Abstract
Background/aim
Although the safety of acupuncture per se in pregnancy is reasonably well accepted, there remains debate regarding needling at points historically considered to be ‘forbidden’ during pregnancy. This article reviews the scientific literature on this topic.
Main findings
There is no objective evidence of harm following needling at forbidden points, summarised by the following four lines of evidence. (1) In 15 clinical trials (n=823 women receiving n=4549–7234 acupuncture treatments at one or more forbidden points) rates of preterm birth (PTB) and stillbirth following are equivalent to those in untreated control groups and consistent with background rates of these complications in the general population. (2) Observational studies, including a large cohort of 5885 pregnant women needled at forbidden points at all stage of pregnancy, demonstrate that rates of miscarriage, PTB, preterm prelabour rupture of membranes (PPROM), and preterm contractions (preterm labour (PTL) or threatened PTL) are comparable with untreated controls and/or consistent with their anticipated incidence. (3) There is no reliable evidence that acupuncture/electroacupuncture (EA) can induce miscarriage/labour, even under otherwise favourable circumstances such as post-dates pregnancy or intrauterine fetal death. (4) Laboratory experiments using pregnant rats have demonstrated that repeated EA at forbidden points throughout gestation does not influence rates of post-implantation embryonic demise or cause miscarriage, fetal loss or resorption.
Conclusions
These findings are reassuring and will help individualised risk:benefit assessment before treating pregnant women. Given the numerous evidence-based indications for obstetric acupuncture and lack of evidence of harm, risk:benefit assessments will often fall in favour of treatment.
Keywords: ACUPUNCTURE, OBSTETRICS
Introduction
The safety of acupuncture per se in pregnancy is reasonably well accepted, with two recent systematic reviews highlighting a low incidence of adverse events.1 2 Although both reviews acknowledged that the overall quality of reporting in obstetric acupuncture studies was poor, the frequency of general adverse events is comparable to that reported by prospective studies of acupuncture outside of pregnancy,1 and to that associated with non-acupuncture-related interventions.2 Most adverse effects are minor and non-obstetric in nature, including fainting, transient falls in blood pressure, drowsiness, needling discomfort, and localised bleeding or haematoma, all of which acupuncturists should be used to dealing with in clinical practice. No miscarriages, preterm deliveries or other obstetric complications were deemed to be attributable to acupuncture in either review. Nevertheless, there remains debate regarding needling at specific points historically considered to be ‘forbidden’ during pregnancy.3–5 The belief that certain points are abortifacient is prevalent among traditional acupuncturists, although there is disagreement over the full spectrum of forbidden points in different classical texts,3 and some practitioners may choose to ignore the recommendations in selected circumstances.6 By contrast, the forbidden points argument is not widely upheld by practitioners of Western medical acupuncture (WMA),7 given that the concerns are historical rather than evidence-based.4
Nevertheless, given the conflicting information in the public domain regarding the perceived safety and potential dangers of acupuncture during pregnancy, there is understandably an undertone of anxiety regarding its use during the antenatal period. Arguably the biggest fear among practitioners is the scenario in which a patient experiences a miscarriage or delivers prematurely and the acupuncture treatment is blamed by association. Professional anxiety surrounding the treatment of pregnant women is not specific to acupuncture. Ultimately, however, it must be remembered that there is an expected rate of naturally-occurring complications within the pregnant population, irrespective of any intervention; therefore, practitioners need to be familiar with the background incidence of adverse outcomes to assess whether the observed frequency of such complications matches that which is expected, whether it be in the acupuncture arm of a randomised controlled trial (RCT) or an audit within clinical practice. This review summarises the scientific evidence regarding forbidden points to help acupuncture practitioners and researchers make decisions regarding their use.
