Abstract
Elastography is a new ultrasound modality that provides images and measurements related to tissue stiffness. Endoscopic ultrasound (EUS) has played an important role in the diagnosis and management of numerous abdominal and mediastinal diseases. Elastography by means of EUS examination can assess the elasticity of tumors in the proximity of the digestive tract that are hard to reach with conventional transcutaneous ultrasound probes, such as pancreatic masses and mediastinal or abdominal lymph nodes, thus improving the diagnostic yield of the procedure. Results from previous studies have promised benefits for EUS elastography in the differential diagnosis of lymph nodes, as well as for assessing masses with pancreatic or gastrointestinal (GI) tract locations. It is important to mention that EUS elastography is not considered a modality that can replace biopsy. However, it may be a useful adjunct, improving the accuracy of EUS-fine needle aspiration biopsy (EUS-FNAB) by selecting the most suspicious area to be targeted. Even more, it may be useful for guiding further clinical management when EUS-FNAB is negative or inconclusive. In the present paper we will discuss the current knowledge of EUS elastography, including the technical aspects, along with its applications in the differential diagnosis between benign and malignant solid pancreatic masses and lymph nodes, as well as its aid in the differentiation between normal pancreatic tissues and chronic pancreatitis. Moreover, the emergent indication and future perspectives are summarized, such as the benefit of EUS elastography in EUS-guided fine needle aspiration biopsy, and its uses for characterization of lesions in liver, biliary tract, adrenal glands and GI tract.
Keywords: Elastography, Endoscopic ultrasound, Characterization, Pancreas, Lymph nodes
Core tip: Endoscopic ultrasound (EUS) has played an important role in the diagnosis and management of numerous abdominal and mediastinal diseases. In the present paper, we discuss the current knowledge of EUS elastography, including the technical aspects, its applications in the differentiation between benign and malignant solid pancreatic masses and lymph nodes, and differentiation between normal pancreatic tissues and chronic pancreatitis. Moreover, the emergent indication and future perspectives are also summarized, such as the benefit of EUS elastography in EUS-guided fine needle aspiration biopsy, and its use for characterization of lesions in liver, biliary tract, adrenal glands and gastrointestinal tract.
INTRODUCTION
Elastography is an imaging modality used to demonstrate tissue stiffness. It has been investigated by ultrasound since the early 1990’s. So far, two (elastography) techniques, i.e., strain technique and shear wave technique, have been developed and clinically used. Endoscopic ultrasound (EUS) elastography is the application of elastography performed during EUS procedure. Currently, only the strain technique has been available for EUS examinations. Shear wave elastography has been equipped in the transrectal ultrasound transducer of Supersonic system (Aixplorer, France), but it is not one of the topics of this paper. Strain elastography (SE) is a qualitative method based on tissues response to an externally or internally generated force[1,2]. It is based on the fact that stiffer tissues have lower strains, meaning that they deform less under compression as compared to softer tissues which deform more. With SE, the compression-induced tissues deformations within a region of interest (ROI) are comparatively assessed. The resultant strains are displayed as transparent colors overlaid on the B-Mode image, just like for Doppler ultrasound. Different colors are used to demonstrate differences between stiffness of the ROI included tissues.
The measurement of displacement is made using a sophisticated algorithm based on the Extended Combined Autocorrelation Method[3-5]. The characteristics of the tissues can be further analyzed either by the color-based qualitative method[6,7] as described above, or by using a semi-quantitative method based on strain ratios between different tissues included within the selected ROI[8,9].
SE with conventional ultrasound systems has been used for the evaluation of lesions in the breast, cervix, prostate gland and thyroid gland as well as for staging of liver fibrosis[10-15] proving good results. It has been shown that malignant tissues are generally harder than adjacent normal tissues, therefore, it could differentiate benign from malignant lesions based on the stiffness characteristics[10-14].
EUS, with high-frequency transducers can offer high-resolution images of the digestive tract and also of the adjacent organs. It plays an important role in the diagnosis and management of numerous abdominal and mediastinal diseases[16-18].
The combination of EUS and elastography improves the diagnostic yield of EUS. It can assess the elasticity of tumors in the proximity of the digestive tract that are hard to reach with conventional transcutaneous ultrasound probes, such as pancreatic masses[19-22] and lymph nodes[23,24]. Results from early studies look promising for the differential diagnosis of solid masses [i.e., lymph nodes, pancreatic or gastrointestinal (GI) tract masses].
Endoscopic ultrasound-guided fine needle aspiration biopsy (EUS-FNAB) is performed when patient management would be affected[25,26]. However, it is an invasive technique and has the risk of bleeding and seeding of malignant cells[27-29]. The accuracy of EUS-FNAB is affected by the selection of the targeted area within the lesion to be assessed and it is dependent upon the lesion’s visibility[30]. Although EUS elastography at present cannot replace EUS-FNAB for the diagnosis of a focal lesion located in the pancreas or for assessing lymph nodes, it still may be a useful adjunct for guiding further clinical management when EUS-FNAB is negative or inconclusive[26,31,32]. In addition, EUS elastography can show the hardest areas within the lesion, thus being useful for the selection of the most suspicious area to be targeted for EUS-FNAB, finally improving the accuracy of the method[25].
In the presented paper, we discuss the current knowledge of EUS elastography, including technical aspects, its current applications for benign-malignant solid pancreatic masses and lymph nodes differentiation, as well as its use for differentiation between normal pancreatic tissues and chronic pancreatitis. Moreover, the emergent indication and future perspectives are also summarized, such as the use of elastography in EUS-FNAB, characterization of lesions in the liver, biliary tract, adrenal glands and GI tracts.
CURRENT EXAMINATION TECHNIQUES USED IN EUS ELASTOGRAPHY (QUALITATIVE AND SEMI-QUANTITATIVE METHODS)
Both qualitative and semi-quantitative methods have been developed in EUS elastography to analyze the tissues stiffness. The former, using hue histogram analysis and artificial neural networks, is the first one equipped in the early generation of ultrasound systems[8,20]. Afterward, strain histogram (SH) and strain ratio (SR) were introduced in the second-generation EUS elastography systems as reproducible, parametric measurements. SH computes the strain values of elemental areas inside a ROI and produces a graph, while SR measures the relative strain between two selected areas inside a ROI[25,33]. They both analyze the tissue stiffness in a (semi-) quantitative manner and, therefore, they are greatly reducing the human bias without the need for a 3rd-party software[34].
Qualitative EUS elastography
EUS elastography detects small structural deformations caused by compression and grades the degree of relative deformation between ROI included tissues on a scale of 1-255. Each value is assigned a different shade from a hue color spectrum for further visual recognition[25]. Most systems are using a red-green-blue color map in which stiffer tissue areas are shown in dark blue to blue, whilst softer tissue areas are displayed in hues of green to red. Because the strain (deformation) will be smaller in stiffer tissues and larger in softer tissues, the stiffness contrast can be displayed in real-time and can be superimposed as a transparent overlay on the real-time gray-scale EUS image[30]. The ROI for the elastographic evaluation is manually selected and should include both the lesion entirety (when possible) and also normal surrounding tissue. Qualitative analysis includes a five-step score method based on the predominant color pattern inside the lesion: homogenously hard, heterogenously hard, mixed, heterogenously soft or homogenously soft[3,7,35-38].
How to perform: As with conventional EUS, the endoscopes have to be carefully manipulated to obtain a good and a reproducible elastographical image. Both longitudinal and radial echoendoscopes can be used for elastography, however, the former has the advantage that suspicious stiffer areas can be targeted for biopsy under direct visualization[30,39].
