1. Introduction1
Substance-using women, including criminal justice-involved women and sex workers (SWs), have historically been neglected by research, prevention and treatment [1, 2]. Recent comprehensive reviews document this deficit among women who use drugs (WWUDs), who are often socially marginalized and neglected from prevention and treatment efforts [1, 3, 4]. Consequently, it is crucial to fill this gap at the interface of treatment and prevention for women with underlying substance use disorders, especially those with or at risk for HIV, and to better understand their social and medical comorbidities. Globally, the pathways to addiction as well as the processes by which WWUDs engage in HIV prevention and treatment differ markedly from their male counterparts [5-24]. Specifically, women differ from men in their motivations for and partnerships in initiating alcohol or drug use [25]. They also have considerably more frequent and intense experiences with interpersonal violence (IPV), sexual abuse and trauma [5, 26, 27]. Disparities in economic opportunities also differ, often with WWUDs engaging in SW, which adds additional stigma beyond substance use alone [28, 29]. Conversely, substance use in SWs may start as a coping mechanism or be deployed as a “power drug” that allows them to service more customers [30, 31]. In the setting of relationship power dynamics, poverty, stigma, and unemployment, WWUDs frequently experience elevated HIV risk by engaging in unprotected sex and/or having a male sexual partner who injects drugs [24, 32-34]. Despite awareness of these gender differences, research on HIV prevalence and risk and access to prevention and treatment among people who use drugs rarely disaggregates men from women [24, 35, 36].
While there are almost no data specifically addressing WWUDs in Southeast Asia, some regional reports focus on SWs and their substance use, unmet addiction treatment needs, psychosocial vulnerabilities, and related health risk behaviors [7, 37]. For example, a 2012 Malaysian study found HIV prevalence to be several-fold higher in SWs (10.7%) compared to the general female population (0.15%) [38], with similar reports in Thailand [39], China [17], and Cambodia [7, 40]. Lower income and engagement in SW increases WWUDs’ risk of experiencing IPV [8, 14, 18, 41-43], which in turn elevates HIV risk through traumatic and risky sexual encounters, extradyadic relationships, and fear and powerlessness to negotiate condom use [8, 41, 42]. Psychiatric disorders are also highly prevalent in WWUDs [5, 15, 44] and exacerbate medical, behavioral, and social complications associated with substance use [9, 15]. These complications also interfere with a woman’s ability to seek supportive addiction treatment and health services [4, 45].
Although 78.5% of cumulative HIV infections in Malaysia in 2013 were among males, the majority of whom were people who inject drugs (PWIDs), the number of cases occurring among females and being attributed to sexual transmission has been increasing since 2000 [46]. Addiction research in Malaysia, however, has remained primarily focused on male opioid injectors, with harm reduction efforts initiated in 2006 to reduce HIV transmission among PWIDs. Consequently, little is known about WWUDs, their medical and social comorbidity, and their engagement in harm reduction and nationally recommended HIV testing and monitoring activities. WWUDs remain under-represented and “hidden” from HIV outreach and prevention programs [46].
In the complex and constrained environment in Malaysia where the HIV epidemic among women is expanding and almost nothing is known about WWUDs [46, 47], we explored HIV risk behaviors, co-morbidities, and barriers to care among 103 WWUDs, including their engagement in nationally recommended HIV testing and monitoring.
2. Methods
2.1 Setting
Kuala Lumpur is home to 1.6 million people, with 7.2 million in the greater metropolitan area [48-50]. Despite harshly imposed criminal penalties, Kuala Lumpur is home to a growing drug trade [50-52]. By 2006 in Malaysia, there were over 300,000 people who use drugs (1.1% of the total population) [53], including an estimated 170,000 PWIDs [46]. With an HIV prevalence of 25-45% in PWIDs [54], harm reduction services with methadone and needle and syringe exchange programs (NSEP) began in 2006 [54, 55]. Methadone is available through formal government-sponsored programs and from primary providers who are paid by the milligram of dose dispensed. Of note, the latter approach is often perceived as treatment even if not continuous. The Malaysian AIDS Council and its partner NGOs with their affiliated community drop-in centers are the primary sources of outreach and support for people with substance use disorders (SUD), including healthcare, education and HIV prevention services such as NSEP.
2.2 Sample and Recruitment
Eligible participants were women aged ≥18 years who self-reported any substance use, including alcohol, in the previous year. Participants were recruited using convenience sampling in three types of facilities identified as key sites for interacting with WWUDs: one community drop-in center (n=55), two women’s shelters (n=27), and two National Anti-Drug Agency (NADA/AADK) voluntary drug treatment centers (n=21). Information sessions and posted fliers describing the study were used for recruitment at each site. After meeting with a trained research assistant to determine eligibility, participants provided written informed consent and were given a description of study risks, benefits, and the voluntary nature of participation. All 103 women who came to learn more about the survey were interviewed during July-August 2011.
2.3 Survey Administration
Administered in Bahasa Malaysia by trained research assistants, a 60-minute questionnaire assessed demographics, criminal justice history, substance use history, addiction treatment needs, HIV risk behaviors, physical health, mental health, social support, history of violence or victimization, and access to medical and social services. Interviews were conducted in private rooms, with no staff members present to ensure privacy and reduce perceived coercion. After completing the interview, participants were paid RM50 (~$16US) for their time.
2.4 Survey Measures and Data Analysis
“Injection drug use” was defined as having ever injected any drug in one’s lifetime. Housing status and injection frequency corresponded to the 30 days prior to the last time the participant used and/or entry into treatment. Primary source of income and frequency of unprotected sex and transactional sex, defined as exchanging sex for money, drugs, a place to stay, food, or clothes, were assessed over the 6-month period prior to the interview date. “Criminal justice involvement” included both jail and prison while “ever incarcerated” included any imprisonment in one’s lifetime. Childhood physical abuse was defined as having been “hit, slapped, punched, or kicked” by an adult before the age of 18 and childhood sexual abuse as having been either raped or sexually assaulted before the age of 18 [56].
Analyses including chi-square testing and bivariate and multiple variable logistic regressions were conducted using SAS version 9.3 (SAS Institute Inc., Cary, NC). Frequencies of overall and unmet need for health and social services were calculated from responses about services needed and utilized in the past 6 months. Poverty was defined using 2010 national estimates as earning ≤800 Malaysian Ringgit (RM) monthly [57, 58]. Housing status was categorized as: living in one’s own home (“stably housed”), living with a friend or family member or in short-term housing (“unstably housed”), and living at a community shelter, outreach center, on the streets, or prison, jail, or a compulsory drug detention center (“homeless”). Frequency of engagement in transactional sex was categorized as follows: women reporting SW as their primary income source were considered to engage “regularly” in transactional sex (i.e., for money), women not reporting SW as their primary income source but still reporting exchanging sex for something at least once during the last 6 months were considered to “intermittently” engage in transactional sex, and women who did not report any transactional sex in the last 6 months were placed in the “No Transactional Sex” category. Because methadone remains an infrequently utilized treatment in outpatient settings, in the regression model women were only considered to be in formal treatment for addiction if they had been living at a residential, governmental treatment facility during the last 30 days. HIV and Hepatitis C status were self-reported. Depression was measured using the 20-item Center for Epidemiologic Studies Depression (CES-D) scale [59]; standard cut-offs of >20 classified moderate to severe symptoms [59, 60]. Social support was measured using the Medical Outcomes Study scale [61], from which selected questions were used to create a binary variable for social isolation; participants were considered socially isolated if they never or almost never had someone to take them to the doctor if they were ill or someone to turn to for suggestions about how to deal with a personal problem and with whom they could discuss their most private worries and fears.