Identifying sources of concern and relevant outcomes
Although there is no consensus on the full spectrum of forbidden points,3 those most frequently cited as contraindicated throughout pregnancy (at least before 37 weeks) are SP6, LI4, BL60, BL67, GB21, LU7, and points in the lower abdomen (eg, CV3–CV7) and sacral region (eg, BL27–34).4 8 9 From a neuroanatomical perspective, there are two assumed sources of concern: (1) segmental effects on the uterus via somatovisceral reflexes;10 and (2) inadvertent uterine penetration (eg, lower abdominal points). The latter assumption is supported by the fact that some forbidden points are gestation-specific. For example, it is classically taught that it is acceptable to needle abdominal points above the umbilicus (eg, CV12) up to 12 weeks, but not thereafter.9
It may be argued that the risk of uterine penetration can be circumvented. From a WMA perspective, if planning to needle myofascial trigger points in the anterior abdominal wall, one must be cognisant of the anatomical alterations in normal pregnancy, which stretch the rectus abdominis and render it much thinner such that needle depth and/or angulation may need to be adjusted. If simply planning to stimulate the myotomes corresponding to the segmental innervation of the uterus at T12/L1, one could always take the alternative approach of treating at the same spinal levels on the dorsal surface of the body, completely negating the risk of uterine perforation. Alternatively one could pick up the sacral segments (S2/S3/S4) instead, by needling in the lower limbs. It seems unlikely that uterine perforation occurs frequently, particularly as there are no published case reports.
Potential concern regarding somatovisceral effects arises from the observation that needling at SP6 may generate uterine contractions and cervical change at various stages of pregnancy.11–14 Although it has been suggested that such effects could be harmful, ultimately they are only surrogate markers. Indeed coordinated uterine contractions (Braxton-Hicks) occur physiologically throughout normal pregnancy and cervical change does not necessarily confer any loss of integrity.15 In order to assess whether needling forbidden points poses any tangible risks to healthy pregnancies, we must specifically examine rates of the following adverse pregnancy outcomes:
Miscarriage, defined in the UK as expulsion of a (non-viable) pregnancy before 24 weeks gestation16
- Preterm birth (PTB), defined in the UK as delivery of a liveborn baby (at any gestation) or a stillborn baby (after 24 weeks but before 37 weeks gestation):
- following preterm prelabour rupture of membranes (PPROM), which may reflect cervical change in the absence of uterine contractions19
- iatrogenically, where the obstetrician interrupts the pregnancy because of specific maternal/fetal complications (eg, pre-eclampsia).
Stillbirth, defined in the UK as the birth of a (potentially viable) baby with no signs of life that is known to have died after 24 weeks gestation.20
In terms of background risks, spontaneous miscarriage complicates at least 20% of pregnancies and 85% of these happen before 12 weeks gestation.16 PTB occurs in 7–11% of pregnancies,18 40% of which (2–5%) follow PPROM,17 19 and the incidence of stillbirth is approximately 0.5%.20
Methods
A literature search was carried out within the following databases from their inception until July 2015: PubMed, EMBASE, Cochrane Library, Biomed Central, AMED (Allied and Complementary Medicine), CINAHL (Cumulative Index to Nursing and Allied Health Literature) Plus, and SCOPUS. Two key search concepts were built around pregnancy and acupuncture, respectively, and then combined. Search terms for acupuncture comprised “acupuncture”, “electroacupuncture”, “dry needling” and the MeSH term “acupuncture therapy”. Search terms for pregnancy consisted of “pregnancy”, “pregnancies”, “pregnant”, “gravid”, “gravidity”, “gestation”, “gestational”, “obstetric”, “obstetrical”, “obstetrics”, “maternal”, “maternity”, “maternities”, “childbearing”, “antenatal”, “prenatal” and “antepartum”. Languages for the full text were restricted to English and German. Lists of included/excluded studies of any systematic reviews and bibliographies were checked for any additional primary research. Research studies using either animals or human subjects (irrespective of study design) were considered only if they were pregnant and receiving needle acupuncture at one or more forbidden points. Trials of acupuncture at other points or moxibustion only were excluded.
