Abstract:
Perfusion technology is a mechanical and visual science traditionally taught with didactic instruction combined with clinical experience. It is difficult to provide perfusion students the opportunity to experience difficult clinical situations, set up complex perfusion equipment, or observe corrective measures taken during catastrophic events because of patient safety concerns. Although high fidelity simulators offer exciting opportunities for future perfusion training, we explore the use of a less costly low fidelity form of simulation instruction, vicarious audiovisual learning. Two low fidelity modes of instruction; description with text and a vicarious, first person audiovisual production depicting the same content were compared. Students (n = 37) sampled from five North American perfusion schools were prospectively randomized to one of two online learning modules, text or video. These modules described the setup and operation of the MAQUET ROTAFLOW standalone centrifugal console and pump. Using a 10 question multiple-choice test, students were assessed immediately after viewing the module (test #1) and then again 2 weeks later (test #2) to determine cognition and recall of the module content. In addition, students completed a questionnaire assessing the learning preferences of today’s perfusion student. Mean test scores from test #1 for video learners (n = 18) were significantly higher (88.89%) than for text learners (n = 19) (74.74%), (p < .05). The same was true for test #2 where video learners (n = 10) had an average score of 77% while text learners (n = 9) scored 60% (p < .05). Survey results indicated video learners were more satisfied with their learning module than text learners. Vicarious audiovisual learning modules may be an efficacious, low cost means of delivering perfusion training on subjects such as equipment setup and operation. Video learning appears to improve cognition and retention of learned content and may play an important role in how we teach perfusion in the future, as simulation technology becomes more prevalent.
Keywords: perfusion, education, simulation, video, computer
See one, do one, teach one is a traditional andragogical method found in medical education. This well-known maxim describes a teaching strategy that is sequential and emphasizes visualization leading to knowledge, execution leading to competence, and finally demonstration or performance of a particular task. It combines the benefits of many different learning styles to produce critical thinkers and nurture the transition from student to medical professional. Similarly, educating future perfusionists and bridging the gap between perfusion school and the practice of perfusion can benefit from utilizing this same sequence. For example, perfusion students often begin their clinical experience by reading about or better yet watching a cardio-pulmonary bypass pump get set up. By practicing what they have learned, they become proficient and master this skill. Eventually they come to understand why they learned to set up a pump in a particular way, are able to merge theory and skill, and teach others what they have learned.
Recent technological advances in web-based education and simulation technology are generating great interest in the medical education community because they offer a novel form of experiential education and provide a means to supplement traditional teaching approaches by combining “seeing” and “doing” in a controlled setting. Vozenilek and colleagues argue that new technology changes the paradigm, to “see one, simulate many, do one competently, and teach everyone” (1). Students can now learn and safely practice techniques repeatedly without threat of harm to patients. The attention simulation technology has garnered and the potential for boosting patient safety has even convinced lawmakers to conceive bills currently in the house and senate asking the government to increase federal funding for studying medical simulation techniques (2).
Emerging research demonstrates that simulation can be a valuable learning tool. Medical educators have found simulation useful in teaching residents how to insert intravenous catheters (3) and increase surgical proficiency (4). Nursing educators have explored using simulation to validate the competency of staff (5) and students (6,7). Perfusion educators are also becoming aware of the instructive potential of using simulation. Innovators are developing perfusion simulators that interface electronically and mechanically with the heart lung machine and bypass circuit (8,9). These machines may provide a means to assess perfusionists’ conceptualization strategies in routine and failure scenarios (10) and help train the next generation of perfusionists (11).
High-fidelity simulation technology comes at a cost in terms of training educators, purchasing the equipment, and creating facilities dedicated to simulated learning. Not all perfusion education programs have the budget or staffing required to successfully use this resource. In addition, the decreasing number of perfusion schools predicted nearly a decade ago by Toomasian and colleagues (12) has resulted in more schools becoming de-centralized, serving students distributed to multiple clinical sites (13). Distribution of students at scattered clinical sites also makes expensive high-fidelity simulators and simulation facilities less appealing.
Lower-fidelity options such as simply using multimedia audio and video presentations offer a low budget alternative. Guillaume Alinier developed a typology of simulation (14) and labels screen based audio-video “Level 2” on a scale from zero to five where zero represents the lowest fidelity simulation methodology, written text. Five represents the high fidelity machines previously described.
