains such as HIV testing (Apanovitch, McCarthy, & Salovey, 2003) and hypothetical health screening decisions (Bartels et al., 2009), showing that a person's unique beliefs about the risks associated with screening shape their responses to framed messages. As such, our findings help clarify the issue of for whom are framed messages most likely to promote mammography screening, and may be useful in informing the development of tailored and targeted interventions promoting mammography.
As ours is the first study to systematically examine how beliefs about risk shape responses to framed messages about cancer screening, a number of findings are worth noting. First, the relationship between perceived susceptibility of developing breast cancer and perceived riskiness associated with obtaining a mammogram is an area that requires further examination. Prospect theory suggests that the risk associated with the behavioral choice at hand—in our case, whether or not to obtain a mammogram— should be the key factor that determines how framing affects decision making. It is interesting to note that we did not find that women's perception of susceptibility to developing breast cancer was associated with either their construal of the purpose of mammography or their perceived risks associated with screening. A majority of women in our sample construed mammography as an illness-detecting behavior, emphasizing that even women who perceived lower susceptibility to breast cancer were likely to construe a mammogram as something that detects a problem rather than affirms that they are healthy. Thus, it may not be surprising that no gain-frame advantage emerged among women with lower perceptions of susceptibility, as they were still more likely to view obtaining a mammogram as a potentially risky, illness-detecting behavior.
We also did not find that the effect of framing on screening was moderated by women's construals of mammography as illness-detecting or health-affirming. Indeed, the only study to show that construals of the function a real screening behavior moderate people's responses to framed messages is Apanovitch et al.'s (2003) study of HIV testing. In this study, gain-framed messages were more effective in promoting screening than loss-framed messages, but only for women who felt certain that the results of the test would be negative. We believe the difference between our findings and Apanovitch et al.'s (2003) findings may be due to differences in how women arrive at either an illness-detecting or health-affirming construal of each screening test. With HIV, risk factors are largely under a person's behavioral control, so a person's construal of an HIV test as being health-affirming is likely to be rooted in a clearer awareness of their own objective risk status. In contrast, risk factors for breast cancer are much less controllable and less well understood by many women (Pearlman, Clark, Rakowski, & Ehrich, 1999), and a woman can never be fully certain that she is at no objective risk. However, factors such as a woman's knowledge of breast cancer risks, her family history of breast cancer, or her history of clear-screening results may lead her to form a firmer construal of mammography as healthaffirming. Therefore, it may be that when a woman's construal of a screening test is rooted in knowledge and experience with the health issue, it may emerge as the belief that shapes how she responds to framed messages. Indeed, we have found that among women who have a family history of breast cancer, their construal of mammography moderates their responses to framed messages, such that loss-framed messages are more effective in promoting screening for those with illness-detecting construals but gain-framed messages are more effective for those with health-affirming construals (Updegraff, Rothman, & Gallagher, 2010). Future research should examine the contexts in which a person's unique construals of screening, rather than perceptions of susceptibility, regulate their response to framed messages.
Although risks associated with mammography screening only marginally moderated the influence of message framing on screening, this was independent of the influence of perceived susceptibility on screening. Thus, we found evidence that other distinct beliefs about risk moderated message-framing effects, albeit to a somewhat lesser degree than perceived susceptibility. Some of the specific beliefs assessed by the measure of risks associated with screening are likely to be increasingly important in understanding women's use of mammography in the future. Public and scientific debate has emerged in regard to the effectiveness of mammography in preventing cancer-related death as well as the proper schedule at which women should be screened (Esserman, Shieh, & Thompson, 2009; U.S. Preventive Services Task Force, 2009). To the extent that these debates lead to greater public uncertainty and ambiguity about mammography, the more these beliefs are likely to shape women's responses to messages that promote screening. Accordingly, as public beliefs of risk and uncertainty of mammography screening increase, loss-framed messages may become more effective at promoting appropriate screening behavior.
