Abstract
The nucleus accumbens (NAc) is a key component of the brain reward system, and it is composed of core and shell subregions. Glutamate transmission through AMPA-type receptors in both core and shell of the NAc has been shown to regulate reward- and aversion-type behaviors. Previous studies have additionally demonstrated a role for AMPA receptor signaling in the NAc in chronic pain states. Here, we show that persistent neuropathic pain, modeled by spared nerve injury (SNI), selectively increases the numbers of GluA1 subunits of AMPA receptors at the synapse of both core and shell subregions. Such increases are not observed, however, for the GluA2 subunits. Furthermore, we find that phosphorylation at Ser845-GluA1 is increased by SNI at both core and shell subregions. These results demonstrate that persistent neuropathic pain increases AMPA receptor delivery to the synapse in both NAc core and shell, implying a role for AMPA receptor signaling in these regions in pain states.
Keywords: GluA1, nucleus accumbens, SNI, neuropathic pain, core, shell
1. Introduction
The nucleus accumbens (NAc) is well-known to mediate reward-based and aversion-driven behaviors [19, 31]. Not surprisingly, human imaging studies have consistently shown that chronic pain activates the NAc [3, 4, 6]. At the circuit level, the NAc forms reciprocal projections with a number of regions critical for pain regulation including the amygdala, thalamus, prefrontal cortex (PFC) and hippocampus [1, 2, 32]. At the molecular level, opioid signaling in the NAc mediates placebo effects, whereas dopamine signaling has been shown to regulate descending inhibition, stress-induced hyperalgesia, and negative reinforcement from pain-relief [20, 38, 41, 48]. Thus, based on imaging and pharmacological studies, the NAc likely plays an important role in the regulation of chronic pain. The NAc is composed of the core and shell subregions, and synaptic events in both regions are involved in reward-based behaviors [7, 25, 34, 42, 43]. However, the effect of chronic pain on molecular signaling specifically in the core or shell subregion is not yet known.
Previous studies have shown that glutamate signaling in the NAc can regulate pain sensitivity [20, 21, 23]. While there are multiple glutamate receptors in the NAc, transmission through AMPA receptors is particularly important in reward- and aversion-driven behaviors [15, 28, 42, 47, 54]. AMPA receptors are composed of four subunits, GluA1-4. The majority of AMPA receptors contains GluA2 subunits and is impermeable to Ca2+. On the other hand, GluA2-lacking AMPA receptors, predominantly formed by GluA1 homomers, conduct Ca2+ and are also known as Ca2+-permeable AMPA receptors (CPARs) [16, 35]. Chronic pain has been shown to selectively increase GluA1 subunit levels at the synapse in the NAc, likely through increased trafficking, and this selective increase in GluA1 subunits leads to the formation of CPARs [24, 51]. CPARs, in turn, can regulate the affective symptoms of chronic pain [24]. However, it is not yet known whether increased synaptic delivery of GluA1 subunits occurs specifically in the core or shell subregion of the NAc in chronic pain states.
In this study, we examined AMPA receptor subunit levels at the synapse of core and shell subregions of the NAc using a well-known chronic neuropathic pain model (spared nerve injury – SNI – model). We found that chronic pain selectively increases GluA1 levels at the synapse in both the core and the shell, hence suggesting a role of AMPA receptor signaling in both regions for pain regulation.
2. Methods
2.1. Animals
All procedures in this study were approved by the New York University School of Medicine Institutional Animal Care and Use Committee (IACUC) as consistent with the National Institute of Health (NIH) Guide for the Care and Use of Laboratory Animals (publication number 85-23) to ensure minimal animal use and discomfort. Male Sprague-Dawley rats were purchased from Taconic Farms, Albany, NY and kept in the NYU Langone Medical Center’s Central Animal Facility and at Mispro Biotech Services Facility in Alexandria Center for Life Science, with controlled humidity, room temperature, and 12-h (6:30 AM to 6:30 PM) light-dark cycle. Food and water were available ad libitum. Animals arrived to the animal facility at 250 to 300 grams and were given on average 10 days to adjust to the new environment prior to the onset of any experiments.
2.2. Spared Nerve Injury (SNI) surgery
The Spared Nerve Injury (SNI) surgery was previously described in detail [17, 57]. Briefly, under Isoflurane anesthesia (1.5 to 2%), the skin on the lateral surface of the right thigh of rat was incised, and a section was made through the biceps femoris muscle to expose the three branches of sciatic nerve: sural, common peroneal and tibial nerves. The common peroneal and tibial nerves were tied with non-absorbent 5.0 silk sutures at the point of trifurcation. The nerves were then cut distal to each knot, and about 3 to 5 mm of the distal ends were removed. In sham surgeries (control), above nerves were dissected but not cut. Muscle layer was then sutured close, while skin was stapled. Staples were removed prior to behavioral testing.