While not as real or true to life as high fidelity trainers, lower fidelity and lower cost forms of simulation may have some merit. Early experimental results by Hartland and associates describe “…powerful and sustained learning” (15) by using short intense audio-visual learning vignettes termed “simulation-based video teaching interventions” to deliver content related to patient safety. The authors find that the realistic, scripted, and acted out negative patient events portrayed in the videos are ideal for learning about real-world events that are difficult or dangerous to reproduce with living patients. Even just adding audio to an online written lecture may improve learning (16). Sometimes it takes very little change in instructive technique to effect a change in learning.
Finding a means to best instruct perfusion students, to let them “see” what is important so that they may then “do” and skillfully practice is the focus of this paper. Instructional methods need to evolve as technology advances and adapt as students become more distributed. Taking inspiration from the now ubiquitous 10-minute video clips found on the internet and the ever-popular first person shooter genre of video games, we created a short instructional video clip designed to immerse viewers vicariously in the content by filming in the first person, making it seem as though one is really there, actively learning. When compared with instruction utilizing simple text and pictures, we believe vicarious audio-visual depiction of the same information will enhance knowledge by stimulating experiential or active learning. It is expected that dual coding this information with images and language and delivering it in a manner whereby students can live vicariously through the actors will result in superior retention of the material and make a more significant cognitive impact than text alone.
MATERIALS AND METHODS
Study Design
This study was a prospective, randomized, and controlled trial comparing text and audiovisual based teaching interventions (Figure 1). Approval for conducting this research was obtained and the study was declared exempt by the Institutional Review Boards at the University of Iowa and the University of Nebraska Medical Center in February 2010. The learning modules and corresponding assessments were computer based and delivered over the internet to perfusion students and practicing perfusionists from all over North America. The trial featured a control group receiving text instruction with accompanying pictures and a treatment group receiving audio-visual instruction of the same material. Both groups took multiple-choice quizzes administered online directly after reviewing the learning modules and then 2–4 weeks later.
Figure 1.
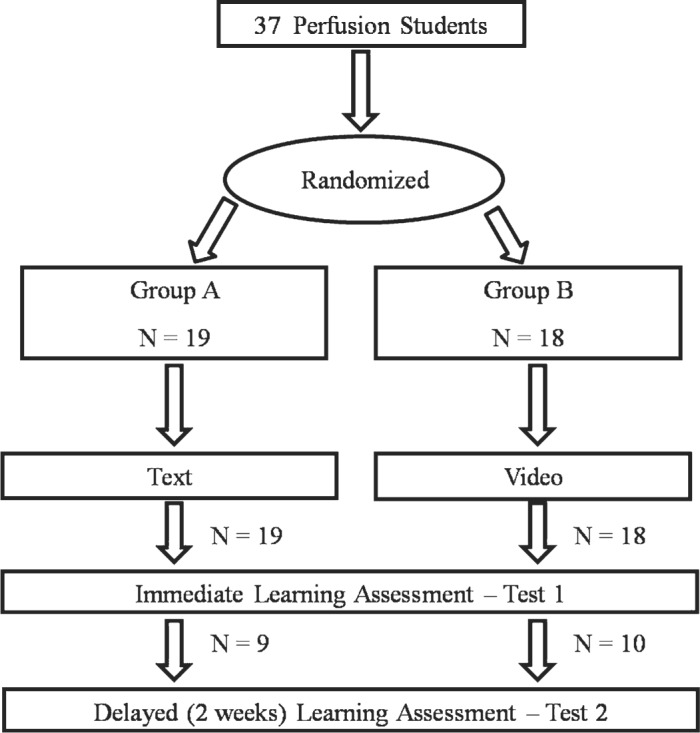
Prospective, randomized study design.
Participants
A convenience sampling of perfusion students and practicing perfusionists (n = 37) from five North American perfusion schools were recruited for the study to be representative of and generalizable to the perfusion student population as a whole. This study population consisted of first and second year traditional perfusion as well as non-traditional Masters Completion students who are already practicing perfusion. Perfusion program directors at The University of Iowa, The University of Nebraska Medical Center, Rush University Medical Center, Texas Heart Institute, and The Michener Institute agreed to forward a recruitment e-mail to their students describing the voluntary study and soliciting their participation. Students who wished to participate were directed to e-mail the study coordinator for instructions and login information.
