Abstract
BACKGROUND
Several inflammatory mediators have been proposed to contribute to the pathogenesis of atherosclerosis. The aim of this study was to evaluate the quantitative expression of pro-inflammatory cytokines in un-stimulated peripheral blood mononuclear cell of patients with coronary artery disease (CAD).
METHODS
Interleukin-1 beta (IL-1β), tumor necrosis factor-alpha, and interferon-gamma (IFN-γ) gene expression were evaluated in angiography confirmed patients with and without CAD in a case-control study using quantitative real-time polymerase chain reaction.
RESULTS
A significant increase (P = 0.030) in IL-1β gene expression was found in patients with CAD [median interquartile range (IQR) = 4.890 (6.084)] compared to patients without CAD [median (IQR) = 1.792 (3.172)]. Despite the increase in IFN-γ gene expression in patients with CAD [median (IQR) = 1.298 (3.896)] versus patients without CAD [median (IQR) = 0.841 (2.79)], there was not statistically significant difference (P = 0.990).
CONCLUSION
Our results provide evidence for possible association between IL-1β and development of atherosclerosis as a crucial cytokine that induce a network of signaling pathways. This finding if proved in future would suggest IL-1β as a potent therapeutic target in CAD.
Keywords: Coronary Artery Disease, Interleukin-1 Beta, Tumor Necrosis Factor-alpha, Interferon-gamma, Gene Expression
Introduction
Several lines of evidence have previously confirmed the contribution of chronic inflammatory process in atherosclerosis.1-3 The Immune responses to accumulation of oxidized lipoproteins in the vessels lead to mobilization of macrophages, dendritic cells, and lymphocytes in areas of disturbed blood flow and secretion of pro-inflammatory, chemokines, and matrix metalloproteinases.4,5 Activation of pro-inflammatory cytokines including interleukin-1 (IL-1) and tumor necrosis factor-alpha (TNF-α) and initiation of an immune mediated response from the site of plaque formation in arterial wall making a complex of reactions with a number of immune component being involved in atherosclerosis.6
Innate immune responses beside adaptive immunity have major role in the initiation of atherosclerosis.5 Infiltrating monocytes and macrophages play major role in pro-inflammatory cytokine productions in atherosclerosis in particular expression of IL-1. IL-1 is a pro-inflammatory cytokine which is shown to have important effects on atherosclerotic lesions cellular constitution.7-10
T helper-1 (Th1) cells are the most abundant T cells observed in atherosclerotic plaque.11 Th1 cytokines with interferon-γ (INF-γ) as the prototype of this group are widely accepted as a key regulator of immune mechanisms in atherogenesis.12 Studies have shown that INF-γ reduces vascular smooth muscle proliferation and collagen production. IL-1 and INF-γ upregulate the matrix metalloproteinases expression at the site of plaque formation; result in atherosclerotic plaque instability.12-15
TNF-α is another pro-inflammatory cytokine which is also reported as a potent risk factor for cardiovascular diseases.12,15 Association between atherosclerosis and augmented risk of thromboembolic complications has also been attributed to several factors related to TNF-α expression. TNF-α is known as an ultimate mediator of the acute phase response and is involved in production of other inflammatory mediators including chemokines with important role in recruitment of leucocytes to the site of inflammation.16
In this study to further examine the role of IL-1 β, IFN-γ, and TNF-α in pathophysiology of coronary artery diseases (CAD), we compared the expression profile of these cytokines in un-stimulated peripheral blood lymphocytes (PBMCs) of patients with CAD (CAD+) versus their age, sex matched patients without CAD (CAD−).
