Abstract
BACKGROUND
Coronary angiography is the gold standard method for diagnosis of coronary heart disease and usually performed by femoral approach that has several complications. To reduce these complications, upper extremity approach is increasingly used and is becoming preferred access site by many interventionists. Although radial approach is relatively well studied, safety, feasibility and risk of applying ulnar approach in not clearly known yet.
METHODS
We followed 97 patients (man = 56%, mean ± standard deviation of age = 57 ± 18) who had undergone coronary angiography or angioplasty via ulnar approach for 6-10 months and recorded their outcomes.
RESULTS
In 97 patients out of 105 ones (92.38%), procedure through ulnar access were successfully done. Unsuccessful puncture (3 patients), wiring (2 patients), passing of sheet (2 patients), and anatomically unsuitable ulnar artery (1 patient) were the reasons of failure. In 94 patients (89.52%), the angiography and angioplasty was done without any complications. Five patients (5.1%) hematoma and 11 patients (11%) experienced low-grade pain that resolved with painkiller. No infection, amputation or need for surgery was reported.
CONCLUSION
This study demonstrated that ulnar access in our patients was a safe and practical approach for coronary angiography or angioplasty, without any major complication. Bearing in mind its high success rate, it can be utilized when a radial artery is not useful for the catheterization and in cases such as prior harvesting of the radial artery (in prior coronary artery bypass grafting).
Keywords: Outcome of Arterial Access, Coronary Angiography, Coronary Angioplasty
Introduction
Coronary angiography (CAG) is the gold standard for detection of arterial narrowing related to atherosclerotic coronary artery disease (CAD). This procedure provides the most reliable information for determining the effectiveness of medical therapy as well as interventional procedures such as percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG) in patients with CAD.1
Coronary angiography is performed through percutaneous approach to arteries; therefore, selecting the best vascular access is one of the first decisions for any percutaneous cardiovascular procedure. For the first time this approach was applied in 1953,2 and brachial artery was the first access to use.3 Then cardiovascular interventionists began to use of femoral access for CAG and PCI due to some complications of brachial access in 1967.4 However, this new access site has shown to have several complications as well.5-9 During 1989 till 1999 percutaneous radial artery approach started to be applied by cardiology interventionists.10 There is already a considerable amount of articles that discuss about the conversion to predominantly radial access and its results.11 Moreover recently, an interest for upper limb approach has been emerged in some patients as it has been shown to result in significantly less clinical complications.12
Trashima and his colleagues were the first who reported the feasibility of trans-ulnar approach for diagnostic catheterization of coronary arteries more than one decade ago13 and their study was followed by limited numbers of investigations later.14 A number of studies has revealed that this method is safe and feasible and has some advantages over trans-radial approach.15 However, while the transradial approach has been proven to be useful and is established as an accepted alternative to femoral approach,16,17 trans-ulnar artery approach, and its potential risks need to be more investigated. In this article, we will discuss this approach based on 6-10 months follow-up of 97 patients undergone CAG or PCI through ulnar access.
Materials and Methods
We examined 97 patients that have been under CAG or PCI through ulnar approach from June 2013 till February 2014.We followed all of the patients that were under ulnar approach.
The patients were from two hospitals of Isfahan University of Medical Sciences, Iran, (Chamran Heart Center and Noor Hospital).
Clinical diagnosis of 78 patients was chronic CAD, while acute coronary syndrome (ACS) and acute myocardial infarction (AMI) were the indications of the intervention in 15 and 4 patients respectively (risk factors for need to intervention is presented in table 1).
Table 1.
Frequency of major cardiovascular risk factors based on sex
| Risk factor | Men n (%) | Women n (%) |
|---|---|---|
| Smoking (ever smoked) | 20 (37) | 1 (2) |
| Diabetes (FBS ≥ 26 mg/dl) | 15 (33) | 19 (44) |
| Hypertension (SBP ≥ 140, DBP ≥ 90 mmHg) | 17 (31) | 15 (35) |
| History of myocardial infarction | 11 (20) | 4 (9) |
| Hyperlipidemia (Chol ≥ 200 mg/dl) | 23 (42) | 25 (58) |
| Family history of coronary artery disease | 11 (20) | 13 (30) |
FBS: Fasting blood sugar; SBP: Systolic blood pressure; DBP: Diastolic blood pressure
CAG was performed in 81 patients and 16 patients underwent PCI. We used right hand ulnar artery in 86 patients and left one in 11 cases.
Assessment of the deep palmar arch (Allen’s test) was done for all of the patients.