Procedure
As shown in Figure 1 , perfusion students who indicated a willingness to participate in the study were randomly sorted by utilizing the Microsoft Excel RAND function. Half were assigned to the control group whereas the other half were assigned to the intervention group. Login information and general instructions for completing the module were e-mailed to the students allowing them to access an online testing software package called Module Viewer. Module Viewer is a proprietary software package developed by programmers in the College of Medicine at the University of Iowa and utilizes the latest technologies in online database connectivity for examination information, results storage, and online delivery of content. The many beneficial aspects of this software include the ability to deliver online multimedia content including audio, video, and text as well as a multitude of testing options including instant scoring and indefinite storage of results on a secure server. Student assigned logins controlled which learning module study participants were able to view and allowed association of test scores with that learning module.
Students logging onto either the video or text learning modules first encountered a welcome slide, which served as an informed consent document. This page emphasized the voluntary nature of the study and gave students the chance to back out of it if they wished. The next two slides determined demographic information including gender and year in school or years experience. They then were given the opportunity to view the learning module (either text or video) for as long as they like or in the case of video as many times as they like. Four questions examining students’ attitudes toward text versus video-based learning followed and were assessed utilizing a Likert psychometric scale (Table 1). The participant was able to login to the learning module as many times as they wished and simply logged out when finished.
Table 1. Likert style psychometric learning preference questions. Likert scale 1–5; 1 = Strongly disagree; 2 = Disagree somewhat; 3 = No opinion; 4 = Agree somewhat; 5 = Strongly agree.
| Question Number | Assessment |
|---|---|
| 1 | I learn best by reading text |
| 2 | I learn best by watching others |
| 3 | The manner in which information in this module was presented enhanced my learning experience |
| 4 | The format of this learning module is appropriate for learning about how to operate perfusion equipment |
Having viewed the learning intervention, the participants again logged in to take the 10 question multiple choice quiz. Results of the quiz could not be linked back to the student, only to the learning module viewed.
A reminder e-mail letter was distributed to all participants 2 weeks after sending the login information to the modules. This letter served to remind students who had not viewed the learning modules or taken the test to do so if they wished. At the same time, the letter provided instructions for all participants to again log on and take a second 10 question multiple-choice quiz that was identical to the first. This second assessment was completed without viewing any learning modules.
Educational Interventions
The learning module content used in this experiment described how to operate the stand-alone ROTAFLOW console (RFC 20–970, MAQUET Cardiopulmonary AG, Hirrlingen, Germany) and centrifugal pump (RF-32, MAQUET Cardiopulmonary AG, Hirrlingen, Germany) and originated from training lectures developed for extra corporeal membrane oxygenation technologists as well as manufacturer informational slides. The learning modules provided three types of information. Technical specifications of the console and pump came directly from user manuals. Orientation type information was examined as well, such as where the battery is located on the console. Finally, sequential pump initiation procedures that are unique and developed specifically for this experiment were described.
The content in the text version was identical to the video version apart from the method of delivery. The text module (Figure 2) had seven slides of information to study, each containing a text based narrative and accompanying slide figure. The video module (Figure 3) delivered a flash-based video entitled “1st Person Perfusion”. The same text narrative provided in the text based learning module was read aloud and a first person video representation of this narrative was portrayed by an actor so as to “dual code” the information audio-visually. The video was 13 minutes long and was produced non-professionally with little cost so it could be easily replicated.
Figure 2.
Sample slide from the text learning module using Module Viewer software.
Figure 3.
Flash video presentation from the video learning module using Module Viewer software.
Outcome Measures
After reviewing the assigned learning module, students in both the control and intervention group again logged on to the Module Viewer website to take a 10 question multiple choice test to assess cognition of the material they just learned. The questions came directly from the content of the learning modules and did not require synthesis or understanding to answer; this experiment is only examining cognition and memory of material. Answers to the questions were definitive and not open to interpretation. Module Maker software graded the quiz instantly and stored the data on a secure server. Compiled scores were placed into an Excel spreadsheet where mean test scores and the standard deviation were calculated to compare the control and treatment group. An identical second test was offered approximately 2 weeks after students had completed the first test and using Module Maker software the data from test two was compiled.