Materials and Methods
Study subjects have been recruited from individuals who had a history of chest- pain and anginal symptoms that underwent coronary artery angiography at Cath Lab Center of Dr. Shariati Hospital, Tehran, Iran, from February 2008 to March 2010. Trained cardiologists performed the whole procedures of angiography. Study power was been set as 80%. The study group comprised of 25 patients with more than 50% stenosis in all three main coronary arteries (right coronary artery, left anterior descending artery, and the left circumflex coronary artery) were known as CAD+ and 25 sex, age, and smoking habits matched subjects with smooth angiography were categorized as CAD−. Patients with history of percutaneous coronary intervention, arteriovenous graft, familial hypercholesterolemia and congenital defects of the heart valves were excluded. Written informed consent was obtained from all individuals attending the study. Study protocol was approved by the Ethics Committee of Tehran University of Medical Sciences. We also completed personal questioner for all the participants and recorded history of diabetes mellitus (DM) (fasting plasma glucose ≥ 126 mg/dl or 2 hours plasma glucose ≥ 200 mg/dl)17 hypertension (HTN) (an average blood pressure of ≥ 140/90 mmHg or history of taking medication for HTN),18 hyperlipidemia [low-density lipoprotein (LDL) ≥ 130 and/or high-density lipoprotein < 40)],19 smoking status (current smoking and/or history of smoking more than one pack/year was defined as smoker) and family history of other cardiovascular disorders such as premature CAD [presence of first elective or emergency coronary artery bypass graft (CABG), first elective or emergency percutaneous transluminal coronary angioplasty (PTCA), acute myocardial infarction without previous CABG and PTCA in the first degree relative men under 55, and women under 65]20 or myocardial infarction (MI) in first degree relatives.
Five ml peripheral blood was collected from each individual in heparin-containing tubes and was processed for Lymphocytes isolation by Lympholyte-H (Cedarlane Laboratories). RNA was extracted from PBMCs as described by Tripure reagents (Roche) manufacturer’s instructions. RNA pellets were stored at -80 °C after solving into DEPC treated water. RNA solution has been qualified by measuring ratio of optical density (OD) 260/280 on a Nano Drop spectrophotometer (NanoDrop Thermo Scientific 2000), and the solution with OD260/280 ratio < 1.6 was discarded. RNA was reverse transcribed by First Strand cDNA Synthesis Kit (Thermo Science) as the manufacturer recommends.
Quantitative real-time polymerase chain reaction (PCR) was performed using SYBR Green PCR Master Mix (Amplicon), primer pairs (Table 1) and an ABI stepOne™ (Applied Biosystems) Real Time PCR machine. Gene expression data were normalized against hypoxanthine-guanine phosphoribosyltransferase as a reference gene. Data analysis was performed using Livak formula, 2−ΔΔCT method.21
Table 1.
Primer sequences for real-time polymerase chain reaction (PCR) quantification
| Gene | Primer pair sequences | Amplicon size |
|---|---|---|
| HPRT F | 5'-CCTGGCGTCGTGATTAGTGAT-3' | 131 bp |
| HPRT R | 5'-AGACGTTCAGTCCTGTCCATAA-3' | |
| TNF-α F | 5´-CCCAGGCAGTCAGATCATCTTC-3´ | 85 bp |
| TNF-α R | 5´-AGCTGCCCCTCAGCTTGA-3´ | |
| IL-1β F | 5'-ATGGCTTATTACAGTGGCAATGAG-3' | 138 bp |
| IL-1β R | 5'-GTAGTGGTGG TCGGAGATTCG-3' | |
| INF-γ F | 5'-AGCGGATAATGGAACTCTTTTCTTAG-3' | 103 bp |
| INF-γ R | 5'-AAGTTTGAAGTAAAAGGAGACAATTTGG-3' |
HPRT: Hypoxanthine-guanine phosphoribosyltransferase; TNF-α: Tumor necrosis factor-alpha; IL-1β: Interleukin-1 beta; IFN-γ: Interferon-gamma
Test of normality for distribution of variables was performed using Kolmogorov-Smirnov test. Qualitative variables were analysis by chi-square test. Quantitative variables were compared using t-test. Since variables of genes expression levels were not normally distributed, these variables were expressed as well as medians with 25th and 75th percentiles and interquartile range, and comparisons were performed using the Mann-Whitney U-test.
Statistical analyses were performed using SPSS software for Windows (version 15, SPSS Inc. Chicago, IL, USA) and P < 0.050 was considered as statistically significant difference.
Results
The means of stenosis in CAD+ was 55% (range 50-90%) and in CAD− was 25% (range 20-45%). Characteristics of cases (range 50-90%) and controls, including age, sex, lipid profiles, and risk factors (e.g. DM, dyslipidemia, HTN, and smoking) are presented in table 2. DM and HTN were more frequent in CAD+ patients (P = 0.050, P = 0.001 respectively). The history of MI which were significantly higher in CAD+ patients compared to their CAD− counter group (P < 0.001), as well as CAD+ patients had higher serum levels of triglyceride (P = 0.044).