A potential limitation of the study was the manner in which the outcome was assessed. Although our outcome was based on self-report rather than medical records, we asked women to provide the location and date of their screening to deter false reports. Furthermore, we have no reason to believe that any biases in self-report would explain our pattern of findings. Our self-reported behavioral follow-up was also short compared with other studies that have used 6-month and 12-month follow-ups (Banks et al., 1995; Schneider et al., 2001), therefore our findings are most descriptive of how perceived susceptibility and message framing interact to motivate more immediate rather than long-term responses.
In sum, this study provides the first systematic test of how women's unique beliefs about the risks and uncertainties of mammography screening and breast cancer shape their responses to framed health messages. As such, it highlights the key role that perceived susceptibility plays in determining which way of framing messages is most effective in motivating cancer screening. Indeed, our finding that loss-framed messages motivated screening for women who were at average and higher perceived susceptibility for breast cancer suggests that message framing has a place in communications that promote mammography, and cancer screenings in general.
Acknowledgments
Funding for this project was provided by Grant R03 CA128468 from the National Cancer Institute and a grant from the Kent-SUMMA Center for the Treatment and Study of Traumatic Stress to John A. Updegraff. We thank Jessica Demming, Laura Glass, and Vanessa Potter for help with data collection.
References
- Aiken LS, Fenaughty AM, West SG, Johnson JJ, Luckett TL. Perceived determinants of risk for breast cancer and the relations among objective risk, perceived risk, and screening behavior over time. Women and Health. 1995;1:27–50. [PubMed] [Google Scholar]
- American Cancer Society . Breast Cancer Facts & Figures 2007–2008. American Cancer Society; Atlanta, GA: 2007. [Google Scholar]
- Apanovitch AM, McCarthy D, Salovey P. Using message framing to motivate HIV testing among low-income, ethnic minority women. Health Psychology. 2003;22:60–67. doi: 10.1037//0278-6133.22.1.60. [DOI] [PubMed] [Google Scholar]
- Banks SM, Salovey P, Greener S, Rothman AJ, Moyer A, Beauvais J, Epel E. The effects of message framing on mammography utilization. Health Psychology. 1995;14:178–184. doi: 10.1037//0278-6133.14.2.178. [DOI] [PubMed] [Google Scholar]
- Bartels RD, Kelly KM, Rothman AJ. Moving beyond the function of the health behaviour: The effect of message frame on behavioural decision-making. Psychology & Health. 2010;25:821–838. doi: 10.1080/08870440902893708. [DOI] [PubMed] [Google Scholar]
- Blackman DK, Bennett EM, Miller DS. Trends in self-reported use of mammograms and papanicolaou tests: Behavioral risk factor surveillance system. Morbidity and Mortality Weekly Report. 1999;48:1–22. [PubMed] [Google Scholar]
- Burack RC, George J, Gurney JG. Mammography use among women as a function of age and patient involvement in decision-making. Journal of American Geriatrics Society. 2000;40:817–821. doi: 10.1111/j.1532-5415.2000.tb04759.x. [DOI] [PubMed] [Google Scholar]
- Champion VL. Revised susceptibility, benefits, and barriers scale for mammography screening. Research in Nursing and Health. 1999;22:341–348. doi: 10.1002/(sici)1098-240x(199908)22:4<341::aid-nur8>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Cioffi D. Asymmetry of doubt in medical self-diagnosis: The ambiguity of “uncertain wellness.”. Journal of Personality and Social Psychology. 1991;62:969–980. doi: 10.1037//0022-3514.61.6.969. [DOI] [PubMed] [Google Scholar]
