Abstract
BACKGROUND
A pacemaker implantation is considered major life event for cardiovascular patients, so they will probably have very interesting experiences of living with this device. The aim of this study was to explore the experiences of cardiovascular patients living with the pacemaker.
METHODS
In this qualitative study, 27 patients were chosen through purposive sampling to achieve data saturation, and their experiences were examined using semi-structured interviews. The patients’ statements were recorded with their consent and analyzed using content analysis method.
RESULTS
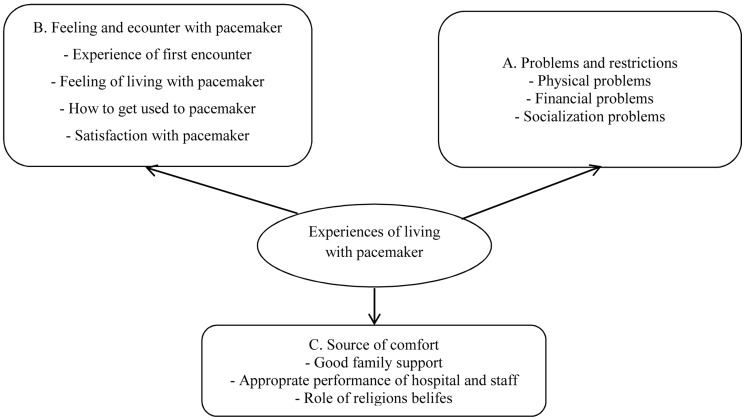
Participants’ experiences included three main themes: “Problems and limitations,” “feeling and dealing with pacemaker”, and “sources of comfort” and 10 sub-themes including: physical problems, financial problems, social problems, the first encounter, the feeling of living with the pacemaker, how to cope with pacemaker, satisfaction with pacemaker, good family support, hospital and hospital staff performance, and role of religious beliefs.
CONCLUSION
Planning to solve social problems, identifying and changing feelings of patients using pacemakers, reinforcing the resources of comfort especially family support seem to be necessary steps for improving quality of life and impact of using pacemaker.
Keywords: Cardio-Vascular Disease, Pacemaker, Experiences
Introduction
Cardiovascular diseases are among the most common causes of disease-associated mortality.1-4 Due to rapid increase in urbanization, industrialized lifestyle, lack of sufficient physical activity, and socio-economic conditions, the morbidity and mortality caused by these diseases is still rising so that today,5 about 30% of all deaths are because of cardiovascular diseases.6,7 In the United States, about 12 million people suffer from coronary artery disease, and annually about 1.5 million people suffer from heart attack and nearly 600 thousand people die due to coronary artery disease.8,9 In Iran also, cardiovascular diseases are considered to be the most common cause of mortality.10,11
One of the most important advances in providing care and service to cardiovascular patients is using pacemaker in patients suffering from acute cardiac problems.12 Pacemaker is a device that continuously monitors the status of the body and regulates heartbeats based on the body need.13 About 3 million people worldwide have a pacemaker and about 600 thousand pacemakers are implanted annually.14 Implantation of pacemaker may lead to changes in one’s mental expectations of this device, and can result in problems relating to psycho-social compatibility and quality of life, and can trigger emotional disorders.15 So, these people will probably have very diverse and interesting experiences of living with this device. Since quantitative studies have certain limitations in exploring such issues,16 the present study has been designed and conducted as a qualitative study with the aim of examining and determining the experiences of people living with a pacemaker.