2.3. Subcellular fractionation and Western blotting
Rats were anesthetized with isofluorane (1.5–2%) and decapitated immediately. Brains were quickly removed and nucleus accumbens were collected on ice. The NAc were dissected from 1.08 to 2.52mm anterior to Bregma, with an average sample weight of 40mg. Dissections of core and shell were performed according to coordinates of the standard rat atlas. The NAc core was dissected using a circular micropunch of approximately 1mm radius centered at the anterior commissure, and areas medial and ventro-lateral to (immediately surrounding) the NAc core were collected as NAc shell under a dissecting microscope [37, 55]. Synaptosome fractions of core and shell were prepared as described previously [29, 46]. Briefly, samples were homogenized in an ice-cold solution A (0.32 M sucrose, 1 mM NaHCO3, 1 mM MgCl2, 0.5 mM CaCl2, 0.1 mM PMSF and 1x Complete Protease Inhibitors). Homogenates were centrifuged at 4,000 rpm for 10 min. The supernatant was collected and the pellet re-homogenized in solution A and centrifuged again for 10 min. Combined supernatants were subjected to a second centrifugation at 3,000 rpm for 10 min. Supernatants were then spun at 14,000 rpm for 30 minutes. Pellet was resuspended in solution B (0.32 M sucrose, 1 mM NaHCO3) and homogenized. Homogenate was layered on top of a 5 mL 1 M sucrose and 1.2 M sucrose gradient and centrifuged at 30,000 rpm for 2 hours. Purified synaptosomes were collected at the 1 M and 1.2 M sucrose interface, suspended in solution B and centrifuged at 40,000 rpm for 45 min. Synaptosomal pellets were resuspended in 25 mM TRIS with 4% SDS. Fractions were analyzed by Western blot on SDS-PAGE gels as described previously [29, 46]. The following antibodies were used: GluA1 (1:1,000, Millipore), phospho-Ser 845 GluA1 (1:1,000, Millipore), GluA2 (1:1,000, Millipore) and tubulin (1:30,000, Sigma).
2.4. Animal Behavioral Tests
Mechanical allodynia test
A traditional Dixon up-down method with von Frey filaments was used to measure mechanical allodynia as described previously [9, 12, 57]. Rats were individually placed into plexiglass chambers over a mesh table and acclimated for 20 min before the onset of examination. Beginning with 2.55g, von Frey filaments in a set with logarithmically incremental stiffness (0.45, 0.75, 1.20, 2.55, 4.40, 6.10, 10.50, 15.10 g) were applied to the lateral 1/3 of right paws (in the distribution of the sural nerve) of rats. 50% withdrawal threshold was calculated as described previously [57].
Cold allodynia test
Animals were individually placed into plexiglass chambers and acclimated for 20 min. A drop of acetone was applied to the lateral plantar surface of the paws. As previously described [26, 30, 57], the following scoring system was applied. 0: no visible response or startle response lasting <0.5 second; 1: paw withdrawal lasting <5 seconds; 2: withdrawal lasting 5 to 10 seconds; 3: prolonged repetitive withdrawal lasting > 10s. Acetone was applied 5 times to each paw, and an average score was calculated. Cold allodynia tests were typically done after mechanical allodynia tests, and observers were blinded to the test conditions.
2.5. Statistical analysis
For mechanical and cold allodynia, a two-way ANOVA with repeated measures and post hoc multiple pair-wise comparison Bonferroni tests was used to compare the 50% withdrawal threshold and cold scores of SNI- and sham-treated rats. For Western blots, unpaired two-tailed Student’s t tests were used to analyze the protein levels in SNI- versus sham-treated rats. All data were analyzed using GraphPad Prism Version 5 software (GraphPad, La Jolla, CA).
3. Results
3.1. SNI causes persistent neuropathic pain
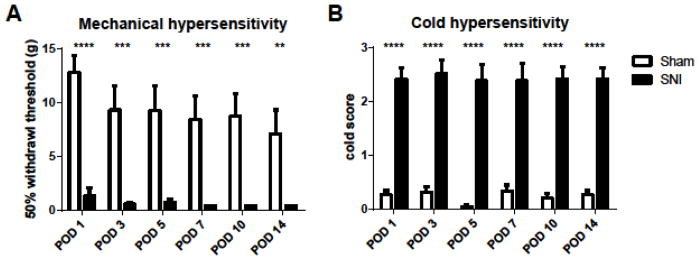
We used the SNI model, a peripheral nerve injury model of chronic neuropathic pain [17, 57], to study the effect of pain on AMPA receptor trafficking in the NAc. We surgically resected two of three branches of the sciatic nerve, causing permanent nerve injury and neuropathic pain [17]. One day after the SNI procedure, rats began to experience mechanical allodynia, as demonstrated by a decreased paw withdrawal threshold compared with control (sham-treated) rats (1.3gm vs. 12.8gm, p<0.0001, Fig. 1A). Likewise, SNI-treated rats displayed cold allodynia, as shown by an increased cold score compared with control rats (2.24 vs. 0.26, p<0.0001, Fig. 1B). Phenotypes of mechanical and cold allodynia indicate the development of neuropathic pain. Similar to earlier reports in SNI-treated rats, symptoms of allodynia persisted for at least 14 days (a decrease in mechanical threshold from 7.1gm to 0.45gm on day 14 after SNI, p<0.01, Fig. 1A; an increase in cold score from 0.27 to 2.24, p<0.0001, Fig. 1B) [17, 24, 57].