For the procedure, after injection of 1.5 cc lidocaine (2%) by 2 cc syringe at the puncture site (usually about 2 cm from the head of ulnar bone) the ulnar artery was punctured with fine needle. A short guide wire was inserted and then a 5-6 French radial hydrophilic sheets was placed over the wire.
After injecting 5 cc of cocktail (consist of nitroglycerine 250 µg, verapamil 2.5 mg and normal saline diluted heparin 2500 units), 0.035ʺ wire was passed through ulnar artery into brachial artery and entered coronary arteries via ascending artery.
6ʺ tiger, right judkins and left judkins catheters were used for CAG and 6ʺ Icari, extra back-up and right judkins guiding catheters for PCI. Using ulnar approach was canceled in four cases due to the severe tortuosity of their ulnar arteries.
The patients were followed by observation and examination at the post catheters laboratory (right after procedure), at coronary care unit (CCU) or ward and every other month for at least 6 months and up to 10 months at the clinical office.
We used a data gathering form to record patients’ related information including demographic data, diagnosis, complications (major complications such as pulselessness, site ischemia, ulnar nerve damage, surgery or need to consult with surgeon, need to blood transfusion or hand amputation, myocardial infarction or pseudoaneurysm, AV fistula and ulnar artery occlusion), (minor complications such as low grade hematoma (Grade 1 hematoma: under 5 cm subcutaneous hematoma or Grade 2: under 10 cm), pain, irritation of ulnar nerve, and methods for resolving the complications and patients outcomes. Risk factors of complications in ulnar approach were emergent procedure, severe tortuosity of ulnar artery, narrowing of ulnar artery and lack of good and new wire.
Results
Totally, 54 patients (55.67%) were males and the age range of patients was from 37 to 84 years (mean ± standard deviation: 57 ± 18). Table 1 showed the frequency of major cardiovascular risk factors in both sexes. In total, 78 (80%), 15 (16%), and 4 (4%) suffer from CAD, ACS, and AMI, respectively. among the patient 81 (83%) and 16 (17%) underwent CABG and PCI, respectively. Angiography procedures performed 86 (88%) by the right hand and 11 (12%) by the left hand.
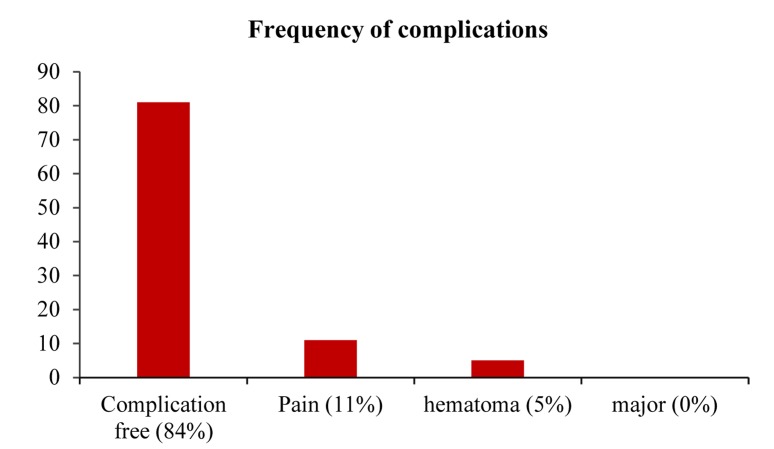
Considering major complications, none of our patients showed any of them. Regarding minor complications, 5 patients in PCI group experienced Grade 1 hematoma in ulnar region (5.1%), which was healed by local compression, bandage and oral analgesics. All of these 5 patients discharged one day after the procedure. Furthermore, 11 patients (11.3%) had a low grade pain in their hand and irritation of ulnar nerve that were resolved by administration of dexamethasone (0/5 mg) + non-steroidal anti-inflammatory drugs (200 mg ibuprofen) + gabapentin (100 mg) (oral). In 8 cases of 105 patients, this approach was not successful. Unsuccessful puncture (3 patients), unsuccessful wiring (2 patients), unsuccessful passing of sheet (2 patients) and anatomically unsuitable ulnar artery (1 patient) were the reasons of failures. Figure 1 shows the frequency of trans-ulnar approach complications among our study population.
Figure 1.
