Abstract
Objectives
To evaluate the cost-effectiveness of the ST-segment elevation myocardial infarction (STEMI) network of Catalonia (Codi Infart).
Design
Cost-utility analysis.
Setting
The analysis was from the Catalonian Autonomous Community in Spain, with a population of about 7.5 million people.
Participants
Patients with STEMI treated within the autonomous community of Catalonia (Spain) included in the IAM CAT II-IV and Codi Infart registries.
Outcome measures
Costs included hospitalisation, procedures and additional personnel and were obtained according to the reperfusion strategy. Clinical outcomes were defined as 30-day avoided mortality and quality-adjusted life-years (QALYs), before (N=356) and after network implementation (N=2140).
Results
A substitution effect and a technology effect were observed; aggregate costs increased by 2.6%. The substitution effect resulted from increased use of primary coronary angioplasty, a relatively expensive procedure and a decrease in fibrinolysis. Primary coronary angioplasty increased from 31% to 89% with the network, and fibrinolysis decreased from 37% to 3%. Rescue coronary angioplasty declined from 11% to 4%, and no reperfusion from 21% to 4%. The technological effect was related to improvements in the percutaneous coronary intervention procedure that increased efficiency, reducing the average length of the hospital stay. Mean costs per patient decreased from €8306 to €7874 for patients with primary coronary angioplasty. Clinical outcomes in patients treated with primary coronary angioplasty did not change significantly, although 30-day mortality decreased from 7.5% to 5.6%. The incremental cost-effectiveness ratio resulted in an extra cost of €4355 per life saved (30-day mortality) and €495 per QALY. Below a cost threshold of €30 000, results were sensitive to variations in costs and outcomes.
Conclusions
The Catalan STEMI network (Codi Infart) is cost-efficient. Further studies are needed in geopolitical different scenarios.
Keywords: HEALTH ECONOMICS
Strengths and limitations of this study.
The ST-segment elevation myocardial infarction (STEMI) guidelines recommend to develop regional networks to optimise their performance and improve clinical outcomes. Our study demonstrates that implementing the STEMI network in Catalonia was cost-efficient, and provides further strength to guideline recommendations.
The conclusions of our study are sensitive to several clinical and cost scenarios.
The lack of a prospective continuous registry of patients with acute coronary syndrome before the implementations of the network forced us to use two different data sources to evaluate clinical effectiveness.
There are limited clinical data in both registries to evaluate outcome measures.
Introduction
Acute myocardial infarction is one of the most frequent causes of death worldwide. Primary percutaneous coronary intervention (PCI), fibrinolysis or a combination of both are current therapies to treat patients with ST-segment elevation myocardial infarction (STEMI). Benefits of reperfusion treatment are time dependent1 and primary PCI is the treatment of choice for patients with STEMI when experienced providers can perform it within an expedited time frame.2 A systematic approach to logistical aspects and clinical protocols is mandatory. Clinical practice guidelines recommend regional STEMI networks in order to organise all key stakeholders2 so that patients can receive optimal and timely reperfusion treatment. Over the past years, the clinical benefits of STEMI networks have been clearly demonstrated.3–6
Although the economic cost of primary PCI compared with fibrinolysis has been evaluated,7 8 scarce data are available on the economic comparison of a STEMI network to the scenario without a network.9 Therefore, the aim of our study was to evaluate the short-term cost-effectiveness of two different scenarios for the treatment of STEMI in Catalonia: before and after the implementation of the regional STEMI network.
Methods
STEMI network and registries in Catalonia
Catalonia is an autonomous community in the northeast part of Spain with a population of approximately 7 500 000. In June 2009, a regional STEMI network was introduced,10 11 with a standardised transfer protocol for patients with STEMI. The network divided Catalonia into referral areas for the 10 pre-existing PCI-equipped hospitals. There was no need to invest in new infrastructure or PCI centres to implement the network.
The Catalan STEMI network (Codi Infart) includes four components: (1) Emergency Medical Services (EMS) ambulances staffed with physicians or nurses able to diagnose symptoms, interpret an ECG, select the reperfusion strategy, and administer fibrinolytic therapy; (2) the EMS dispatch centre that coordinates the logistics between the ambulances or community hospitals and the primary PCI hospitals; (3) the 10 primary PCI hospitals, 5 of them with 24/7 availability and (4) inclusion of all patients treated within the network in a prospective registry (Catalonian STEMI network registry).