Figure 1.
SNI causes persistent neuropathic pain. A, SNI-operated rats developed mechanical allodynia after surgery, compared with sham-operated rats. Two-way ANOVA with repeated measures and Bonferroni post-test. n=9–10, ** p<0.01. B, Animals after SNI developed cold allodynia. Two-way ANOVA. n=9–10, **** p<0.0001. Error bars show mean and s.e.m.
3.2. SNI increases GluA1 levels at the synapse of core and shell subregions of the NAc
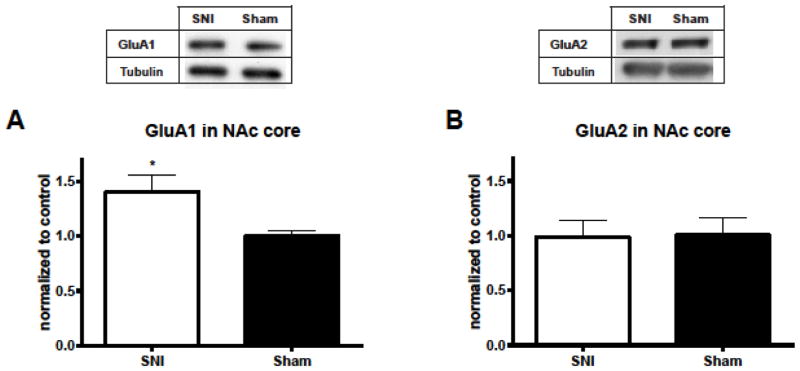
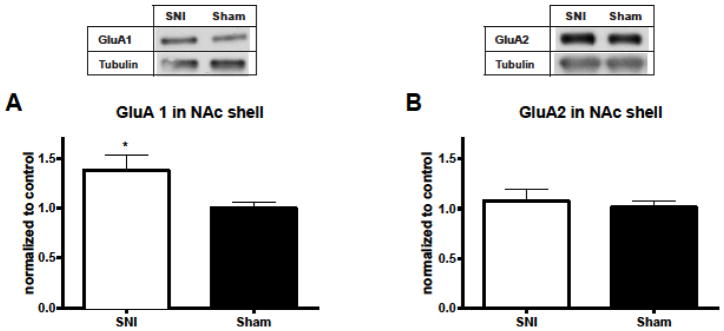
To understand how chronic pain regulates AMPA receptor signaling in the NAc, we measured the levels of AMPA receptor subunits from synaptoneurosome preparations of NAc neurons 14 days after SNI or sham surgery. Over 90% of neurons in the NAc are medium spiny neurons (MSNs), and synaptoneurosome preparations reflect synaptic fractions of these neurons. GluA1 and 2 are predominantly expressed in the MSNs. The NAc is comprised of core and shell subregions. This anatomic distinction has been shown to have functional significance [50]. Thus, we measured GluA1 and GluA2 levels in the core and the shell. We found a substantial (40%) increase in the GluA1 subunit levels in the NAc core of SNI-treated animals compared with GluA1 levels in sham controls (p<0.05, Fig. 2A). The level of GluA2 subunits in the core, in contrast, remained unchanged (Fig. 2B). Next, we measured GluA1 and GluA2 levels in the shell subregion of NAc. Similar to what we found in the NAc core, GluA1 levels are also elevated (by 37%) at the synapse of the shell in SNI-treated rats, whereas GluA2 levels remain the same (Fig. 3A, B). These results indicate that chronic pain causes a selective increase in the GluA1 subunit levels in both core and shell subregions of the NAc.
Figure 2.
SNI selectively increases GluA1 levels at the synapse of the core subregion of NAc. A, SNI resulted in an increase in GluA1 subunits in the synaptoneurosomes of NAc core. Student’s t test, n=13, * p<0.05. B, SNI caused no changes in GluA2 subunit levels at the synapse. n=9, p>0.05. Data were normalized to values in the sham group.
Figure 3.
SNI selectively increases GluA1 levels at the synapse of the shell subregion of NAc. A, SNI resulted in an increase in GluA1 subunits in the synaptoneurosomes of NAc shell. Student’s t test, n=12, * p<0.05. B, SNI caused no changes in GluA2 subunits at the synapse. n=12, p>0.05. Data were normalized to values in the sham group.