Three women refused to answer HIV-related questions and were excluded from HIV-specific analyses. The Malaysian Ministry of Health (MOH) and the World Health Organization (WHO) recommend HIV testing annually for anyone using drugs and CD4 monitoring at least twice annually for people living with HIV. Poor adherence to these HIV testing and monitoring guidelines was the primary outcome of interest. Bivariate and multiple variable logistic regression models were fitted using both backward elimination and forward selection of main effect variables as well as all possible interaction terms with a α=0.05 threshold for inclusion in the final multivariable model. Findings were robust to both analytical models and a model selected based on minimization of the AIC. Main effect variables did not exhibit multicollinearity.
2.5 Human Subjects approval
The Institutional Review Boards (IRBs) at Yale University and the University of Malaya approved the study. All women were assigned a unique code to maintain anonymity and no names were recorded.
3. Results
3.1 Sample Demographics
Table 1 provides the characteristics of the women, who primarily identified as ethnically Malay (61.2%) and Muslim (66%). They had low education levels (39.9% had not attended high school) and the majority (69.9%) was single and unstably housed (62.1%), living below the national poverty line. Nearly all (93.2%) had criminal justice involvement, with 70.9% having previously been to prison, often for extensive periods of time. Almost 20% engaged in SW as their primary source of income.
Table 1.
Participants’ Demographic Characteristics, HIV Risk Behaviors, and Related Co-morbidities (N=103)
| Variable | N (%) |
|---|---|
| Mean age (±SD) | 39.4 ±10.7 |
|
| |
| Monthly income, median (range) | RM 800 (0 – 30,000) |
|
| |
| Above national poverty level | 45 (43.7) |
|
| |
| At or below national poverty level | 58 (56.3) |
|
| |
| Ethnicity | |
|
| |
| Malay | 63 (61.2) |
|
| |
| Indian | 17 (16.5) |
|
| |
| Chinese | 15 (14.6) |
|
| |
| Other | 8 (7.8) |
|
| |
| Religion | |
|
| |
| Muslim | 68 (66.0) |
|
| |
| Buddhist | 11 (10.7) |
|
| |
| Hindu | 11 (10.7) |
|
| |
| Christian | 7 (6.8) |
|
| |
| Other | 4 (3.9) |
|
| |
| None | 2 (1.9) |
|
| |
| Housing Status | |
|
| |
| Stably Housed | 39 (37.9) |
|
| |
| Unstably Housed | 32 (31.1) |
|
| |
| Homeless | 32 (31.1) |
|
| |
| Education | |
|
| |
| None / Kindergarten | 12 (11.7) |
|
| |
| Elementary / Middle (Primary) | 29 (28.2) |
|
| |
| Early High School (Secondary- Form 3) | 29 (28.2) |
|
| |
| Late High School (Secondary- Form 5) | 27 (26.2) |
|
| |
| Pre-University (Form 6) / University | 6 (5.8) |
|
| |
| Relationship Status | |
|
| |
| Single | 72 (69.9) |
|
| |
| Partnered / married | 31 (30.1) |
|
| |
| Primary Income Sourcea | |
|
| |
| Full-time, traditional | 32 (31.4) |
|
| |
| Part-time, traditional | 23 (22.5) |
|
| |
| Sex work | 20 (19.6) |
|
| |
| Financial assistance | 4 (3.9) |
|
| |
| Friend | 3 (2.9) |
|
| |
| Other | 20 (19.6) |
|
| |
| Criminal Justice Involvement | 96 (93.2) |
|
| |
| Ever incarcerated | 73 (70.9) |
|
| |
| Length of incarceration, median (range) | 46 months (2 months – 33 years) |
|
| |
| Injection drug use | |
|
| |
| Lifetime | 33 (32.0) |
|
| |
| Last 30 days | 22/33 (66.7) |
|
| |
| Shared injection equipment | 15/22 (68.2) |
|
| |
| Been injected by another person | 21/22 (95.5) |
|
| |
| Condom use a – last 6 months | |
|
| |
| Unprotected sex | 36 (35.3) |
|
| |
| Protected sex | 49 (48.0) |
|
| |
| No sex | 17 (16.7) |
|
| |
| Violence & victimization | |
|
| |
| Childhood sexual trauma b | 31 (30.7) |
|
| |
| Childhood physical abuse | 51 (49.5) |
|
| |
| Adulthood sexual trauma b | 24 (23.8) |
|
| |
| Adulthood physical abuse c | 62 (62.0) |
|
| |
| Intimate partner violence | 47/62 (75.8) |
|
| |
| Any transactional sex – last 6 months | 46 (44.7) |
|
| |
| Regular | 20 (19.4) |
|
| |
| Intermittent | 26 (25.2) |
|
| |
| None | 57 (55.3) |
|
| |
|
Elements of Social Isolation
Never or almost never is there someone… |
|
|
| |
| To give her love and affection | 30 (29.1) |
|
| |
| To help if she was confined to bed | 33 (32.0) |
|
| |
| To take her to the doctor | 33 (32.0) |
|
| |
| To hug her | 40 (38.8) |
|
| |
| To turn to for suggestions about how to deal with a personal problem a |
40 (39.2) |
|
| |
| With whom she can share her most private worries and fears a |
44 (43.1) |
|
| |
| Health Co-Morbidities | |
|
| |
| Severe depression | 50 (48.5) |
|
| |
| HIV c | 20 (20.0) |
|
| |
| Viral hepatitis (C and/or B) b | 13 (12.9) |
|
| |
| Tuberculosis (active) b | 3 (3.0) |
n=102
n=101
n=100
3.2 Substance Use, Sexual Risk Behaviors, and Social Isolation
Amphetamine-type substances (ATS) were the most commonly (45.6%) used drugs, followed by heroin (41.7%). Half of the sample (53.4%) reported lifetime poly-substance use and one-third (30.1%) did so in the previous 30 days. One-third of women had previously injected drugs, the majority of which had injected recently and shared injection equipment; all but one recent injector reported being injected by another person (Table 1). Sexual risk behaviors were prevalent with almost one half (n=46; 44.7%) of women having recently engaged in transactional sex for money (n=42; 40.8%), drugs (n=12, 11.7%), a place to stay (n=11, 10.7%), food (n=7; 6.8%), or clothing (n=5, 4.9%).
