Abstract
Although health professionals may be assumed to make healthier lifestyle choices and have better health outcomes than others due to greater health literacy, little is known about how actual health outcomes of health professionals compare to the overall population. We analyzed how trends in obesity, diabetes, hypertension, and coronary artery disease prevalence as well as several health behaviors (smoking, alcohol use, and exercise) varied between health professionals and the general U.S. population from 2002 to 2013, using nationally representative data collected by the National Health Interview Survey. We estimated multivariable logistic regressions of each disease and behavior adjusted for age, race, sex, geographic region, and year. Although rates of obesity, diabetes, and hypertension were lower among health professionals compared to the overall population, disease was still common among health professionals and increased at a similar rate over time compared to the overall population. For example, obesity prevalence was lower among health professionals but increased similarly from 2002 to 2013 (health professionals, 20.5% in 2002 to 22.1% in 2013; other occupations, 28.4% to 31.7%; P=.64 for difference in trend). Diabetes prevalence was modestly lower among health professionals but increased at a similar trend (health professionals, 7.4% in 2005 to 8.6% in 2013; other occupations, 8.7% to 9.9%; P=.67 for difference in trend). Similar patterns were noted in hypertension. Coronary artery disease prevalence declined over time among health professionals but increased for others. Health professionals reported better health behaviors than others in smoking and physical activity, but not in moderate-to-heavy alcohol use.
INTRODUCTION
Health professionals may be assumed to make healthier lifestyle choices and have better health outcomes than others due to greater health literacy, education, and experience with patients. Despite data on how the prevalence of health behaviors compares between health professionals and others,1 it is unknown how actual health outcomes compare. We analyzed how trends in several health behaviors as well as obesity, diabetes, hypertension, and coronary artery disease prevalence varied between health professionals and the general U.S. population from 2002 to 2013.
METHODS
We compared trends in health behaviors and disease prevalence between health professionals and others using the National Health Interview Survey for 2002, 2005, 2007, 2010, and 2013. This probability-based survey of U.S. adults includes data on demographics, occupation, health behaviors, and chronic diseases.2 Health professionals included physicians, dentists, chiropractors, pharmacists, physician assistants, therapists, and nurse practitioners.3 Specific occupation was unavailable.
Respondents were asked about smoking, drinking, and exercise habits as well as height, weight, and whether they were ever diagnosed with diabetes, coronary artery disease, or hypertension (the latter three conditions were queried in 2005 onwards). Body-mass index was computed based on height and weight.
We estimated the association between each disease outcome (or behavior) with individual occupation (health professional versus general population), adjusting for individual age, race, sex, and census geographic region in a multivariable logistic regression. Each disease outcome or behavior was used as the dependent binary variable in separate logistic regressions. A separate regression was estimated for each outcome variable and for each of four time periods (2005, 2007, 2010, and 2013), comprising 24 total regressions. The key independent variable in all models was occupation. Based on these models, we computed adjusted disease and behavior prevalence according to year and occupation, holding other covariates at their mean values. In other words, we use the statistical technique of marginal effect at the mean to determine the marginal effect occupation has on outcome prevalence while holding other covariates like age, sex, and geographic region at their mean values in the sample. Analyses stratifying by sex were also performed.
RESULTS
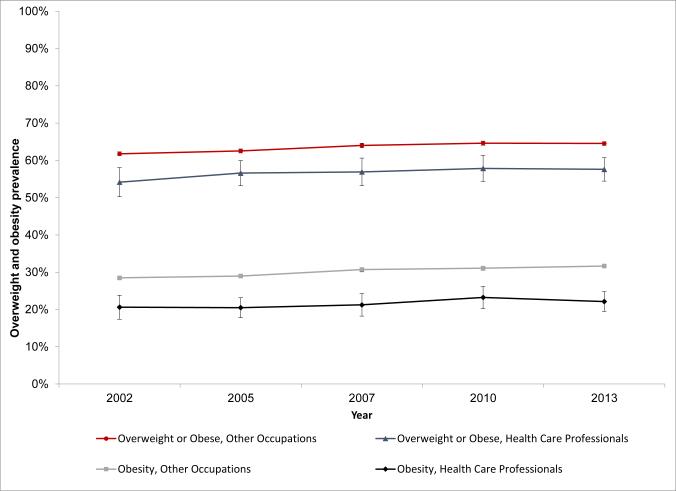
Our sample consisted of 147,129 respondents (3,869 health professionals; 2.6%). Obesity prevalence among health professionals increased from 20.5% in 2002 to 22.1% in 2013. Among other occupations, obesity increased from 28.4% to 31.7% (Figure). While obesity was less common among health professionals than other occupations, both groups experienced similar absolute percentage point increases in prevalence (P=.64 for difference in absolute percentage point change among health professionals versus absolute percentage point change among others).