3.3. SNI causes increased GluA1 trafficking to the synaptic surface of NAc core and shell
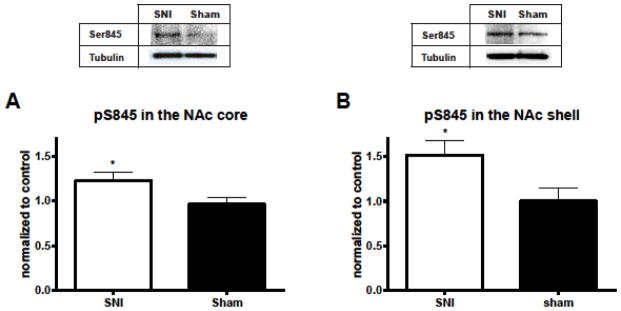
Increased GluA1 subunit expression at the synapse can be caused by increased exocytotic trafficking or localized synthesis. It can also be caused by decreased endocytosis or degradation [5]. To assess the role of trafficking, we measured the level of phosphorylation of the Ser845 residue on the GluA1 protein. The phosphorylation of Ser845 is known to be a required step for the delivery of GluA1 to the synaptic surface [49]. We found that phospho-Ser845 was increased in both core and shell subregions after SNI (p<0.05, Fig. 4A, B). This level of increase is comparable to the increase in levels of GluA1 (Fig. 2A, 3A). These data suggest that this trafficking mechanism is conserved in the chronic pain state and contributes to the accumulation of GluA1 subunits at the synaptic surface.
Figure 4.
SNI increases phosphorylation at Ser845 at synapses of the core and shell subregions. A, SNI increased phosphorylation at the Ser845 residue of GluA1 subunits in the synaptoneurosomes of NAc core. Student’s t test, n=10–11, * p<0.05. B, SNI increased phosphorylation at Ser845 in the synaptoneurosomes of NAc shell. Student’s t test, n=6, * p<0.05. Data were normalized to values in the sham group.
4. Discussion
Imaging studies have identified that chronic pain activates the NAc [3, 4, 6, 22]. However, direct biochemical or biophysical analysis of molecular signaling in the NAc remains lacking in chronic pain models. Particularly, AMPA receptor signaling, which is crucial for the NAc function under rewarding conditions, remains poorly studied at detailed anatomic levels in pain states. Our current study provides the first evidence for pain-induced GluA1 increases at MSN synapses in both core and shell subregions of the NAc.
The SNI model is widely used to study molecular changes in the brain in response to chronic pain [10, 11, 17, 33, 39]. SNI, however, can lead to both nerve injury and pain. A previous study has shown that increases in GluA1 levels at the NAc synapse do not manifest until at least 7 days after SNI, suggesting that persistent pain, rather than acute nerve injury, triggers the synaptic targeting of GluA1 subunits [52]. More importantly, increased GluA1 delivery to the NAc synapse has also been demonstrated in a persistent inflammatory pain model that does not involve nerve injuries [52]. Thus, we believe that chronic pain, rather than nerve injury, causes the GluA1 increases observed in the current study.
A selective increase in GluA1 levels at the synapse suggests the formation of GluA2-lacking AMPA receptors [16, 27, 35]. GluA2-lacking receptors, also known as CPARs, can facilitate intracellular Ca2+ signaling and have higher single unit conductance. These unique biophysical properties enable CPARs to play an important role at the synapse, including the induction of long-term potentiation (LTP) or long-term depression (LTD) [16, 27, 35]. By regulating synaptic strength, CPARs modulate a diverse set of behaviors [14, 15, 24, 34, 55, 56]. Our data raises the possibility of CPAR formation in both the core and shell subregions in pain states. Of course, further physiological studies are needed to test such possibilities. Additionally, whereas GluA2 subunits are constitutively trafficked to the synapse, the synaptic incorporation of GluA1 subunits requires sequential phosphorylations at Ser845 and Ser818 residues [8, 18, 49, 53]. Our data confirms that the phosphorylation of Ser845 is involved in the synaptic targeting of GluA1 subunits to the NAc synapse in chronic pain states. Our data, however, do not necessarily exclude other potential causes for increased GluA1 levels such as increased local synthesis.
A number of studies have described GluA1 upregulation in the NAc after repeated or prolonged consumption of natural rewards or cocaine [45, 55]. In these studies, homeostatic plasticity has been posited as a possible mechanism for the increase in GluA1 subunits. In these studies on rewards, the length of time required to increase GluA1 levels is in general compatible with the time course found in our study. Similarly, in a previous study on AMPA receptor trafficking, GluA1 upregulation at the NAc synapse is found to occur after pain has become persistent or chronic [52]. Thus, we speculate that GluA1 upregulation in the core and shell of NAc in persistent pain states may represent a form of homeostatic plasticity in the reward system. It would be interesting to test this potential mechanism in future studies.