The protocol dictates that once a healthcare professional diagnoses a patient with STEMI, the network is activated and the reperfusion strategy is selected according to standard guidelines. If primary PCI is selected as the reperfusion strategy, the patient is transferred to the nearest primary PCI centre; once the patient is clinically stable, he or she is transported to the reference centre to avoid oversaturation of PCI centres. Patients treated with fibrinolysis are transferred to a PCI centre immediately in any case of failed fibrinolysis or otherwise for elective coronary angiography.
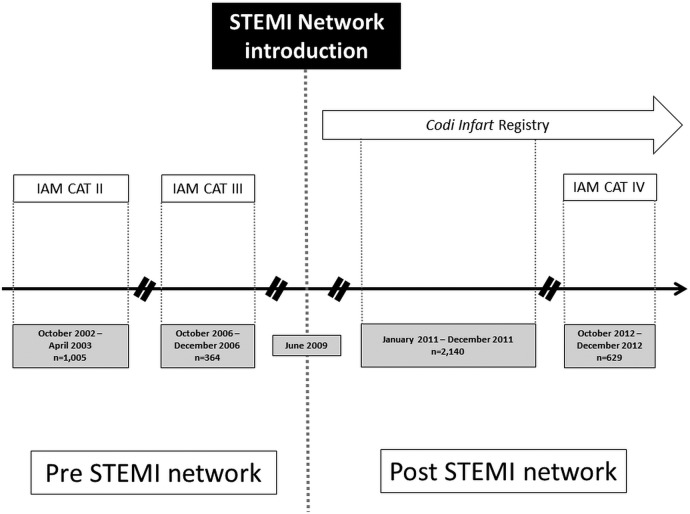
IAM CAT II-IV and Catalonian STEMI network (Codi Infart) were used to evaluate the demographic and clinical data and 30-day mortality before and after the implementation of the network. To evaluate the distribution of reperfusion therapies for both periods, IAM CAT II, III and IV registries were used. Reperfusion therapy distribution for the period after the network implementation was obtained from the IAM CAT IV registry and not from the Catalonian STEMI network (Codi Infart) registry in order to avoid selection bias, as all patients admitted in Catalonian hospitals with an acute coronary syndrome were prospectively included in the IAM CAT IV registry, and not only those treated within the network who were included in the Codi Infart registry. The specific methodology of the IAM CAT and Codi Infart registries is described elsewhere.11–13 The Catalonian STEMI network (Codi Infart) registry includes demographic, clinical and procedural data, and 30-day mortality from patients treated within the network. All registries were in accordance with the institutional ethics committee of each participating centre, and all patients gave informed written consent for the procedures. The main characteristics of the registries are depicted in table 1.
Table 1.
Source of data
| Type of registry | Inclusion period | Centres | Inclusion criteria | Sample size (STEMI) | STEMI reperfusion strategy | Data extracted for analysis | Follow-up (30-days) | |
|---|---|---|---|---|---|---|---|---|
| IAM CAT II | Snapshot | October 2002–April 2003 | 27 | Patients with STEMI with fibrinolysis or primary PCI indication | 1005 | Primary PCI 10.2% Rescue PCI NA Fibrinolysis 62.5% No reperfusion 27.3% |
|
98% (985/1005) |
| IAM CAT III | Snapshot | October 2006 –December 2006 | 22 | Acute coronary syndrome | 364 | Primary PCI 31% Rescue PCI 11% Fibrinolysis 37% No Reperfusion 21% |
|
100% |
| IAM CAT IV | Snapshot | October 2012 –December 2012 | 42 | Acute coronary syndrome | 629 | Primary PCI 88.5% Rescue PCI 3% Fibrinolysis 3.9% No Reperfusion 4.6% |
|
100% |
| Codi Infart Registry | Continuous registry | January 2011–December 2011 | 10 | Patients with STEMI | 2140 | Primary PCI 86.2% Rescue PCI 4.2% Fibrinolysis 3.6% No Reperfusion 6% |
|
94% (2140/2269) |
*Sample size refers to confirmed patients with STEMI included in the registries.
NA, not applicable; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction.
Economic evaluation
We compared the results of the procedure used to treat patients with STEMI before and after implementation of the regional network. In addition to comparing health improvements measured as lives saved, we took into account secondary measures of quality of life in comparable circumstances. We obtained a ratio of cost variation per outcome unit and will refer to our analysis as a cost-effectiveness analysis. (Incremental cost-effectiveness ratio (ICER)=(costs with the protocol—costs without the protocol/effectiveness with the protocol—effectiveness without the protocol)). Sensitivity analysis was performed with information obtained from previously published data in order to evaluate different scenarios.