Figure. Trends in adjusted prevalence of overweight status and obesity in health care professionals and other occupations.
Overweight defined as body mass index (BMI) 25 to 30. Obesity defined as BMI greater than or equal to 30.
The Table summarizes the results of the logistic regression analyses. Adjusted diabetes prevalence increased from 7.4% in 2005 to 8.6% in 2013 among health professionals and from 8.7% to 9.9% for other occupations (Table). Although diabetes prevalence was lower in health professionals than other occupations, absolute percentage point increases in prevalence were similar between both groups (P=.67 for difference in absolute percentage point change among health professionals versus absolute percentage point change among others). Similar patterns were noted for hypertension, whereas coronary artery disease decreased among health professionals compared to others.
Table.
Trends in adjusted prevalence of health outcomes and lifestyle behaviors in health care professionals and other occupations
| 2005 | 2007 | 2010 | 2013 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Health care Professionals (n = 838) | Others (n = 30,590) | Health care Professionals (n = 664) | Others (n = 22,279) | Health care Professionals (n = 771) | Others (n = 26,386) | Health care Professionals (n = 974) | Others (n = 33,583) | |||||
| Adjusted Prevalence (95% CI) | P | Adjusted Prevalence (95% CI) | P | Adjusted Prevalence (95% CI) | P | Adjusted Prevalence (95% CI) | P | |||||
| Health outcomes | ||||||||||||
| Diabetes | 7.4 (5.4, 9.0) |
8.7 (8.4, 9.0) |
.11 | 8.2 (6.1, 10.2) |
8.9 (8.6,9.3) |
.49 | 9.0 (6.9,11.0) |
10.2 (9.8,10.5) |
.25 | 8.6 (6.8,10.4) |
9.9 (9.6,10.2) |
.16 |
| Coronary heart disease | 5.8 (4.2,7.5) | 6.4 (6.2,6.7) |
.47 | 6.2 (4.4,8.0) |
6.1 (5.8,6.4) |
.90 | 5.1 (3.5,6.7) |
6.3 (6.1,6.6) |
.12 | 4.8 (3.5,6.2) |
6.3 (6.1,6.5) |
.03 |
| Hypertension | 25.8 (23.1,28.4) |
28.9 (28.5,29.4) |
.02 | 30.1 (27.1,33.1) |
29.8 (29.3,30.3) |
.83 | 30.3 (27.4,33.2) |
32.6 (32.1,33.1) |
.13 | 28.2 (25.6,30.7) |
31.5 (31.1,31.9) |
.01 |
| Health behaviors | ||||||||||||
| Currently smoke | 9.7 (7.6, 11.7) |
20.7 (20.2, 21.1) |
<.001 | 9.0 (6.8, 11.2) |
18.8 (18.3,19.3) |
<.001 | 8.6 (6.6,10.7) |
19.2 (18.8,19.7) |
<.001 | 7.2 (5.5,8.9) |
18.6 (18.2,19.1) |
<.001 |
| Currently moderate-heavy alchohol consumptiona | 19.5 (16.5,22.5) |
17.9 (17.5,18.4) |
.31 | 16.7 (13.6,19.8) |
17.5 (17.0,18.0) |
.63 | 24.8 (21.4,28.3) |
18.9 (18.4,19.3) |
<.001 | 23.2 (20.2,26.3) |
20.1 (19.7,20.5) |
.04 |
| Sedentary activityb | 50.4 (46.9,53.8) |
66.6 (66.1,67.1) |
<.001 | 51.0 (47.3,54.7) |
66.6 (66.1,67.2) |
<.001 | 46.8 (43.3,50.4) |
60.8 (60.3,61.4) |
<.001 | 40.3 (37.2,43.4) |
58.0 (57.5,58.6) |
<.001 |
Notes:
= Moderate drinking was defined as 4-14 drinks per week in men and 4-7 drinks per week in women. Heavy drinking was defined as >14 drinks in men and >7 drinks in women.
= Respondents were considered sedentary if they reported engaging in light, moderate, and vigorous activity less than once a week.
P-value reflects comparison of adjusted chronic condition disease prevalence between health care professionals and others, in each time period. Prevalence was adjusted for age, sex, race, and geographic region.