Both core and shell subregions of the NAc have been shown to regulate reward and aversion-driven behaviors [13, 34, 40], and previous studies indicate that the core plays a role in nociception as well [20, 36]. While core and shell are both composed primarily of MSNs, there are differences between these two regions in terms of cellular morphology, neurochemistry, and afferent and efferent projections [50]. Functionally, the core is thought to mediate cue-conditioned behavioral activation, such as reward-seeking. The shell, meanwhile, has been shown to code the salience of a behavioral condition [50]. Our data demonstrates that AMPA receptor plasticity occurs in both regions under chronic pain conditions. Thus, we expect that glutamate signaling in the core could regulate behavioral responses to pain such as drug seeking or avoidance of pain stimulus, whereas signaling in the shell could regulate the processing of the aversive quality of pain [13, 40, 44].
5. Conclusion
In conclusion, our results show that chronic pain leads to selective GluA1 upregulation at the synapse of core and shell regions of the NAc. These results indicate that AMPA receptor signaling in both regions is likely to play an important role in the pathogenesis and regulation of chronic pain.
HIGHLIGHTS.
We showed that spared nerve injury causes persistent neuropathic pain
We showed that GluA1 levels at synapses are increased in both core and shell subregions of the NAc in chronic pain conditions
We showed that chronic pain causes an increase in the phosphorylation of Ser845 residue of the GluA1 in the NAc
Acknowledgments
This work was supported by the National Institute for General Medical Sciences (GM102691 and GM115384) and the Foundation for Anesthesia Education and Research (MRTG-BS-02/15/2010).
Footnotes
The authors declare no competing financial interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ansah OB, Bourbia N, Goncalves L, Almeida A, Pertovaara A. Influence of amygdaloid glutamatergic receptors on sensory and emotional pain-related behavior in the neuropathic rat. Behav Brain Res. 2010;209:174–178. doi: 10.1016/j.bbr.2010.01.021. [DOI] [PubMed] [Google Scholar]
- 2.Apkarian AV, Sosa Y, Sonty S, Levy RM, Harden RN, Parrish TB, Gitelman DR. Chronic back pain is associated with decreased prefrontal and thalamic gray matter density. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2004;24:10410–10415. doi: 10.1523/JNEUROSCI.2541-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baliki MN, Geha PY, Fields HL, Apkarian AV. Predicting value of pain and analgesia: nucleus accumbens response to noxious stimuli changes in the presence of chronic pain. Neuron. 2010;66:149–160. doi: 10.1016/j.neuron.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baliki MN, Petre B, Torbey S, Herrmann KM, Huang L, Schnitzer TJ, Fields HL, Apkarian AV. Corticostriatal functional connectivity predicts transition to chronic back pain. Nat Neurosci. 2012;15:1117–1119. doi: 10.1038/nn.3153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barry MF, Ziff EB. Receptor trafficking and the plasticity of excitatory synapses. Curr Opin Neurobiol. 2002;12:279–286. doi: 10.1016/s0959-4388(02)00329-x. [DOI] [PubMed] [Google Scholar]
- 6.Becerra L, Borsook D. Signal valence in the nucleus accumbens to pain onset and offset. Eur J Pain. 2008;12:866–869. doi: 10.1016/j.ejpain.2007.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berton O, McClung CA, Dileone RJ, Krishnan V, Renthal W, Russo SJ, Graham D, Tsankova NM, Bolanos CA, Rios M, Monteggia LM, Self DW, Nestler EJ. Essential role of BDNF in the mesolimbic dopamine pathway in social defeat stress. Science. 2006;311:864–868. doi: 10.1126/science.1120972. [DOI] [PubMed] [Google Scholar]
- 8.Boehm J, Kang MG, Johnson RC, Esteban J, Huganir RL, Malinow R. Synaptic incorporation of AMPA receptors during LTP is controlled by a PKC phosphorylation site on GluR1. Neuron. 2006;51:213–225. doi: 10.1016/j.neuron.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 9.Bourquin AF, Suveges M, Pertin M, Gilliard N, Sardy S, Davison AC, Spahn DR, Decosterd I. Assessment and analysis of mechanical allodynia-like behavior induced by spared nerve injury (SNI) in the mouse. Pain. 2006;122:14 e11–14. doi: 10.1016/j.pain.2005.10.036. [DOI] [PubMed] [Google Scholar]