- Clark MA, Rakowski W, Bonacore LB. Repeat mammography: Prevalence estimates and considerations for assessment. Annals of Behavioral Medicine. 2003;26:201–211. doi: 10.1207/S15324796ABM2603_05. [DOI] [PubMed] [Google Scholar]
- Edwards A, Elwyn G, Covey J, Matthews E, Pill R. Presenting risk information—a review of the effects of framing and other manipulations on patient outcomes. Journal of Health Communication. 2001;6:61–82. doi: 10.1080/10810730150501413. [DOI] [PubMed] [Google Scholar]
- Esserman L, Shieh Y, Thompson I. Rethinking screening for breast cancer and prostate cancer. Journal of the American Medical Association. 2009;302:1685–1692. doi: 10.1001/jama.2009.1498. [DOI] [PubMed] [Google Scholar]
- Finney LJ, Iannotti RJ. The impact of family history of breast cancer on women's health beliefs, salience of breast cancer family history, and degree of involvement in breast cancer issues. Women and Health. 2001;33:15–28. [PubMed] [Google Scholar]
- Finney LJ, Iannotti RJ. Message framing and mammography screening: A theory-driven intervention. Behavioral Medicine. 2002;28:5–14. doi: 10.1080/08964280209596393. [DOI] [PubMed] [Google Scholar]
- Fox SA, Murata PJ, Stein JA. The impact of physician compliance on screening mammography for older women. Archives of Internal Medicine. 1991;151:50–56. [PubMed] [Google Scholar]
- Han PKJ, Kobrin SC, Klein WMP, Davis WW, Stefanek M, Taplin SH. Perceived ambiguity about screening mammography recommendations: Association with future mammography uptake and perceptions. Cancer Epidemiology, Biomarkers & Prevention. 2007;16:458. doi: 10.1158/1055-9965.EPI-06-0533. [DOI] [PubMed] [Google Scholar]
- Horner MJ, Ries LAG, Krapcho M, Neyman N, Aminou R, Howlader N, Edwards BK. SEER Cancer Statistics Review, 1975–2006. National Cancer Institute. 2006 Retrieved from http://seer.cancer.gov/csr/1975_2006/
- Howard M, Agarwal G, Lytwyn A. Accuracy of self-reports of Pap and mammography screening compared to medical record: A meta-analysis. Cancer Causes & Control. 2009;20:1–13. doi: 10.1007/s10552-008-9228-4. [DOI] [PubMed] [Google Scholar]
- Humphrey LL, Helfand M, Chan BKS, Woolf SH. Breast cancer screening: Summary of the evidence. Annals of Internal Medicine. 2002;137:344–346. doi: 10.7326/0003-4819-137-5_part_1-200209030-00012. [DOI] [PubMed] [Google Scholar]
- Jaccard J. Interaction effects in logistic regression. Sage; Thousand Oaks, CA: 2001. [Google Scholar]
- Kahneman D, Tversky A. Prospect theory: An analysis of decision under risk. Econometrica. 1979;47:263–291. [Google Scholar]
- Katapodi MC, Lee KA, Facione NC, Dodd MJ. Predictors of perceived breast cancer risk and the relation between perceived risk and breast cancer screening: A meta-analytic review. Preventive Medicine. 2004;38:388–402. doi: 10.1016/j.ypmed.2003.11.012. [DOI] [PubMed] [Google Scholar]
- Lalor KM, Hailey BJ. The effects of message framing and feelings of susceptibility to breast cancer on reported frequency of breast self-examination. International Quarterly of Community Health Education. 1990;10:183–192. doi: 10.2190/GMFB-WYND-QJYA-8LJC. [DOI] [PubMed] [Google Scholar]
- Lerman C, Ross E, Boyce A, Gorchov PM, McLaughlin R, Rimer B, Engstrom P. The impact of mailing psychoeducational materials to women with abnormal mammograms. American Journal of Public Health. 1992;82:729–730. doi: 10.2105/ajph.82.5.729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerman C, Schwartz M. Adherence and psychological adjustment among women at high risk for breast cancer. Breast Cancer Research and Treatment. 1993;28:145–155. doi: 10.1007/BF00666427. [DOI] [PubMed] [Google Scholar]