Cost assessment
Cost evaluation was divided into two components: (1) Hospitalisation costs and (2) Other costs. Net costs were defined as the difference in costs between both protocols. They were obtained by subtracting from the mean STEMI network costs the costs of treating patients with STEMI without the network. Mean costs per patient were calculated according to the reperfusion strategy selected (primary PCI, rescue PCI, fibrinolysis and no reperfusion). Differences in costs were secondary to materials, medications and hospital stay. Hospitalisation costs were calculated by multiplying the mean cost of 1 day of inpatient care by the average length of stay. The cost of 1 day of hospital care was obtained from the cognisant public agency, Central de Balanços,14 which provided an average cost for the analysed hospitals. The mean length of a single stay for the pre-network period was obtained for 2008 from one representative tertiary centre. Length of stay after implementation of the STEMI network was obtained from the IAM CAT IV registry. Other costs included supplies, devices, medication, salaries and wages and fixed costs. There was no need for infrastructure investments, so no extra costs were attributed to that. Marketed unit prices and other unit costs in 2012 were obtained from a single inpatient centre considered representative of the rest of the network hospitals. Costs were calculated per patient, and unit costs were kept invariable throughout the periods of analysis in order to avoid drawing any biased conclusions resulting only from price changes. Total cost per protocol was calculated as the sum of costs per patient per reperfusion strategy weighted by the percentage of patients treated in each reperfusion strategy.
Outcome measures
For the purpose of the study, effectiveness was defined as 30-day avoided mortality. The IAM CAT II-III registries were used to measure 30-day mortality for the pre-network period: IAM CAT II for patients treated with fibrinolysis and no reperfusion, and IAM CAT III for patients treated with primary PCI and rescue PCI. The Catalonian STEMI network registry was used for the period after the network was implemented (figure 1). To estimate quality-adjusted life-years (QALYs), it is necessary to quality adjust the period of time the patient is alive within the model using an appropriate utility or preference score. In the absence of data from the Catalonian registries, external estimates were used. The estimates applied in our study were based on the results from published data sets validated for patients with STEMI.7 EuroQol (EQ-5D) was the utility used to compute QALYs as a measure of self-perceived health status. For the first year of the non-event state, a weighted utility value was estimated on the basis that half of this period would be covered by the estimate derived for the first year after and half the period would be covered by the value for the post-myocardial infarction state. These estimated utility values were considered the most appropriate source for the model as they provide outcomes measured as QALYs according to the reperfusion strategy.
Figure 1.
Catalonian acute coronary syndrome registries used to extract outcome of patients with STEMI (30-day mortality) before and after the network implementation (STEMI, ST-segment elevation myocardial infarction).
Statistical analysis
Categorical variables were expressed as the total number and percentage and compared between groups with the χ2 test or Fisher test. Continuous variables were expressed as the mean and SD and compared between groups using the Student t test. Data were analysed with SPSS V.20.
Results
Clinical outcomes and reperfusion therapies
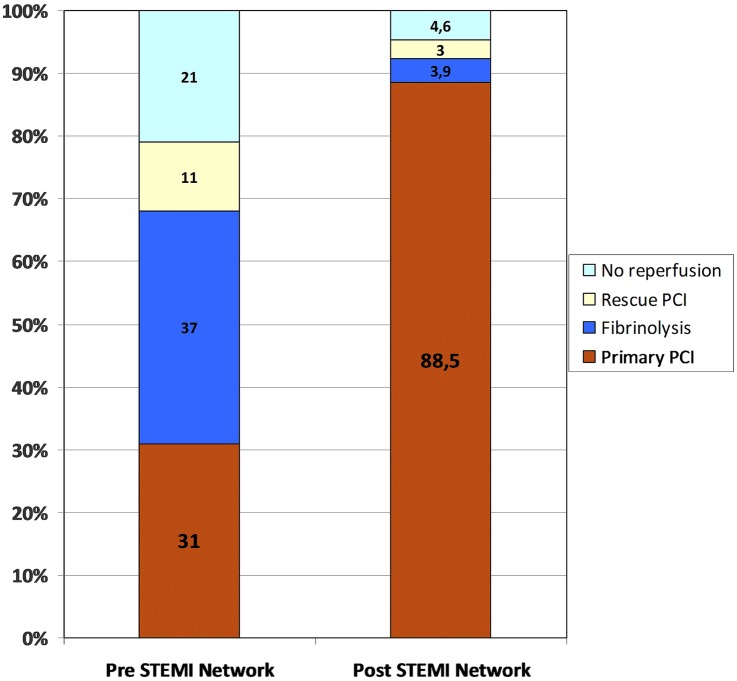
Clinical and demographic information is shown in table 2. The implementation of a STEMI network modified the distribution of procedures (figure 2), with a significant decrease in patients with STEMI treated with fibrinolysis (37% vs 3%; p<0.01), rescue PCI (11% vs 4%; p<0.01), and no reperfusion (21% vs 4%; p<0.01), against a significant increase in primary PCI (31% vs 89%; p<0.01). The rate of 30-day mortality in patients treated with primary PCI decreased from 7.7% to 5.6% (OR 0.69 95% CI 0.29 to 1.63), and the percentage of inpatients treated with rescue PCI decreased from 15.1% to 13.6% (OR 0.68; 95% CI 0.19 to 2.39) after the STEMI network was established (table 3).