Materials and Methods
This qualitative study was conducted in 2014 at Tabriz University of Medical Sciences, Iran, (TUMS). The rationale for choosing the method of qualitative studies was because of the capability of these studies in accessing the experiences and the unknown knowledge within the participants and their ability to pull them out.16,17 Among different approaches of qualitative studies, the phenomenological approach was chosen due to its ability of reviewing human experiences and believing that in the life experiences and phenomena, there are essences that can be fathomed and studied.18,19 The participants were selected from among cardiovascular patients, who had the history of using pacemaker, and had referred to subspecialty Heart clinics in TUMS for care and follow-up. Some patients did not participate in the study because of some physical problems and lack of time. These people were selected due to having great experiences of living with pacemaker. Inclusion criteria included: At least 6 months experience of using pacemaker and having the desire and ability to participate in the study. Purposive sampling was used for selection of participants (In this method, people who have the greatest and richest information and could appropriately provide the researchers with their information are selected as the participants17,20 and was continued until data saturation, i.e., to the point that the researchers feel that they cannot get new information by continuing the sampling.21 This stage was fulfilled with 21 participants in the present study but for obtaining more confidence, the researchers continued the sampling up to 27 patients. Semi-structure interviews were used for data collection. During the interviews, guided questions designed using the literature review and the opinions of experts in this field were used (Appendix 1). Duration of each interview ranged from 30 to 60 minutes. The interviews were recorded with the participants’ consent, and also the interviewers took notes for recording information. Soon after each interview, the record was assessed several times by the researchers and implemented. Content-analysis, which is a method for identifying, analyzing and reporting themes within a text and applicable in the analysis of qualitative data, was used for data analysis.22,23 Responded validity was used for data rigor so that at the end of the meeting, the participants’ statements were summarized and retold to give the chance to the participants to confirm the accuracy of the notes and perceptions of researchers. Peer check and immersed in data which are methods for creating rigor were used as well. Considering the ethics, informed consent was obtained from participants, and they could withdraw and leave the study at any time they would like to. Besides, the objectives of the study were explained to the participants at the beginning. To conduct the present study, ethical approval was obtained from the Regional Committee of ethics in research at TUMS.
Results
In this study, the experiences of 27 cardiovascular patients with a history of using pacemakers were extracted. 14 patients (52%) were female. 11 patients (40%) were illiterate. The mean duration of pacemaker use was about 43 months.
Some demographic characteristics of participants are shown in table 1.
Table 1.
Some demographic characteristics of participants
| Number | Sex/age | Job | Education | History of pacemaker implant (month) |
|---|---|---|---|---|
| 1 | M 71 | Carpenter | Illiterate | 4 |
| 2 | M 66 | Farmer | Elementary | 11 |
| 3 | F 73 | Housewife | Illiterate | 21 |
| 4 | F 68 | Housewife | Illiterate | 20 |
| 5 | F 81 | Housewife | Illiterate | 60 |
| 6 | F 77 | Housewife | Illiterate | 72 |
| 7 | M 82 | Army officer | Elementary | 18 |
| 8 | F 61 | Housewife | Elementary | 96 |
| 9 | F 46 | Housewife | Elementary | 72 |
| 10 | F 53 | Housewife | Elementary | 36 |
| 11 | F 60 | Housewife | Elementary | 48 |
| 12 | M 73 | Carpet maker | Illiterate | 72 |
| 13 | M 87 | Medicine man | Elementary | 60 |
| 14 | M 67 | Clerk | Illiterate | 30 |
| 15 | F 58 | Housewife | Illiterate | 6 |
| 16 | F 35 | Housewife | Elementary | 60 |
| 17 | F 76 | Housewife | Illiterate | 120 |
| 18 | M 52 | Unemployed | Illiterate | 84 |
| 19 | F 75 | Housewife | Elementary | 72 |
| 20 | M 79 | Clerk | Illiterate | 8 |
| 21 | M 53 | Tailor | Elementary | 3 |
| 22 | M 69 | Clerk | Elementary | 12 |
| 23 | F 51 | Housewife | Diploma | 108 |
| 24 | M 65 | Repairman | Diploma | 14 |
| 25 | M 82 | Army officer | Elementary | 18 |
| 26 | M 77 | Teacher | Bachelor's degree | 8 |
| 27 | F 56 | Faculty member | Bachelor's degree | 24 |
The results of the analysis and coding of the participants’ experiences were three main themes and 10 subthemes shown in figure 1.
Figure 1.