- Meyerowitz BE, Chaiken S. The effect of message framing on breast self-examination attitudes, intentions, and behavior. Journal of Personality and Social Psychology. 1987;52:500–510. doi: 10.1037//0022-3514.52.3.500. [DOI] [PubMed] [Google Scholar]
- O'Keefe DJ, Jensen JD. The relative persuasiveness of gain-framed and loss-framed messages for encouraging disease detection behaviors: A meta-analytic review. Journal of Communication. 2009;59:296–316. doi: 10.1080/10810730701615198. [DOI] [PubMed] [Google Scholar]
- Pearlman DN, Clark MA, Rakowksi W, Ehrich B. Screening for breast and cervical cancers: The importance of knowledge and perceived cancer survivability. Women and Health. 1999;28:93–112. doi: 10.1300/J013v28n04_06. [DOI] [PubMed] [Google Scholar]
- Rakowski W, Andersen MR, Stoddard AM, Urban N, Rimer BK, Lane DS, Costanza ME. Confirmatory analysis of opinions regarding the pros and cons of mammography. Health Psychology. 1997;5:433–441. doi: 10.1037//0278-6133.16.5.433. [DOI] [PubMed] [Google Scholar]
- Rakowski W, Breen N, Meissner H, Rimer BK, Vernon SW, Clark MA, Freedman AN. Prevalence and correlates of repeat mammography among women aged 55–79 in the Year 2000 National Health Interview Survey. Preventive Medicine. 2004;39:1–10. doi: 10.1016/j.ypmed.2003.12.032. [DOI] [PubMed] [Google Scholar]
- Rauscher GH, Johnson TP, Cho YI, Walk JA. Accuracy of self-reported cancer-screening histories: A meta-analysis. Cancer Epidemiology, Biomarkers & Prevention. 2008;17:748–757. doi: 10.1158/1055-9965.EPI-07-2629. [DOI] [PubMed] [Google Scholar]
- Rothman AJ, Kelly KM, Hertel A, Salovey P. Message frames and illness representations: Implications for interventions to promote and sustain healthy behavior. In: Cameron LD, Leventhal H, editors. The self-regulation of health and illness behavior. Routledge; London, England: 2003. pp. 278–296. [Google Scholar]
- Rothman AJ, Salovey P. Shaping perceptions to motivate healthy behavior: The role of message framing. Psychological Bulletin. 1997;121:3–19. doi: 10.1037/0033-2909.121.1.3. [DOI] [PubMed] [Google Scholar]
- Schneider TR, Salovey P, Apanovitch AM, Pizarro J, McCarthy D, Zullo J, Rothman AJ. The effects of message framing and ethnic targeting on mammography use among low-income women. Health Psychology. 2001;20:256–266. doi: 10.1037//0278-6133.20.4.256. [DOI] [PubMed] [Google Scholar]
- Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211:453–458. doi: 10.1126/science.7455683. [DOI] [PubMed] [Google Scholar]
- Updegraff JA, Rothman AJ, Gallagher KM. Tailoring framed messages to women's construals of mammography. 2010. Manuscript in preparation. [Google Scholar]
- U.S. Preventive Services Task Force Screening for breast cancer: U.S. preventive services task force recommendation statement. Annals of Internal Medicine. 2009;151:716–726. doi: 10.7326/0003-4819-151-10-200911170-00008. [DOI] [PubMed] [Google Scholar]
- Vernon SW, Vogel VG, Halabi S, Bondy ML. Factors associated with perceived risk of breast cancer among women attending a screening program. Breast Cancer Research and Treatment. 1993;28:137–144. doi: 10.1007/BF00666426. [DOI] [PubMed] [Google Scholar]
- Williams T, Clarke V, Borland R. Effects of message framing on breast-cancer-related beliefs and behaviors: The role of mediating factors. Journal of Applied Social Psychology. 2001;31:925–950. [Google Scholar]