Among the 12 women who exchanged sex for drugs, all but one had used ATS in the last 30 days (p=0.03; Fisher’s exact test). In addition, 42.4% (36/85) of women sexually active within the last 6 months reported unprotected sex and, of the 35 women who had unprotected sex in the last 30 days, almost one-third (10/35) had done so with multiple different partners. Physical violence (49.5-62%) and sexual victimization (23.8-30.7%) were highly prevalent in both childhood and adulthood; 75.8% of physical abuse was intimate partner violence. In addition, 25.2% had no close friends or relatives to talk to and 24.3% felt they could “count on” only one person (data not shown); nearly 40% did not have anyone who made them feel loved and 32-43.1% never or almost never had someone to help them in times of need such as illness or personal crisis (Table 1).
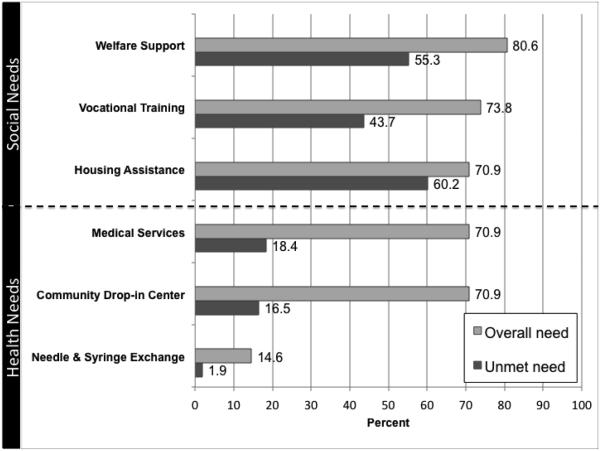
3.3 Unmet Social and Medical Needs
More than 70% of the sample reported a need for social and medical services; the greatest unmet need was for financial and housing assistance (Figure 1). One-fourth of women who reported a need for medical services and/or a community drop-in center were unable to access these services. Despite the appearance that need for medical services is better met than other services, 70.9% of all women additionally reported an unmet need for reproductive healthcare; only 47.6% of the sample had received a pelvic exam or PAP smear within the last three years. The majority of women (62.1%) felt their SUD was a barrier to receiving reproductive healthcare. Thirteen of 15 women needing NSEP services were able to successfully access these services. Of the 74 women who had ever used heroin and the 21 who had used other opioids, 47 (63.5%) and 15 (71.4%), respectively, had ever received methadone treatment.
Figure 1.
Percentage of participants reporting a need for social support and health services in past six months
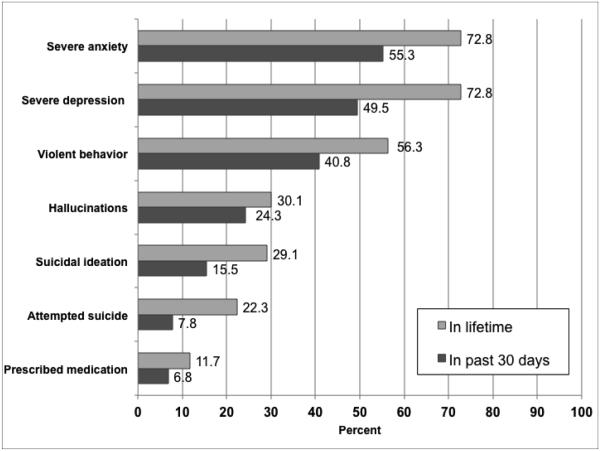
3.4 Psychiatric Comorbidity
Psychiatric illness symptoms were prevalent with 60.2% meeting criteria for moderate (11.7%) or severe (48.5%) depression (Table 1). Of severely depressed women, 35 (70%) used heroin (p=0.02) and 34 (68%) used ATS (p=0.23) in the last 30 days. As shown in Figure 2, depression and anxiety were the most common psychiatric issues reported. Almost one-third reported suicidal ideation in their lifetime and half of these women seriously considered suicide within the last 30 days. Almost a quarter of women (23/103) had previously attempted suicide, of which 8 had done so within the past month. Only 11.7% and 18.4% of all women had ever been prescribed psychiatric medications or received treatment or counseling for psychological or emotional problems, respectively.
Figure 2.
Percentage of participants reporting mental health issues
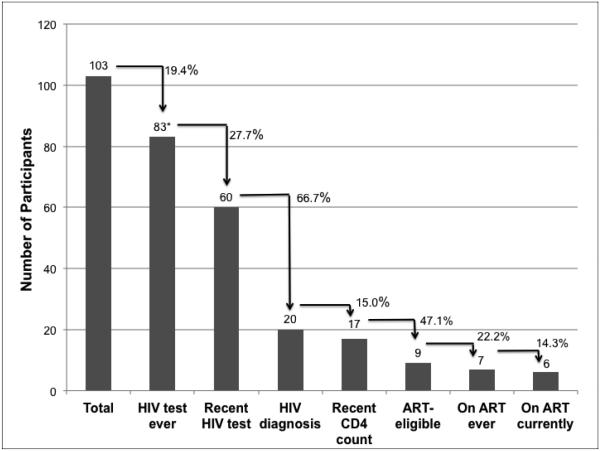
3.5 HIV Continuum of Care
As illustrated in Figure 3, 19.4% had never been tested for HIV and 27.7% of reported test results were more than one year old, thus failing to meet MOH national recommendations for annual testing for people who use drugs. While three women refused to provide details about their HIV statuses, 25% (20/80) of the remaining sample reported that their most recent HIV test was positive. Of those identifying as HIV-infected, 15% did not have a recent CD4 count (within the last 6 months). Nine (52.9%) of 17 women were eligible (CD4<350 cells/mL) for ART per WHO guidelines; two never initiated ART and one defaulted. With regard to other medical co-morbidities (Table 1), 8.9% and 4% reported having Hepatitis C and B, respectively, and 3% had had active tuberculosis. Self-reported rates of diagnosed STIs (gonorrhea, chlamydia, and syphilis) were 2.9%, although 32% reported at least one STI symptom such as painful urination, genital swelling, genital pain or sores, or abnormal vaginal discharge within the last year.
Figure 3.
HIV Continuum of Care
Legend: ART: antiretroviral therapy; * Three participants refused to answer additional HIV-related questions.
After controlling for all covariates (Table 2), drug injection (AOR 0.28, p=0.01) and experiencing adulthood IPV (AOR 2.73, p=0.04) were independently associated with not adhering to HIV testing and monitoring guidelines.
Table 2.