- 10.Cardoso-Cruz H, Dourado M, Monteiro C, Matos MR, Galhardo V. Activation of dopaminergic D2/D3 receptors modulates dorsoventral connectivity in the hippocampus and reverses the impairment of working memory after nerve injury. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2014;34:5861–5873. doi: 10.1523/JNEUROSCI.0021-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cardoso-Cruz H, Lima D, Galhardo V. Impaired spatial memory performance in a rat model of neuropathic pain is associated with reduced hippocampus-prefrontal cortex connectivity. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2013;33:2465–2480. doi: 10.1523/JNEUROSCI.5197-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL. Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods. 1994;53:55–63. doi: 10.1016/0165-0270(94)90144-9. [DOI] [PubMed] [Google Scholar]
- 13.Chen YW, Rada PV, Butzler BP, Leibowitz SF, Hoebel BG. Corticotropin-releasing factor in the nucleus accumbens shell induces swim depression, anxiety, and anhedonia along with changes in local dopamine/acetylcholine balance. Neuroscience. 2012;206:155–166. doi: 10.1016/j.neuroscience.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 14.Clem RL, Huganir RL. Calcium-permeable AMPA receptor dynamics mediate fear memory erasure. Science. 2010;330:1108–1112. doi: 10.1126/science.1195298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Conrad KL, Tseng KY, Uejima JL, Reimers JM, Heng LJ, Shaham Y, Marinelli M, Wolf ME. Formation of accumbens GluR2-lacking AMPA receptors mediates incubation of cocaine craving. Nature. 2008;454:118–121. doi: 10.1038/nature06995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cull-Candy S, Kelly L, Farrant M. Regulation of Ca2+-permeable AMPA receptors: synaptic plasticity and beyond. Curr Opin Neurobiol. 2006;16:288–297. doi: 10.1016/j.conb.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 17.Decosterd I, Woolf CJ. Spared nerve injury: an animal model of persistent peripheral neuropathic pain. Pain. 2000;87:149–158. doi: 10.1016/S0304-3959(00)00276-1. [DOI] [PubMed] [Google Scholar]
- 18.Esteban JA, Shi SH, Wilson C, Nuriya M, Huganir RL, Malinow R. PKA phosphorylation of AMPA receptor subunits controls synaptic trafficking underlying plasticity. Nat Neurosci. 2003;6:136–143. doi: 10.1038/nn997. [DOI] [PubMed] [Google Scholar]
- 19.Fields HL. Understanding how opioids contribute to reward and analgesia. Reg Anesth Pain Med. 2007;32:242–246. doi: 10.1016/j.rapm.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 20.Gear RW, Aley KO, Levine JD. Pain-induced analgesia mediated by mesolimbic reward circuits. Journal of Neuroscience. 1999;19:7175–7181. doi: 10.1523/JNEUROSCI.19-16-07175.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gear RW, Levine JD. Rostral ventral medulla cholinergic mechanism in pain-induced analgesia. Neurosci Lett. 2009;464:170–172. doi: 10.1016/j.neulet.2009.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Geha PY, Baliki MN, Harden RN, Bauer WR, Parrish TB, Apkarian AV. The brain in chronic CRPS pain: abnormal gray-white matter interactions in emotional and autonomic regions. Neuron. 2008;60:570–581. doi: 10.1016/j.neuron.2008.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ghalandari-Shamami M, Hassanpour-Ezatti M, Haghparast A. Intra-accumbal NMDA but not AMPA/kainate receptor antagonist attenuates WIN55,212-2 cannabinoid receptor agonist-induced antinociception in the basolateral amygdala in a rat model of acute pain. Pharmacol Biochem Behav. 2011;100:213–219. doi: 10.1016/j.pbb.2011.08.027. [DOI] [PubMed] [Google Scholar]
- 24.Goffer Y, Xu D, Eberle SE, D’Amour J, Lee M, Tukey D, Froemke RC, Ziff EB, Wang J. Calcium-permeable AMPA receptors in the nucleus accumbens regulate depression-like behaviors in the chronic neuropathic pain state. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2013;33:19034–19044. doi: 10.1523/JNEUROSCI.2454-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Golden SA, Christoffel DJ, Heshmati M, Hodes GE, Magida J, Davis K, Cahill ME, Dias C, Ribeiro E, Ables JL, Kennedy PJ, Robison AJ, Gonzalez-Maeso J, Neve RL, Turecki G, Ghose S, Tamminga CA, Russo SJ. Epigenetic regulation of RAC1 induces synaptic remodeling in stress disorders and depression. Nat Med. 2013;19:337–344. doi: 10.1038/nm.3090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hao JX, Shi TJ, Xu IS, Kaupilla T, Xu XJ, Hokfelt T, Bartfai T, Wiesenfeld-Hallin Z. Intrathecal galanin alleviates allodynia-like behaviour in rats after partial peripheral nerve injury. Eur J Neurosci. 1999;11:427–432. doi: 10.1046/j.1460-9568.1999.00447.x. [DOI] [PubMed] [Google Scholar]