Main themes and subthemes extracted from participants’ experiences of living with pacemaker
Problems and restrictions
Physical problems
Many participants complained about health problems after pacemaker implantation. The most common of these were neurological problems; the participants noted that they were bored and bad tempered after pacemaker implant. Participant number 6 stated that, “… I have become impatient; I get angry quickly ….” Another common problem that patients complained about were pain.
Participant number 15 mentioned that, “… When I’m walking, it aches (the heart) … when I want to work, it aches (the heart) …” Other health problems that participants were suffering from included dyspnea, fatigue, and sleeping problems.
Financial problems
Some participants complained about high costs of the pacemaker and said that financial problem was their main concern about the pacemaker implant surgery. Participant number 2 stated that, “… It costed too much…” and participant number 6 said that, “… I was upset both in terms of operation and its costs (pacemaker implant) …” Some other participants were also upset about the high cost of surgery and pacemaker implant.
Socialization problems
Most of the participants mentioned the limitation of their social relationships and activities after pacemaker implant. Participant number 4 said that, “… my heart has become like a broken dish since I had the battery in (the pacemaker), just like a broken dish if it is hit, it’ll break. I go out with fear.” Or participant number 7 said that, “… I cannot go out a lot anymore …” And participant number 20 said that, “having tour and going out cannot be the way it used to be (before pacemaker implant).”
Feeling and dealing with pacemaker
The experience of first encounter
Feelings of fear, sickness and getting shocked were the most common feelings and experiences among the participants when they had first heard that they needed the pacemaker. Participant number 3 said that, “The first time I heard, I was a little scared ….” Participant number 7 said: “… I felt I was ill…I got a little upset …” and participant number 16 also said that, “… It was a shock to me, I cried all night …”
What it is like to live with the pacemaker
Some participants despite satisfaction of the pacemaker did not feel comfortable living with it. Feelings of absurdity, worthlessness and weakness in life were the most common types of these unpleasant feelings. Participant number 7 said: “… At that time (prior to pacemaker implant) I was like a king but now I’m like a worthless paper … I have home, I have money … but I am not pleased with anything …” Or participant number 12 said: “… I feel I am retarded, I feel like a chipped dish and people think that if they touch me, I will break.”
Coping with pacemaker
Most participants pointed to a spontaneous process and others to a compulsory one as the ways to get used to living with pacemaker. For example, when the interviewer asked the participants how they coped with the pacemaker, participant number 2 answered, “… spontaneously, little by little …” or participant number 7 said, “Gradually I got used to it …” and participants number 5 and 18 replied, “… I had no choice…”
Satisfaction with pacemaker
As mentioned in the discussion of the feeling of living with pacemakers, most participants were satisfied with the performance and implanting of pacemaker and were happy with it. Here are some views of the participants:
Number 3: “… I have been comfortable since the battery was implanted…”
Number 13: “… Battery is a good thing … it is like a help … reassures you…”
Number 9: “Battery is good, not bad.”
As a general view, the participants were satisfied with the performance of pacemakers.
Resources of comfort
Good family support
Most participants were happy and satisfied with the good support and help of family and friends and considered it as an effective factor to tolerate and improve the life with pacemaker. Participant number 3 said: “… they care a lot (i.e., spouse and children) … they are very nice …,” or participant number 16 who was satisfied with help and affection of relatives said: “My husband is so nice to me … my mom, my sister, my sister-in-law and my mother-in-law help me a lot …” and participant number 26 stated that “I get along with my family and relatives really well and I have great relationships with them…”
Good performance of hospital and its staff
Almost all participants were well-satisfied with the performance of the hospital and doctors. Participant number 11 said that, “I had a good time at the hospital … I was not annoyed at all …” and participant number 18 said: “… I did not know how it passed (having a good time in the hospital) … I was satisfied with them (doctors and nurses)…”
Constructive role of religious beliefs
High religious faith made some of the participants get along well with the pacemaker and not be afraid of its consequences particularly death. Some ideas of the participants were as follows:
Participant number 2: “Man is born once and dies once…”
Participant number 4: “I said to myself I will either die or live; ultimately everybody will meet death…”
Participant number 11: “… I didn’t think of anything … I just trusted in God…”.