Frequency of trans-ulnar approach complications
Discussion
This study showed that ulnar approach for CAG or PCI in our patients could be consider as a safe and practical method with only minor and easily resolvable complications. Our patients showed very limited minor complications that relieved easily and quickly. In line with this, two studies had been designed to evaluate safety and feasibility of this approach. In the first study 13 patients had been followed for 30 days and in the second study 28 patients were followed for 1 week.15,18 In both studies they didn’t find any major complication due to this access and have concluded that ulnar artery is a safe and feasible approach for cardiac CABG and PCI. Furthermore in a recent study on 410 patients, access site related complications were reported only in 3.9% of patients without any incidence of major complications.19 De Andrade et al.19 have listed their reasons for using ulnar approach and a wider and easily palpable pulse of the ulnar artery compared to the radial, was reported as the first reason which accounts for 73.2% of the cases. According to this article, this approach results in decreasing the incidence of vasospasm and consequently procedure failure and leads to more patient satisfaction.
Success rate of using this approach in our study was 92%. The reported success rates in some other studies have been 100% (20), 98.5% (19) and 88%.13 Besides, results of an investigation done to compare two upper limb accesses for arterial cannulation, showed that arterial cannulation success rate is equivalent in radial and ulnar (with strong pulse) approache.20
Ulnar artery is usually larger than radial which may make it less disposed to catheter-induced vasospasm compared to the radial artery. Furthermore, this can lead to taking advantage of larger arterial sheaths. Moreover, ulnar nerve trauma is a potential complication of this method, which has not been reported in some studies. It is believed that applying a proper size needle and careful placement of it would be helpful to avoid the occurrence of this complication.15,21-23
Furthermore, we recommend performance of Doppler sonography of upper limb in patients with persistent signs or weak end pulses. Furthermore, coronary angiography via femoral artery access should be considered in the case of severe hand ischemia, although we didn’t need to use any of these procedures.
In summary, in our patients, trans-ulnar approach for PCI and CAG was safe an alternative to the trans-femoral and trans-radial approaches that can be safely applied when those accesses are at high risk of complications or failure and even potentially may be considered as the preferred primary access site.
Acknowledgments
This project is funded by the Isfahan University of Medical Sciences. The authors have no conflicts of interest in the study design, data collection, analysis, interpretation of data, writing of the report, or the decision to submit the paper for publication.
Footnotes
Conflicts of Interest
Authors have no conflict of interests.
REFERENCES
- 1.Golabchi A, Sadeghi M, Sanei H, Akhbari MR, Seiedhosseini SM, Khosravi P, et al. Can timi risk score predict angiographic involvement in patients with st-elevation myocardial infarction? ARYA Atheroscler. 2010;6(2):69–73. [PMC free article] [PubMed] [Google Scholar]
- 2.Sadeghi M, Sarrafzadegan N, Shahabi J, Naghnaiian M, Hedayat P. The Five-Year Trend of Coronary Artery Diseases Based on Angiography Results in Central Part of IRAN. Iranian Heart Journal. 2012;13(2):12–9. [Google Scholar]
- 3.Alvarez-Tostado JA, Moise MA, Bena JF, Pavkov ML, Greenberg RK, Clair DG, et al. The brachial artery: a critical access for endovascular procedures. J Vasc Surg. 2009;49(2):378–85. doi: 10.1016/j.jvs.2008.09.017. [DOI] [PubMed] [Google Scholar]
- 4.Mueller RL, Sanborn TA. The history of interventional cardiology: cardiac catheterization, angioplasty, and related interventions. Am Heart J. 1995;129(1):146–72. doi: 10.1016/0002-8703(95)90055-1. [DOI] [PubMed] [Google Scholar]
- 5.Tavris DR, Wang Y, Jacobs S, Gallauresi B, Curtis J, Messenger J, et al. Bleeding and vascular complications at the femoral access site following percutaneous coronary intervention (PCI): an evaluation of hemostasis strategies. J Invasive Cardiol. 2012;24(7):328–34. [PubMed] [Google Scholar]
- 6.Alonso M, Tascon J, Hernandez F, Andreu J, Albarran A, Velazquez MT. Complications with femoral access in cardiac cathetization. Impact of previous systematic femoral angiography and hemostasis with VasoSeal-ES collagen plug. Rev Esp Cardiol. 2003;56(6):569–77. doi: 10.1016/s0300-8932(03)76918-8. [DOI] [PubMed] [Google Scholar]