A ROI is used to define the area of interest in a similar manner to that used for a color Doppler examination. By manipulating the probe, the necessary pressure can be applied. Very little extra compression is seldom needed to obtain an elastographical image, since with careful placement of the endoscope, the regular pressure variation from the pulsation of adjacent vessels will normally be sufficient if the system settings are appropriately sensitive. However, the size of the ROI that defines the elastographic image is important. The ROI should be sufficiently large to include both the pathological tissue under investigation and surrounding “normal” tissue as a reference. The best image quality was recorded in phantom experiments when the lesion of interest covered 25%-50% of the ROI[40]. In practice, for EUS elastography applications, a ratio of approximately 50% lesion, 50% normal surrounding tissue is usually achievable[35,41]. If the ROI is too small, only the relative elasticity differences within the lesion will be measured and displayed rather than the assessment of the lesion stiffness compared to normal surrounding tissues[1,30].
(Semi-)quantitative EUS elastography
Two quantitative techniques have been developed to improve the accuracy and reproducibility of the method and to minimize the operator bias in stiffness evaluation.
One is based on the comparison between two tissue areas within the ROI to compute a SR[3,9,21,42]. This technique is a semi-quantitative method since the elasticity is expressed as a relative ratio but not as an absolute value[43]. Using this technique, two non-overlapping areas are selected, usually area A is the lesion, area B is the reference zone, and SR represents the B/A quotient[9].
Another method that has been used is the calculation of the mean value of the hue histogram SH, which represents the mean strain value within the selected area[8,15]. The histogram is a graph that quantifies and represents a specific characteristic (e.g., digitized color distribution) inside the ROI of an elastography image[25]. SH software has been equipped in the newer ultrasound machines, and the graph can be automatically created. Within the graph, the X-axis represents the elasticity values (each value represents a pixel color) from 0 to 255, where 0 is hardest and 255 is softest, the Y-axis values represent the number of pixels of each value.
CURRENT CLINICAL APPLICATIONS OF EUS ELASTOGRAPHY
EUS elastography is only applied to assess the elasticity of solid lesions based on its principles, while cystic lesions are usually shown as an artifact, i.e., BGR (blue-green-red) artifact[4,5]. A lesion that has cystic components should not be evaluated by EUS elastography. Therefore, the current clinical indications of EUS elastography are mainly solid pancreatic lesions, submucosal GI masses, lymph nodes, focal left liver lesions and left adrenal lesions. Few other indications have been also reported[44].
Pancreas
The normal pancreas appears elastographically soft (homogenously green) on EUS elastography in most cases, which has been shown to be highly reproducible[6,45].
Focal pancreatic masses: Malignant pancreatic lesions are generally harder than adjacent pancreatic tissue. Therefore, measuring strain might aid classification of pancreatic masses. Meta-analyses demonstrated that EUS elastography is a reliable technique for the differentiation of solid pancreatic masses with a pooled sensitivity of 95%-97% and a specificity of 67%-76%, respectively[46-48].
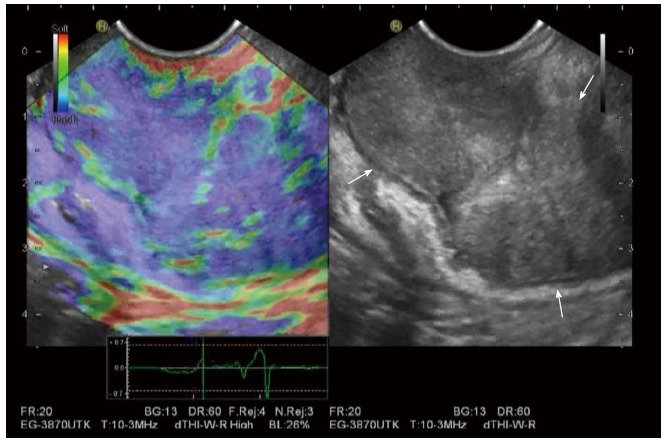
Qualitative techniques: EUS elastography has been considered a promising tool for differentiation of benign and malignant solid pancreatic masses[6,7,34,36,38]. On EUS elastography, malignant lesions (e.g., pancreatic ductal adenocarcinoma), due to the presence of fibrosis and marked desmoplasia, appears stiffer than the adjacent normal pancreatic parenchyma[7]. Still, no evidence shows that there is a correlation between the tumor stiffness and either the tumor grading, or collagenous content[42] (Figure 1).
Figure 1.
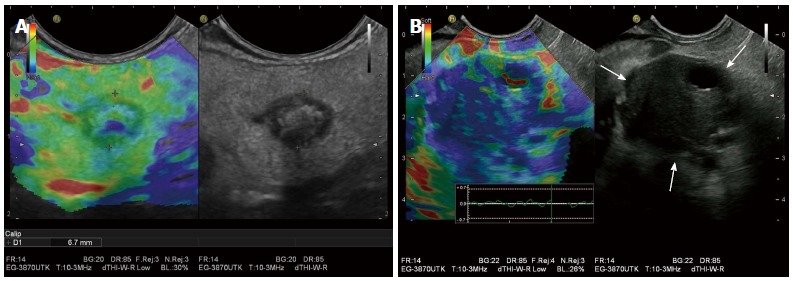
Benign and malignant pancreatic masses on endoscopic ultrasound elastography. A: A pancreatic teratoma is shown as heterogeneous soft (green) pattern (left: EUS elastography image; right: B-mode image); B: A pancreatic ductal adenocarcinoma appears stiffer (blue) than the adjacent normal pancreatic parenchyma, probably due to the presence of fibrosis and marked desmoplasia.
Different classification of color patterns has been used to distinguish malignant masses from benign ones[6], though this simplistic approach has been contradicted by other authors and later articles[35]. A five score classification was firstly reported in 2006 based on the color patterns of lesions, by Giovannini et al[6], with a sensitivity of 100% and a specificity of 67% (Table 1). In this scoring system, scores 3-5 were considered malignant, while 1 and 2 were considered benign. In 2009, Giovannini et al[34] published their results based on a multicenter study using the same scoring system, the accuracy being 89.2%, and both sensitivity and positive predictive value (PPV) being over 90%. A four score classification has also been used by other authors (Table 2), the diagnostic sensitivity, specificity and overall accuracy of EUS elastography for diagnosing malignancy being of 100%, 85.5% and 94%, respectively based on this score[38].
Table 1.
Five score classification system for endoscopic ultrasound elastography
| Score | Color pattern | Stiffness | Histology | Ref. |
| 1 | Green | Homogeneous soft | Normal pancreatic tissue | [6,34] |
| 2 | Green, yellow and red | Soft heterogeneity | Fibrosis | [6,34] |
| 3 | Mostly blue with minimal heterogeneity | Hard | Early pancreatic adenocarcinoma | [6,34] |
| 4 | Central green hypoechoic region and blue tissue outer layer | Hard | Neuroendocrine tumor, metastasis | [6,34] |
| 5 | Blue lesions with heterogeneity due to necrosis | Hard | Advanced pancreatic adenocarcinoma | [6,34] |
Table 2.
Four score classification system for endoscopic ultrasound elastography
| Score | Color pattern | Stiffness | Histology | Ref. |
| 1 | Homogeneous green | Soft | Normal pancreas | [38] |
| 2 | Heterogeneous, green-Predominant | Soft | Inflammatory pancreatic masses | [38] |
| 3 | heterogeneous, blue-Predominant | Hard | Pancreatic malignant tumors | [38] |
| 4 | homogeneous blue | Hard | Pancreatic neuroendocrine malignant lesions | [38] |
However, disappointing results of qualitative EUS elastography have also reported in two studies[7,35]. Hirche et al[35] found that the diagnostic sensitivity, specificity and accuracy for predicting the nature of pancreatic lesions were just 41%, 53% and 45%, respectively. Also, Janssen et al[7], as the result of their study, concluded that chronic pancreatitis and hard malignant tumors cannot be distinguished by elastography, probably due to their similar fibrous structure.
Therefore, the diagnostic accuracy of qualitative EUS elastography is variable among studies, probably because of the subjective interpretation of the elastographic pattern caused by perception errors and the inability of the human eye to completely characterize all color hues[45,49]. Even though some bias cannot be avoided, one study showed very good correlation between observers by analyzing the videos recorded from 258 patients with chronic pancreatitis and pancreatic cancer[20].