Other Measures
As previously described, the learning modules also collected additional information; gender and experience level were determined as well as questions designed to determine learning preference and assess the effectiveness of the learning intervention. Studies similar to the present one (15,16) used a course questionnaire to assess whether participants endorsed the intervention. We used a 1–5 Likert scale to assess four questions determining participant satisfaction and enthusiasm for the intervention (Table 1). In addition to proving or disproving the educational merits of each teaching intervention it is important to understand attitudes of the students and preferences for learning.
Statistical Analysis
Test scores were reported as mean percentages with the standard deviation. Analysis of variance was used to reveal any differences in the mean percentage scores between the text and video group while adjusting for gender and years of experience. The Fisher’s exact test was used to determine if there was an association between the interventional groups and their responses to the four Likert style learning preference questions.
RESULTS
Demographics
Of the 44 respondents who indicated an interest in the study, 37 consented to view the learning modules, answer the demographic and learning preference questions, and take the first post-module test (text, n = 19; video, n = 18). Participation decreased for the delayed test (test #2) with 19 students consenting to take the test again (text, n = 9; video n = 10). Information about the gender and experience level of these participants is shown in Tables 2 and 3.
Table 3. Demographic data of participants taking the delayed test (test #2). Reported as number of individuals, with the percentage representation in the learning group in parentheses.
| Characteristic | Text Group | Video Group | Total |
|---|---|---|---|
| Gender | |||
| Male | 2 (22%) | 7 (70%) | 9 (57%) |
| Female | 7 (78%) | 3 (30%) | 10 (43%) |
| Total | 9 (100%) | 10 (100%) | 19 (100%) |
| Experience | |||
| 1st Year Traditional Perfusion Student | 3 (33%) | 2 (20%) | 5 (26%) |
| 2nd Year Traditional Perfusion Student | 4 (45%) | 3 (30%) | 7 (37%) |
| 1–5 Years Practicing Perfusionist | 1 (11%) | 0 (0%) | 1 (5%) |
| >5 Years Practicing Perfusionist | 1 (11%) | 5 (50%) | 6 (32%) |
| Total | 9 (100%) | 10 (100%) | 19 (100%) |
Table 2. Demographic data of participants viewing the learning module and taking the first test. Reported as number of individuals, with the percentage representation in the learning group in parentheses.
| Characteristic | Text Group | Video Group | Total |
|---|---|---|---|
| Gender | |||
| Male | 7 (36.8%) | 14 (77.7%) | 21 (57%) |
| Female | 12 (63.2%) | 4 (22.3%) | 16 (43%) |
| Total | 19 (100%) | 18 (100%) | 37 (100%) |
| Experience | |||
| 1st Year Traditional Perfusion Student | 4 (21.1%) | 2 (11.2%) | 6 (16%) |
| 2nd Year Traditional Perfusion Student | 5 (26.2%) | 3 (16.6%) | 8 (22%) |
| 1–5 Years Practicing Perfusionist | 4 (21.1%) | 3 (16.6%) | 7 (19%) |
| >5 Years Practicing Perfusionist | 6 (31.6%) | 10 (55.6%) | 16 (43%) |
| Total | 19 (100%) | 18 (100%) | 37 (100%) |
Test scores
The primary research outcomes are displayed graphically in Figure 4 and in text on Table 4 , which compares the test scores of the text versus video participants. This is reported as mean percentage correct plus or minus the standard deviation in parentheses. Based on ANOVA analysis, the video group scored significantly higher than the text group on the immediate post test (test #1) after adjusting for gender and experience (p = .0027). This was also the case with the delayed (test #2) scores after adjusting for gender and experience (p = .046). Both groups scored lower on the delayed test than on the immediate test (p < .05).
Figure 4.
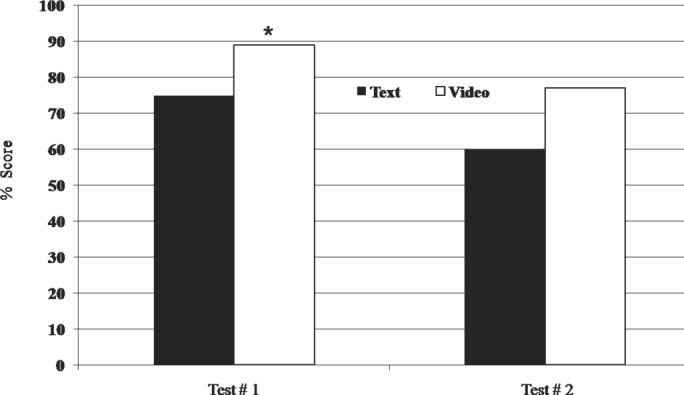
Relationships between learning module (text and video) and mean test scores. Test #1 was taken immediately after viewing the module and Test #2 was 2 weeks later.
