Abstract
Objective
Spaceflight is associated with cardiovascular deregulation. However, the influence of microgravity on the cardiovascular system and its mechanisms and countermeasures remain unknown. Our previous studies have demonstrated that transcutaneous electrical acupuncture stimulation (TEAS) is effective in improving orthostatic tolerance (OT). The purpose of this study was to determine if TEAS treatment can attenuate cardiovascular deconditioning induced by a 4-day −6° head-down bed rest (HDBR).
Methods
Fourteen healthy male subjects were randomly allocated to a control group (control, n=6, 4 days HDBR without countermeasures) and a TEAS treatment group (TEAS, n=8, 4 days HDBR with TEAS at Neiguan (PC6) for 30 min each day for 4 consecutive days during HDBR). OT, plasma hormones, plasma volume and heart rate variability were assessed before and after HDBR. Cardiac function and cerebral blood flow were measured before, during and after HDBR.
Results
The data showed that TEAS treatment mitigated the decrease in OT that was observed in the control group and cardiac function, alleviated autonomic dysfunction, and partially prevented plasma volume reduction after HDBR. Angiotensin II and aldosterone were significantly increased by 129.3% and 133.3% after HDBR in the TEAS group (p<0.05).
Conclusions
These results indicate that 30 min of daily TEAS treatment at PC6 is partially effective in maintaining OT, probably due to increased plasma volume-regulating hormones and activation of the peripheral sympathetic nervous system. TEAS treatment appears effective at reducing cardiovascular deconditioning induced by HDBR for 4 days.
Trial registration number
Keywords: ACUPUNCTURE
Introduction
After exposure to real (spaceflight) or simulated (head-down bed rest, HDBR) microgravity, astronauts can experience orthostatic intolerance (OI), and become hypotensive and presyncopal when they assume an upright position. Cardiovascular deconditioning is thought to induce OI after return from space missions, and crew members can experience syncope in a standing position.1 Therefore, it is important to evaluate the orthostatic tolerance (OT) of each crew member to optimise countermeasures designed to improve their tolerance.
Current therapeutic countermeasures, including resistance training for myocardial atrophy, wearing of load suits, fluid loading, lower body negative pressure (LBNP) and selected drugs, have been proposed to counteract the harmful effects of microgravity.2 However, studies have shown that, even with extensive use of these countermeasures, benefits are limited in preventing observed post-flight problems.3
The underlying pathophysiological mechanisms are only partially understood and the symptoms of OI are thought to result from acute dysregulated cardiovascular function. Therefore, improving cardiovascular function via sympathetic activation may beneficially ameliorate OT. Recent studies have demonstrated that electrical acupuncture (EA) could strengthen the cardiovascular sympathetic system and vascular pressure responses through somatosympathetic reflexes,4 5 and in particular, EA at PC6 increases cardiovascular variables and alleviates haemorrhagic hypotension.4 6 7 Our previous studies have demonstrated that transcutaneous electrical acupuncture stimulation (TEAS) is a novel intervention against OI. Cardiac function improvement and sympathetic activation are responsible for the enhanced OT.8 However, whether TEAS as a countermeasure is capable of improving OT by activating the sympathetic system and enhancing cardiac function after 4 days of HDBR in humans has not been studied.
The aim of the present study was to examine the effects of TEAS treatment on cardiovascular function during a 4-day HDBR. Furthermore, alterations in cerebral circulation and volume-regulating hormones were measured to evaluate cerebrovascular function. We hypothesised that TEAS treatment might improve OT and prevent cardiovascular deconditioning during short-term simulated microgravity.
Materials and methods
We conducted a randomised controlled trial comparing TEAS with no intervention during 4 days of HDBR in volunteers.
Ethics approval
Each participant provided signed consent to the protocol methods. The protocol methods were approved by the Medical Ethical Committee of Fourth Military Medical University and conformed to the standards set by the latest revision of the Declaration of Helsinki.
Subjects
Fourteen healthy male volunteers were enrolled in the study. The subjects were randomly assigned to a control group (control; n=6, age 20–26 years, height 169–174 cm, weight 54–68 kg) and a TEAS group (TEAS; n=8, age 20–28 years, height 168–175, weight 55–70 kg). Selection of participants was based on the results of comprehensive physical, psychological and routine blood chemistry tests. No medication, smoking, alcohol or caffeinated drinks were allowed during the study. The study was performed in a quiet environment controlled at 25±0.5°C and relative humidity of 60–70%.