Quantitative EUS elastography: As previously described, both SR and SH are possible methods to quantitatively characterize pancreatic lesions. It is reported that there are no differences regarding the accuracy of the two techniques for the differentiation between benign and malignant pancreatic masses[33].
SR: Iglesias-Garcia et al[9] firstly published the results of a prospective study concerning the accuracy of quantitative EUS elastography for the differential diagnosis of solid pancreatic masses on 86 consecutive patients. The results of their study showed that quantitative EUS elastography with strain ratio has higher accuracy (97.7%) and specificity (92.9%) as compared to the qualitative analysis. A SR higher than 6.04 or a mass elasticity lower than 0.05% is 100% sensitive for classification of tumors as being malignant. The specificity can be improved to 100% with a SR higher than 15.41 or a mass elasticity value below 0.03%. In addition, EUS elastography could differentiate pancreatic cancers from inflammatory masses (100% sensitivity and 96% specificity), and pancreatic cancers from neuroendocrine tumors (100% sensitivity and 88% specificity).
Using the same methods as within the above study[9], another study retrospectively evaluated 109 patients with solid pancreatic masses[21]. With the qualitative technique, all pancreatic cancers presented intense blue coloration, however, the inflammatory masses showed mixed colorations (green, yellow, and low-intensity blue). With the quantitative technique, the mean SR was 39.08 ± 20.54 for pancreatic cancer, and 23.66 ± 12.65 for the inflammatory masses (P < 0.05).
SH: Quantitative EUS elastography with SH has also been investigated in studies. Using 175 as the cut off value of the mean SH, Săftoiu et al[8] reported sensitivity, specificity, PPV, negative predictive value (NPV) and accuracy of 91.4%, 87.9%, 88.9%, 90.6%, and 89.7%, respectively, in differentiating between benign and malignant pancreatic masses. Recently, a multicenter study with 258 patients used the same cut-off value (175), and found that sensitivity, specificity, PPV, NPV and accuracy of EUS elastography were 93.4%, 66.0%, 92.5%, 68.9%, and 85.4%, respectively[20]. In another study, Schrader et al[42] evaluated the usefulness of SH in differentiating malignant pancreatic masses from normal pancreas and found a very promising result with 100% sensitivity and 100% specificity for malignancy detection. However, a limitation of this study was the selection of the control group, since the authors used normal pancreas as control group compared with the group with malignant pancreatic diseases, but did not use patients with pancreatic masses or chronic pancreatitis as control group.
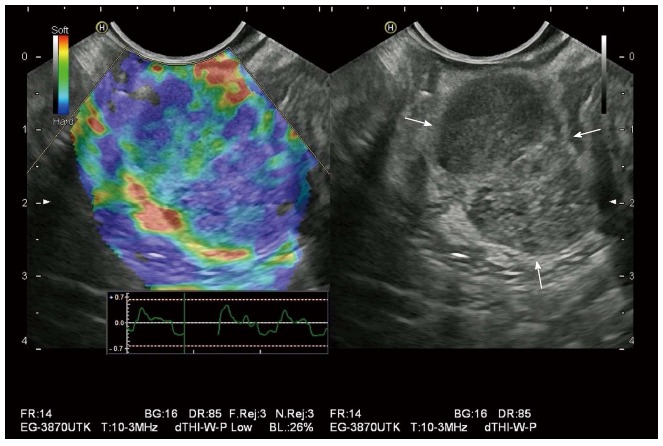
Combination of elastography and contrast-enhanced color Doppler ultrasound in EUS: Malignant solid pancreatic masses are usually hypo-vascular on (contrast enhanced) color Doppler ultrasound and hypo-enhancing on contrast-enhanced ultrasound[50] (Figure 2). A study by Săftoiu et al[22] found that the combination between EUS elastography and contrast-enhanced color Doppler EUS could offer important information for the decision-making process, especially in patients with negative EUS-FNAB and strong clinical suspicion of malignancy. In their study, both modalities were performed sequentially during the same EUS examination in 21 patients with chronic pancreatitis and in 33 patients with pancreatic ductal adenocarcinoma. The sensitivity, specificity, accuracy, PPV and NPV of the combined techniques for differentiation of hypo-vascular hard masses suggestive of pancreatic carcinoma were 75.8%, 95.2%, 83.3%, 96.2% and 71.4%, respectively.
Figure 2.
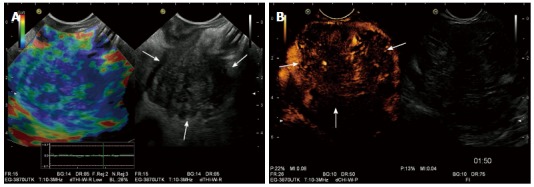
Combination of elastography and contrast-enhanced ultrasound in endoscopic ultrasound. A: A pancreatic ductal adenocarcinoma is demonstrated as a heterogeneous hard (blue) pattern; B: On contrast-enhanced endoscopic ultrasound, pancreatic ductal adenocarcinoma is hypo-enhancing.
Diffuse pancreatic diseases
Chronic pancreatitis: EUS has become one important method for the diagnosis of chronic pancreatitis in clinical practice. Still, there are many challenges with the criteria from EUS, especially for diagnosing non-advanced stages. EUS elastography can provide additional relevant information of tissue stiffness and thus may benefit the diagnosis of chronic pancreatitis. In a recent published prospective study[51], quantitative EUS elastography was performed in 191 patients (from which 92 were finally diagnosed with chronic pancreatitis), The SR was measured in the head, body and tail of the pancreas and the mean value was used for analysis. For each measurement of SR, area A was the largest possible area of pancreatic parenchyma, and area B referred to a soft (red) reference area corresponding to normal surrounding gut wall. Results showed that there was a highly significant direct linear correlation between the SR and the number of EUS criteria of chronic pancreatitis (r = 0.813). The accuracy of EUS-elastography for diagnosing chronic pancreatitis was 91.1 % (cut-off strain ratio of 2.25). Therefore, EUS-elastography is proven to be an accurate tool for the diagnosis of chronic pancreatitis according to this study.
Pancreatic fibrosis: The usefulness of EUS elastography for diagnosing the grade of pancreatic fibrosis has been evaluated in one study[52]. EUS elastography was performed in 58 consecutive patients before pancreatectomy for both pancreatic tumors and upstream pancreas. Quantitative technique with novel software was used to analyze the EUS elastography images, and 4 parameters (mean, standard deviation, skewness, and kurtosis) were calculated. Histological fibrosis was graded into 4 categories (normal, mild fibrosis, marked fibrosis, and severe fibrosis). The results showed that fibrosis grade was significantly correlated with all 4 quantification parameters, and that the mean was the most useful parameter for diagnosing pancreatic fibrosis. The area under the ROC curves for the diagnosis of mild or higher-grade fibrosis, marked or higher-grade fibrosis and severe fibrosis were 0.90, 0.90, and 0.90, respectively. Therefore, EUS elastography may be a useful tool for the accurate diagnosis of pancreatic fibrosis.
Future developments
Future developments of EUS elastography for pancreatic related pathologies include evaluation of the role of elastography-guided biopsy of the pancreas. EUS elastography has high sensitivity for detecting even very small pancreatic masses, and in addition, can be helpful in staging pancreatic cancer and for guiding a biopsy to obtain samples for cytological or histological diagnosis[1,46-48]. The additional value of elastography combined with other techniques such as contrast-enhanced endoscopic ultrasound (CE-EUS), fusion imaging or 3D elastography examinations might also be feasible[30,49].