Bivariate and Multivariate Associations with Lack of Adherence to National HIV Testing and Monitoring Guidelines (N=100)
| Characteristic | N a | % (n/N) not in adherence |
Unadjusted OR (95% CI) |
Adjusted OR b
(95% CI) |
|---|---|---|---|---|
|
In residential treatment for
substance use |
||||
| Yes | 81 | 32.1 (26/81) | 0.34 (0.12-0.96) | -- |
| No | 19 | 57.9 (11/19) | referent | |
|
| ||||
| Homeless or unstably housed | ||||
| Yes | 63 | 28.6 (18/63) | 0.38 (0.16-0.88) | -- |
| No | 37 | 51.4 (19/37) | referent | |
|
| ||||
| Relationship status | ||||
| Relationship | 29 | 41.4 (12/29) | 1.30 (0.54-3.15) | -- |
| Single | 71 | 35.2 (25/71) | referent | |
|
| ||||
| Ever injected drugs | ||||
| Yes | 33 | 21.2 (7/33) | 0.33 (0.13-0.87) | 0.28 (0.10-0.77) |
| No | 67 | 44.8 (30/67) | referent | referent |
|
| ||||
| Heroin as favorite drug | ||||
| Yes | 43 | 25.6 (11/43) | 0.41 (0.17-0.97) | -- |
| No | 57 | 45.6 (26/57) | referent | |
|
| ||||
| ATS as favorite drug | ||||
| Yes | 46 | 43.5 (20/46) | 1.67 (0.74-3.80) | -- |
| No | 54 | 31.5 (17/54) | referent | |
|
| ||||
| Transactional Sex | ||||
| Yes | 44 | 38.6 (17/44) | 1.13 (0.50-2.57) | -- |
| No | 56 | 35.7 (20/56) | referent | |
|
| ||||
| Interpersonal violence | ||||
| Yes | 63 | 41.3 (26/63) | 2.03 (0.82-5.04) | 2.73 (1.04-7.14) |
| No | 35 | 25.7 (9/35) | referent | referent |
|
| ||||
| Social Isolation | ||||
| Yes | 55 | 36.4 (20/55) | 0.94 (0.42-2.13) | -- |
| No | 45 | 37.8 (17/45) | referent | |
|
| ||||
| Severe Depression | ||||
| Yes | 48 | 33.3 (16/48) | 0.74 (0.33-1.67) | -- |
| No | 52 | 40.4 (21/52) | referent | |
Numbers may not sum to total due to missing data.
For the fully adjusted model, N=98 with Pearson Goodness of Fit Test p=0.702.
4. Discussion
Despite the vast body of literature on men who use drugs in Malaysia [62-64], to our knowledge this is the first study to focus exclusively on the hidden population of WWUDs who “appear” absent and marginalized from HIV prevention and treatment strategies. The women in this study demonstrate considerable medical and psychiatric comorbidity exacerbated by profound poverty, unstable living situations, and social isolation. These factors likely converge, leading to engagement in SW as a survival mechanism and resultant high rates of IPV [43]. While active substance use complicates diagnosis of mental illness, psychiatric symptoms are high, potentially as a consequence of post-traumatic stress disorder from IPV, may result in engagement in high-risk behaviors but low rates of entry into medical care [43, 65]. Due to substance use and sexual risk behaviors, these women are at significant risk for contracting or transmitting HIV but the majority are unable to access appropriate medical and social support services due in part to their ongoing substance use and social destabilization from recurrent incarceration [43, 45, 66, 67].
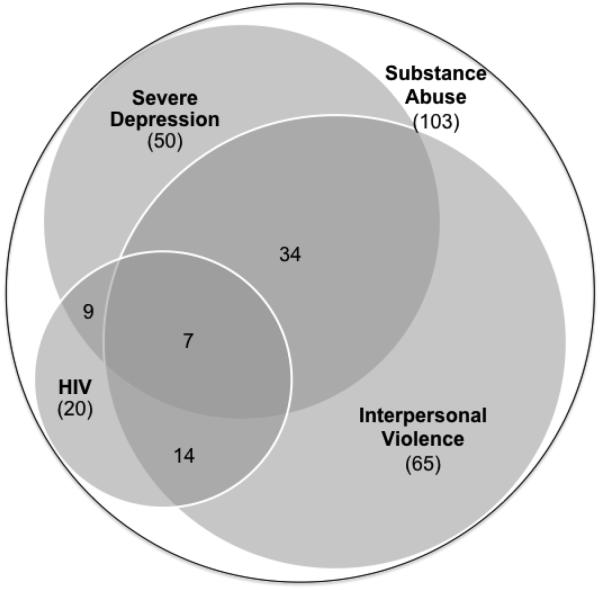
Syndemics such as the Substance Abuse, Violence, and HIV/AIDS (SAVA) syndemic have been successfully used to describe mutually reinforcing interactions between two or more health conditions (e.g., substance use, HIV/AIDS or HIV-related risk, or psychiatric illness) that negatively affect the burden of disease when combined with adverse social conditions (e.g., homelessness or IPV) [65]. These concomitant dynamics magnify each other (Figure 4) and may in part explain why WWUDs are disenfranchised from systems of HIV prevention and treatment [10, 16, 25, 68, 69]. Our sample of challenging-to-recruit WWUDs in urban Malaysia exemplifies the ways in which key issues at the individual, relationship, community, healthcare setting, and policy levels, when left unsupported and unaddressed, conspire against HIV prevention and treatment efforts particularly in women [70-74].
Figure 4.
The Syndemic of HIV/AIDS, Interpersonal Violence and Major Depression among 103 Substance-Using Women
Unlike the pattern reported among their male counterparts who primarily injected opioids [75-78], only one-third of women had injected drugs, mostly with ATS or opioids. Most women who had recently injected, however, were at increased risk of blood-borne diseases like HIV and viral hepatitis due to their injecting behaviors (e.g. being injected by someone else) [24, 45, 67].
Poverty facilitates a risk environment in which women face unequal access to healthcare, marginalized treatment by healthcare providers, gender inequalities, competing life priorities, denial of health problems, and the inability to leverage social capital and economic resources to provide for their families [66, 79]. Likely as a consequence of poverty, social isolation, and a lack of resources and social services, many women had engaged in SW, either just to survive or to maintain their level of drug use. This work involved sex with multiple partners often without using condoms, further stigmatizing these women and placing them at even greater health risk.
Multiple co-morbid conditions including HIV, viral hepatitis, STI symptoms, and high rates of depression and anxiety affected the women surveyed. Over 60% of women met screening criteria for major depression, likely related to a multitude of factors including childhood trauma and abuse, adulthood IPV, or SUDs. The circular influence of mental illness and substance use, with one affecting the other, can result in an interaction that complicates and worsens health conditions [80, 81].
Consistent with the SAVA syndemic, 30.7% of our sample reported sexual trauma and half reported childhood physical abuse. There is a known bidirectional relationship between violence and substance use; women who have experienced childhood trauma have higher rates of substance use and those who use substances tend to more frequently be involved in abusive relationships [42]. As high rates of sexual and physical abuse and IPV were also reported in adulthood, this trauma history may have affected the women’s behaviors and relationships as adults.