Table 2.
Clinical characteristics
| Pre-STEMI network (n=367) | Post-STEMI network (n=2140) | p Value | |
|---|---|---|---|
| Age (years) | 65.0 (14.0) | 62.7 (13.5) | 0.23 |
| Sex (female) | 96 (26.2%) | 486 (22.7%) | 0.11 |
| Diabetes mellitus | 119 (33%) | 464 (22%) | 0.48 |
| Anterior MI | 158 (43%) | 882 (41%) | 0.22 |
| Cardiogenic shock at admission | 22 (6.0%) | 141 (6.6%) | 0.67 |
MI, myocardial infarction; STEMI, ST-segment elevation myocardial infarction.
Figure 2.
Reperfusion strategy distribution after the implementation of the STEMI network, showing a significant decrease in the proportion of patients treated with rescue PCI, fibrinolysis or non-reperfused and a significant increase in the proportion of patients treated with primary PCI (PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction).
Table 3.
Clinical parameters
| Pre-STEMI network (n=356)* | Post-STEMI network (n=2140)* | OR (95% CI) | |
|---|---|---|---|
| Primary PCI | (7.7%) | (5.6%) | 0.69 (0.29 to 1.63) |
| Fibrinolysis | (10.5%)* | (3.6%) | 0.46 (0.12 to 1.78) |
| Rescue PCI | (15.1%) | (13.6%) | 0.68 (0.19 to 2.39) |
| No reperfusion | (13.4%)* | (15.1%) | 1.27 (0.48 to 3.32) |
Mortality after 30 days of follow-up according to reperfusion strategy.
*N refers to the total number of patients included in the registry. Mortality rates were obtained from the total number of patients treated with each strategy.
†Mortality data for these patients were obtained from the IAM CAT II registry.
PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction.
Cost assessment
Fibrinolytic treatment generates the lowest mean inpatient expenditure. Rescue PCI is the most expensive, and primary PCI is the second highest. As a result of the substitution effect generated by the implementation of the STEMI network protocol, costs increased by €1656 per patient with STEMI, from €2284 to €3940. At the same time, however, improved efficiencies in the PCI procedure (which could be attributed to technology innovations and to increased operator experience) allowed for a decrease of €1458 per patient in hospital costs, from €5397 to €3939. The combined cost effect was a slight (2.6%) increase of €198 in mean costs of patients with STEMI, from €7681 to €7879. (Detailed cost information is shown in online supplementary material).
Cost-effectiveness ratio
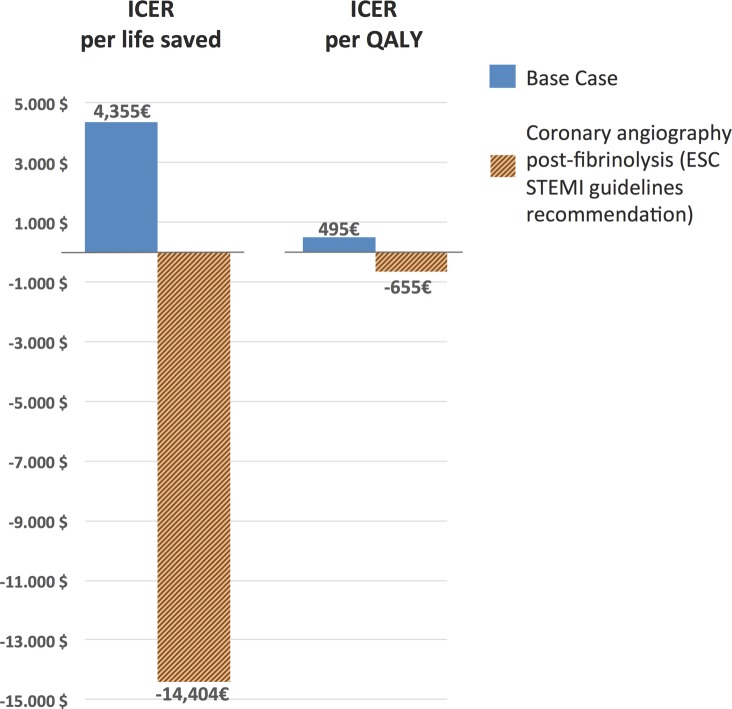
The ICER associated with the network was €4355 for each life saved as at the 30-day follow-up. Adjustment of the survival period by quality of life according to Bravo Vergel et al7 resulted in a cost-effectiveness ratio of €495 for each QALY. Cost and effectiveness values that were used to calculate the ICER are shown in table 4.