Lymph nodes
The differentiation of benign and malignant lymph nodes (LNs) is crucial for staging, for prediction of prognosis and for selection of appropriate treatment options in many cancers, such as esophageal, stomach, bronchial, and pancreatic carcinomas. LNs that are close to the gut can be imaged with EUS, but the differential diagnosis of benign and malignant nodes with EUS remains a challenge. Although there are already some established criteria on B-mode EUS for the diagnosis of malignant LNs (such as hypoechoic structure, round shape, sharp margins, > 10 mm diameter), these features overlap sometimes with benign nodes. Also, it should be considered that malignant nodes at early stages may have less or even none of these typical features[53], the specificity and accuracy with these criteria being rather low[25,30,54,55]. In this setting, EUS-elastography, as a minimally invasive imaging modality may be helpful for the differential diagnosis of benign and malignant LNs or to single out the more suspicious nodes to be targeted for endosonographic guided tissue sampling[23,39].
Qualitative EUS elastography
Similar with pancreatic masses, malignant LNs are considered to be harder than benign ones, which has been studied in several publications[6,23,24,34,56] (Figure 3). Giovannini et al[6] first published their results on evaluation of the usefulness of qualitative EUS elastography in differentiating the benign from malignant LNs with different locations (cervical, celiac, mediastinal and aortocaval). A number of 31 lymph nodes from 25 patients were included in this study. The predominance of blue areas was considered to be related to malignancy, however, mostly green nodes and indeterminate ones (shown as heterogenicity), were classified as benign. The obtained sensitivity and specificity for determining malignancy were 100% and 50%, respectively. Janssen et al[24] evaluated the feasibility and the usefulness of qualitative EUS elastography for characterizing the LNs in the dorsal mediastinum, regarding the histological results obtained in the same session from EUS-FNAB as the gold standard. Benign LNs exhibited predominantly intermediate homogeneous deformation (yellow/green), while malignant LNs showed a quantitative dominance of hard (blue) units. The three examiners who participated in the study had accuracies ranging from 84.6% to 86.4% for malignant lymph nodes, and from 81.8% to 87.9% for benign ones. The interobserver agreement was good (kappa = 0.84).
Figure 3.
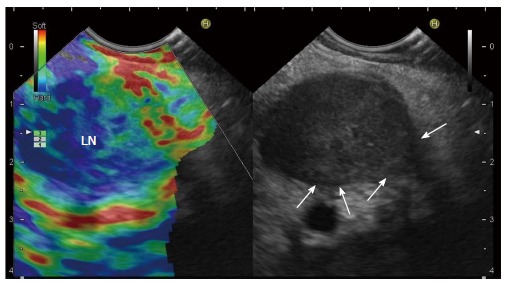
Malignant Lymph nodes on endoscopic ultrasound elastography. A malignant lymph node is revealed as predominantly hard (blue). Arrows indicate infiltration. LN: Lymph node.
A five-point scoring system has also been evaluated. In a multicenter study, scores 1 and 2 were interpreted as benign, score 3 as indeterminate and scores 4 and 5 as malignant. The obtained sensitivity, specificity, PPV, NPV, and accuracy for the detection of malignancy were 91.8%, 82.5%, 88.8%, 86.8%, and 88.1%, respectively[34]. The interobserver agreement yielded a kappa score of 0.657 for the detection of malignant LNs[34]. Săftoiu et al[56], also using a 5-score system, evaluated LNs in cervical, mediastinal, and abdominal areas, and got better results. The obtained sensitivity, specificity, and accuracy for the distinction of benign and malignant LNs were 91.7%, 94.4%, and 92.86%, respectively.
One meta-analysis including 7 studies, 368 patients and 431 LNs, has investigated the application of EUS elastography for the differentiation between benign and malignant LNs. The pooled sensitivity and specificity of EUS elastography for the differential diagnosis of benign and malignant LNs were 88% and 85%, respectively. The area under the summary receiver operating characteristic curve was 0.9456. Authors concluded that EUS elastography is a promising, non-invasive technique for the differentiation of malignant LNs, and that it may become a valuable supplemental method to EUS-guided FNAB[23].
Quantitative EUS elastography
The previously referred study by Săftoiu et al[56] also included a quantitative analysis, i.e., a separate RGB channel histograms. With a cut-off level of 0.84, the sensitivity, specificity, and accuracy for malignancy detection were 95.8%, 94.4%, and 95.2%, respectively. A subsequent study also by Săftoiu et al[57] used quantitative EUS elastography based on SH to investigate cervical, mediastinal and abdominal LNs. With a cut off value of 166 for the mean of the SH (between blue and green on the rainbow scale), the sensitivity, specificity, and accuracy of EUS elastography in the detection of malignancy were 85.4%, 91.9%, and 88.5%, respectively. The corresponding area under the curve was 0.928. Two recent studies using not only SH but also SR showed superior accuracy of EUS elastography as compared to conventional EUS criteria in differentiating benign and malignant LNs for the nodal staging of esophageal cancer[58,59].
However, only one study by Larsen et al[60], using both qualitative and quantitative (with SR) EUS elastography, did not find that EUS elastography is better than EUS morphology in differentiating between benign and malignant LNs, at least for included patients with resectable upper GI cancers.
Future development (EUS elastography for EUS-FNA)
EUS-FNA offers the most reproducible results in the diagnosis of metastatic LN infiltration, with an accuracy greater than 85%[39,54,61]. But the accuracy depends on the appropriate selection of LNs and targeting of focal infiltration within LNs for biopsy. Both B-mode diagnosis and EUS-FNAB may fail to detect the smallest LN metastases. Elastography is able to identify the smallest metastatic related changes in tissue hardness, thus it has the potential to be useful for target selection prior to endosonographic guided tissue sampling[39] (Figure 4). The European guidelines[4] for the use of elastography in clinical practice suggest that EUS elastography adds information to the B-mode evaluation of LNs and can better guide an EUS-FNA procedure by identifying stiffer and thus, most suspicious regions for malignant infiltration.
Figure 4.
Endoscopic ultrasound elastography adds information to the B-mode evaluation of lymph nodes and can better guide a fine needle aspiration procedure by identifying stiffer (blue in the image) and thus, most suspicious regions for malignant infiltration. Arrow indicates needle tip.
Subepithelial masses
Imaging the layers of the GI tract is one of the major indications of the EUS examination[30]. EUS with high-frequency transducers of at least 7 MHz is used to improve visualization of wall layers, thickened bowel walls and target lesions. In the case of subepithelial masses, EUS elastography can provide information on stiffness, which may help increase the diagnostic confidence and accuracy of the staging. So far, there have been only few reports concerning the use of EUS elastography in characterizing subepithelial masses[62-64].
On B-mode EUS, the characteristics of benign subepithelial masses include (1) specific layer location (in the case of lipoma); (2) size smaller than 3 cm; (3) a smooth contour; (4) uniform echogenicity; and (5) lack of infiltration signs. On EUS elastography, benign subepithelial masses usually are showing an intermediate stiffness with homogenous strain pattern[30,61,63-65]. During follow-up, they usually have little to no changes in regards to the aforementioned criteria. However, the detection of some degenerative changes makes the diagnosis of benignity very difficult[63].
Lipomas are the most common subepithelial lesions. On EUS elastography, they are usually homogenously soft but occasionally, stiffer lipoma may also occur[1,30,63].
Malignant subepithelial masses have the following B-mode EUS criteria: (1) size > 3-4 cm; (2) an irregular contour or ulceration; (3) heterogeneous structure; and (4) LNs infiltration[30]. They usually show a heterogeneously stiff pattern on EUS elastography[63,64] (Figure 5).
Figure 5.
Gastric carcinoma is shown as heterogeneously stiff pattern (blue) on endoscopic ultrasound elastography.
Gastrointestinal stromal tumors (GISTs) are difficult cases. EUS elastography does not currently provide a good enough resolution to properly assess the microfoci found in GISTs[30,63] (Figure 6).
Figure 6.
Gastrointestinal stromal tumor is revealed heterogeneous hard (blue) pattern on endoscopic ultrasound elastography.