HIV is concentrated in incarcerated populations, with the majority of prisoners having SUDs, thereby increasing their HIV risk [82]. Most (70.9%) of the women surveyed had been incarcerated, primarily due to drugs or drug-related arrests (91.7%). Criminal justice involvement disrupts social networks [83] and alters the women’s stability [84], housing conditions, and ability to attain medical and social services, creating increased likelihood of marginalization upon their release and further exacerbating stigma and poor health outcomes.
While most (80.6%) women surveyed had been tested for HIV at some point in time, likely as a result of mandatory HIV screening policies in prisons, nearly one-third of test results were outdated, perhaps due to high-risk women not accessing voluntary testing in community settings. Nonetheless, self-reported HIV prevalence was 20%. One-third of ART-eligible women were not receiving treatment and 15% of women potentially eligible for ART had not been recently assessed by laboratory CD4 count. Adherence to recommended HIV screening and laboratory monitoring in this high-risk population are crucial steps in the HIV continuum and will likely require the development of gender-specific services to more effectively engage WWUDs in HIV prevention and treatment to prevent HIV infection and transmission.
HIV testing and monitoring is central to HIV treatment as prevention strategies [85, 86]. Important in these findings are factors that may facilitate and impede treatment as prevention efforts. One reason that being a PWID appears to facilitate HIV testing is the continued focus on targeted HIV testing despite evidence of a more generalizing HIV epidemic in Malaysia [47]. These findings emphasize the need to expand targeted HIV screening and treatment efforts beyond PWIDs to include women who use but do not inject drugs and those who experience IPV, since IPV can be a consequence of unequal relationship power dynamics, violence or fear of violence upon discussing HIV risk and prevention methods with sexual partners, and even victimization by police [8, 21, 45, 87].
In socially and religiously conservative societies like Malaysia, women are increasingly marginalized, thereby increasing their vulnerability and experiences with discrimination against them in the setting of substance use [25, 69]. WWUDs demonstrate high levels of unmet need for addiction treatment programs and related health and social services but in many cases are less likely than men to access these services [10, 16, 68]. Some studies suggest this is due to their desire to uphold their role as family caretaker and unwillingness to leave their children in order to seek help for themselves [16, 18]. Their own families may also restrict their access to addiction treatment services out of shame or denial of their addiction or an attempt to protect them from being identified as having a SUD [18].
WWUDs in this study reported relatively little unmet need for medical and community outreach services including NSEP. One explanation is that only one-third of WWUDs had injected drugs; the remaining women, especially ATS users, may not have perceived a need for NSEP services. For these women, access to NSEP may not be a reliable measurement of access to addiction treatment and support services. In addition, most women who had used opioids also reported receiving methadone in their lifetime, indicating their unmet addiction treatment needs may not be as great as their unmet need for social support services. Moreover, they themselves reported poor access to social services, including financial assistance, housing assistance and vocational training. This services gap places women at a social and economic disadvantage, thus impacting their drug use and sexual risk taking behaviors and overall health status. In Malaysia in particular, social expectations for women and stigma toward WWUDs may compound the challenges they face when seeking addiction treatment and other forms of care [88-90].
4.1 Limitations
In this exploratory pilot study, small sample size and convenience sampling limited the power to detect differences in potential covariates. Moreover, we cannot generalize these findings to all drug-using women in Malaysia; nonetheless, this is the largest sample of WWUDs assessed in Malaysia to date, which speaks to Malaysia’s marginalized epidemic of drug use, HIV risk and social disenfranchisement among women and provides a glimpse into the problems faced by WWUDs. Finally, while HIV status was not confirmed by laboratory-based testing, we believe the high self-reported prevalence likely represents the minimum prevalence since most women were not recently tested, yet engaged in high-risk behaviors. Notwithstanding these limitations, this study’s exploratory nature allowed the detection of key issues for WWUDs, laying the groundwork for future studies.
4.2 Conclusions
Our findings demonstrate a syndemic of substance abuse, IPV, HIV/AIDS, mental illness, and social instability. In our study, most WWUDs were not regular injectors but remained at risk for HIV due to high-risk sexual behaviors and injecting practices. Inconsistent medical care and insufficient mental health and addiction treatment created further vulnerability to poor health outcomes. Of particular concern are the observed suboptimal HIV screening and monitoring rates amongst the women in our sample, despite their connection to outreach and addiction treatment services. In the context of Malaysia’s PWID-targeted HIV interventions, non-injecting WWUDs and those who experience IPV may be at greatest risk for poor HIV treatment outcomes. Interventions to improve addiction treatment strategies and reduce HIV transmission should be sensitive to these unique patterns of drug use, risk behaviors, and social vulnerability among WWUDs [4, 45]. Future research on women and transgender people with SUDs is needed in Malaysia to better inform HIV and reproductive health policies. Mental health and social support are potentially key targets for future interventions directed at WWUDs in Malaysia.
Highlights.
Women who use drugs are a hidden group of people with or at risk for HIV infection.
In Malaysia, these women are inadequately engaged in the HIV continuum of care.
Prevalence of HIV, psychiatric comorbidity and exposure to violence (IPV) is high.
Non-injection drug use and IPV undermine HIV prevention and treatment strategies.
Gender-specific interventions are needed for the growing HIV epidemic among women.
Acknowledgements
The authors thank Elisabeth Powelson and Jeannia Fu for their assistance with preliminary study design, Tunku Noor Hayati Tunku Abdul for her time and effort dedicated to study coordination and data collection, and Paula Dellamura for her assistance throughout the entire process. They also acknowledge research assistants Tengku Nur Qistina, Nik Fikri, Noriana Nazuir, Aneeza Sharifah, Nurul Huda, and Nora Hashim for their critical efforts with data collection and entry. Key staff members at the Malaysian AIDS Council were invaluable for their insight and guidance. Lastly, the study participants are sincerely thanked for their time and willingness to share their stories.
Author Disclosures
Role of Funding Sources: Funding for this study was provided by the National Institutes on Drug Abuse for Research (R01 DA025943), Career Development Awards for FLA (K24 DA017072), JAW (K01 DA038529, and the National Institutes of Health Medical Scientist Training Program at Yale University (TG T32GM07205). The NIH had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
- PWIDs
- People who inject drugs
- WWUDs
- Women who use drugs
- SUD
- Substance Use Disorder
- NGO
- Non-governmental organization
- WHO
- World Health Organization
- MOH
- Ministry of Health
- NSEP
- Needle Syringe Exchange Program
- ATS
- Amphetamine-type stimulants
- SW(s)
- Sex work(ers)
- IPV
- Interpersonal violence
- SAVA Syndemic
- Syndemic of Substance Abuse, Violence, and HIV/AIDS
Contributors: K.B. Loeliger and V. Pillai designed the study and collected the data. K.B. Loeliger and R. Marcus analyzed the data and wrote the first draft of the manuscript. J.A. Wickersham conducted a literature review and helped to analyze the data. F.L. Altice and A. Kamarulzaman guided the study design, data analysis, and writing of the manuscript. All authors contributed to and have approved the final manuscript.