Table 4. Relationships between learning module (text and video) and mean test scores. Test 1 was taken immediately after viewing the module and Test 2 was 2 weeks later. Reported as mean test score percentage with standard deviation and percentage difference between treatment groups.
| Tests | Text Group | Video Group | % Difference | p value |
|---|---|---|---|---|
| Test 1 mean % (SD) | 74.74 (13.9) | 88.89 (9.0) | + 14.15 | < .05 |
| (n = 19) | (n = 18) | |||
| Test 2 mean % (SD) | 60 (18) | 77 (14.9) | + 17 | < .05 |
| (n = 9) | (n = 10) | |||
| % Difference | −14.74 | −11.89 | ||
| p–value | < .05 | < .05 |
Likert Preferences
Both of the learning modules included four Likert style attitude or preference survey questions as shown on Table 1. The Likert scale ranges from 1 (strongly disagree with statement) to 5 (strongly agree with statement). For questions 1, 2, and 4 there was no statistically significant associations between groups and the student response to the question. For question 3, there was a statistically significant association between group and student response (p = .029). A higher proportion of students in the video group (77%) compared with students in the text group (23%) strongly agreed that the manner in which the information in their learning module was presented enhanced their learning experience.
DISCUSSION
With regard to the study objective, the results demonstrate that providing learning in an experiential or vicarious audiovisual format significantly improves posttest scores compared to text learning alone. The treatment group (video learning) in this prospective, randomized study scored higher than the control group (text learning) in both the immediate as well as the delayed assessment indicating that in addition to improving immediate cognition, video learning may improve retention of learned material well past the learning event. Used alone or as an adjunct to traditional teaching methods, vicarious video learning proves to be a useful tool for improving learning. Aside from this data showing improved learning, a teaching strategy utilizing vicarious audio-visual simulation lends itself particularly well to certain facets of the perfusion education curriculum and allows instructors to tailor their teaching style to a wide range of student learning styles or preferences.
How do these results relate to perfusion education and the curriculum that perfusion educators typically teach? Perfusion technology is a highly mechanical and visual science. Reading about it in texts or listening to lectures is often no substitute for hands on experience and intuitively one would think that successful perfusion students would learn best kinesthetically or vicariously. The dilemma is that it is difficult to provide perfusion students, whether located on campus or distributed, the opportunities to experience difficult clinical situations, review complex yet rarely used protocols, or observe corrective measures taken during catastrophic events. First, these circumstances happen infrequently and second, when they do occur patient safety often trumps education of the student and clinical staff step in. Perfusion equipment setup and troubleshooting is another topic that is difficult to teach with the traditional text and lecture format. Learning how to operate the myriad of increasingly complex perfusion equipment used daily without trying it yourself or at least watching someone else try it is difficult.
How then do perfusion educators fill this experiential gap and teach students how to properly operate perfusion equipment or react in the face of catastrophic events? As previously discussed, simulation technology has already gained popularity in medical education and holds great promise as an educational tool, but high fidelity simulators are often prohibitively expensive and unobtainable for the average perfusion program. In addition, using simulators requires the proper facilities and educated staff to run them. Vicarious audiovisual learning may be the more cost effective answer. You do not need specialized facilities or personnel, in fact video is extremely portable and can be downloaded and played on any number of electronic devices. People typically go to the movies for two reasons, to escape into another reality and to live vicariously through the actors and the situations in which they find themselves. It is often the next best thing to being there. Similarly, digital immersion in a learning experience, utilizing tools such as video or interactive gaming technology, can enhance the engagement and interest of students in their learning (17) and potentially enhance cognition and retention of information (15) as found in this study. Other than as a form of entertainment, audiovisual presentation of events, protocols, or other educational materials may provide an outlet for vicarious learning and improved cognition that is particularly well suited to perfusion education.