Table 4.
Cost and effectiveness assessment
| Panel A: Effectiveness assessment (30-day avoided mortality) |
||||||
|---|---|---|---|---|---|---|
| Pre-STEMI network |
Post-STEMI network |
|||||
| 30-Day mortality (%) (a) | Reperfusion strategy distribution (%) (b) | Weighted mortality (%) (c)=(a)*(b) | 30-Day mortality (%) (a) | Reperfusion strategy distribution (%) (b) | Weighted mortality (%) (c)=(a)*(b) | |
| Primary PCI | 7.7 | 31 | 2.39 | 5.6 | 88.5 | 4.96 |
| Fibrinolysis | 10.5 | 37 | 3.88 | 3.6 | 3.9 | 0.14 |
| Rescue PCI | 15.1 | 11 | 1.66 | 13.6 | 3 | 0.41 |
| No reperfusion | 13.4 | 21 | 2.81 | 15.1 | 4.6 | 0.69 |
| Protocol Effectiveness* |
89.2 | 93.8 | ||||
| Panel B: Costs assessment |
||||||
|---|---|---|---|---|---|---|
| Pre-STEMI network |
Post-STEMI network |
|||||
| Mean costs (€) (a) |
Reperfusion strategy distribution (%) (b) | Weighted costs (€) (c)=(a)*(b) |
Mean costs (€) (a) |
Reperfusion strategy distribution (%) (b) | Weighted costs (€) (c)=(a)*(b) |
|
| Primary PCI | 8306 | 31 | 2572.9 | 7874 | 88.5 | 6968.5 |
| Fibrinolysis | 5956 | 37 | 2203.7 | 5956 | 3.9 | 232.3 |
| Rescue PCI | 10 806 | 11 | 1188.7 | 10 086 | 3 | 302.6 |
| No reperfusion | 8160 | 21 | 1713.6 | 8160 | 4.6 | 375.4 |
| Protocol Cost (€) |
7680.8 | 7878.7 | ||||
*Protocol effectiveness=100-(Σ weighted mortality).
PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction.
Sensitivity analyses
Sensitivity analysis for the cost-effectiveness ratio, using previously published data on 30-day mortality and different cost scenarios, is shown in table 5. Also, we carry out a sensitivity analysis with the scenario of performing coronary angiography in all patients after being treated with fibrinolytics as recommended by current guidelines. With the previous scenario, the network would be cost-saving with an ICER of −€14 404 for each life saved as at the 30-day follow-up, and −€655 for each QALY (figure 3).
Table 5.
Cost-effectiveness and sensitivity analyses
| Control cost (€) | STEMI network cost (€) | Control 30-day mortality (%) | STEMI network 30-day mortality (%) | ICER*(€) mortality |
ICER* (€) QALYs |
|
|---|---|---|---|---|---|---|
| Scenario | ||||||
| Base case | 4355 | 495 | ||||
| Primary PCI | 8306 | 7874 | 7.7 | 5.6 | ||
| Fibrinolysis | 5956 | 5956 | 10.5 | 3.6 | ||
| Rescue PCI | 10 806 | 10 086 | 15.1 | 13.6 | ||
| No reperfusion | 8160 | 8160 | 13.4 | 15.1 | ||
| Alternative scenario | ||||||
| 30-day mortality | 2838 | 308 | ||||
| Primary PCI15 | 8306 | 7874 | 7.7 | 3.2 | ||
| Fibrinolysis16 | 5956 | 5956 | 10.5 | 6.2 | ||
| Rescue PCI17 | 10 806 | 10 086 | 15.1 | 6.2 | ||
| No reperfusion18 | 8160 | 8160 | 13.4 | 11.2 | ||
ICER calculated using different measures of effectiveness: mortality and QALYs, that is, €4355 for each additional life saved and €495 for each additional QALY.
ICER, incremental cost-effectiveness ratio; PCI, percutaneous coronary intervention; QALY, quality-adjusted life-year; STEMI, ST-segment elevation myocardial infarction.
Figure 3.