EMERGENT INDICATIONS AND FUTURE PERSPECTIVES
Fecal incontinence
The anal canal has the same layered structure as the rest of the GI tract and different layers have different elasticities, which is shown as different color patterns of each layer on elastography[1,66]. Allgayer et al[66] evaluated the elastography of anal sphincters in 50 patients with fecal incontinence, and found that the inner anal sphincter and external anal sphincter had different elastographical color distributions. However, there was no significant correlation between the elastographic appearance of sphincters and the functional and clinical parameters of the patients. Therefore, EUS elastography may not yield additional information in patients with fecal incontinence.
Liver
Although transcutaneous ultrasound elastography has been established as a modality for assessing the stiffness of liver tissue and even of focal liver lesions[67,68], there is still a lack of data on the use of EUS elastography for the liver. A possible reason is that EUS can usually only image the left liver lobe but not the entire organ, which limits its application for the liver. Our previous publications have briefly described the use of EUS elastography for the detection and differentiation of superficial liver tumors in the left liver lobe[1,3].
Biliary tract
Less data has been published concerning the use of EUS elastography for the diagnosis of disorders of the biliary tract[44]. Choledocholithiasis, chronic inflammatory or sclerosing processes may cause stiffness of the bile duct walls[30]. Our previous paper has reported that biliary papillomatosis showed a homogenously hard pattern of the distal stenosis when the mass infiltrates beyond the wall and the stenosis caused is severe[44].
Adrenal glands
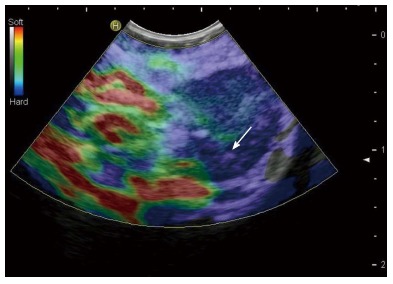
The left adrenal gland is anatomically located near the posterior gastric body wall, and thus it can be visualized using EUS in almost every case[69,70]. However, the right adrenal gland can be visualized more readily using the transcutaneous route[30,69-72]. Studies regarding EUS-FNAB found that EUS-FNAB provided an accurate diagnosis of adrenal metastasis[73]. No studies have been published regarding the use of EUS elastography in differentiating malignant adrenal masses from benign ones, except few reports[1,3,36,65,74] (Figure 7). Malignant infiltrations tend to be stiffer than benign tumors, inflammatory processes and fatty deposits[30].
Figure 7.
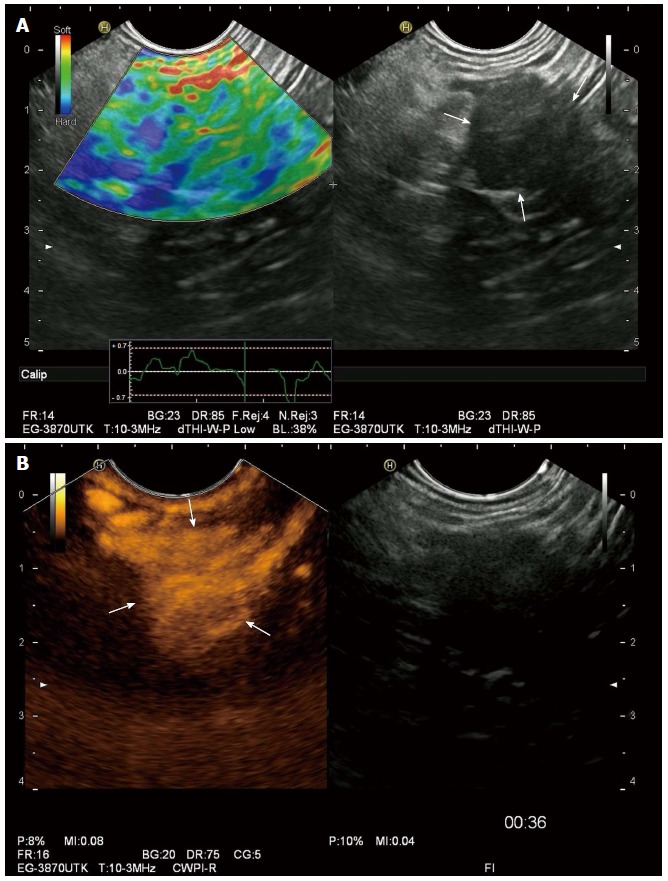
Benign adrenal gland tumor is typically soft (green) on endoscopic ultrasound elastography (A) and hyper-enhancing on contrast-enhanced endoscopic ultrasound (B).
Future perspective on techniques
Shear wave elastography, including acoustic radiation force impulse imaging and supersonic shear wave imaging, has been proven useful in assessing the stiffness of breast lesions, thyroid lesions and liver fibrosis[4,5,68]. However, this technique is still not available with an endoscope. Supersonic shear wave imaging has been already equipped on the transrectal ultrasound transducers, and its usefulness in the distinction of benign and malignant prostate lesions has been published[75]. It is expected that shear wave elastography could be also available on an endoscope, which would provide a new way to assess the stiffness of pancreatic masses and adjacent LNs, etc.
LIMITATIONS
The limitations of EUS elastography are the following: (1) both qualitative and quantitative methods are observer-dependent with operator bias in the selection of ROI and areas for analysis, which could cause intra- and inter-observer variability; (2) it is difficult to control the tissue compression by the endosonographer, and excessive pressure applied to the tissues can artificially increase their strain; (3) since a high-frequency transducer is used in the EUS elastography, the depth of penetration is limited, thus only the organ or part of the organ near the GI tract can be imaged; (4) presence of motion artifacts; (5) the strain value can be impacted by the vessels, cysts and bones in the selected ROI; and (6) the strain value may be also impacted if there is insufficient surrounding “normal tissue” as reference in the ROI, thus, the SR method may be occasionally unavailable due to this issue[47]. Other limitations include that EUS elastography needs more training and costs more time in procedure than conventional US elastography.
CONCLUSION
As a minimally invasive method, EUS plays an important role in assessing malignancies of the GI tract and nearby organs. Elastography adds valuable information to EUS by providing a qualitative and quantitative evaluation of tissue stiffness, thus reflecting the malignant or benign nature of the disease. Pancreas and LNs are the two most investigated organs with EUS elastography. Both qualitative and quantitative techniques have been proven useful in the differentiation between benign and malignant solid pancreatic masses and lymph nodes, and differentiation between normal pancreatic tissues and chronic pancreatitis, all with a high accuracy. EUS elastography can be combined with other imaging techniques, such as CE-EUS, which may be helpful to further improve the accuracy of EUS assessment.
EUS elastography is currently not ready to replace EUS-FNAB in any of its indications. However, EUS elastography may be useful for making clinical decisions, such as whether biopsies are necessary for a patient, which LNs are most likely to be malignant and thus selected for biopsy. In addition, a suspicious finding on EUS elastography can be helpful for guiding further clinical management when EUS-FNAB is inconclusive or negative.
Few publications have suggested that EUS elastography may be also useful to identify the hard (most likely to be malignant) areas within the pancreatic masses and lymph nodes for targeted EUS-FNAB. However, future studies are needed to further define the role of EUS elastography in this indication.
Emergent indications include the use of EUS elastography for the characterization of lesions located in the liver, biliary tract, adrenal glands, and GI tract. Still, additional evidence is required to define the role of EUS elastography in these clinical applications. Future perspectives also include monitoring treatment response in antiangiogenic therapy with elastography technique and application of EUS elastography in pediatric patients[76] and adequate reimbursement[77].
ACKNOWLEDGMENTS
The authors acknowledge Bad Mergentheimer Leberzentrum e.V. for supporting Dr. Xin-Wu Cui.