Lack of evidence of harm: the four lines of evidence
Acupuncture at forbidden points does not increase the risk of adverse pregnancy outcome in controlled clinical trials
To date there have been 15 controlled clinical trials of acupuncture that have included one or more forbidden points in their protocols, as detailed in table 1.w1─w16 Thirteen were RCTs and two were quasi-randomised.w9 w10 The most common indications for acupuncture were low back and/or pelvic girdle pain (n=6) and breech presentation (n=6). Although BL67 stimulation is traditionally used to promote non-cephalic version, moxibustion is generally recommended over needling9 and may still have effects on uterine tone/contractility, given that women receiving antenatal moxibustion at BL67 in RCTs demonstrate a reduced need for oxytocin in labour compared to controls (RR 0.28, 95% CI 0.13 to 0.60).21
Table 1.
Adverse pregnancy outcomes in clinical trials of acupuncture using the ‘forbidden’ points of pregnancy
| Study | Design | Number of women | Clinical indication | Gestation (weeks) | ‘Forbidden’ points | Stimulation | Sessions | Adverse pregnancy outcomes | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Miscarriage | PTB | Stillbirth | ||||||||
| Coulon et alw1 | RCT | 164 | Breech presentation | 34.5±0.6 (33–35) | BL67 | De qi | Up to 6 | N/A | 11 | 1 |
| Guerreiro da Silva et alw2 | RCT | 20 | Tension-type headache | 19.8±4.0 (15–30) | LI4, GB21, LU7 | De qi | 8–12 | 0 | 0 | 0 |
| Guerreiro da Silva et alw3 | RCT | 21 | Dyspepsia | 20.5±5.4 (15–30) | LI4 | De qi | 8–12 | 0 | 0 | 0 |
| Elden et alw4 | RCT | 58 | Pelvic girdle pain | 22.0±3.0 (12–29) | LI4, BL60, BL32, BL33, KI11, SP12 | Manual stimulation every 10 min | 12 | * | * | * |
| Neri et alw5 | RCT | 24 | Breech presentation | 34.6±0.9 (33–36) | BL67 | * | Average = 3 | N/A | * | * |
| Lund et alw6 | RCT | 70 | Pelvic girdle pain | Median 26 (18–35) | SP6, LI4, CV3, BL27, BL28, BL29, BL31, BL32, KI11 | De qi | 10 | 0 | * | * |
| Elden et alw7 w8 | RCT | 125 | Pelvic girdle pain | Median 24 (12–31) | LI4, BL60, BL32, BL33, KI11, SP12 | Manual stimulation every 10 min | 12 | 0 | 5 | 0 |
| Guerreiro da Silva et alw9 | CCT | 17 | Insomnia | 20.6±5.5 (15–30) | GB21 | De qi | 8–12 | 0 | 0 | 0 |
| Guerreiro da Silva et alw10 | CCT | 27 | Low back pain | 19.9±4.6 (15–30) | Huatojiaji points in the lower back | De qi | 8–12 | 0 | 0 | 0 |
| Kvorning et alw11 | RCT | 50 | Low back and pelvic girdle pain | 30.0±4.2 (24–37) | BL60, sacroiliac tendons, pubic symphysis | De qi+ repeat after 30–60s | Up to 18 | N/A | 0 | 0 |
| Neri et al w12 | RCT | 120 | Breech presentation | 33.7±0.7 (33–35) | BL67 | De qi | Up to 4 | N/A | 0 | 0 |
| Habek et al w13 | RCT | 34 | Breech presentation | 34.0±1.3 (34–37) | BL67 | De qi | Mean=6 | N/A | 0 | 0 |
| Neri et alw14 | RCT | 15 | Breech presentation | 33.1±0.2 (33–34) | BL67 | * | Up to 6 | N/A | 0 | 0 |
| Wedenberg et alw15 | RCT | 30 | Low back and pelvic girdle pain | Mean 24.2 (20–32) | CV2, BL27, BL28, BL29, BL30, BL60, lumbosacral and pelvic local points | Manual stimulation every 15 min | 10 | 0 | * | * |
| Li and Wangw16 | RCT | 48 | Breech presentation | Not stated but all >28 weeks gestation | BL67 | Electrical stimulation | Up to 6 | N/A | * | * |
Controlled clinical trials involving (penetrating) needle acupuncture at one of more so-called ‘forbidden’ points of pregnancy, listed in reverse chronological order. Numbers of women include only those in acupuncture group(s). Gestational age is mean±SD (range) unless otherwise stated. N/A under miscarriage rate indicates trials where the gestational age at recruitment was >24 weeks, which is already beyond that required for the diagnosis of miscarriage.