Sensitivity analysis. ICER modifications as a result of a sensitivity analysis with the scenario of performing coronary angiography within the next 24 h after fibrinolysis (ICER, incremental cost-effectiveness ratio; QALY, quality-adjusted life-year).
Discussion
The major findings of this study can be summarised as follows: (1) the STEMI network in Catalonia is efficient in the short term; (2) use of the STEMI network protocol increases the use of PCI, a more expensive treatment, but a large portion of the increased cost is offset by cost reduction associated with a shorter mean length of the hospital stay of the patient with STEMI; (3) in a sensitivity analysis that assumed that all patients underwent coronary angiography after being treated with fibrinolytics, the ICER was negative, saving €14 404 for each life as at the 30-day follow-up, and €655 for each QALY; (4) sensitivity analyses using previously published data for costs and 30-day mortality showed an ICER under the recommended threshold of €30 000,19
Before the implementation of the network, double antiplatelet therapy, β-blockers and statins were prescribed according to guidelines, with a compliance of 77%, 82% and 86%, respectively.13 The main change after the STEMI network started was organisational, with the establishment of prespecified protocols that permitted direct transfer of patients with a diagnosis of STEMI without the need for approval by the PCI centre. As a result, the distribution of reperfusion therapies changed significantly, with an increase in primary PCI and a decline in the use of fibrinolysis and in the need for rescue PCI in accordance with the guidelines. The STEMI network was associated with this major change in reperfusion strategies, as well as with a shorter hospital stay. The mean hospital stay was known to be shorter for patients treated with primary PCI, compared to other reperfusion therapies; implementation of the network further decreased the mean length of stay for patients treated with primary or rescue PCI, perhaps due to increased operator experience as well as continued technological improvements.
The increase of mortality in patients without reperfusion treatment observed after the protocol started might be secondary to the result of a selection bias. Before the network started, two factors were needed to take the decision to transfer a patient to the primary PCI centre: (1) Accessibility of a catheterisation laboratory outside ‘office hours’ and (2) delay from medical contact to reperfusion therapy. After the network started, the first factor was almost eliminated and the second factor was reduced significantly as the number of PCI centres with 24/7 increased. As a result, the rate of reperfusion increased up to 97%, meaning that almost all patients that present with a STEMI within the network receive some therapy either as a PCI or, to a lesser extent, fibrinolysis. This could imply that patients who were not treated with PCI or fibrinolysis are not candidates to reperfusion therapy because of futility or an extreme high risk.
There is scarce information regarding the cost-effectiveness of STEMI networks. The findings of our investigation are in concordance with Birkemeyer et al,9 who analysed the short-term cost-effectiveness of a STEMI network in Germany and concluded that it was within well-accepted boundaries. Two differences should be pointed out in comparison with the present study. First, the previous study was performed in a rural area that serves approximately 350 000 people with one high-volume primary PCI centre; our study covered a much larger and more varied (urban, suburban and rural) population. Our study compared mean cost per patient according to the reperfusion strategy, whereas the German study compared annual hospital reimbursement from the health services to the hospitals analysed.
Another earlier study in a large urban, suburban and rural region demonstrated that an EMS strategy of transporting all patients to existing PCI-capable hospitals was more effective and less costly than separate hospital-based strategies of new construction and staffing.20 Our analysis was performed in an area that was well staffed and equipped before the implementation of the STEMI network. In Catalonia, according to the Spanish Society of Cardiology registry, there was one PCI centre for every 736 409 inhabitants when the network was implemented in 2009,21 which is within the recommended boundaries.22 Although the study by Concannon et al is useful for those aiming to implement a network in a region without proper infrastructure, the main problem in Catalonia was organisational rather than structural: in 2008, there was no registry for all patients admitted with STEMI in Catalonia. However, in Spain, all patients discharged from hospital with a diagnosis of acute coronary syndrome are recorded in the National Statistics Institute database; the proportion of these patients with STEMI is approximately 38.9%.23 Given that patient discharge with a diagnosis of acute coronary syndrome in Catalonia was similar in 2008 and 2010 (8429 vs 8166), we can assume that the total number of patients admitted with an STEMI was also similar.
Current guidelines recommend that coronary angiography should be performed in all patients after treating them with fibrinolytics.2 In Catalonia, before implementing the STEMI network, not all patients treated with fibrinolytics were systematically transferred for elective coronary angiography. The Catalonian STEMI network protocol recommends transferring to a PCI centre for elective coronary angiography all patients treated with fibrinolytics. According to the Interventional Cardiology Working Group of the Spanish Society of Cardiology registry, the total number of PCIs, including elective and primary PCIs in Catalonia, did not vary significantly after the implementation of the network, suggesting that after implementing the network, the coronary angiography was performed early after the procedure, and as a result there might be an increase in the effectiveness of the network. We performed a sensitivity analysis using the previous scenario, and if all patients treated with fibrinolysis were transferred for coronary angiography as recommended by current guidelines, the network would be cost saving with an ICER of −€14 404 for each life saved as at the 30-day follow-up, and −€655 for each QALY.