Footnotes
Conflict-of-interest statement: We declare that we do not have anything to disclose regarding funding or conflict of interest with respect to this manuscript.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: March 2, 2015
First decision: July 13, 2015
Article in press: September 30, 2015
P- Reviewer: Velayos B S- Editor: Ma YJ L- Editor: Filopodia E- Editor: Ma S
References
- 1.Dietrich CF. Real-time tissue elastography. Multiple clinical applications. Multiple clinical solutions. Endo Heute. 2011;24:177–212. [Google Scholar]
- 2.Dietrich CF. [Elastography, the new dimension in ultrasonography] Praxis (Bern 1994) 2011;100:1533–1542. doi: 10.1024/1661-8157/a000735. [DOI] [PubMed] [Google Scholar]
- 3.Dietrich CF. Echtzeit-Gewebeelastographie. Anwendungsmöglichkeiten nicht nur im Gastrointestinaltrakt. Endo Heute. 2011;23:177–212. [Google Scholar]
- 4.Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, Klauser AS, Sporea I, Calliada F, Cantisani V, et al. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: Clinical applications. Ultraschall Med. 2013;34:238–253. doi: 10.1055/s-0033-1335375. [DOI] [PubMed] [Google Scholar]
- 5.Bamber J, Cosgrove D, Dietrich CF, Fromageau J, Bojunga J, Calliada F, Cantisani V, Correas JM, D’Onofrio M, Drakonaki EE, et al. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 1: Basic principles and technology. Ultraschall Med. 2013;34:169–184. doi: 10.1055/s-0033-1335205. [DOI] [PubMed] [Google Scholar]
- 6.Giovannini M, Hookey LC, Bories E, Pesenti C, Monges G, Delpero JR. Endoscopic ultrasound elastography: the first step towards virtual biopsy? Preliminary results in 49 patients. Endoscopy. 2006;38:344–348. doi: 10.1055/s-2006-925158. [DOI] [PubMed] [Google Scholar]
- 7.Janssen J, Schlörer E, Greiner L. EUS elastography of the pancreas: feasibility and pattern description of the normal pancreas, chronic pancreatitis, and focal pancreatic lesions. Gastrointest Endosc. 2007;65:971–978. doi: 10.1016/j.gie.2006.12.057. [DOI] [PubMed] [Google Scholar]
- 8.Săftoiu A, Vilmann P, Gorunescu F, Gheonea DI, Gorunescu M, Ciurea T, Popescu GL, Iordache A, Hassan H, Iordache S. Neural network analysis of dynamic sequences of EUS elastography used for the differential diagnosis of chronic pancreatitis and pancreatic cancer. Gastrointest Endosc. 2008;68:1086–1094. doi: 10.1016/j.gie.2008.04.031. [DOI] [PubMed] [Google Scholar]
- 9.Iglesias-Garcia J, Larino-Noia J, Abdulkader I, Forteza J, Dominguez-Munoz JE. Quantitative endoscopic ultrasound elastography: an accurate method for the differentiation of solid pancreatic masses. Gastroenterology. 2010;139:1172–1180. doi: 10.1053/j.gastro.2010.06.059. [DOI] [PubMed] [Google Scholar]
- 10.Itoh A, Ueno E, Tohno E, Kamma H, Takahashi H, Shiina T, Yamakawa M, Matsumura T. Breast disease: clinical application of US elastography for diagnosis. Radiology. 2006;239:341–350. doi: 10.1148/radiol.2391041676. [DOI] [PubMed] [Google Scholar]
- 11.Cochlin DL, Ganatra RH, Griffiths DF. Elastography in the detection of prostatic cancer. Clin Radiol. 2002;57:1014–1020. doi: 10.1053/crad.2002.0989. [DOI] [PubMed] [Google Scholar]
- 12.Friedrich-Rust M, Ong MF, Martens S, Sarrazin C, Bojunga J, Zeuzem S, Herrmann E. Performance of transient elastography for the staging of liver fibrosis: a meta-analysis. Gastroenterology. 2008;134:960–974. doi: 10.1053/j.gastro.2008.01.034. [DOI] [PubMed] [Google Scholar]
- 13.Thomas A, Kümmel S, Gemeinhardt O, Fischer T. Real-time sonoelastography of the cervix: tissue elasticity of the normal and abnormal cervix. Acad Radiol. 2007;14:193–200. doi: 10.1016/j.acra.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 14.Lyshchik A, Higashi T, Asato R, Tanaka S, Ito J, Mai JJ, Pellot-Barakat C, Insana MF, Brill AB, Saga T, et al. Thyroid gland tumor diagnosis at US elastography. Radiology. 2005;237:202–211. doi: 10.1148/radiol.2363041248. [DOI] [PubMed] [Google Scholar]
- 15.Sãftoiu A, Gheonea DI, Ciurea T. Hue histogram analysis of real-time elastography images for noninvasive assessment of liver fibrosis. AJR Am J Roentgenol. 2007;189:W232–W233. doi: 10.2214/AJR.07.2571. [DOI] [PubMed] [Google Scholar]
- 16.Dye CE, Waxman I. Endoscopic ultrasound. Gastroenterol Clin North Am. 2002;31:863–879. doi: 10.1016/s0889-8553(02)00031-6. [DOI] [PubMed] [Google Scholar]
- 17.Tamerisa R, Irisawa A, Bhutani MS. Endoscopic ultrasound in the diagnosis, staging, and management of gastrointestinal and adjacent malignancies. Med Clin North Am. 2005;89:139–158, viii. doi: 10.1016/j.mcna.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 18.Byrne MF, Jowell PS. Gastrointestinal imaging: endoscopic ultrasound. Gastroenterology. 2002;122:1631–1648. doi: 10.1053/gast.2002.33576. [DOI] [PubMed] [Google Scholar]
- 19.Hocke M, Ignee A, Dietrich CF. Advanced endosonographic diagnostic tools for discrimination of focal chronic pancreatitis and pancreatic carcinoma--elastography, contrast enhanced high mechanical index (CEHMI) and low mechanical index (CELMI) endosonography in direct comparison. Z Gastroenterol. 2012;50:199–203. doi: 10.1055/s-0031-1281824. [DOI] [PubMed] [Google Scholar]
- 20.Săftoiu A, Vilmann P, Gorunescu F, Janssen J, Hocke M, Larsen M, Iglesias-Garcia J, Arcidiacono P, Will U, Giovannini M, et al. Accuracy of endoscopic ultrasound elastography used for differential diagnosis of focal pancreatic masses: a multicenter study. Endoscopy. 2011;43:596–603. doi: 10.1055/s-0030-1256314. [DOI] [PubMed] [Google Scholar]
- 21.Itokawa F, Itoi T, Sofuni A, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Umeda J, Tanaka R, et al. EUS elastography combined with the strain ratio of tissue elasticity for diagnosis of solid pancreatic masses. J Gastroenterol. 2011;46:843–853. doi: 10.1007/s00535-011-0399-5. [DOI] [PubMed] [Google Scholar]
- 22.Săftoiu A, Iordache SA, Gheonea DI, Popescu C, Maloş A, Gorunescu F, Ciurea T, Iordache A, Popescu GL, Manea CT. Combined contrast-enhanced power Doppler and real-time sonoelastography performed during EUS, used in the differential diagnosis of focal pancreatic masses (with videos) Gastrointest Endosc. 2010;72:739–747. doi: 10.1016/j.gie.2010.02.056. [DOI] [PubMed] [Google Scholar]
- 23.Xu W, Shi J, Zeng X, Li X, Xie WF, Guo J, Lin Y. EUS elastography for the differentiation of benign and malignant lymph nodes: a meta-analysis. Gastrointest Endosc. 2011;74:1001–1009; quiz 1115.e1-1115.e4. doi: 10.1016/j.gie.2011.07.026. [DOI] [PubMed] [Google Scholar]