Table 2.
Baseline characteristics in subjects with and without coronary artery disease (CAD)
| Variable | CAD+ (n = 25) | CAD− (n = 25) | P |
|---|---|---|---|
| Sex* (male) [n (%)] | 18 (71) | 17 (68) | 0.500 |
| Current smokers* [n (%)] | 4 (16) | 2 (8) | 0.384 |
| HTN* [n (%)] | 19 (76) | 11 (44) | 0.050 |
| DM* [n (%)] | 14 (56) | 2 (8) | 0.001 |
| Dyslipidemia | 9 (36) | 4 (16) | 0.070 |
| Past MI* [n (%)] | 15 (60) | 0 (0) | < 0.001 |
| TChol£ | 183.40 ± 42.70 | 184.73 ± 44.24 | 0.914 |
| TG£ | 185.43 ± 77.04 | 148.15 ± 47.10 | 0.044 |
| LDL£ | 108.50 ± 36.75 | 129.27 ± 42.47 | 0.068 |
| HDL£ | 40.88 ± 10.86 | 41.00 ± 8.88 | 0.623 |
| Age£ (year) | 60.19 ± 8.55 | 59.68 ± 11.01 | 0.855 |
CAD: Coronary artery disease; HTN: Hypertension; DM: Diabetes mellitus; Past MI: Past history of myocardial infarction; TChol: Total cholesterol; TG: Triglyceride; LDL: Low-density lipoprotein; HDL: High-density lipoprotein;
Comparisons were performed using chi-square analysis;
Variables are described based mean ± standard deviation
Medians of genes expression was shown in table 3. A significant increase in expression of IL-1β gene was observed (P = 0.037) in the patients with CAD (CAD+) compared to the patients without CAD (CAD−).
Table 3.
IL-1β, TNF-α and IFN-γ gene expression median (IQR) in CAD+ versus CAD− individuals
| Variable | CAD−* (n = 25) | CAD+* (n = 25) | P |
|---|---|---|---|
| IL-1β gene expression** | 1.792 (3.172) | 4.890 (6.084) | 0.037 |
| TNF-α gene expression** | 0.841 (2.790) | 1.298 (3.896) | 0.930 |
| IFN-γ gene expression** | 0.946 (1.089) | 0.986 (1.121) | 0.991 |
Comparisons were performed using Mann–Whitney U-test;
CAD+: Patients with CAD; CAD−: Patients without CAD;
Variables are described based median (IQR);
CAD: Coronary artery disease; IL-1β: Interleukin-1 beta; TNF-α: Tumor necrosis factor-alpha; IFN-γ: Interferon-gamma
The level of INF-γ gene expression was higher in CAD+ compared to the CAD- patients; however it was not a significant difference (P = 0.930). We found no significant differences in quantitative expression of TNF-α gene in patients with and without CAD (P = 0.980).
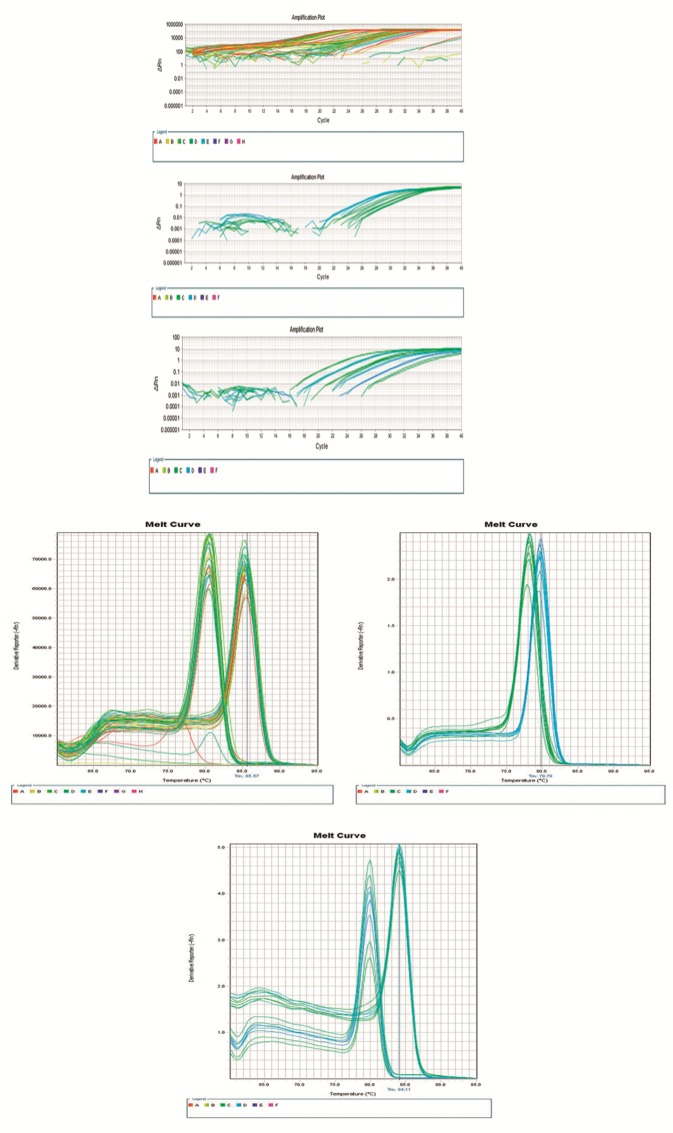
Figures 1a-f, shows melt curve and amplification plot for quantitative analysis of IL-1 IFN and TNF gene expression respectively, using real time PCR analysis (Figure 1a-f).
Figure 1.
(a-f) Melt curve and amplification plot for quantitative analysis of interleukin-1 interferon and tumor necrosis factor gene expression, respectively, using real time polymerase chain reaction analysis
Discussion