*Indicates trials in which the relevant outcome data were not explicitly presented but ‘no adverse events’ was stated.
CCT, controlled clinical trial; N/A, not applicable; PTB, preterm birth; RCT, randomised controlled trial.
As can be seen from table 1, no adverse pregnancy outcomes were reported in the majority of trials using forbidden points. Where relevant adverse events did occur, these consistently fell within expected limits (in absolute terms) and were equivalent to those observed in the respective control groups (in relative terms). Elden et al reported PTB rates of 4.0% and 5.4% in the acupuncture and control groups, respectively (p>0.05), with all preterm deliveries in the acupuncture group occurring after 34 weeks gestation.w8 Coulon et al reported PTB rates of 6.7% and 6.1% in their acupuncture and control groups, respectively (p=0.82), and one stillbirth in the acupuncture group at 35 weeks due to recurrent massive histiocytic intervillositis (a rare placental inflammatory disease) in a patient who had previously been similarly affected.w1 These complication rates are similar to those reported by trials of acupuncture at points widely accepted to be completely safe in pregnancy for the treatment of nausea and vomiting during the first trimester. For example, Smith et al reported a PTB rate of 5.0% and single case of stillbirth in 278 women receiving acupuncture at PC6±additional (unforbidden) points.22
Of the 13 studies that did not report any adverse outcomes, eight detailed livebirth rates and gestational age at delivery, objectively confirming that there had been no cases of miscarriage, stillbirth or PTB. The five studies that did not report birth outcomes all explicitly stated that no adverse events occurred. While the general quality of adverse event reporting in obstetric acupuncture trials is poor,1 2 it seems improbable that devastating outcomes like pregnancy loss or neonatal unit admission due to prematurity would have been overlooked by trial data and safety monitoring boards. Thus, it appears unlikely that any additional adverse outcomes occurred yet remained unreported (excluding any loss to follow-up). We can therefore estimate that there have been 16 cases of PTB, one stillbirth, and no late miscarriages associated with 4549–7234 acupuncture sessions in a total of 823 pregnant participants across a total of 15 clinical trials (table 1).
Acupuncture at forbidden points is not associated with increased rates of adverse pregnancy outcome in observational studies
Although measuring adverse events within RCTs confers the advantage of being able to quantify relative risk and minimise confounding, overall patient numbers are often much smaller compared to observational studies, which provide useful information on safety despite being less reliable in demonstrating effectiveness. For example, Kvorning Ternov et al, before their RCT of acupuncture for low back and pelvic girdle pain,w11 published a retrospective cohort study of 167 women treated at forbidden points (including LI4, BL60, and local points in the lumbosacral and pelvic areas) from 14 weeks gestation onwards.23 The PTB rate was minimal at 1.2% (n=2) and both women delivered after 35 weeks gestation at intervals of 4 and 9 weeks, respectively, after their last acupuncture session, making causation extremely unlikely. Another patient reportedly experienced uterine contractions following her sixth acupuncture treatment at 16 weeks gestation, which was classified as an unexpected serious event attributable to acupuncture in the recent review by Clarkson et al.2 However, the symptoms resolved spontaneously and the pregnancy continued uneventfully and even reached post-maturity, as labour did not begin until 42 weeks gestation. This series is notably bigger than the acupuncture arm of any of the RCTs in table 1; however, it has since been relatively eclipsed by the large retrospective cohort study of Römer et al17 that reports outcomes for a total of 5885 women treated at forbidden points at all stages of pregnancy between 1995 and 2003, compared with a control group cared for in the same unit but receiving no acupuncture (figure 1). Despite his traditional approach, Römer clearly states in his textbook of obstetric acupuncture that he considers there to be no such thing as contraindicated points in pregnancy.24 Accordingly all the forbidden points are frequently needled without anxiety at the University Hospital Mannheim, irrespective of gestation.17 24 As illustrated in figure 1, absolute rates of miscarriage (in both first and subsequent trimesters) and PPROM were as expected and did not differ in women receiving forbidden points acupuncture compared with the control group. Rates of PTL were not reported independently but rather combined with threatened PTL as a single entity. Reassuringly, however, the proportion of women experiencing any type of preterm contractions did not differ between the acupuncture and control groups (15.4% vs 15.8%, p>0.05) and fell below the anticipated incidence (up to 20%). Rates of PTB according to its conventional definition were similarly not reported; however, the proportion of women delivering before their due date (<40 weeks gestation) following forbidden points acupuncture was not different to that observed in the untreated control group (14.7% vs 15.4%, p>0.05).17
Figure 1.