Vicarious audiovisual learning is also advantageous in that it allows instructors to tailor their instruction to meet the needs of their students. Matching optimal learning for the student with teaching style by an instructor is often a difficult task. Everyone as it turns out learns differently, what stimulates and enhances interest in one learner may do nothing for another. Neil Fleming (18), utilizing his V.A.R.K. survey, has categorized “learning styles” or preferences whereby students favor visual or auditory stimulation, others written, and others learn best by utilizing a hands on approach. Successful students, according to Fleming are multi-modal, able to adapt, and learn from whatever form of learning is available. The popular Myers Briggs survey, commonly used in healthcare education, (19) is another method used to evaluate students’ learning preferences by analyzing certain personality traits. It turns out there are hundreds of learning style measures, all of which point to a common conclusion; everyone differs in how they learn best.
Whether instructors should alter their teaching methodology to satisfy a particular student’s learning preference is debatable. Some feel as though understanding and teaching to learning styles is not a worthwhile endeavor (20), while others feel that understanding how people learn and how to instruct them is important (21). Perhaps endeavoring to present learning material in a variety of ways that are unique and memorable might be the superior choice, benefiting all students regardless of their preferred learning style. Vicarious audiovisual learning can accomplish this by allowing instructors to vary content (text, audio, graphics, music, etc.) and perspective to meet the needs of all types of learners. For instance, in the video produced for this experiment, text labels of machine components were placed over the video footage and at the same time audio narration described the specified component.
To examine the learning preferences of the study population, four survey questions were included in both learning modules. There was no difference between the groups in how they preferred to receive learning material, by text or by watching others. Perhaps this question should have specified the nature of the learning content to be more exact. However when asked whether the module they viewed enhanced their learning a greater proportion of the video learners strongly agreed compared with the text learners. The video learners appeared to be more satisfied with their learning experience. Perhaps this increased enthusiasm for the mode of delivery may explain the improved testing results.
This study has several limitations. Even though it randomly sampled perfusion students from all over North America, participation was low. A larger sampling of perfusion students from all the perfusion schools may have provided a clearer picture of how these students learn best. A future study of larger scale than this one, comparing multiple text and video interventions given to a larger student population may prove interesting.
The traditional research design used to examine the efficacy of educational treatments follows a pre-test then intervention then post-test format. We chose not to include a pre-test in this study design because proper randomization should equalize subject differences, knowledge and skills, and baseline similarity is assumed. According to Cook and Beckman (22) the randomized post-test only design is sometimes more desirable. It is thought that pre-tests can result in “testing-threats” whereby exposure to a pretest can affect performance on a post-test due to student familiarity with the material.
This study indicates that vicarious audiovisual learning may be superior to traditional text based learning for learning about perfusion equipment. Students who viewed the video learning modules had higher scores than those who viewed text learning modules. What is of prime importance and is a topic this study does not address has to do with transfer. Is a student learning a fact or procedure today able to apply that knowledge in the future? Will a perfusion student learning the mechanics of getting rid of an airlock in the venous line remember how to perform this task when they experience this in clinical practice? Whether academic competence is equivalent to clinical competence and increased patient safety is an interesting topic that needs to be explored. Enhanced future clinical performance and patient safety is the ultimate endpoint of perfusion education and research focused on how to accomplish this in the short span of perfusion schooling is important. In the coming years we believe simulation technology will provide exciting educational and research opportunities for perfusionists and perfusion educators. Low fidelity simulators like vicarious audiovisual learning will help the perfusion student to “see” what is important and high fidelity mechanical simulators will help them to “do it” many times and “teach” others. Being able to learn and practice skills in a controlled setting should, in the end, improve clinical aptitude and ensure patient safety.
ACKNOWLEDGMENT
We thank Justin Stone, University of Iowa Carver College of Medicine for his programming expertise and help with the Module Maker software utilized in this study. In addition, we thank Elizabeth Lyden, statistical coordinator for the College of Public Health at the University of Nebraska Medical Center for expert assistance with statistical analysis and advice.