In this study, we found a significant increase in IL-1 gene expression in un-stimulated PBMCs of patients with angiography confirmed CAD compared to patients without CAD. However, the results were not significantly different for INF-γ and TNF-α gene expression between these groups. To the best of our knowledge, this is the first study which evaluates the quantitative expression of IL-1, IFN-γ, and TNF-a gene in un-stimulated PBMCs of patients with CAD. Compelling data suggested that IL-1β, INF-γ, and TNF-α play an important role in the development of atherosclerosis.22
The involvements of these cytokines are supported by their increased expression in human atherosclerotic plaques.23-27 IL-1β is a pro-inflammatory cytokine which has been previously proposed as a pro-atherogenic element.28,29 The increased expression of IL-1β observed in our study is in line with previous reports supporting the role of IL-1β in acceleration of atherosclerosis.30-38 Recent studies on animal models have shown a significant decrease in the severity of atherosclerosis in IL-1β/ apolipoprotein E (APOE) double knockout mice.39
We did not find a significant difference for expression of TNF-α gene between our groups. Although increased serum levels of TNF-α has been suggested to be associated with increased risk of recurrent MI and age related atherosclerosis,16 however this might not certainly reflect the expression of TNF-α at the mRNA level which has been examined in our study.
We also did not find any significant difference in IFN-γ gene expression in PBMCs of patients with CAD compared to patients without CAD. IFN-γ is a proinflammatory cytokine with pleiotropic biological effects which is reported to be highly expressed by various cell types including macrophages and Th1-cells in atherosclerotic plaques. IFN-γ is proposed to be rather directly or indirectly implicated during atherogenesis. Several animal experiments using APOE-/-mice for modeling atherosclerosis suggested that daily injection of IFN-γ in APOE-/- mice is associated with significant increase in lesion size and number of T-cells within lesion. Furthermore, it has been shown that development of athersclerotic lesion and severity of the phenotype in female and male LDLR-/- mice with IFN-γ deficiencies are significantly decreased.40-42 As our gene expression study was carried out on PBMCs of patients not from the cells obtained from the site of atherosclerotic plaque, therefore, the discrepancies in our finding compared to previous reports might be due to the fact that IFN-γ is produced and initiates its effect at the site of inflammation and might not have a significant role in immune milieu of subjects with atherosclerosis.