- 7.Ellis SG, Bhatt D, Kapadia S, Lee D, Yen M, Whitlow PL. Correlates and outcomes of retroperitoneal hemorrhage complicating percutaneous coronary intervention. Catheter Cardiovasc Interv. 2006;67(4):541–5. doi: 10.1002/ccd.20671. [DOI] [PubMed] [Google Scholar]
- 8.Bhatty Sh, Cooke R, Shetty R, Jovin IS. Femoral vascular access-site complications in the cardiac catheterization laboratory: diagnosis and management. Interventional Cardiology. 2011;3(4):503–14. [Google Scholar]
- 9.Masterson LL, Corby T, Haurani M, Yu L, Starr J. Access Site Complications Are Commonly Found on Femoral Artery Duplex Ultrasound and Associated With Age and Manual Pressure. Journal of Vascular Surgery. 2014;60(4):1100. [Google Scholar]
- 10.Campeau L. Percutaneous radial artery approach for coronary angiography. Cathet Cardiovasc Diagn. 1989;16(1):3–7. doi: 10.1002/ccd.1810160103. [DOI] [PubMed] [Google Scholar]
- 11.Turner S, Sacrinty M, Manogue M, Little W, Gandhi S, Kutcher M, et al. Transitioning to the radial artery as the preferred access site for cardiac catheterization: an academic medical center experience. Catheter Cardiovasc Interv. 2012;80(2):247–57. doi: 10.1002/ccd.23387. [DOI] [PubMed] [Google Scholar]
- 12.Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am Heart J. 2009;157(1):132–40. doi: 10.1016/j.ahj.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 13.Terashima M, Meguro T, Takeda H, Endoh N, Ito Y, Mitsuoka M, et al. Percutaneous ulnar artery approach for coronary angiography: a preliminary report in nine patients. Catheter Cardiovasc Interv. 2001;53(3):410–4. doi: 10.1002/ccd.1192. [DOI] [PubMed] [Google Scholar]
- 14.Bruschke AV, Sheldon WC, Shirey EK, Proudfit WL. A half century of selective coronary arteriography. J Am Coll Cardiol. 2009;54(23):2139–44. doi: 10.1016/j.jacc.2009.06.051. [DOI] [PubMed] [Google Scholar]
- 15.Limbruno U, Rossini R, De CM, Amoroso G, Ciabatti N, Petronio AS, et al. Percutaneous ulnar artery approach for primary coronary angioplasty: safety and feasibility. Catheter Cardiovasc Interv. 2004;61(1):56–9. doi: 10.1002/ccd.10671. [DOI] [PubMed] [Google Scholar]
- 16.Balwanz CR, Javed U, Singh GD, Armstrong EJ, Southard JA, Wong GB, et al. Transradial and transfemoral coronary angiography and interventions: 1-year outcomes after initiating the transradial approach in a cardiology training program. Am Heart J. 2013;165(3):310–6. doi: 10.1016/j.ahj.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 17.Bertrand OF, Rao SV, Pancholy S, Jolly SS, Rodes-Cabau J, Larose E, et al. Transradial approach for coronary angiography and interventions: results of the first international transradial practice survey. JACC Cardiovasc Interv. 2010;3(10):1022–31. doi: 10.1016/j.jcin.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 18.Knebel AV, Cardoso CO, Correa Rodrigues LH, Sarmento-Leite RE, de Quadros AS, Mascia Gottschall CA. Safety and feasibility of transulnar cardiac catheterization. Tex Heart Inst J. 2008;35(3):268–72. [PMC free article] [PubMed] [Google Scholar]
- 19.de Andrade PB, Tebet MA, Nogueira EF, Esteves VC, de Andrade MV, Labrunie A, et al. Transulnar approach as an alternative access site for coronary invasive procedures after transradial approach failure. Am Heart J. 2012;164(4):462–7. doi: 10.1016/j.ahj.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 20.Karacalar S, Ture H, Baris S, Karakaya D, Sarihasan B. Ulnar artery versus radial artery approach for arterial cannulation: a prospective, comparative study. J Clin Anesth. 2007;19(3):209–13. doi: 10.1016/j.jclinane.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 21.Dashkoff N, Dashkoff PB, Zizzi JA, Wadhwani J, Zizzi JA. Ulnar artery cannulation for coronary angiography and percutaneous coronary intervention: case reports and anatomic considerations. Catheter Cardiovasc Interv. 2002;55(1):93–6. doi: 10.1002/ccd.10089. [DOI] [PubMed] [Google Scholar]
- 22.de Andrade PB, Tebet M, Andrade M, Mattos L, Labrunie A. Performance of coronary procedures through the transulnar access without assessment of the integrity of the deep palmar arch. J Interv Cardiol. 2008;21(6):562–5. doi: 10.1111/j.1540-8183.2008.00388.x. [DOI] [PubMed] [Google Scholar]
- 23.Khosravi A, Pourbehi MR, Pourmoghaddas M, Akhbari MR, Ziaee-Bideh F. Evaluating the impact of fractional flow reserve-guided percutaneous coronary intervention in intermediate coronary artery lesions on the mode of treatment and their outcomes: An Iranian experience. ARYA Atheroscler. 2015;11(2):153–9. [PMC free article] [PubMed] [Google Scholar]