Head-down bed rest
Subjects were placed in a resting, flat, head-down position −6° from the horizontal. The entire bed rest period consisted of the 4-day HDBR and 2 days of data collection (1 day before and 1 day after the HDBR). There was intensive care monitoring over the entire period. All eating, washing, urination and defaecation was carried out in the bedridden state. Changing position around the body axis was permitted. Dietary intake was 2300–2500 kcal/day, and water intake was 1.0–1.5 L/day. Urine samples (24 h) were collected each day throughout the study. Body weight, heart rate (HR) and blood pressure (BP) were measured in the morning before breakfast. During the bed rest phase, subjects in the TEAS groups received 30 min of daily TEAS treatment, while subjects in the control group received no treatment.
Transcutaneous electrical acupuncture stimulation
TEAS was performed daily using small (1.5 cm) cutaneous electrode pads placed bilaterally at the PC6 points on the forearms (see online supplementary figure S1). The intensity of the electrical stimulation was adjusted to produce the most intense tolerable electrical sensation without muscle contractions or discomfort at a frequency of 50 Hz using the Hwato electronic acupuncture treatment instrument (Model No. SDZ-II; Suzhou Medical Appliances, Suzhou, China).
OT test
A combination of head-up tilt (HUT) and LBNP testing was applied to evaluate OT on the data collection days before and after 4 days of bed rest. Beat-by-beat arterial blood pressure (BP) was obtained from the finger of the right hand by photoplethysmography using a Finometer (TNO, Delft, Netherlands). ECGs were performed for each subject using a PowerLab system (ADInstruments, Perth, Australia). The subjects remained at rest in a supine position for 15 min for the collection of control data, and then were tilted to 75° HUT for 5 s followed by increasing steps of LBNP. LBNP began at −20 mm Hg for 5 min followed by an increase of −20 mm Hg every 5 min until −60 mm Hg (total duration 20 min) or presyncope. Presyncope was defined as a decrease in systolic BP (SBP; finger BP) to <80 mm Hg, or a decrease in SBP to <90 mm Hg associated with symptoms of lightheadedness, nausea, sweating or diaphoresis, or progressive symptoms of presyncope accompanied by a request by the subject to terminate the test. The main outcome was time, in seconds, until the test had to be terminated in each individual, up to a maximum of 1200 s.
Measurement of cardiac systolic function and cerebral blood flow
Cardiac systolic function and cerebral blood flow were measured daily in the morning. ECGs, continuous carotid pulses and phonocardiograms (PCGs) were collected simultaneously and analysed on a digital data recorder (Zhenqin; Xi'an, China) to assess cardiac systolic function including left ventricular ejection time (LVET), pre-ejection period (PEP) and ejection fraction (EF). The parameters were calculated automatically by averaging five normal wave shapes. Cerebral blood flow velocity (CBFV) in the left middle cerebral artery (MCA) was measured continuously via a 2 MHz ultrasound probe (Multi-Dop X4, TCD-8·01, DWL) kept in place with a headset.
Spectral analysis of HR variability
Fast Fourier transform was applied to the R–R interval obtained from the ECG to determine the power spectral density. This was computed using the HR variability (HRV) analysing module, which was integrated into Chart 5.5. Total spectral power was defined in the range of 0.04–0.40 Hz with high-frequency power (HF) from 0.15 to 0.40 Hz, and low-frequency power (LF) from 0.04 to 0.15 Hz.
Normalised low frequency (LFn) and high frequency (HFn) were also calculated by dividing by the total spectral power to minimise the effect of the changes in total power on the values of low- and high-frequency components.
Blood analysis and measurement of plasma volume
Blood samples were collected on the morning before and the morning after 4 days of HDBR. Plasma angiotensin II (Ang II), aldosterone (Ald) and atrial natriuretic peptide (ANP) were assayed using commercially available sandwich technique ELISA kits (IBL International, Hamburg, Germany) according to the test protocol of the manufacturer, and were analysed on a Fluostar OPTIMA Microplate Reader (BMG Labtech, Offenbach, Germany). The reduction in plasma volume from before to after bed rest was calculated from the changes in haematocrit using the Van Beaumont formula.9
The two investigators who independently evaluated these measurement before, during and after HDBR were blinded to treatments.
Statistical analysis
All data are expressed as means±SD. The BP, HR, cardiac systolic function and cerebrovascular function measurements between the control and TEAS groups were compared using repeated measures ANOVA. If a significant effect was detected, the ANOVA test for comparisons of means between the two groups was used to determine which specific values were significantly different. The differences in values before, during and after HDBR were inspected by one-way ANOVA. The HUT test, HRV and blood samples were analysed by Student's t test. A value of p<0.05 was considered statistically significant.