Conflict of Interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.El-Bassel N, Strathdee SA. Bringing Female Substance Users to the Center of the Global HIV Response. J Acquir Immune Defic Syndr. 2015;69(Suppl 1):S94–5. doi: 10.1097/QAI.0000000000000625. [DOI] [PubMed] [Google Scholar]
- 2.Springer SA, et al. Drug Treatment as HIV Prevention Among Women and Girls Who Inject Drugs From a Global Perspective: Progress, Gaps, and Future Directions. J Acquir Immune Defic Syndr. 2015;69:S155–S161. doi: 10.1097/QAI.0000000000000637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Springer SA, et al. Drug Treatment as HIV Prevention Among Women and Girls Who Inject Drugs From a Global Perspective: Progress, Gaps, and Future Directions. J Acquir Immune Defic Syndr. 2015;69(Suppl 1):S155–61. doi: 10.1097/QAI.0000000000000637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malinowska-Sempruch K. What interventions are needed for women and girls who use drugs? A global perspective. J Acquir Immune Defic Syndr. 2015;69(Suppl 1):S96–7. doi: 10.1097/QAI.0000000000000621. [DOI] [PubMed] [Google Scholar]
- 5.Brecht ML, et al. Methamphetamine use behaviors and gender differences. Addict Behav. 2004;29(1):89–106. doi: 10.1016/s0306-4603(03)00082-0. [DOI] [PubMed] [Google Scholar]
- 6.Cheng WS, et al. Differences in sexual risk behaviors among male and female HIV-seronegative heterosexual methamphetamine users. Am J Drug Alcohol Abuse. 2009;35(5):295–300. doi: 10.1080/00952990902968585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Couture MC, et al. Correlates of amphetamine-type stimulant use and associations with HIV-related risks among young women engaged in sex work in Phnom Penh, Cambodia. Drug Alcohol Depend. 2012;120(1-3):119–26. doi: 10.1016/j.drugalcdep.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El-Bassel N, et al. Intimate partner violence and HIV among drug-involved women: contexts linking these two epidemics--challenges and implications for prevention and treatment. Subst Use Misuse. 2011;46(2-3):295–306. doi: 10.3109/10826084.2011.523296. [DOI] [PubMed] [Google Scholar]
- 9.Greenfield SF, et al. Substance abuse in women. Psychiatr Clin North Am. 2010;33(2):339–55. doi: 10.1016/j.psc.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hansen H, et al. Drug treatment, health, and social service utilization by substance abusing women from a community-based sample. Med Care. 2004;42(11):1117–24. doi: 10.1097/00005650-200411000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Lorvick J, et al. Sexual and injection risk among women who inject methamphetamine in San Francisco. J Urban Health. 2006;83(3):497–505. doi: 10.1007/s11524-006-9039-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McCoy CB, et al. Drug use and barriers to use of health care services. Subst Use Misuse. 2001;36(6-7):789–806. doi: 10.1081/ja-100104091. [DOI] [PubMed] [Google Scholar]
- 13.Nguyen AT, et al. Intravenous drug use among street-based sex workers: a high-risk behavior for HIV transmission. Sex Transm Dis. 2004;31(1):15–9. doi: 10.1097/01.OLQ.0000105002.34902.B5. [DOI] [PubMed] [Google Scholar]
- 14.Shannon K, et al. Social and structural violence and power relations in mitigating HIV risk of drug-using women in survival sex work. Soc Sci Med. 2008;66(4):911–21. doi: 10.1016/j.socscimed.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 15.Sordo L, et al. Depression among regular heroin users: the influence of gender. Addict Behav. 2012;37(1):148–52. doi: 10.1016/j.addbeh.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 16.Tucker JS, et al. Predictors of substance abuse treatment need and receipt among homeless women. J Subst Abuse Treat. 2011;40(3):287–94. doi: 10.1016/j.jsat.2010.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang H, et al. Prevalence and predictors of HIV infection among female sex workers in Kaiyuan City, Yunnan Province, China. Int J Infect Dis. 2009;13(2):162–9. doi: 10.1016/j.ijid.2008.05.1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wechsberg WM, Luseno W, Ellerson RM. Reaching women substance abusers in diverse settings: stigma and access to treatment 30 years later. Subst Use Misuse. 2008;43(8-9):1277–9. doi: 10.1080/10826080802215171. [DOI] [PubMed] [Google Scholar]
- 19.Wenzel SL, et al. The social context of homeless women's alcohol and drug use. Drug Alcohol Depend. 2009;105(1-2):16–23. doi: 10.1016/j.drugalcdep.2009.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wickersham J, et al. Drug use and injection risk behaviors among female drug users in Malaysia: Results from a pilot study; 2013, 7th IAS Conference on HIV Pathogenesis, Treatment and Prevention: Kuala Lumpur, Malaysia. [Google Scholar]
- 21.Aziz M, Smith KY. Treating women with HIV: is it different than treating men? Curr HIV/AIDS Rep. 2012;9(2):171–8. doi: 10.1007/s11904-012-0116-x. [DOI] [PubMed] [Google Scholar]
- 22.Malaysian AIDS Council . Understanding Women Who Use Drugs In Malaysia. Kuala Lumpur, Malaysia: 2014. [Google Scholar]
- 23.Powelson E, et al. Unmet healthcare need among women who use methamphetamine in San Francisco. Subst Use Misuse. 2014;49(3):243–52. doi: 10.3109/10826084.2013.825919. [DOI] [PubMed] [Google Scholar]
- 24.Roberts AM, Degenhardt L. Women who inject drugs: a review of their risks, experiences and needs. National Drug and Alcohol Research Centre; Sydney: 2010. p. 132. BM. [Google Scholar]