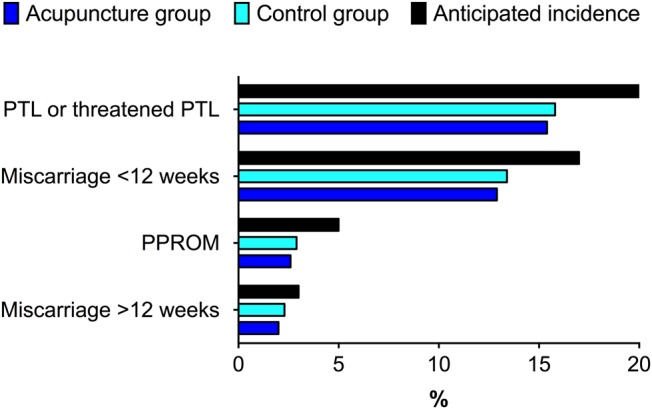
Incidence of various pregnancy outcomes in 5885 pregnant women receiving acupuncture at ‘forbidden’ points throughout gestation (acupuncture group) relative to a cohort of pregnant women not receiving acupuncture (control group) at the University Hospital Mannheim from 1995 to 2003, adapted from Römer et al.17 The anticipated incidence of these respective complications derived from the literature is shown for comparison.16 18 19 PPROM, preterm prelabour rupture of membranes; PTL, preterm labour.
Acupuncture at forbidden points does not induce miscarriage or labour
Despite anecdotes regarding the use of acupuncture to induce miscarriage of ongoing pregnancies in China, there is no published literature to support this claim. Tsuei et al12 used electroacupuncture (EA) at SP6/LI4 in an attempt to terminate seven healthy but unwanted mid-trimester pregnancies with 0% success, despite cervical softening/effacement and strong uterine contractions. Ying et al applied EA at SP6/LI4 before surgical termination of 20 first trimester pregnancies and similarly failed to demonstrate any abortifacient potential of acupuncture (with no adverse effects on β-human chorionic gonadotropin values) despite a slight (2.8 mm) increase in cervical dilatation relative to controls.13 Consequently, there is no objective evidence that acupuncture can induce the miscarriage of a healthy pregnancy. Moreover, there is no conclusive evidence that acupuncture can even induce miscarriage/labour under favourable circumstances, for example, approaching term, post-dates or in cases of intrauterine fetal death (IUFD) where the body is preparing for expulsion. Of 55 published cases of mid-trimester IUFD managed with acupuncture/EA at forbidden points, delivery of the fetus without recourse to pharmacological methods was achieved in only 13% of cases (n=7),11 12 17 which is comparable with conservative management (reflecting the natural history of IUFD).20 Regarding term induction of labour, a Cochrane review of 14 RCTs (n=2220 women) clearly showed no effect of acupuncture on timing of delivery, despite measurable effects on cervical ripening.14 The lack of efficacy of acupuncture to induce labour is further supported by the aforementioned study by Römer et al,17 in which the proportion of women reaching 42 weeks gestation (post-term) following forbidden points acupuncture did not differ from controls (10.3% vs 10.4%, p>0.05), despite the availability of ‘birth preparation’ acupuncture (including SP6/BL67) which can accelerate cervical ripening but similarly does not influence the timing of delivery.24 Collectively, these findings suggest that acupuncture-induced uterine contractions and cervical change per se do not trigger expulsion at any gestation, and indicate that additional factors are involved in the initiation of miscarriage and parturition.