Discussion
In this study, physical problem was one of the main problems and complaints of patients using pacemaker. In the study conducted by Afrasiabifar et al.24 on the experiences of the elderly having had heart attack and in the study of Sadat et al.25 on the experiences of the patients with multiple sclerosis, physical problems was one of the main problems and complaints of the participants. Furthermore, this was the case with the studies of Hildingh et al.26 and Kerr and Fothergill-Bourbonnais.27 Thus, regarding the results of this study and other similar studies, physical problems are among the major problems of the cardiovascular patients specially those using pacemakers, who indicates the need for serious consideration of the patients’ problems, that must be reduced and eliminated using medical techniques, rehabilitation, and other supportive programs.
Some patients complained about financial problems during and after pacemaker implant in the present study. In the study of Rybarczyk et al.28 financial problems and unemployment are referred to as major problems of the participants unlike the present study. This could be justified by two factors, the first could be high cost of pacemaker implant and lack of appropriate insurance coverage for these costs and the second might be due to the fact that the majority of participants in this study were from rural areas and did not have good financial status.
One of the major limitations and problems of patients using pacemaker was limitation in social interaction and relationships with others. In a way that most of the participants noted a limitation in their social relationships and interactions after pacemaker implantation. In most of similar studies conducted in other categories of cardiovascular patients, these problems and limitations were also regarded as the main problem. Among the most important of these studies are the study of Abedi et al.29 in which the psychological experiences of patients receiving heart transplants were examined, and the study of Jones et al.30 reviewing the experiences of fatigue in patients with congestive heart failure. Other studies have also demonstrated these limitations and problems.12,31,32
Although the participants in this study stated that their social relationships and communication have been limited, they referred to the good support of family members, relatives, neighbors, and others along with them. Despite this encouraging culture, providing the conditions and supportive programs for the patients’ collaboration and social activities seems to be inevitable.
In this study, the feelings of sickness, absurdity and depression were the most common emotions and experiences when the participants found out they needed pacemaker for the first time and were feelings of living with. In some other studies also similar feelings have been expressed by the participants.33,34 So, considering the effect of the feelings and attitudes of patients in their recovery and treatment process,33 providing supportive and consulting programs aiming at improving the feelings of these patients seems to be necessary.
Most participants in our study pointed out to a spontaneous and compulsory process of getting used to pacemaker. Yet in most studies conducted in other countries, the participants regarded the lifestyle changes and increasing awareness of their condition as strategies for coping with their disease situation.35,36 The reason could be due to the illiteracy and low awareness of the participants in this study. This indicates the need for increasing the awareness and helping to change lifestyle in the patients using pacemakers.
Good family support, proper performance of the hospital and the hospital staff and the constructive role of religious beliefs were relaxing factors for the patients using pacemaker. In the study conducted by Shafipour et al.,37 patients with a history of cardiac surgery noted the proper relationship with nurses, being placed in a safe and suitable environment for patients and good family support as the resources of comfort. The results of many other studies confirm these results.38-40 So, considering the constructive outcomes of the mentioned factors inpatients’ recovery, endeavors must be done for increasing the good family and relative support, improving the quality of hospital care, and reinforcing the religious beliefs to help the patients recover and feel comfortable.
The fear of pacemaker implantation and its impacts on life was also very common among study participants; an issue that was observed in Campbell et al’s.33 study too. Regarding the effect of feelings and attitudes of patients toward their treatment process,33 providing supportive and consulted programs to change and improve these patients’ feelings seems to be an important and necessary action.