- 25.Brady KT, Randall CL. Gender differences in substance use disorders. Psychiatr Clin North Am. 1999;22(2):241–52. doi: 10.1016/s0193-953x(05)70074-5. [DOI] [PubMed] [Google Scholar]
- 26.Meyer JP, et al. Partner violence and health among HIV-infected jail detainees. International J Prisoner Health. 2013;9(3):124–41. doi: 10.1108/IJPH-03-2013-0011. PMCID: PMC3873166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meyer JP, Springer SA, Altice FL. Substance abuse, violence, and HIV in women: a literature review of the syndemic. J Womens Health. 2011;20(7):991–1006. doi: 10.1089/jwh.2010.2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saggurti N, et al. Motivations for entry into sex work and HIV risk among mobile female sex workers in India. J Biosoc Sci. 2011;43(5):535–54. doi: 10.1017/S0021932011000277. [DOI] [PubMed] [Google Scholar]
- 29.Fielding-Miller R, et al. "There is hunger in my community": a qualitative study of food security as a cyclical force in sex work in Swaziland. BMC Public Health. 2014;14:79. doi: 10.1186/1471-2458-14-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maher L, et al. Amphetamine-type stimulant use and HIV/STI risk behaviour among young female sex workers in Phnom Penh, Cambodia. Int J Drug Policy. 2011;22(3):203–9. doi: 10.1016/j.drugpo.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Strathdee SA, et al. Characteristics of female sex workers with US clients in two Mexico-US border cities. Sex Transm Dis. 2008;35(3):263–8. doi: 10.1097/OLQ.0b013e31815b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.El-Bassel N, et al. People who inject drugs in intimate relationships: it takes two to combat HIV. Curr HIV/AIDS Rep. 2014;11(1):45–51. doi: 10.1007/s11904-013-0192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Strathdee SA, Sherman SG. The role of sexual transmission of HIV infection among injection and non-injection drug users. J Urban Health. 2003;80(4 Suppl 3):iii7–14. doi: 10.1093/jurban/jtg078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ravi A, Blankenship KM, Altice FL. The association between history of violence and HIV risk: a cross-sectional study of HIV-negative incarcerated women in Connecticut. Womens Health Issues. 2007;17(4):210–6. doi: 10.1016/j.whi.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 35.Des Jarlais DC, et al. Gender disparities in HIV infection among persons who inject drugs in Central Asia: a systematic review and meta- analysis. Drug Alcohol Depend. 2013;132(Suppl 1):S7–12. doi: 10.1016/j.drugalcdep.2013.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Des Jarlais DC, et al. Are females who inject drugs at higher risk for HIV infection than males who inject drugs: an international systematic review of high seroprevalence areas. Drug Alcohol Depend. 2012;124(1-2):95–107. doi: 10.1016/j.drugalcdep.2011.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tran TN, et al. Drug use among female sex workers in Hanoi, Vietnam. Addiction. 2005;100(5):619–25. doi: 10.1111/j.1360-0443.2005.01055.x. [DOI] [PubMed] [Google Scholar]
- 38.Baral S, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(7):538–49. doi: 10.1016/S1473-3099(12)70066-X. [DOI] [PubMed] [Google Scholar]
- 39.Manopaiboon C, et al. Unexpectedly high HIV prevalence among female sex workers in Bangkok, Thailand in a respondent-driven sampling survey. Int J STD AIDS. 2013;24(1):34–8. doi: 10.1177/0956462412472300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Couture MC, et al. Young women engaged in sex work in Phnom Penh, Cambodia, have high incidence of HIV and sexually transmitted infections, and amphetamine-type stimulant use: new challenges to HIV prevention and risk. Sex Transm Dis. 2011;38(1):33–9. doi: 10.1097/OLQ.0b013e3182000e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.El-Bassel N, et al. Correlates of partner violence among female street-based sex workers: substance abuse, history of childhood abuse, and HIV risks. AIDS Patient Care STDS. 2001;15(1):41–51. doi: 10.1089/108729101460092. [DOI] [PubMed] [Google Scholar]
- 42.Meyer JP, Springer SA, Altice FL. Substance abuse, violence, and HIV in women: a literature review of the syndemic. J Womens Health (Larchmt) 2011;20(7):991–1006. doi: 10.1089/jwh.2010.2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Singer M, editor. Introduction to Syndemics: A Critical Systems Approach to Public and Community Health. 1st Wiley; 2009. [Google Scholar]
- 44.Vik PW. Methamphetamine use by incarcerated women: comorbid mood and anxiety problems. Womens Health Issues. 2007;17(4):256–63. doi: 10.1016/j.whi.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 45.Pinkham S, Malinowska-Sempruch K. Women, harm reduction and HIV. Reprod Health Matters. 2008;16(31):168–81. doi: 10.1016/S0968-8080(08)31345-7. [DOI] [PubMed] [Google Scholar]
- 46.United Nations Programme on HIV/AIDS (UNAIDS) Country Progress Report. HIV/STI Section of Ministry of Health, Malaysia; Geneva: 2014. The Global AIDS Response Progress Report, 2014: Malaysia. [Google Scholar]
- 47.Joint United Nations Programme on HIV/AIDS (UNAIDS) The Gap Report. Geneva, Switzerland: 2014. [Google Scholar]
- 48.Malaysia Department of Statistics 2010 Population and Housing Census of Malaysia. 2014 [cited 2014 1 July]; Available from: http://www.statistics.gov.my/portal/index.php?option=com_content&id=1215&Itemid=89&lang=en.
- 49.World Capital Institute 2013 Kuala Lumpur, Malaysia. 2013 [cited 2014 1 July]; Available from: http://www.worldcapitalinstitute.org/makciplatform/2013-kuala-lumpur-malaysia.