The EMS system in Catalonia was well developed and equipped when the protocol started in 2009; they could perform and interpret a 12-lead ECG and treat with out-of-hospital fibrinolysis. EMS activity is regulated by a contract with the public health insurance provider (CatSalut), receiving a fixed yearly fee independent of the number of transports and with no automatic or specific annual EMS increase in the CatSalut budget. Even so, implementation of the network did not increase the number of emergency activations from 2008 to 2010 (801 676 vs 795 628).24
Several limitations of our study must be taken into account. First, the absence of a prospective continuous registry of patients with acute coronary syndrome before the implementation of the network forces us to use two different data sources to evaluate clinical effectiveness. Also, there are limited clinical data in both registries to evaluate outcome measures. Second, we lack knowledge about the number of false positive activations of the catheterisation laboratory before the implementation. Third, the results of this study cannot be generalised to all scenarios. This STEMI network was implemented in a community with a mature EMS system and without the need to add infrastructure. Finally, we could not perform a sensitivity analysis using the distribution of cost parameters to evaluate the uncertainty of our conclusions, as this information was unavailable.
Conclusions
The Catalan STEMI network (‘Codi Infart’) is cost-efficient. Further studies are needed in different geopolitical scenarios.
Acknowledgments
The authors would like to thank all participant centres of the Catalonian STEMI network (“Codi infart”).
Footnotes
Contributors: AR, JAG-H, AF-O, CM and MS conceived the study. AR, JAG-H, AF-O, CM, RT and MS obtained research funding. AR, VM-Y, AR, MTF, JAG-H, JF, AC, RS and MS supervised the data collection and undertook recruitment of participating centres. AR, JB and LP analysed the data. AR and JB drafted the manuscript and all authors contributed substantially to its revision. MS takes responsibility for the paper as a whole.
Funding: This work was partially supported by the Spanish Heart Foundation of the Spanish Society of Cardiology.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Terkelsen CJ, Sørensen JT, Maeng M et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA 2010;304:763–71. 10.1001/jama.2010.1139 [DOI] [PubMed] [Google Scholar]
- 2.Steg PG, James SK, Atar D et al. , Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC)1. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012;33:2569–619. 10.1093/eurheartj/ehs215 [DOI] [PubMed] [Google Scholar]
- 3.Kristensen SD, Fajadet J, Di Mario C et al. Implementation of primary angioplasty in Europe: stent for life initiative progress report. EuroIntervention 2012;8:35–42. 10.4244/EIJV8I1A7 [DOI] [PubMed] [Google Scholar]
- 4.Widimský P, Groch L, Zelízko M et al. Multicentre randomized trial comparing transport to primary angioplasty vs immediate thrombolysis vs combined strategy for patients with acute myocardial infarction presenting to a community hospital without a catheterization laboratory. The PRAGUE study Eur Heart J 2000;21:823–31. 10.1053/euhj.1999.1993 [DOI] [PubMed] [Google Scholar]
- 5.Khot UN, Johnson ML, Ramsey C et al. Emergency department physician activation of the catheterization laboratory and immediate transfer to an immediately available catheterization laboratory reduce door-to-balloon time in ST-elevation myocardial infarction. Circulation 2007;116:67–76. 10.1161/CIRCULATIONAHA.106.677401 [DOI] [PubMed] [Google Scholar]
- 6.Gómez-Hospital JA, Dallaglio PD, Sánchez-Salado JC et al. Impact on delay times and characteristics of patients undergoing primary percutaneous coronary intervention in the southern metropolitan area of Barcelona after implementation of the infarction code program. Rev Esp Cardiol 2012;65:911–18. 10.1016/j.recesp.2012.06.009 [DOI] [PubMed] [Google Scholar]