The results of this study might indicate the significant role of IL-1β as an atherogenic cytokine in pathogenesis of CAD, and if proved in future study it would be a potential target for treatment of atherosclerosis. Our data shows that IL-1 might be involved in atherosclerosis in a distinct manner compared to INF-γ and TNF-α. However regarding the limitations in our study the data needs to be interpreted with cautious. Previous reports indicate the crucial role of IL-1 receptor antagonist in development of atherosclerosis emphasizing the IL-1/IL-1Ra ratio as an important factor in the process of atherogenesis.43 It has been reported that IL-1Ra-/- knock-out mice are unable to produce cholesterol 7α-hydroxylase enzyme resulting in increased plasma cholesterol levels compared to the normal mice.44 It is known that Pro IL-1β maturation to IL-β is through caspase-1 pathway.45 This process is activated by NALP3-inflammasome.46 A recent study support the fact that cholesterol crystals and oxidized LDL as a ligand might induce NALP3-inflammasome by CD36 cell surface marker, leading to the production of IL-1β consequently. In support of this notion, Sheedy et al. reported decrease of IL-1β serum concentrations after targeting CD36 in atherosclerotic mice.47
Future studies on larger number of samples are required to further clarify the role of pro-inflammatory cytokines particularly IL-1β in pathogenesis of CAD.
Since controls of this study recruited from patients with chest pain and normal angiography, they could assign as cardiac syndrome X.48 It has been shown that degrees of increased inflammation in these patients is responsible for their symptoms, hence loss of significant difference in pro-inflammatory cytokines might be due to probable mild increased inflammation in our controls. In addition, our controls are not matched for DM, TG, and HTN which could have an effect on the cytokines release. Studies on age, sex, and other CAD risk factors matched symptomatic healthy controls (subclinical atherosclerosis should be rolled out) are suggested and could further enhance our findings. Our findings constitute a significant increased IL-1 gene expression in CAD patients which confirms the previously described role of IL-1 in atherosclerosis. This finding in addition to some prognostic implications could be utilized in therapeutic strategies focusing on modulation of inflammatory pathways involved in CAD.
Conclusion
In conclusion, our data reinforce the potential role of the IL-1β as a critical atherosclerotic marker.
Acknowledgments
This study was financially supported by Tehran University of Medical Sciences.
Footnotes
Conflicts of Interest
Authors have no conflict of interests.
REFERENCES
- 1.Khojasteh-Fard M, Abolhalaj M, Amiri P, Zaki M, Taheri Z, Qorbani M, et al. IL-23 gene expression in PBMCs of patients with coronary artery disease. Dis Markers. 2012;33(6):289–93. doi: 10.3233/DMA-2012-00933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amoli MM, Amiri P, Alborzi A, Larijani B, Saba S, Tavakkoly-Bazzaz J. VEGF gene mRNA expression in patients with coronary artery disease. Mol Biol Rep. 2012;39(9):8595–9. doi: 10.1007/s11033-012-1713-x. [DOI] [PubMed] [Google Scholar]
- 3.Ghorbanihaghjo A, Kolahi S, Seifirad S, Rashtchizadeh N, Argani H, Hajialilo M, et al. Effect of fish oil supplements on serum paraoxonase activity in female patients with rheumatoid arthritis: a double-blind randomized controlled trial. Arch Iran Med. 2012;15(9):549–52. [PubMed] [Google Scholar]
- 4.Mallat Z, Taleb S, Ait-Oufella H, Tedgui A. The role of adaptive T cell immunity in atherosclerosis. J Lipid Res. 2009;50(Suppl):S364–S369. doi: 10.1194/jlr.R800092-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hansson GK, Hermansson A. The immune system in atherosclerosis. Nat Immunol. 2011;12(3):204–12. doi: 10.1038/ni.2001. [DOI] [PubMed] [Google Scholar]