Results
Weight, HR and arterial BP
The online supplementary table shows the mean values for weight, HR, SBP and diastolic BP (DBP) during the study. No significant differences were observed between the control and TEAS groups.
Orthostatic tolerance
OT data are presented in figure 1. The OT time was significantly decreased after HDBR compared with before HDBR in the control group (968±201 s vs 493±104 s, respectively; p<0.05). However, the decrease was not significant in the TEAS group (920±192 s vs 756±156 s, respectively; p>0.05). Moreover, the OT time after HDBR was significantly less in the control group than in the TEAS group (493±104 s vs 756±156 s, respectively; p<0.05).
Figure 1.
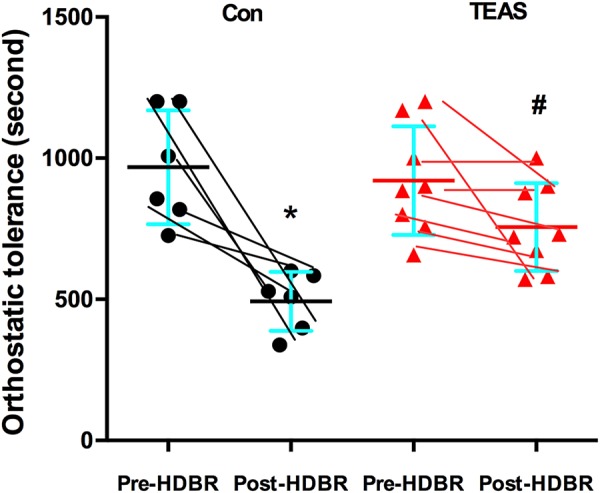
Orthostatic tolerance values before and after bed rest in the control (Con) and transcutaneous electrical acupuncture stimulation (TEAS) groups. *p<0.05, versus before head-down bed rest (HDBR); #p<0.05, versus the Con group. Con group, without any countermeasures; TEAS group, received 30 min of TEAS treatment each day.
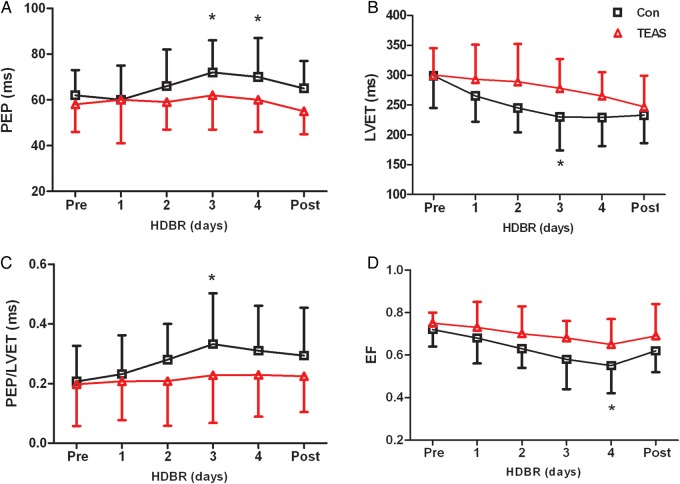
Cardiac systolic function and cerebral blood flow
The cardiac systolic functions variables PEP, LVET, PEP/LVET and EF are shown in figure 2. During the 4 days of HDBR, no statistically significant changes were seen in PEP, LVET, PEP/LVET or EF in the TEAS group compared with before HDBR. However, the mean LVET value in the control group was significantly lower on day 3 of HDBR than before HDBR (p<0.05). When compared with values before HDBR in the control group, PEP was significantly increased on days 3–4 of HDBR, while PEP/LVET was significantly increased on day 3 of HDBR. No significant differences were observed in these cardiac function-related indices between the control and TEAS groups after HDBR.
Figure 2.
Cardiac systolic function before, during and after 4 days of head-down bed rest (HDBR) in the control (Con) and transcutaneous electrical acupuncture stimulation (TEAS) groups. Mean values of (A) PEP, (B) LVET, (C) PEP/LVET ratio, and (D) EF before, during and after a 4-day HDBR in both the Con and TEAS groups. EF, ejection fraction; LVET, left ventricular ejection time; PEP, pre-ejection period. *p<0.05, compared with before HDBR.