Acupuncture at forbidden points does not cause harm to healthy pregnant rats
The fourth line of evidence is preclinical in nature and comes courtesy of Guerreiro da Silva et al,25 26 who performed a set of experiments using time-mated pregnant Wistar rats to examine for adverse pregnancy outcomes following EA at forbidden points SP6/LI4 and BL27/BL28 (n=12 dams each). Electrical stimulation was applied across each pair (5 Hz frequency, moderate intensity, 25 min) on six occasions throughout the 21-day rat gestation period, and sessions were deliberately timed to target the periods of implantation (up to day 7), embryonic development (day 8–14), and fetal development (day 15–18). Embryonic losses following implantation in the SP6/LI4 and BL27/BL28 groups were 4.6±2.9 and 4.0±2.4, respectively, which were not significantly different compared with two contemporaneous untreated control groups (6.7±2.1 and 3.3±1.9). Subsequently there were no fetal losses or resorptions in either EA group, with each dam bearing an average of nine live pups at the point of necropsy on day 19, and no adverse maternal effects. These findings are consistent with previous research involving direct electrical stimulation of sacral nerve roots in pregnant Sprague-Dawley rats, which similarly did not cause miscarriage or resorption.27
Summary and recommendations for practice
Objective examination of the scientific literature does not reveal any evidence of harm following needling at ‘forbidden’ points of pregnancy, despite historical or theoretical concerns. Although acupuncture appears to be able to stimulate uterine contractions and/or cervical change, there is no evidence that these putative somatovisceral effects translate into adverse pregnancy outcomes. This assertion is based on the following four lines of evidence:
Across a total of 15 clinical trials (n=823 women, n=4549–7234 treatments), rates of PTB and stillbirth following acupuncture at one or more forbidden points are equivalent to those in the untreated control groups and consistent with background rates of these complications within the general population
Observational studies, including one particularly large retrospective cohort of 5885 pregnant women needled at forbidden points at all stages of pregnancy, demonstrate that rates of miscarriage, PTB, PPROM, and preterm contractions (PTL and threatened PTL) are comparable with untreated control groups and/or consistent with their anticipated incidence
Systematic review and meta-analysis of trials of acupuncture for term labour induction and scrutiny of case series of miscarriage and IUFD indicate there is no reliable evidence that acupuncture/EA at forbidden points can induce miscarriage or labour even under favourable circumstances
Laboratory experiments on pregnant rats have demonstrated that repeated EA at forbidden points throughout gestation does not influence rates of post-implantation embryonic demise or cause miscarriage, fetal loss or resorption.
Collectively, these findings are greatly reassuring and will provide acupuncture practitioners with an up-to-date, evidence-based portfolio of information to aid the counselling of patients regarding the safety of acupuncture during pregnancy. Hopefully they will also reassure researchers that they may continue to conduct trials including the so-called forbidden points where they are clinically indicated. However, it must be emphasised that evidence of lack of harm (however robust) is not the same as unequivocal evidence of safety, which requires studies on up to tens of thousands of subjects to confidently exclude adverse effects that are subtle or involve rare outcomes. It must also be acknowledged that virtually all of the research (animal and human) that has been undertaken to date, on which this article is based, has been in generally healthy pregnancies, with or without relatively minor concurrent problems such as musculoskeletal pain, headache, insomnia and dyspepsia. Consequently, the efficacy and safety of acupuncture in pregnancies complicated by specific obstetric conditions such as uteroplacental insufficiency (pre-eclampsia and intrauterine growth restriction) or gestational diabetes has yet to be determined.