- 6.Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105(9):1135–43. doi: 10.1161/hc0902.104353. [DOI] [PubMed] [Google Scholar]
- 7.Hyka N, Dayer JM, Modoux C, Kohno T, Edwards CK, Roux-Lombard P, et al. Apolipoprotein A-I inhibits the production of interleukin-1beta and tumor necrosis factor-alpha by blocking contact-mediated activation of monocytes by T lymphocytes. Blood. 2001;97(8):2381–9. doi: 10.1182/blood.v97.8.2381. [DOI] [PubMed] [Google Scholar]
- 8.Cha JK, Jeong MH, Bae HR, Han JY, Jeong SJ, Jin HJ, et al. Activated platelets induce secretion of interleukin-1beta, monocyte chemotactic protein-1, and macrophage inflammatory protein-1alpha and surface expression of intercellular adhesion molecule-1 on cultured endothelial cells. J Korean Med Sci. 2000;15(3):273–8. doi: 10.3346/jkms.2000.15.3.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gawaz M, Brand K, Dickfeld T, Pogatsa-Murray G, Page S, Bogner C, et al. Platelets induce alterations of chemotactic and adhesive properties of endothelial cells mediated through an interleukin-1-dependent mechanism. Implications for atherogenesis. Atherosclerosis. 2000;148(1):75–85. doi: 10.1016/s0021-9150(99)00241-5. [DOI] [PubMed] [Google Scholar]
- 10.Zohlnhofer D, Brand K, Schipek K, Pogatsa-Murray G, Schomig A, Neumann FJ. Adhesion of monocyte very late antigen-4 to endothelial vascular cell adhesion molecule-1 induces interleukin-1beta-dependent expression of interleukin-6 in endothelial cells. Arterioscler Thromb Vasc Biol. 2000;20(2):353–9. doi: 10.1161/01.atv.20.2.353. [DOI] [PubMed] [Google Scholar]
- 11.Erbel C, Sato K, Meyer FB, Kopecky SL, Frye RL, Goronzy JJ, et al. Functional profile of activated dendritic cells in unstable atherosclerotic plaque. Basic Res Cardiol. 2007;102(2):123–32. doi: 10.1007/s00395-006-0636-x. [DOI] [PubMed] [Google Scholar]
- 12.Tedgui A, Mallat Z. Cytokines in atherosclerosis: pathogenic and regulatory pathways. Physiol Rev. 2006;86(2):515–81. doi: 10.1152/physrev.00024.2005. [DOI] [PubMed] [Google Scholar]
- 13.Apostolopoulos J, Davenport P, Tipping PG. Interleukin-8 production by macrophages from atheromatous plaques. Arterioscler Thromb Vasc Biol. 1996;16(8):1007–12. doi: 10.1161/01.atv.16.8.1007. [DOI] [PubMed] [Google Scholar]
- 14.Tipping PG, Hancock WW. Production of tumor necrosis factor and interleukin-1 by macrophages from human atheromatous plaques. Am J Pathol. 1993;142(6):1721–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Belkaid Y. Regulatory T cells and infection: a dangerous necessity. Nat Rev Immunol. 2007;7(11):875–88. doi: 10.1038/nri2189. [DOI] [PubMed] [Google Scholar]
- 16.Bruunsgaard H, Skinhoj P, Pedersen AN, Schroll M, Pedersen BK. Ageing, tumour necrosis factor-alpha (TNF-alpha) and atherosclerosis. Clin Exp Immunol. 2000;121(2):255–60. doi: 10.1046/j.1365-2249.2000.01281.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37(Suppl 1):S81–S90. doi: 10.2337/dc14-S081. [DOI] [PubMed] [Google Scholar]
- 18.Carretero OA, Oparil S. Essential hypertension. Part I: definition and etiology. Circulation. 2000;101(3):329–35. doi: 10.1161/01.cir.101.3.329. [DOI] [PubMed] [Google Scholar]
- 19.Lorenzo C, Williams K, Hunt KJ, Haffner SM. The National Cholesterol Education Program - Adult Treatment Panel III, International Diabetes Federation, and World Health Organization definitions of the metabolic syndrome as predictors of incident cardiovascular disease and diabetes. Diabetes Care. 2007;30(1):8–13. doi: 10.2337/dc06-1414. [DOI] [PubMed] [Google Scholar]
- 20.Kotseva K, Wood D, De BG, De BD, Pyorala K, Keil U. EUROASPIRE III: a survey on the lifestyle, risk factors and use of cardioprotective drug therapies in coronary patients from 22 European countries. Eur J Cardiovasc Prev Rehabil. 2009;16(2):121–37. doi: 10.1097/HJR.0b013e3283294b1d. [DOI] [PubMed] [Google Scholar]