- 50.World Population Review Kuala Lumpur Population 2014. 2014 [cited 2014 1 July]; Available from: http://worldpopulationreview.com/world-cities/kuala-lumpur-population/
- 51.Tanguay P. IDPC Briefing Paper: Policy responses to drug issues in Malaysia. International Drug Policy Consortium; London, U.K.: 2011. [Google Scholar]
- 52.U.N. Department of State . Malaysia 2013 Crime and Safety Report. Overseas Security Advisory Council-Bureau of Diplomatic Security; Washington, D.C.: 2013. [Google Scholar]
- 53.Nazar M, Ahlam Z. Current trends of drug abuse in Malaysia: its implications for the HIV problems; Paper Presented at the WHO Workshop on Drug Abuse and HIV AIDS.2007. [Google Scholar]
- 54.Kamarulzaman A. Impact of HIV prevention programs on drug users in Malaysia. J Acquir Immune Defic Syndr. 2009;52(Suppl 1):S17–9. doi: 10.1097/QAI.0b013e3181bbc9af. [DOI] [PubMed] [Google Scholar]
- 55.Reid G, Kamarulzaman A, Sran SK. Malaysia and harm reduction: the challenges and responses. Int J Drug Policy. 2007;18(2):136–40. doi: 10.1016/j.drugpo.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 56.CDC . Behavioral Risk Factor Surveillance System Questionnaire (BRFSS) Center for Disease Control; 2006. Editor. [Google Scholar]
- 57.Hatta ZA, Ali I. Poverty Reduction Policies in Malaysia: Trends, Strategies and Challenges. Asian Culture and History. 2013;5(2) [Google Scholar]
- 58.Mat Zin R. Measuring and monitoring poverty and inequality: The Malaysian experience. Institute of Southeast Asian Studies; Singapore: 2011. [Google Scholar]
- 59.Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied psychological measurement. 1977;1(3):385–401. [Google Scholar]
- 60.Chwastiak L, et al. Depressive symptoms and severity of illness in multiple sclerosis: epidemiologic study of a large community sample. Am J Psychiatry. 2002;159(11):1862–8. doi: 10.1176/appi.ajp.159.11.1862. [DOI] [PubMed] [Google Scholar]
- 61.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 62.Bazazi AR, et al. High prevalence of non-fatal overdose among people who inject drugs in Malaysia: Correlates of overdose and implications for overdose prevention from a cross-sectional study. Int J Drug Policy. 2015;26(7):675–81. doi: 10.1016/j.drugpo.2014.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Singh D, et al. Substance Abuse and the HIV Situation in Malaysia. J Food Drug Anal. 2013;21(4):S46–S51. doi: 10.1016/j.jfda.2013.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vijay A, et al. Treatment readiness, attitudes toward, and experiences with methadone and buprenorphine maintenance therapy among people who inject drugs in Malaysia. J Subst Abuse Treat. 2015;54:29–36. doi: 10.1016/j.jsat.2015.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Singer M. Syndemics. The Wiley Blackwell Encyclopedia of Health, Illness, Behavior, and Society; 2006. [Google Scholar]
- 66.Rhodes T, et al. The social structural production of HIV risk among injecting drug users. Soc Sci Med. 2005;61(5):1026–44. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- 67.Csete J. "Second on the needle": human rights of women who use drugs. HIV AIDS Policy Law Rev. 2006;11(2-3):66–7. [PubMed] [Google Scholar]
- 68.Greenfield SF, et al. Substance abuse treatment entry, retention, and outcome in women: a review of the literature. Drug Alcohol Depend. 2007;86(1):1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zilberman M, Tavares H, el-Guebaly N. Gender similarities and differences: the prevalence and course of alcohol- and other substance- related disorders. J Addict Dis. 2003;22(4):61–74. doi: 10.1300/j069v22n04_06. [DOI] [PubMed] [Google Scholar]
- 70.Auerbach J. Transforming social structures and environments to help in HIV prevention. Health Aff (Millwood) 2009;28(6):1655–65. doi: 10.1377/hlthaff.28.6.1655. [DOI] [PubMed] [Google Scholar]
- 71.Auerbach JD, Coates TJ. HIV prevention research: accomplishments and challenges for the third decade of AIDS. Am J Public Health. 2000;90(7):1029–32. doi: 10.2105/ajph.90.7.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Auerbach JD, Parkhurst JO, Caceres CF. Addressing social drivers of HIV/AIDS for the long-term response: conceptual and methodological considerations. Glob Public Health. 2011;6(Suppl 3):S293–309. doi: 10.1080/17441692.2011.594451. [DOI] [PubMed] [Google Scholar]
- 73.Earnshaw VA, et al. Exploring intentions to discriminate against patients living with HIV/AIDS among future healthcare providers in Malaysia. Trop Med Int Health. 2014;19(6):672–679. doi: 10.1111/tmi.12306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jin H, et al. An assessment of health-care students' attitudes toward patients with or at high risk for HIV: implications for education and cultural competency. AIDS Care. 2014;26(10):1223–8. doi: 10.1080/09540121.2014.894616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Vicknasingam B, Narayanan S, Navaratnam V. Prevalence rates and risk factors for hepatitis C among drug users not in treatment in Malaysia. Drug Alcohol Rev. 2009;28(4):447–54. doi: 10.1111/j.1465-3362.2009.00087.x. [DOI] [PubMed] [Google Scholar]
- 76.Vicknasingam B, et al. Injection of buprenorphine and buprenorphine/naloxone tablets in Malaysia. Drug Alcohol Depend. 2010;111(1-2):44–9. doi: 10.1016/j.drugalcdep.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 77.Chawarski MC, et al. Lifetime ATS use and increased HIV risk among not-in-treatment opiate injectors in Malaysia. Drug Alcohol Depend. 2012;124(1-2):177–80. doi: 10.1016/j.drugalcdep.2011.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bachireddy C, et al. Attitudes toward opioid substitution therapy and pre-incarceration HIV transmission behaviors among HIV-infected prisoners in Malaysia: implications for secondary prevention. Drug Alcohol Depend. 2011;116(1-3):151–7. doi: 10.1016/j.drugalcdep.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rhodes T, Simic M. Transition and the HIV risk environment. BMJ. 2005;331(7510):220–3. doi: 10.1136/bmj.331.7510.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Treisman G, Angelino A. Interrelation between psychiatric disorders and the prevention and treatment of HIV infection. Clin Infect Dis. 2007;45(Suppl 4):S313–7. doi: 10.1086/522556. [DOI] [PubMed] [Google Scholar]
- 81.Treisman G, et al. Mood disorders in HIV infection. Depress Anxiety. 1998;7(4):178–87. doi: 10.1002/(sici)1520-6394(1998)7:4<178::aid-da6>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 82.Dolan K, et al. HIV in prison in low-income and middle-income countries. Lancet Infect Dis. 2007;7(1):32–41. doi: 10.1016/S1473-3099(06)70685-5. [DOI] [PubMed] [Google Scholar]
- 83.Maru DS, Basu S, Altice FL. HIV control efforts should directly address incarceration. Lancet Infect Dis. 2007;7(9):568–9. doi: 10.1016/S1473-3099(07)70190-1. [DOI] [PubMed] [Google Scholar]
- 84.Samuel R, Omar R. Female prisoners in Malaysia: An examination of sociodemographic characteristics. Procedia - Social and Behavioral Sciences. 2012;65:505–510. ICIBSoS 2012. [Google Scholar]
- 85.Granich RM, et al. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373(9657):48–57. doi: 10.1016/S0140-6736(08)61697-9. [DOI] [PubMed] [Google Scholar]
- 86.Montaner J. Treatment as prevention: toward an AIDS-free generation. Top Antivir Med. 2013;21(3):110–4. [PMC free article] [PubMed] [Google Scholar]
- 87.Kermode M, et al. Meeting the needs of women who use drugs and alcohol in North-east India - a challenge for HIV prevention services. BMC Public Health. 2012;12:825. doi: 10.1186/1471-2458-12-825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hammad A, et al. Substance Abuse. In: Nassar-McMillan Sylvia C., Ajrouch Kristine J., Hakim-Larson Julie., editors. Biopsychosocial Perspectives on Arab Americans: Culture, Development, and Health. Springer; New York, NY.: 2014. pp. 287–305. [Google Scholar]
- 89.Rehman T. Social Stigma, Cultural Constraints, or Poor Policies: Examining the Pakistani Muslim Female Population in the United States and Unequal Access to Professional Mental Health Services. Columbia Undergraduate Journal of South Asian Studies. 2010;II:1–21. [Google Scholar]
- 90.Cheemeh PE, et al. HIV/AIDS in the Middle East: a guide to a proactive response. J R Soc Promot Health. 2006;126(4):165–71. doi: 10.1177/1466424006066280. [DOI] [PubMed] [Google Scholar]