REFERENCES
- 1.Vozenilek J, Huff JS, Reznek M, Gordon JA.. See one, do one, teach one: Advanced technology in medical education. Acad Emerg Med. 2004;11:1149–54. [DOI] [PubMed] [Google Scholar]
- 2.Voelker R.. Medical simulation gets real. JAMA. 2009;302:2190–2. [DOI] [PubMed] [Google Scholar]
- 3.Barsuk JH, Cohen ER, Feinglass J, McGaghie WC, Wayne DB.. Use of simulation-based education to reduce catheter-related bloodstream infections. Arch Intern Med. 2009;169:1420–3. [DOI] [PubMed] [Google Scholar]
- 4.Gorman PJ, Meier AH, Rawn C, Krummel TM.. The future of medical education is no longer blood and guts, it is bits and bytes. Am J Surg. 2000;180:353–6. [DOI] [PubMed] [Google Scholar]
- 5.Decker S, Sportsman S, Puetz L, Billings L.. The evolution of simulation and its contribution to competency. J Contin Educ Nurs. 2008;39:74–80. [DOI] [PubMed] [Google Scholar]
- 6.Kaakinen J, Arwood E.. Systematic review of nursing simulation literature for use of learning theory. Int J Nurs Educ Scholarsh. 2009;6:16. [DOI] [PubMed] [Google Scholar]
- 7.Medley CF, Horne C.. Using simulation technology for undergraduate nursing education J Nurs Educ. 2005;44:31–4. [DOI] [PubMed] [Google Scholar]
- 8.Turkmen A, Rosinski D, Noyes N.. A simulator for perfusion training. Perfusion. 2007;22:397–400. [DOI] [PubMed] [Google Scholar]
- 9.Morris RW, Pybus DA.. “Orpheus” cardiopulmonary bypass simulation system. J Extra Corpor Technol. 2007;39:228–33. [PMC free article] [PubMed] [Google Scholar]
- 10.Power G, Miller A.. Preliminary analysis of perfusionists’ strategies for managing routine and failure mode scenarios in cardiopulmonary bypass. J Extra Corpor Technol. 2007;39:160–7. [PMC free article] [PubMed] [Google Scholar]
- 11.Fernandez A.. Simulation in perfusion: Where do we go from here? Perfusion. 2010;25:17–20. [DOI] [PubMed] [Google Scholar]
- 12.Toomasian JM, Searles B, Kurusz M.. The evolution of perfusion education in America. Perfusion. 2003;18:257–65. [DOI] [PubMed] [Google Scholar]
- 13.Austin JW, Evans EL, Hoerr HR Jr.. Distributed perfusion educational model: A shift in perfusion economic realities. J Extra Corpor Technol. 2005;37:360–3. [PMC free article] [PubMed] [Google Scholar]
- 14.Alinier G.. A typology of educationally focused medical simulation tools. Med Teach. 2007;29:e243–50. [DOI] [PubMed] [Google Scholar]
- 15.Hartland W, Biddle C, Fallacaro M.. Audiovisual facilitation of clinical knowledge: A paradigm for dispersed student education based on Paivio’s dual coding theory. AANA J. 2008;76:194–8. [PubMed] [Google Scholar]
- 16.Spickard A, Smithers J, Cordray D, Gigante J, Wofford JL.. A randomised trial of an online lecture with and without audio. Med Educ. 2004;38:787–90. [DOI] [PubMed] [Google Scholar]
- 17.Dede C.. Immersive interfaces for engagement and learning. Science. 2009;323:66–9. [DOI] [PubMed] [Google Scholar]
- 18.Fleming ND.. I’m different; not dumb. Modes of presentation (VARK) in the tertiary classroom. In: Zelmer A, ed. Research and Development in Higher Education, Proceedings of the 1995 Annual Conference of the Higher Education and Research Development Society of Australasia (HERDSA). Higher Education Research and Development; 1995:308–13. [Google Scholar]
- 19.Allchin L, Dzurec LC, Engler AJ.. Psychological type and explanatory style of nursing students and clinical faculty. J Nurs Educ. 2009;48:196–202. [DOI] [PubMed] [Google Scholar]
- 20.McDonough JR.. Learning styles: An issue in clinical education? AANA J. 2005;73:89. [PubMed] [Google Scholar]
- 21.Rogers JL, Lautar CJ, Dunn LR.. Allied health students’ perceptions of effective clinical instruction. Health Care Manag (Frederick). 2010;29:63–7. [DOI] [PubMed] [Google Scholar]
- 22.Cook DA, Beckman TJ.. Reflections on experimental research in medical education. Adv Health Sci Educ Theory Pract. 2010;15:455–64. [DOI] [PubMed] [Google Scholar]