- 21.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25(4):402–8. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 22.Lahoute C, Herbin O, Mallat Z, Tedgui A. Adaptive immunity in atherosclerosis: mechanisms and future therapeutic targets. Nat Rev Cardiol. 2011;8(6):348–58. doi: 10.1038/nrcardio.2011.62. [DOI] [PubMed] [Google Scholar]
- 23.Schrader JW, Moyer C, Ziltener HJ, Reinisch CL. Release of the cytokines colony-stimulating factor-1, granulocyte-macrophage colony-stimulating factor, and IL-6 by cloned murine vascular smooth muscle cells. J Immunol. 1991;146(11):3799–808. [PubMed] [Google Scholar]
- 24.Frostegard J, Ulfgren AK, Nyberg P, Hedin U, Swedenborg J, Andersson U, et al. Cytokine expression in advanced human atherosclerotic plaques: dominance of pro-inflammatory (Th1) and macrophage-stimulating cytokines. Atherosclerosis. 1999;145(1):33–43. doi: 10.1016/s0021-9150(99)00011-8. [DOI] [PubMed] [Google Scholar]
- 25.Hansson GK, Holm J, Jonasson L. Detection of activated T lymphocytes in the human atherosclerotic plaque. Am J Pathol. 1989;135(1):169–75. [PMC free article] [PubMed] [Google Scholar]
- 26.Arbustini E, Grasso M, Diegoli M, Pucci A, Bramerio M, Ardissino D, et al. Coronary atherosclerotic plaques with and without thrombus in ischemic heart syndromes: a morphologic, immunohistochemical, and biochemical study. Am J Cardiol. 1991;68(7):36B–50B. doi: 10.1016/0002-9149(91)90383-v. [DOI] [PubMed] [Google Scholar]
- 27.Barath P, Fishbein MC, Cao J, Berenson J, Helfant RH, Forrester JS. Detection and localization of tumor necrosis factor in human atheroma. Am J Cardiol. 1990;65(5):297–302. doi: 10.1016/0002-9149(90)90291-8. [DOI] [PubMed] [Google Scholar]
- 28.Vicenova B, Vopalensky V, Burysek L, Pospisek M. Emerging role of interleukin-1 in cardiovascular diseases. Physiol Res. 2009;58(4):481–98. doi: 10.33549/physiolres.931673. [DOI] [PubMed] [Google Scholar]
- 29.Weber A, Wasiliew P, Kracht M. Interleukin-1 (IL-1) pathway. Sci Signal. 2010;3(105):cm1. doi: 10.1126/scisignal.3105cm1. [DOI] [PubMed] [Google Scholar]
- 30.Sheedy FJ, Moore KJ. IL-1 signaling in atherosclerosis: sibling rivalry. Nat Immunol. 2013;14(10):1030–2. doi: 10.1038/ni.2711. [DOI] [PubMed] [Google Scholar]
- 31.Alexander MR, Moehle CW, Johnson JL, Yang Z, Lee JK, Jackson CL, et al. Genetic inactivation of IL-1 signaling enhances atherosclerotic plaque instability and reduces outward vessel remodeling in advanced atherosclerosis in mice. J Clin Invest. 2012;122(1):70–9. doi: 10.1172/JCI43713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bhaskar V, Yin J, Mirza AM, Phan D, Vanegas S, Issafras H, et al. Monoclonal antibodies targeting IL-1 beta reduce biomarkers of atherosclerosis in vitro and inhibit atherosclerotic plaque formation in Apolipoprotein E-deficient mice. Atherosclerosis. 2011;216(2):313–20. doi: 10.1016/j.atherosclerosis.2011.02.026. [DOI] [PubMed] [Google Scholar]
- 33.Chi H, Messas E, Levine RA, Graves DT, Amar S. Interleukin-1 receptor signaling mediates atherosclerosis associated with bacterial exposure and/or a high-fat diet in a murine apolipoprotein E heterozygote model: pharmacotherapeutic implications. Circulation. 2004;110(12):1678–85. doi: 10.1161/01.CIR.0000142085.39015.31. [DOI] [PubMed] [Google Scholar]
- 34.Dewberry R, Holden H, Crossman D, Francis S. Interleukin-1 receptor antagonist expression in human endothelial cells and atherosclerosis. Arterioscler Thromb Vasc Biol. 2000;20(11):2394–400. doi: 10.1161/01.atv.20.11.2394. [DOI] [PubMed] [Google Scholar]