- 27.Isaac JT, Ashby MC, McBain CJ. The role of the GluR2 subunit in AMPA receptor function and synaptic plasticity. Neuron. 2007;54:859–871. doi: 10.1016/j.neuron.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 28.Javitt DC, Zukin SR. The role of excitatory amino acids in neuropsychiatric illness. J Neuropsychiatry Clin Neurosci. 1990;2:44–52. doi: 10.1176/jnp.2.1.44. [DOI] [PubMed] [Google Scholar]
- 29.Jordan BA, Fernholz BD, Boussac M, Xu C, Grigorean G, Ziff EB, Neubert TA. Identification and verification of novel rodent postsynaptic density proteins. Mol Cell Proteomics. 2004;3:857–871. doi: 10.1074/mcp.M400045-MCP200. [DOI] [PubMed] [Google Scholar]
- 30.Jorum E, Warncke T, Stubhaug A. Cold allodynia and hyperalgesia in neuropathic pain: the effect of N-methyl-D-aspartate (NMDA) receptor antagonist ketamine--a double-blind, crossover comparison with alfentanil and placebo. Pain. 2003;101:229–235. doi: 10.1016/S0304-3959(02)00122-7. [DOI] [PubMed] [Google Scholar]
- 31.Kalivas PW, Volkow ND. The neural basis of addiction: a pathology of motivation and choice. Am J Psychiatry. 2005;162:1403–1413. doi: 10.1176/appi.ajp.162.8.1403. [DOI] [PubMed] [Google Scholar]
- 32.Kim H, Chen L, Lim G, Sung B, Wang S, McCabe MF, Rusanescu G, Yang L, Tian Y, Mao J. Brain indoleamine 2,3-dioxygenase contributes to the comorbidity of pain and depression. J Clin Invest. 2012;122:2940–2954. doi: 10.1172/JCI61884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li XY, Ko HG, Chen T, Descalzi G, Koga K, Wang H, Kim SS, Shang Y, Kwak C, Park SW, Shim J, Lee K, Collingridge GL, Kaang BK, Zhuo M. Alleviating neuropathic pain hypersensitivity by inhibiting PKMzeta in the anterior cingulate cortex. Science. 2010;330:1400–1404. doi: 10.1126/science.1191792. [DOI] [PubMed] [Google Scholar]
- 34.Lim BK, Huang KW, Grueter BA, Rothwell PE, Malenka RC. Anhedonia requires MC4R-mediated synaptic adaptations in nucleus accumbens. Nature. 2012;487:183–189. doi: 10.1038/nature11160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu SJ, Zukin RS. Ca2+-permeable AMPA receptors in synaptic plasticity and neuronal death. Trends Neurosci. 2007;30:126–134. doi: 10.1016/j.tins.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 36.Magnusson JE, Martin RV. Additional evidence for the involvement of the basal ganglia in formalin-induced nociception: the role of the nucleus accumbens. Brain Research. 2002;942:128–132. doi: 10.1016/s0006-8993(02)02489-7. [DOI] [PubMed] [Google Scholar]
- 37.McCutcheon JE, Wang X, Tseng KY, Wolf ME, Marinelli M. Calcium-permeable AMPA receptors are present in nucleus accumbens synapses after prolonged withdrawal from cocaine self-administration but not experimenter-administered cocaine. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2011;31:5737–5743. doi: 10.1523/JNEUROSCI.0350-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mickey BJ, Sanford BJ, Love TM, Shen PH, Hodgkinson CA, Stohler CS, Goldman D, Zubieta JK. Striatal dopamine release and genetic variation of the serotonin 2C receptor in humans. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2012;32:9344–9350. doi: 10.1523/JNEUROSCI.1260-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mitsi V, Terzi D, Purushothaman I, Manouras L, Gaspari S, Neve RL, Stratinaki M, Feng J, Shen L, Zachariou V. RGS9-2-controlled adaptations in the striatum determine the onset of action and efficacy of antidepressants in neuropathic pain states. Proceedings of the National Academy of Sciences of the United States of America. 2015;112:E5088–5097. doi: 10.1073/pnas.1504283112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Muschamp JW, Van’t Veer A, Parsegian A, Gallo MS, Chen M, Neve RL, Meloni EG, Carlezon WA., Jr Activation of CREB in the nucleus accumbens shell produces anhedonia and resistance to extinction of fear in rats. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2011;31:3095–3103. doi: 10.1523/JNEUROSCI.5973-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Navratilova E, Xie JY, Okun A, Qu C, Eyde N, Ci S, Ossipov MH, King T, Fields HL, Porreca F. Pain relief produces negative reinforcement through activation of mesolimbic reward-valuation circuitry. Proceedings of the National Academy of Sciences of the United States of America. 2012;109:20709–20713. doi: 10.1073/pnas.1214605109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nestler EJ, Carlezon WA., Jr The mesolimbic dopamine reward circuit in depression. Biol Psychiatry. 2006;59:1151–1159. doi: 10.1016/j.biopsych.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 43.Park SK, Nguyen MD, Fischer A, Luke MP, Affar el B, Dieffenbach PB, Tseng HC, Shi Y, Tsai LH. Par-4 links dopamine signaling and depression. Cell. 2005;122:275–287. doi: 10.1016/j.cell.2005.05.031. [DOI] [PubMed] [Google Scholar]