- 24.Janssen J, Dietrich CF, Will U, Greiner L. Endosonographic elastography in the diagnosis of mediastinal lymph nodes. Endoscopy. 2007;39:952–957. doi: 10.1055/s-2007-966946. [DOI] [PubMed] [Google Scholar]
- 25.Popescu A, Săftoiu A. Can elastography replace fine needle aspiration? Endosc Ultrasound. 2014;3:109–117. doi: 10.4103/2303-9027.123009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hawes RH. Indications for EUS-directed FNA. Endoscopy. 1998;30 Suppl 1:A155–A157. doi: 10.1055/s-2007-1001503. [DOI] [PubMed] [Google Scholar]
- 27.Chong A, Venugopal K, Segarajasingam D, Lisewski D. Tumor seeding after EUS-guided FNA of pancreatic tail neoplasia. Gastrointest Endosc. 2011;74:933–935. doi: 10.1016/j.gie.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 28.Topazian M. Endoscopic ultrasonography in the evaluation of indeterminate biliary strictures. Clin Endosc. 2012;45:328–330. doi: 10.5946/ce.2012.45.3.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yasuda K. Imaging alone is sufficient in most circumstances--making the case for limited need for FNA. Gastrointest Endosc. 2009;69:S155–S156. doi: 10.1016/j.gie.2008.12.039. [DOI] [PubMed] [Google Scholar]
- 30.Dietrich CF, Săftoiu A, Jenssen C. Real time elastography endoscopic ultrasound (RTE-EUS), a comprehensive review. Eur J Radiol. 2014;83:405–414. doi: 10.1016/j.ejrad.2013.03.023. [DOI] [PubMed] [Google Scholar]
- 31.Yamao K, Sawaki A, Mizuno N, Shimizu Y, Yatabe Y, Koshikawa T. Endoscopic ultrasound-guided fine-needle aspiration biopsy (EUS-FNAB): past, present, and future. J Gastroenterol. 2005;40:1013–1023. doi: 10.1007/s00535-005-1717-6. [DOI] [PubMed] [Google Scholar]
- 32.Erickson RA. EUS-guided FNA. Gastrointest Endosc. 2004;60:267–279. doi: 10.1016/s0016-5107(04)01529-9. [DOI] [PubMed] [Google Scholar]
- 33.Iglesias-Garcia J, Lindkvist B, Lariño-Noia J, Domínguez-Muñoz JE. Endoscopic ultrasound elastography. Endosc Ultrasound. 2012;1:8–16. doi: 10.7178/eus.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Giovannini M, Thomas B, Erwan B, Christian P, Fabrice C, Benjamin E, Geneviève M, Paolo A, Pierre D, Robert Y, et al. Endoscopic ultrasound elastography for evaluation of lymph nodes and pancreatic masses: a multicenter study. World J Gastroenterol. 2009;15:1587–1593. doi: 10.3748/wjg.15.1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hirche TO, Ignee A, Barreiros AP, Schreiber-Dietrich D, Jungblut S, Ott M, Hirche H, Dietrich CF. Indications and limitations of endoscopic ultrasound elastography for evaluation of focal pancreatic lesions. Endoscopy. 2008;40:910–917. doi: 10.1055/s-2008-1077726. [DOI] [PubMed] [Google Scholar]
- 36.Saftoiu A, Vilman P. Endoscopic ultrasound elastography-- a new imaging technique for the visualization of tissue elasticity distribution. J Gastrointestin Liver Dis. 2006;15:161–165. [PubMed] [Google Scholar]
- 37.Dietrich CF, Jenssen C, Allescher HD, Hocke M, Barreiros AP, Ignee A. [Differential diagnosis of pancreatic lesions using endoscopic ultrasound] Z Gastroenterol. 2008;46:601–617. doi: 10.1055/s-2008-1027523. [DOI] [PubMed] [Google Scholar]
- 38.Iglesias-Garcia J, Larino-Noia J, Abdulkader I, Forteza J, Dominguez-Munoz JE. EUS elastography for the characterization of solid pancreatic masses. Gastrointest Endosc. 2009;70:1101–1108. doi: 10.1016/j.gie.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 39.Jenssen C, Dietrich CF. Endoscopic ultrasound-guided fine-needle aspiration biopsy and trucut biopsy in gastroenterology - An overview. Best Pract Res Clin Gastroenterol. 2009;23:743–759. doi: 10.1016/j.bpg.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 40.Havre RF, Elde E, Gilja OH, Odegaard S, Eide GE, Matre K, Nesje LB. Freehand real-time elastography: impact of scanning parameters on image quality and in vitro intra- and interobserver validations. Ultrasound Med Biol. 2008;34:1638–1650. doi: 10.1016/j.ultrasmedbio.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 41.Dietrich CF, Hirche TO, Ott M, Ignee A. Real-time tissue elastography in the diagnosis of autoimmune pancreatitis. Endoscopy. 2009;41:718–720. doi: 10.1055/s-0029-1214866. [DOI] [PubMed] [Google Scholar]
- 42.Schrader H, Wiese M, Ellrichmann M, Belyaev O, Uhl W, Tannapfel A, Schmidt W, Meier J. Diagnostic value of quantitative EUS elastography for malignant pancreatic tumors: relationship with pancreatic fibrosis. Ultraschall Med. 2012;33:E196–E201. doi: 10.1055/s-0031-1273256. [DOI] [PubMed] [Google Scholar]
- 43.Giovannini M. Endoscopic ultrasound elastography. Pancreatology. 2011;11 Suppl 2:34–39. doi: 10.1159/000323496. [DOI] [PubMed] [Google Scholar]
- 44.Cui XW, Ignee A, Braden B, Woenckhaus M, Dietrich CF. Biliary papillomatosis and new ultrasound imaging modalities. Z Gastroenterol. 2012;50:226–231. doi: 10.1055/s-0031-1281967. [DOI] [PubMed] [Google Scholar]
- 45.Lee TH, Cha SW, Cho YD. EUS elastography: advances in diagnostic EUS of the pancreas. Korean J Radiol. 2012;13 Suppl 1:S12–S16. doi: 10.3348/kjr.2012.13.S1.S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hu DM, Gong TT, Zhu Q. Endoscopic ultrasound elastography for differential diagnosis of pancreatic masses: a meta-analysis. Dig Dis Sci. 2013;58:1125–1131. doi: 10.1007/s10620-012-2428-5. [DOI] [PubMed] [Google Scholar]
- 47.Mei M, Ni J, Liu D, Jin P, Sun L. EUS elastography for diagnosis of solid pancreatic masses: a meta-analysis. Gastrointest Endosc. 2013;77:578–589. doi: 10.1016/j.gie.2012.09.035. [DOI] [PubMed] [Google Scholar]
- 48.Li X, Xu W, Shi J, Lin Y, Zeng X. Endoscopic ultrasound elastography for differentiating between pancreatic adenocarcinoma and inflammatory masses: a meta-analysis. World J Gastroenterol. 2013;19:6284–6291. doi: 10.3748/wjg.v19.i37.6284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gheonea DI, Săftoiu A. Beyond conventional endoscopic ultrasound: elastography, contrast enhancement and hybrid techniques. Curr Opin Gastroenterol. 2011;27:423–429. doi: 10.1097/MOG.0b013e328349cfab. [DOI] [PubMed] [Google Scholar]
- 50.Piscaglia F, Nolsøe C, Dietrich CF, Cosgrove DO, Gilja OH, Bachmann Nielsen M, Albrecht T, Barozzi L, Bertolotto M, Catalano O, et al. The EFSUMB Guidelines and Recommendations on the Clinical Practice of Contrast Enhanced Ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med. 2012;33:33–59. doi: 10.1055/s-0031-1281676. [DOI] [PubMed] [Google Scholar]