It is recommended that acupuncturists use the same guiding principles regarding treatment of the pregnant woman, as doctors do when prescribing in pregnancy─that is, to treat only where necessary. It is always good practice to carry out an individualised risk:benefit assessment before providing acupuncture for any patient. Accordingly, one may decide not to treat a pregnant woman in the absence of any condition amenable to acupuncture treatment. However, given the numerous evidence-based indications for obstetric acupuncture and the lack of objective evidence of harm detailed in this article, such risk:benefit assessments are highly likely to fall in favour of proceeding with acupuncture treatment, as any reasonable chance of positive gain for the patient is likely to outweigh purely historical or theoretical risks.
Summary points.
Acupuncture at forbidden points:
does not increase the risk of adverse pregnancy outcome in controlled clinical trials
is not associated with increased rates of adverse pregnancy outcome in observational studies
does not induce miscarriage or labour
does not cause harm to pregnant rats
Supplementary Material
Footnotes
Twitter: Follow David Carr at @IntegrativeMFM
Competing interests: DJC is the current Editor-in-Chief of Acupuncture in Medicine; however, he had absolutely no involvement in the external peer review or decision-making process related to this manuscript, as per BMJ policy.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Park J, Sohn Y, White AR, et al. The safety of acupuncture during pregnancy: a systematic review. Acupunct Med 2014;32:257–66. 10.1136/acupmed-2013-010480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clarkson CE, O'Mahony D, Jones DE. Adverse event reporting in studies of penetrating acupuncture during pregnancy: a systematic review. Acta Obstet Gynecol Scand 2015;94:453–64. 10.1111/aogs.12587 [DOI] [PubMed] [Google Scholar]
- 3.Guerreiro da Silva AV, Nakamura MU, Guerreiro da Silva JB. ‘Forbidden points’ in pregnancy: do they exist? Acupunct Med 2011;29:135–6. 10.1136/aim.2010.003699 [DOI] [PubMed] [Google Scholar]
- 4.Betts D, Budd S. ‘Forbidden points’ in pregnancy: Historical wisdom? Acupunct Med 2011;29:137–9. 10.1136/aim.2010.003814 [DOI] [PubMed] [Google Scholar]
- 5.Cummings M. ‘Forbidden points’ in pregnancy: no plausible mechanism for risk. Acupunct Med 2011;29:140–2. 10.1136/acupmed-2011-010037 [DOI] [PubMed] [Google Scholar]
- 6.Betts D, Smith CA, Dahlen HG. “Well I'm safe because…”—acupuncturists managing conflicting treatment recommendations when treating threatened miscarriage: a mixed-methods study. J Altern Complement Med 2014;20:838–45. 10.1089/acm.2014.0139 [DOI] [PubMed] [Google Scholar]
- 7.White AR, Editorial Board of Acupuncture in Medicine. Western medical acupuncture: a definition. Acupunct Med 2009;27:33–5. 10.1136/aim.2008.000372 [DOI] [PubMed] [Google Scholar]
- 8.Dale RA. The contraindicated (forbidden) points of acupuncture for needling, moxibustion and pregnancy. Am J Acupunct 1997;25:51–7. [Google Scholar]
- 9.Maciocia G. Obstetrics and gynaecology in Chinese medicine. 2nd edn Edinburgh: Churchill Livingstone; 2011. [Google Scholar]
- 10.Hotta H, Uchida S, Shimura M, et al. Uterine contractility and blood flow are reflexively regulated by cutaneous afferent stimulation in anesthetized rats. J Auton Nerv Syst 1999;15;75:23–31. 10.1016/S0165-1838(98)00170-2 [DOI] [PubMed] [Google Scholar]
- 11.Tsuei JJ, Lai YF. Induction of labor by acupuncture and electrical stimulation. Obstet Gynecol 1974;43:337–42. [PubMed] [Google Scholar]
- 12.Tsuei JJ, Lai Y, Sharma SD. The influence of acupuncture stimulation during pregnancy: the induction and inhibition of labor. Obstet Gynecol 1977;50:479–8. [PubMed] [Google Scholar]
- 13.Ying YK, Lin JT, Robins J. Acupuncture for the induction of cervical dilatation in preparation for first-trimester abortion and its influence on HCG. J Reprod Med 1985;30:530–4. [PubMed] [Google Scholar]
- 14.Smith CA, Crowther CA, Grant SJ. Acupuncture for induction of labour. Cochrane Database Syst Rev 2013;8:CD002962. [DOI] [PubMed] [Google Scholar]
- 15.Lockwood CJ, Dudenhausen JW. New approaches to the prediction of preterm delivery. J Perinat Med 1993;21:441–52. 10.1515/jpme.1993.21.6.441 [DOI] [PubMed] [Google Scholar]
- 16.National Collaborating Centre for Women's and Children's Health. Diagnosis and Initial Management in Early Pregnancy of Ectopic Pregnancy and Miscarriage (NICE Clinical Guideline) 2012. http://www.nice.org.uk/guidance/cg154/evidence/cg154-ectopic-pregnancy-and-miscarriage-full-guideline3 (accessed 09 Aug 2015).