Online supplementary figure S2 shows cerebrovascular function values before, during and after HDBR with and without TEAS. In the control group, CBFV systolic and CBFV diastolic were significantly decreased on days 3 and 4 compared with before HDBR. There were no significant changes in the pulsatility index (PI) or resistance index (RI) in the control group before, during and after bed rest. Furthermore, similar changes were seen in these parameters in the TEAS group during the 4-day HDBR, but were not significant.
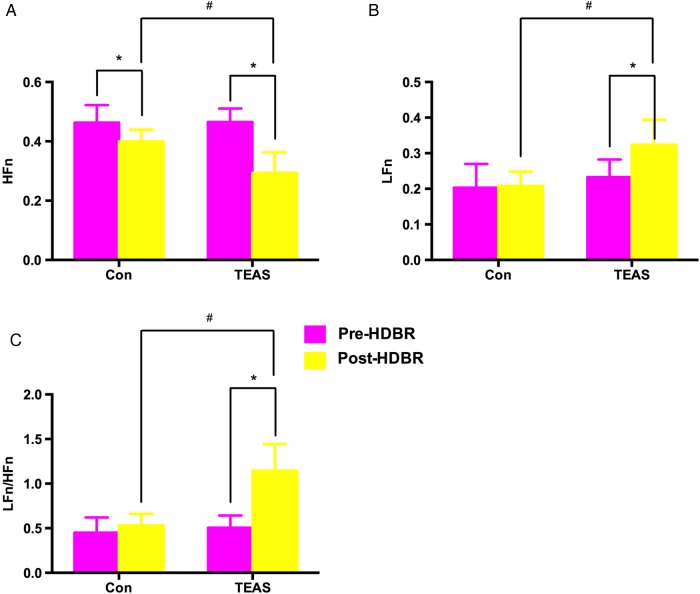
Heart rate variability
HRV data are presented in figure 3. In the control group, HFn as an indicator of vagal nerve activity was significantly decreased after compared with before HDBR, but the increases in LFn and LFn/HFn ratio were not significant. In the TEAS group, LFn and LFn/HFn were increased after bed rest compared with before. Moreover, LFn/HFn as an indicator of cardiac sympathovagal balance in the control group was significantly lower than in the TEAS group after 4 days of bed rest.
Figure 3.
Changes in R–R interval variability before and after bed rest in the control (Con) and transcutaneous electrical acupuncture stimulation (TEAS) groups. (A) Normalised high frequency power of the R–R interval (high frequency (HFn)). (B) Normalised low frequency power of the R–R interval (low frequency (LFn)). (C) Ratio of low to high frequency power of the R–R interval (LFn/HFn). *p<0.05, versus before head-down bed rest (HDBR); #p<0.05, versus the Con group.
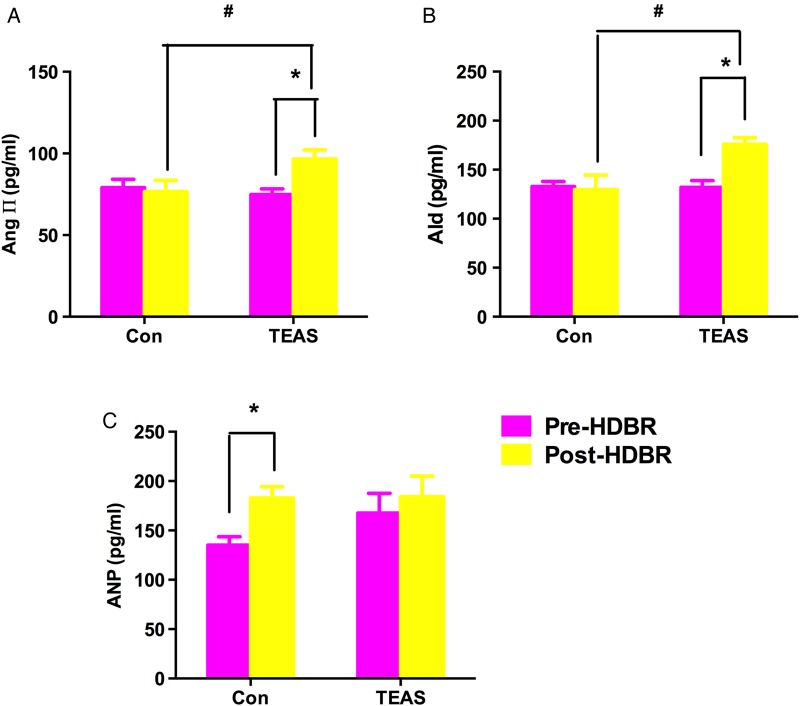
Volume-regulating hormones
Figure 4 shows the plasma concentrations of Ang II, Ald and ANP in the control and TEAS groups before and after 4 days of bed rest. Ang II and Ald were significantly increased by 129.3% and 133.3%, respectively, after 4-day HDBR in the TEAS group (p<0.05) but not in the control group. Moreover, the magnitude of Ang II and Ald increase after bed rest was significantly higher in the TEAS group than in the control group. ANP (135.2±18.8 pg/mL) increased significantly after 4 days of bed rest in the control group (182.8±25.7 pg/mL; p<0.05). In contrast, ANP tended to increase after 4 days of bed rest in the TEAS group, but not significantly.