- 35.Kim TW, Febbraio M, Robinet P, Dugar B, Greene D, Cerny A, et al. The critical role of IL-1 receptor-associated kinase 4-mediated NF-kappaB activation in modified low-density lipoprotein-induced inflammatory gene expression and atherosclerosis. J Immunol. 2011;186(5):2871–80. doi: 10.4049/jimmunol.1002242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Moyer CF, Sajuthi D, Tulli H, Williams JK. Synthesis of IL-1 alpha and IL-1 beta by arterial cells in atherosclerosis. Am J Pathol. 1991;138(4):951–60. [PMC free article] [PubMed] [Google Scholar]
- 37.Merhi-Soussi F, Kwak BR, Magne D, Chadjichristos C, Berti M, Pelli G, et al. Interleukin-1 plays a major role in vascular inflammation and atherosclerosis in male apolipoprotein E-knockout mice. Cardiovasc Res. 2005;66(3):583–93. doi: 10.1016/j.cardiores.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 38.Worrall BB, Azhar S, Nyquist PA, Ackerman RH, Hamm TL, DeGraba TJ. Interleukin-1 receptor antagonist gene polymorphisms in carotid atherosclerosis. Stroke. 2003;34(3):790–3. doi: 10.1161/01.STR.0000057815.79289.EC. [DOI] [PubMed] [Google Scholar]
- 39.Kirii H, Niwa T, Yamada Y, Wada H, Saito K, Iwakura Y, et al. Lack of interleukin-1beta decreases the severity of atherosclerosis in APOE-deficient mice. Arterioscler Thromb Vasc Biol. 2003;23(4):656–60. doi: 10.1161/01.ATV.0000064374.15232.C3. [DOI] [PubMed] [Google Scholar]
- 40.Whitman SC, Ravisankar P, Daugherty A. IFN-gamma deficiency exerts gender-specific effects on atherogenesis in apolipoprotein E-/- mice. J Interferon Cytokine Res. 2002;22(6):661–70. doi: 10.1089/10799900260100141. [DOI] [PubMed] [Google Scholar]
- 41.Gupta S, Pablo AM, Jiang X, Wang N, Tall AR, Schindler C. IFN-gamma potentiates atherosclerosis in APOE knock-out mice. J Clin Invest. 1997;99(11):2752–61. doi: 10.1172/JCI119465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Buono C, Come CE, Stavrakis G, Maguire GF, Connelly PW, Lichtman AH. Influence of interferon-gamma on the extent and phenotype of diet-induced atherosclerosis in the LDLR-deficient mouse. Arterioscler Thromb Vasc Biol. 2003;23(3):454–60. doi: 10.1161/01.ATV.0000059419.11002.6E. [DOI] [PubMed] [Google Scholar]
- 43.Merhi-Soussi F, Berti M, Wehrle-Haller B, Gabay C. Intracellular interleukin-1 receptor antagonist type 1 antagonizes the stimulatory effect of interleukin-1 alpha precursor on cell motility. Cytokine. 2005;32(3-4):163–70. doi: 10.1016/j.cyto.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 44.Isoda K, Ohsuzu F. The effect of interleukin-1 receptor antagonist on arteries and cholesterol metabolism. J Atheroscler Thromb. 2006;13(1):21–30. doi: 10.5551/jat.13.21. [DOI] [PubMed] [Google Scholar]
- 45.Netea MG, Nold-Petry CA, Nold MF, Joosten LA, Opitz B, van der Meer JH, et al. Differential requirement for the activation of the inflammasome for processing and release of IL-1beta in monocytes and macrophages. Blood. 2009;113(10):2324–35. doi: 10.1182/blood-2008-03-146720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Guo L, Wei G, Zhu J, Liao W, Leonard WJ, Zhao K, et al. IL-1 family members and STAT activators induce cytokine production by Th2, Th17, and Th1 cells. Proc Natl Acad Sci U S A. 2009;106(32):13463–8. doi: 10.1073/pnas.0906988106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sheedy FJ, Grebe A, Rayner KJ, Kalantari P, Ramkhelawon B, Carpenter SB, et al. CD36 coordinates NLRP3 inflammasome activation by facilitating intracellular nucleation of soluble ligands into particulate ligands in sterile inflammation. Nat Immunol. 2013;14(8):812–20. doi: 10.1038/ni.2639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vasheghani-Farahani A, Nouri N, Seifirad S, Sheikh FM, Hakki E, Alidoosti M, et al. Comparison of cardiovascular risk factors and biochemical profile in patients with cardiac syndrome X and obstructive coronary artery disease: A propensity score-matched study. ARYA Atheroscler. 2013;9(5):269–73. [PMC free article] [PubMed] [Google Scholar]