- 44.Pliakas AM, Carlson RR, Neve RL, Konradi C, Nestler EJ, Carlezon WA., Jr Altered responsiveness to cocaine and increased immobility in the forced swim test associated with elevated cAMP response element-binding protein expression in nucleus accumbens. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2001;21:7397–7403. doi: 10.1523/JNEUROSCI.21-18-07397.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reimers JM, Loweth JA, Wolf ME. BDNF contributes to both rapid and homeostatic alterations in AMPA receptor surface expression in nucleus accumbens medium spiny neurons. Eur J Neurosci. 2014;39:1159–1169. doi: 10.1111/ejn.12422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Restituito S, Khatri L, Ninan I, Mathews PM, Liu X, Weinberg RJ, Ziff EB. Synaptic autoregulation by metalloproteases and gamma-secretase. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2011;31:12083–12093. doi: 10.1523/JNEUROSCI.2513-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sanacora G, Treccani G, Popoli M. Towards a glutamate hypothesis of depression: an emerging frontier of neuropsychopharmacology for mood disorders. Neuropharmacology. 2012;62:63–77. doi: 10.1016/j.neuropharm.2011.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Scott DJ, Stohler CS, Egnatuk CM, Wang H, Koeppe RA, Zubieta JK. Placebo and nocebo effects are defined by opposite opioid and dopaminergic responses. Arch Gen Psychiatry. 2008;65:220–231. doi: 10.1001/archgenpsychiatry.2007.34. [DOI] [PubMed] [Google Scholar]
- 49.Serulle Y, Zhang S, Ninan I, Puzzo D, McCarthy M, Khatri L, Arancio O, Ziff EB. A GluR1-cGKII interaction regulates AMPA receptor trafficking. Neuron. 2007;56:670–688. doi: 10.1016/j.neuron.2007.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sesack SR, Grace AA. Cortico-Basal Ganglia reward network: microcircuitry. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology. 2010;35:27–47. doi: 10.1038/npp.2009.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Su C, D’Amour J, Lee M, Lin HY, Manders T, Xu D, Eberle SE, Goffer Y, Zou AH, Rahman M, Ziff E, Froemke RC, Huang D, Wang J. Persistent pain alters AMPA receptor subunit levels in the nucleus accumbens. Molecular brain. 2015;8:46. doi: 10.1186/s13041-015-0140-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Su C, D’Amour J, Lee M, Lin HY, Manders T, Xu D, Eberle SE, Goffer Y, Zou AH, Rahman M, Ziff E, Froemke RC, Huang D, Wang J. Persistent pain alters AMPA receptor subunit levels in the nucleus accumbens. Molecular brain. 2015;8:46. doi: 10.1186/s13041-015-0140-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sun X, Zhao Y, Wolf ME. Dopamine receptor stimulation modulates AMPA receptor synaptic insertion in prefrontal cortex neurons. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2005;25:7342–7351. doi: 10.1523/JNEUROSCI.4603-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tokita K, Yamaji T, Hashimoto K. Roles of glutamate signaling in preclinical and/or mechanistic models of depression. Pharmacol Biochem Behav. 2011 doi: 10.1016/j.pbb.2011.04.016. [DOI] [PubMed] [Google Scholar]
- 55.Tukey DS, Ferreira JM, Antoine SO, D’Amour AJ, Ninan I, Cabeza de Vaca S, Incontro S, Wincott C, Horwitz JK, Hartner DT, Guarini CB, Khatri L, Goffer Y, Xu D, Titcombe RF, Khatri M, Marzan DS, Mahajan SS, Wang J, Froemke RC, Carr KD, Aoki C, Ziff EB. Sucrose ingestion induces rapid AMPA receptor trafficking. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2013;33:6123–6132. doi: 10.1523/JNEUROSCI.4806-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vialou V, Robison AJ, Laplant QC, Covington HE, 3rd, Dietz DM, Ohnishi YN, Mouzon E, Rush AJ, 3rd, Watts EL, Wallace DL, Iniguez SD, Ohnishi YH, Steiner MA, Warren BL, Krishnan V, Bolanos CA, Neve RL, Ghose S, Berton O, Tamminga CA, Nestler EJ. DeltaFosB in brain reward circuits mediates resilience to stress and antidepressant responses. Nat Neurosci. 2010;13:745–752. doi: 10.1038/nn.2551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang J, Goffer Y, Xu D, Tukey DS, Shamir DB, Eberle SE, Zou AH, Blanck TJ, Ziff EB. A single subanesthetic dose of ketamine relieves depression-like behaviors induced by neuropathic pain in rats. Anesthesiology. 2011;115:812–821. doi: 10.1097/ALN.0b013e31822f16ae. [DOI] [PMC free article] [PubMed] [Google Scholar]