- 17.Romer A, Zieger W, Melchert F. [Prohibition of acupuncture points during pregnancy—an outdated tradition or objective evidence?]. Deutsche Zeitschrift Für Akupunktur 2013;56:10–13. 10.1016/j.dza.2013.09.003 [DOI] [Google Scholar]
- 18.Honest H, Bachmann LM, Sundaram R, et al. The accuracy of risk scores in predicting preterm birth—a systematic review. J Obstet Gynaecol 2004;24:343–59. 10.1080/01443610410001685439 [DOI] [PubMed] [Google Scholar]
- 19.Royal College of Obstetricians and Gynaecologists. Preterm Prelabour Rupture of Membranes (Green-Top Guideline No. 44) 2006. https://www.rcog.org.uk/globalassets/documents/guidelines/gtg_44.pdf (accessed 09 Aug 2015).
- 20.Royal College of Obstetricians and Gynaecologists. Late Intrauterine Fetal Death and Stillbirth (Green-Top Guideline No. 55) 2010. https://www.rcog.org.uk/globalassets/documents/guidelines/gtg_55.pdf (accessed 09 Aug 2015).
- 21.Coyle ME, Smith CA, Peat B. Cephalic version by moxibustion for breech presentation. Cochrane Database Syst Rev 2012;5:CD003928 10.1002/14651858.CD003928 [DOI] [PubMed] [Google Scholar]
- 22.Smith C, Crowther C, Beilby J. Pregnancy outcome following women's participation in a randomised controlled trial of acupuncture to treat nausea and vomiting in early pregnancy. Complement Ther Med 2002;10:78–83. 10.1054/ctim.2002.0523 [DOI] [PubMed] [Google Scholar]
- 23.Kvorning Ternov N, Grennert L, Aberg A, et al. Acupuncture for lower back and pelvic pain in late pregnancy: a retrospective report on 167 consecutive cases. Pain Med 2001;2:204–7. 10.1046/j.1526-4637.2001.01031.x [DOI] [PubMed] [Google Scholar]
- 24.Romer AT. Medical acupuncture in pregnancy. Stuttgart: Thieme, 2005. [Google Scholar]
- 25.Guerreiro da Silva AV, Nakamura MU, Cordeiro JA, et al. The effects of so-called ‘forbidden acupuncture points’ on pregnancy outcome in Wistar rats. Forsch Komplementmed 2011;18:10–14. 10.1159/000323566 [DOI] [PubMed] [Google Scholar]
- 26.Guerreiro da Silva AV, Nakamura MU, Silva JB, et al. Could acupuncture at the so-called forbidden points be harmful to the health of pregnant Wistar rats? Acupunct Med 2013;31:202–6. 10.1136/acupmed-2012-010246 [DOI] [PubMed] [Google Scholar]
- 27.Wang Y, Hassouna M. Electrical stimulation has no adverse effect on pregnant rats and fetuses. J Urol 1999;162:1785–7. 10.1016/S0022-5347(05)68238-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