The illiteracy or low education of many participants could be a limitation of the present study which caused most of the participants not to be able to give better and richer information about their experiences to the researchers in spite of the purposive selection. To compensate this problem, researchers continued sampling after saturation (21 patients) up to 27 participants by participants who were more educated to get more detailed and richer information than the previous interviews. Another limitation that could be pointed out as well was the lack of similar studies on the pacemaker patients’ experiences in literature review which caused us not to be capable of comparing the results of this study with the results of other studies. Therefore, it is suggested that similar studies on pacemaker and its various aspects be designed and carried out. The results of this study could not be generalized to various conditions and patients like other studies’ results. However, the method of this study can be used in other studies.
Conclusion
The study results showed that patients show different feelings about living with pacemaker ranging from fear and being shocked to spontaneous or compulsive adaptation to living with the pacemaker. It also showed that patients face different problems such as financial, physical and social problems after pacemaker implantation and to reduce or eliminate these problems they rely on care provided by relatives, appropriate medical care and religious beliefs. Due to the increasing rate of cardiovascular patients using pacemaker and the lack of studies conducted in this field, the need to study the effects, patients’ experiences and other aspects can be felt more than ever. The present study examined the experiences of pacemaker patients using qualitative research methods whose results can be used in providing high quality care, finding the best way to interact with patients, identifying and solving problems arising from pacemaker implantation, identifying and taking advantage of the experiences and feelings of patients and finally helping the patients using pacemakers.
Acknowledgments
The researchers would like to render their thanks to all the participants in this study, the officials and staff of the clinics of Tabriz University of Medical Sciences and Dr. Akbarzade (cardiologist) for his sincere cooperation.
Appendix 1: Interviews guides.
1. When for the first time you realized that you have to live the rest of your life with a cardiovascular device how did it feel like?
2. What feelings or experiences do you have about this situation (living with a device) regarding your familial relationships and the role you play in your family?
3. What feelings or experiences do you have about this situation (living with a device) regarding he society and your role in it?
4. What feelings or experiences do you have about this situation (living with a device) regarding hospitals or other healthcare providing centers and the care they have brought to you since?
5. How have you adapted to this situation (living with a device) and come along with it?
6. What are the most important barriers and obstacles for you regarding this situation (living with a device) and how do you feel about them?
7. Eventually what general experiences or feelings do you have regarding this situation (living with the pacemaker)?
Footnotes
Conflicts of Interest
Authors have no conflict of interests.
REFERENCES
- 1.Berwick DM. Continuous improvement as an ideal in health care. N Engl J Med. 1989;320(1):53–6. doi: 10.1056/NEJM198901053200110. [DOI] [PubMed] [Google Scholar]
- 2.Mariotto A, Chitarin M. External evaluation of health care in Italy. Qual Health Care. 1998;7(3):168–9. doi: 10.1136/qshc.7.3.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grol R, Lawrence M. Quality Improvement by Peer Review. Oxford, UK: Oxford University Press; 1995. [Google Scholar]