- 7.Bravo Vergel Y, Palmer S, Asseburg C et al. Is primary angioplasty cost effective in the UK? Results of a comprehensive decision analysis. Heart 2007;93:1238–43. 10.1136/hrt.2006.111401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wailoo A, Goodacre S, Sampson F et al. Primary angioplasty versus thrombolysis for acute ST-elevation myocardial infarction: an economic analysis of the National Infarct Angioplasty project. Heart 2010;96:668–72. 10.1136/hrt.2009.167130 [DOI] [PubMed] [Google Scholar]
- 9.Birkemeyer R, Dauch A, Müller A et al. Short term cost effectiveness of a regional myocardial infarction network. Health Econ Rev 2013;3:10 10.1186/2191-1991-3-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Regueiro A, Tresserras R, Goicolea J et al. Primary percutaneous coronary intervention: models of intervention in Spain. EuroIntervention 2012;8(Suppl P):P90–3. 10.4244/EIJV8SPA16 [DOI] [PubMed] [Google Scholar]
- 11.Bosch X, Curós A, Argimon JM et al. Modelo de intervención coronaria percutánea primaria en Cataluña. Rev Esp Cardiol 2011;11:51–60. [Google Scholar]
- 12.Figueras J, Masip J, Bruguera J et al. [II. Resultats del II Registre de l'infart agut de miocardi amb elevació del segment ST a Catalunya]. Rev Soc Catalana Cardiol 2005;5:298–310. [Google Scholar]
- 13.Figueras J, Heras M, Baigorri F et al. [III Catalan registry of ST elevation acute myocardial infarction. Comparison with former Catalan registries I and II from Catalonia, Spain]. Med Clin (Barc) 2009;133:694–701. 10.1016/j.medcli.2009.07.017 [DOI] [PubMed] [Google Scholar]
- 14.Generalitat de Catalunya G. Central de Balanços. http://observatorisalut.gencat.cat/ca/ (accessed 23 Apr 2015).
- 15.Puymirat E, Simon T, Steg PG et al. Association of changes in clinical characteristics and management with improvement in survival among patients with ST-elevation myocardial infarction. JAMA 2012;308:998–1006. 10.1001/2012.jama.11348 [DOI] [PubMed] [Google Scholar]
- 16.Van De Werf F, Adgey J, Ardissino D et al. , Assessment of the Safety and Efficacy of a New Thrombolytic (ASSENT-2) Investigators. Single-bolus tenecteplase compared with front-loaded alteplase in acute myocardial infarction: the ASSENT-2 double-blind randomised trial. Lancet 1999;354:716–22. 10.1016/S0140-6736(99)07403-6 [DOI] [PubMed] [Google Scholar]
- 17.Shugman IM, Hsieh V, Cheng S et al. Safety and efficacy of rescue angioplasty for ST-elevation myocardial infarction with high utilization rates of glycoprotein IIb/IIIa inhibitors. Am Heart J 2012;163:649–56.e1. 10.1016/j.ahj.2012.01.014 [DOI] [PubMed] [Google Scholar]
- 18.Cohen M, Gensini GF, Maritz F et al. Prospective evaluation of clinical outcomes after acute ST-elevation myocardial infarction in patients who are ineligible for reperfusion therapy: preliminary results from the TETAMI registry and randomized trial. Circulation 2003;108:III14–21. 10.1161/01.CIR.0000091832.74006.1C [DOI] [PubMed] [Google Scholar]
- 19.McCabe C, Claxton K, Culyer AJ. The NICE cost-effectiveness threshold: what it is and what that means. Pharmacoeconomics 2008;26:733–44. 10.2165/00019053-200826090-00004 [DOI] [PubMed] [Google Scholar]
- 20.Concannon TW, Kent DM, Normand SL et al. Comparative effectiveness of ST-segment-elevation myocardial infarction regionalization strategies. Circ Cardiovasc Qual Outcomes 2010;3:506–13. 10.1161/CIRCOUTCOMES.109.908541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Díaz de la Llera LS, Ballesteros S, Nevado J et al. Sirolimus-eluting stents compared with standard stents in the treatment of patients with primary angioplasty. Am Heart J 2007;154: 164.e1–6. 10.1016/j.ahj.2007.04.007 [DOI] [PubMed] [Google Scholar]
- 22.Knot J, Widimsky P, Wijns W et al. How to set up an effective national primary angioplasty network: lessons learned from five European countries. EuroIntervention 2009;5:299, 301–9. [PubMed] [Google Scholar]
- 23.Ferreira-González I, Permanyer-Miralda G, Marrugat J et al. , MASCARA study research team. MASCARA (Manejo del Síndrome Coronario Agudo. Registro Actualizado) study. General findings. Rev Esp Cardiol 2008;61:803–16. 10.1157/13124991 [DOI] [PubMed] [Google Scholar]
- 24.Generalitat de Catalunya. Departament de Salut. Memòries d'activitat anual del CatSalut. http://catsalut.gencat.cat/ca/coneix-catsalut/informes-memories-activitat/ma-anual-regions/ (accessed 23 Apr 2015).