Health professionals reported better health behaviors than others in smoking and physical activity, but not in alcohol use. Smoking prevalence among health professionals decreased from 9.7% in 2005 to 7.2% in 2013. Among other occupations, smoking decreased from 20.7% to 18.6%. Similar patterns were seen among respondents reporting a sedentary lifestyle. Moderate-to-heavy alcohol consumption was more common among health professionals in recent years and increased from 19.5% in 2005 to 23.2% in 2013, with a similar increase observed in other occupations (17.9% to 20.1%). However, it should be noted that the percent of health professionals reporting heavy alcohol consumption was consistently less than 1%, while up to 4% of individuals in all other occupations reported heavy drinking.
In sex-stratified analysis, health behavior and disease trends did not vary by sex, with two exceptions. First, diabetes among male health professionals modestly declined, while it increased among males in other occupations and females regardless of profession. Second, males reporting moderate-to-heavy alcohol consumption remained stable, while females of all occupations reported increases in alcohol consumption.
DISCUSSION
Health professionals have lower rates of smoking, sedentary activity, obesity, diabetes, hypertension and coronary artery disease compared to other occupations, but higher rates of moderate-to-heavy alcohol use. Non-health professionals had a higher prevalence of heavy alcohol use. With the exception of coronary artery disease, changes in disease burden among health professionals have mirrored those in other occupations, suggesting that common factors have affected both groups similarly. While public health strategies can be effective in reversing growth in chronic disease and unhealthy behaviors,4 they may have their limits if health professionals, who are arguably more knowledgeable about these topics, experience similar chronic disease trends. Nonetheless, the overall population's knowledge regarding unhealthy behaviors such as smoking and sedentary activity appears to be improving, given the decrease in these behaviors observed over the time period.
The similar increase in diabetes and hypertension across health professionals and all other occupations suggests that despite how much the knowledge gap may have changed between health professionals and all other occupations, the overall change in health behaviors contributing to these diseases has remained relatively constant across occupation groups.
Our study had limitations. First, disease was self-reported. Differences in disease prevalence between health professionals and others may be larger than estimated if health professionals are more likely to be diagnosed or recall their diseases when surveyed. Moreover, some health behaviors such as alcohol consumption may be considerably underreported.5 For this reason, we deemed it appropriate to group moderate and heavy alcohol consumption together to better capture high risk drinking behavior.
Second, specific occupation data was unavailable; health outcomes may vary across types of health care providers. For instance, a study examining the health of U.S. cardiologists showed that cardiologists engaged in better health behaviors and had more favorable health outcomes than the general population.6
Third, it is possible that some individuals switched from health professional to an “all other” occupation (or vice versa) over the study's time period. However, each year the NHIS draws a new national sample so the likelihood of sampling the same individual in more than one year is low.
CONCLUSION
Although health professionals may arguably make healthier lifestyle choices and have better health outcomes than others due to greater health literacy, little is known about how actual health outcomes of health professionals compare to the overall population. Using nationally representative data collected by the National Health Interview Survey, we found that rates of obesity, diabetes, and hypertension were lower among health professionals compared to the overall population but were still considerable in prevalence. For each disease, prevalence increased at a similar rate over time compared to the overall population. Coronary artery disease prevalence declined over time among health professionals but increased for others. Health professionals reported better health behaviors than others in smoking and physical activity, but not in moderate-to-heavy alcohol use.
Acknowledgements
The authors report funding from the Office of the Director, National Institutes of Health (Dr. Jena, NIH Early Independence Award, Grant 1DP5OD017897-01).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
conflicts of interest:
The authors have no conflicts of interest to report. The funders had no involvement in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Dr. Jena had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCES
- 1.Helfand BK, Mukamal KJ. Healthcare and lifestyle practices of healthcare workers: do healthcare workers practice what they preach? JAMA Intern Med. 2013;173(3):242–4. doi: 10.1001/2013.jamainternmed.1039. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention, National Center for Health Statistics [February 24, 2015];National Health Interview Survey. www.cdc.gov/nchs/nhis.htm.
- 3.United States Department of Labor Bureau of Labor Statistics. [February 24, 2015];Standard Occupational Classification. www.bls.gov/soc/2010/soc290000.htm.
- 4.Diabetes Prevention Program Research Group. Knowler WC, Fowler SE, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374(9702):1677–86. doi: 10.1016/S0140-6736(09)61457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feunekes GI, van 't Veer P, van Staveren WA, et al. Alcohol intake assessment: the sober facts. Am J Epidemiol. 1999;150(1):105–12. doi: 10.1093/oxfordjournals.aje.a009909. [DOI] [PubMed] [Google Scholar]
- 6.Abuissa H, Lavie C, Spertus J, et al. Personal health habits of American cardiologists. Am J Cardiol. 2006;97(7):1093–6. doi: 10.1016/j.amjcard.2005.10.057. [DOI] [PubMed] [Google Scholar]