- 4.Sadegh Tabrizi J, Ghojazadeh M, Azami-Aghdash S, Daemi A, Hassanzadeh R. Quality of Angiography Services as Perceived by the Cardiovascular Diseases Patient. Int Jof Hospital Res. 2014;3(4):167–72. [Google Scholar]
- 5.Azami-Aghdash S, Ghojazadeh M, Fardid M, Aghaei H, Nikanfar R, Mohseni M. A Systematic Review and Content-Analysis of Service Quality Indicators Provided to Patients with Cardiovascular Disease Using Donabedian Model. J ofCardi and Ther. 2015;1(19):228–24. [Google Scholar]
- 6.Wright CC, Whittington D. Quality Assurance: An Introduction for Health Care Professionals. London, UK: Churchill Livingstone; 1992. [Google Scholar]
- 7.Black N. Quality assurance of medical care. J Public Health Med. 1990;12(2):97–104. doi: 10.1093/oxfordjournals.pubmed.a042538. [DOI] [PubMed] [Google Scholar]
- 8.Azami-Aghdash S, Ghaffari S, Sadeghi-Bazargani H, Tabrizi JS, Yagoubi A, Naghavi-Behzad M. Developing Indicators of Service Quality Provided for CardiovascularPatients Hospitalized in Cardiac Care Unit. J Cardiovasc Thorac Res. 2013;5(1):23–8. doi: 10.5681/jcvtr.2013.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azami-Aghdash S, Ghojazadeh M, Naghavi-Behzad M, Imani S, Aghaei MH. Perspectives of Cardiac Care Unit Nursing Staff about Developing Hospice Services in Iran for Terminally ill Cardiovascular Patients: A Qualitative Study. Indian J Palliat Care. 2015;21(1):56–60. doi: 10.4103/0973-1075.150185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Naghavi M, Jafari N. Mortality in the 29 provinces of Iran in 2004. Tehran, Iran: Vice-Chancellor for Health, Ministry of Health and Medical Education; 2007. [Google Scholar]
- 11.Mohanty RP, Lakhe RR. TQM in the Service Sector. New Delhi, India: Jaico Publishing House; 2008. [Google Scholar]
- 12.Silimperi DR, Franco LM, Veldhuyzen van Zanten T, MacAulay C. A framework for institutionalizing quality assurance. Int J Qual Health Care. 2002;14(Suppl 1):67–73. doi: 10.1093/intqhc/14.suppl_1.67. [DOI] [PubMed] [Google Scholar]
- 13.Dreifus LS, Cohen D. Editorial: Implanted pacemakers: Medicolegal implications. Am J Cardiol. 1975;36(2):266–7. doi: 10.1016/0002-9149(75)90536-6. [DOI] [PubMed] [Google Scholar]
- 14.Bodart C, Shresta L. Identifying information needsand indicator. Design and Implementation of Health Information System. In: WHO, editor. Design and Implementation of Health Information System. Geneva, Switzerland: WHO; 2000. pp. 49–72. [Google Scholar]
- 15.Freedman DB. Clinical governance--bridging management and clinical approaches to quality in the UK. Clin Chim Acta. 2002;319(2):133–41. doi: 10.1016/s0009-8981(02)00034-7. [DOI] [PubMed] [Google Scholar]
- 16.Department of Health & Human Services. Credentialling and defining the scope of clinical practice in Victorian health services [Online]. 2007. [2011 Sep 16]. Available from: https://www2.health.vic.gov.au/getfile/?sc_itemid=%.
- 17.Office of the Health Services Commissioner home. Guide to Complaint Handling in Health Care Services [Online]. 2005. [2012 Jan 24]. Available from: http://www.health.vic.gov.au/hsc/resources/guide.htm.
- 18.Morris B, Bell L. Quality in health care. In: Glynn JJ, Perkins DA, editors. Managing Health Care: Challenges for the 90s. Philadelphia, PA: W.B. Saunders Company; 1995. [Google Scholar]
- 19.Shaw CD. Introducing Quality Assurance. London, UK: King's Fund; 1986. [DOI] [PubMed] [Google Scholar]
- 20.Ellis R, Whittington D. Quality Assurance in Health Care: A handbook. London, UK: Edward Arnold; 1993. [Google Scholar]
- 21.Maxwell RJ. Dimensions of quality revisited: from thought to action. Qual Health Care. 1992;1(3):171–7. doi: 10.1136/qshc.1.3.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Attride-Stirling J. Thematic networks: an analytic tool for qualitative research. Qualitative Research. 2001;1(3):385–405. [Google Scholar]