- 51.Iglesias-Garcia J, Domínguez-Muñoz JE, Castiñeira-Alvariño M, Luaces-Regueira M, Lariño-Noia J. Quantitative elastography associated with endoscopic ultrasound for the diagnosis of chronic pancreatitis. Endoscopy. 2013;45:781–788. doi: 10.1055/s-0033-1344614. [DOI] [PubMed] [Google Scholar]
- 52.Itoh Y, Itoh A, Kawashima H, Ohno E, Nakamura Y, Hiramatsu T, Sugimoto H, Sumi H, Hayashi D, Kuwahara T, et al. Quantitative analysis of diagnosing pancreatic fibrosis using EUS-elastography (comparison with surgical specimens) J Gastroenterol. 2014;49:1183–1192. doi: 10.1007/s00535-013-0880-4. [DOI] [PubMed] [Google Scholar]
- 53.Cui XW, Jenssen C, Saftoiu A, Ignee A, Dietrich CF. New ultrasound techniques for lymph node evaluation. World J Gastroenterol. 2013;19:4850–4860. doi: 10.3748/wjg.v19.i30.4850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Janssen J. [(E)US elastography: current status and perspectives] Z Gastroenterol. 2008;46:572–579. doi: 10.1055/s-2008-1027379. [DOI] [PubMed] [Google Scholar]
- 55.Bhutani MS, Hawes RH, Hoffman BJ. A comparison of the accuracy of echo features during endoscopic ultrasound (EUS) and EUS-guided fine-needle aspiration for diagnosis of malignant lymph node invasion. Gastrointest Endosc. 1997;45:474–479. doi: 10.1016/s0016-5107(97)70176-7. [DOI] [PubMed] [Google Scholar]
- 56.Săftoiu A, Vilmann P, Hassan H, Gorunescu F. Analysis of endoscopic ultrasound elastography used for characterisation and differentiation of benign and malignant lymph nodes. Ultraschall Med. 2006;27:535–542. doi: 10.1055/s-2006-927117. [DOI] [PubMed] [Google Scholar]
- 57.Săftoiu A, Vilmann P, Ciurea T, Popescu GL, Iordache A, Hassan H, Gorunescu F, Iordache S. Dynamic analysis of EUS used for the differentiation of benign and malignant lymph nodes. Gastrointest Endosc. 2007;66:291–300. doi: 10.1016/j.gie.2006.12.039. [DOI] [PubMed] [Google Scholar]
- 58.Knabe M, Günter E, Ell C, Pech O. Can EUS elastography improve lymph node staging in esophageal cancer? Surg Endosc. 2013;27:1196–1202. doi: 10.1007/s00464-012-2575-y. [DOI] [PubMed] [Google Scholar]
- 59.Paterson S, Duthie F, Stanley AJ. Endoscopic ultrasound-guided elastography in the nodal staging of oesophageal cancer. World J Gastroenterol. 2012;18:889–895. doi: 10.3748/wjg.v18.i9.889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Larsen MH, Fristrup C, Hansen TP, Hovendal CP, Mortensen MB. Endoscopic ultrasound, endoscopic sonoelastography, and strain ratio evaluation of lymph nodes with histology as gold standard. Endoscopy. 2012;44:759–766. doi: 10.1055/s-0032-1309817. [DOI] [PubMed] [Google Scholar]
- 61.Dietrich CF. Endoscopic ultrasound. An introductory manual and atlas. 2nd ed. Stuttgart: Thieme; 2011. [Google Scholar]
- 62.Kocaman O, Sentürk H, Danalıoğlu A, Türkdoğan K, Arabacı E, Yıldız K, Ince AT. Endosonography and elastography in the diagnosis of esophageal tuberculosis. Turk J Gastroenterol. 2013;24:290–291. doi: 10.4318/tjg.2013.0488. [DOI] [PubMed] [Google Scholar]
- 63.Jenssen C, Dietrich CF. Endoscopic ultrasound of gastrointestinal subepithelial lesions. Ultraschall Med. 2008;29:236–256; quiz 257-264. doi: 10.1055/s-2008-1027388. [DOI] [PubMed] [Google Scholar]
- 64.Dietrich CF, Jenssen C, Hocke M, Cui XW, Woenckhaus M, Ignee A. Imaging of gastrointestinal stromal tumours with modern ultrasound techniques - a pictorial essay. Z Gastroenterol. 2012;50:457–467. doi: 10.1055/s-0031-1282076. [DOI] [PubMed] [Google Scholar]
- 65.Dietrich CF, Jenssen C. [Evidence based endoscopic ultrasound] Z Gastroenterol. 2011;49:599–621. doi: 10.1055/s-0029-1246021. [DOI] [PubMed] [Google Scholar]
- 66.Allgayer H, Ignee A, Dietrich CF. Endosonographic elastography of the anal sphincter in patients with fecal incontinence. Scand J Gastroenterol. 2010;45:30–38. doi: 10.3109/00365520903383251. [DOI] [PubMed] [Google Scholar]
- 67.Cui XW, Pirri C, Ignee A, De Molo C, Hirche TO, Schreiber-Dietrich DG, Dietrich CF. Measurement of shear wave velocity using acoustic radiation force impulse imaging is not hampered by previous use of ultrasound contrast agents. Z Gastroenterol. 2014;52:649–653. doi: 10.1055/s-0034-1366036. [DOI] [PubMed] [Google Scholar]
- 68.Cui XW, Friedrich-Rust M, De Molo C, Ignee A, Schreiber-Dietrich D, Dietrich CF. Liver elastography, comments on EFSUMB elastography guidelines 2013. World J Gastroenterol. 2013;19:6329–6347. doi: 10.3748/wjg.v19.i38.6329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jenssen C, Dietrich CF. [Ultrasound and endoscopic ultrasound of the adrenal glands] Ultraschall Med. 2010;31:228–247; quiz 248-50. doi: 10.1055/s-0029-1245449. [DOI] [PubMed] [Google Scholar]
- 70.Dietrich CF, Wehrmann T, Hoffmann C, Herrmann G, Caspary WF, Seifert H. Detection of the adrenal glands by endoscopic or transabdominal ultrasound. Endoscopy. 1997;29:859–864. doi: 10.1055/s-2007-1004322. [DOI] [PubMed] [Google Scholar]
- 71.Dietrich CF, Ignee A, Barreiros AP, Schreiber-Dietrich D, Sienz M, Bojunga J, Braden B. Contrast-enhanced ultrasound for imaging of adrenal masses. Ultraschall Med. 2010;31:163–168. doi: 10.1055/s-0028-1109357. [DOI] [PubMed] [Google Scholar]
- 72.Trojan J, Schwarz W, Sarrazin C, Thalhammer A, Vogl TJ, Dietrich CF. Role of ultrasonography in the detection of small adrenal masses. Ultraschall Med. 2002;23:96–100. doi: 10.1055/s-2002-25190. [DOI] [PubMed] [Google Scholar]
- 73.Uemura S, Yasuda I, Kato T, Doi S, Kawaguchi J, Yamauchi T, Kaneko Y, Ohnishi R, Suzuki T, Yasuda S, et al. Preoperative routine evaluation of bilateral adrenal glands by endoscopic ultrasound and fine-needle aspiration in patients with potentially resectable lung cancer. Endoscopy. 2013;45:195–201. doi: 10.1055/s-0032-1325988. [DOI] [PubMed] [Google Scholar]
- 74.Dietrich CF, Hocke M, Jenssen C. [Interventional endosonography] Ultraschall Med. 2011;32:8–22, quiz 23-25. doi: 10.1055/s-0029-1246017. [DOI] [PubMed] [Google Scholar]
- 75.Ahmad S, Cao R, Varghese T, Bidaut L, Nabi G. Transrectal quantitative shear wave elastography in the detection and characterisation of prostate cancer. Surg Endosc. 2013;27:3280–3287. doi: 10.1007/s00464-013-2906-7. [DOI] [PubMed] [Google Scholar]
- 76.Schreiber-Dietrich D, Dietrich CF. Contrast enhanced ultrasound (CEUS) and off-label use (in children) Ultraschall Med. 2012;33:295–296. doi: 10.1055/s-0032-1318769. [DOI] [PubMed] [Google Scholar]
- 77.Dietrich CF, Riemer-Hommel P. Challenges for the German Health Care System. Z Gastroenterol. 2012;50:557–572. doi: 10.1055/s-0032-1312742. [DOI] [PubMed] [Google Scholar]