- 23.Sadeghi-Bazargani H, Tabrizi JS, Azami-Aghdash S. Barriers to evidence-based medicine: a systematic review. J Eval Clin Pract. 2014;20(6):793–802. doi: 10.1111/jep.12222. [DOI] [PubMed] [Google Scholar]
- 24.Afrasiabifar A, Hosseini P, Fallahi KHoshkanab M, Yaghmaaei F. Analysis of Iranian elder patients from myocardial infraction. Salmand Iran J Ageing. 2008;3(9-10):66–74. [Google Scholar]
- 25.Sadat J, Allimohammadi N, Zoladl M. Experience of Patients with Multiple Sclerosis About Physical Effects of Their Illness; A Phenomenological Study. Dana. 2007;1(1):51–63. [Google Scholar]
- 26.Hildingh C, Fridlund B, Lidell E. Access to the world after myocardial infarction: Experiences of the recovery. Rehabilitation Nursing. 2006;31(2):63–96. doi: 10.1002/j.2048-7940.2006.tb00127.x. [DOI] [PubMed] [Google Scholar]
- 27.Kerr EE, Fothergill-Bourbonnais F. The recovery mosaic: older women's lived experiences after a myocardial infarction. Heart Lung. 2002;31(5):355–67. doi: 10.1067/mhl.2002.127939. [DOI] [PubMed] [Google Scholar]
- 28.Rybarczyk B, Grady KL, Naftel DC. Emotional Adjustment 5 Years After Heart Transplant: A Multisite Study. Rehabilitation Psychology. 2007;52(2):206–14. [Google Scholar]
- 29.Abedi HA, Monemiyan Sh, Naji SA. Spiritual-Psychological experiences of heart transplant recipients. Journal of Qualitative Research in Health Sciences. 2012;1(1):52–8. [Google Scholar]
- 30.Jones J, McDermott CM, Nowels CT, Matlock DD, Bekelman DB. The experience of fatigue as a distressing symptom of heart failure. Heart Lung. 2012;41(5):484–91. doi: 10.1016/j.hrtlng.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 31.Ovretveit J. Formulating a health quality improvement strategy for a developing country. Int J Health Care Qual Assur Inc Leadersh Health Serv. 2004;17(7):368–76. doi: 10.1108/09526860410563177. [DOI] [PubMed] [Google Scholar]
- 32.Arah OA, Klazinga NS, Delnoij DM, ten Asbroek AH, Custers T. Conceptual frameworks for health systems performance: a quest for effectiveness, quality, and improvement. Int J Qual Health Care. 2003;15(5):377–98. doi: 10.1093/intqhc/mzg049. [DOI] [PubMed] [Google Scholar]
- 33.Campbell SM, Braspenning J, Hutchinson A, Marshall M. Research methods used in developing and applying quality indicators in primary care. Qual Saf Health Care. 2002;11(4):358–64. doi: 10.1136/qhc.11.4.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chiu WT, Yang CM, Lin HW, Chu TB. Development and implementation of a nationwide health care quality indicator system in Taiwan. Int J Qual Health Care. 2007;19(1):21–8. doi: 10.1093/intqhc/mzl063. [DOI] [PubMed] [Google Scholar]
- 35.Europe E, Tyni-Lenne R. Qualitative analysis of the male experience of heart failure. Heart Lung. 2004;33(4):227–34. doi: 10.1016/j.hrtlng.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 36.Stull DE, Starling R, Haas G, Young JB. Becoming a patient with heart failure. Heart Lung. 1999;28(4):284–92. doi: 10.1016/s0147-9563(99)70075-0. [DOI] [PubMed] [Google Scholar]
- 37.Shafipour V, Mohamadi E, Ahmadi F. The Perception of Cardiac Surgery Patients on Comfortable Resources: A Qualitative Study. J Qual Res Health Sci. 2012;1(2):123–34. [Google Scholar]
- 38.Marshall M, Campbell S. Introductionto quality indicators in general practice. In: Marshall M, Campbell S, Hacker J, Roland M, editors. Quality indicators for general practice: a practical guide for health professionals and managers. London, UK: Royal Society of Medicine Press Ltd; 2001. [Google Scholar]
- 39.Ebadi Fardazar F, Safari H, Habibi F, Akbari HF, Rezapour A. Hospitals' readiness to implement clinical governance. Int J Health Policy Manag. 2015;4(2):69–74. doi: 10.15171/ijhpm.2014.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Azami-Aghdash S, Sadegh Tabrizi J, Ghojazadeh M, Naghavi-Behzad M, Imani S. Customer Quality: A Self-reporting Survey among Angiography Patients. Int J of Hospital Res. 2013;2(3):118–24. [Google Scholar]