Figure 4.
Changes in plasma Ald, Ang II and ANP concentrations before and after 4-day head-down bed rest (HDBR) in both the control (Con) and transcutaneous electrical acupuncture stimulation (TEAS) groups. (A) Changes in plasma Ang II concentrations before and after a 4-day HDBR. (B) Changes in plasma Ald concentrations before and after a 4-day HDBR. (C) Changes in plasma ANP concentrations before and after a 4-day HDBR. *p<0.05, versus before HDBR. Ald, aldosterone; Ang II, angiotensin; ANP, atrial natriuretic peptide. #p<0.05, versus the Con group.
Plasma volume change
Plasma volume changes calculated from the haematocrit before and after bed rest are listed in table 1. Plasma volume decreased after HDBR in the control group, suggesting hypovolaemia. The reduction in plasma volume in the TEAS group was not statistically significant.
Table 1.
Mean plasma volumes before and after 4-day HDBR in both the Con and TEAS groups
| Before HDBR | After HDBR | |
|---|---|---|
| Con | 2272±187 | 2157±138* |
| TEAS | 2212±180 | 2150±200 |
Values are expressed as mean±SD (mL).
*p<0.05 versus Con, before HDBR.
Con (control) group, without any countermeasures; TEAS group, received 30 min of TEAS treatment each day.
HDBR, head-down bed rest; TEAS, transcutaneous electrical acupuncture stimulation.
Discussion
This is the first study to examine the effects of TEAS used as a countermeasure against cardiovascular deconditioning during HDBR in humans. The main finding is that TEAS treatment for 30 min each day for 4 days produced a marked improvement in OT, primarily by changing volume-regulating hormone levels, improving cardiac performance, and activating the peripheral sympathetic nervous system.
Microgravity experienced during manned spaceflight may lead to long-term deregulated cardiovascular function, compromised OT, bone demineralisation, body fluid loss and muscular atrophy.2 10 Cardiovascular deconditioning is one of the biggest problems for space missions, and OI tends to appear on return to Earth.1 Deteriorating cardiac systolic function is the main factor contributing to cardiovascular deconditioning.11 EA at PC6 is known to increase stroke volume and cardiac output and alleviate haemorrhagic hypotension.4 6 In a previous study on hypotension, we also found that TEAS stimulation produced a remarkable improvement in OT through enhancement of cardiac performance and activation of the peripheral sympathetic nervous system.7 Clinical evidence indicates that acupuncture or TEAS has therapeutic effects on certain types of hypotension,7 arrhythmias12 and myocardial ischaemia.13 In the present study, we found that cardiac systolic function decreased significantly in the control group during HDBR (on days 3 and 4) and was associated with a tendency to decreased cardiovascular function; however, there were no marked changes in the TEAS group. Such observations suggest that TEAS treatment may help maintain OT by preventing cardiac deconditioning during HDBR as one possible mechanism. However, the reasons why TEAS protects against OI and cardiac deconditioning are still not fully understood and need to be further explored.
Autonomic dysregulation has been recognised as a crucial factor in cardiovascular deconditioning, with alteration of the sympathetic–parasympathetic balance.1 Previous studies have also found that spontaneous baroreflex sensitivity is reduced after bed rest and spaceflight.14 EA is known to influence haemodynamics and cardiovascular sympathoexcitatory responses.5 15 Previous studies have also demonstrated that electrical stimulation of the median nerve could enhance left ventricular contractility and sympathetic activity via a somatosympathetic reflex.4 15 Syuu et al4 reported that EA at PC6 could mimic the effect of median nerve stimulation to activate the sympathetic nervous system and cause a depressor response. Therefore, we selected TEAS at PC6 to test our hypothesis concerning the effect of TEAS treatment on cardiovascular function during a 4-day HDBR. In the present study, HFn decreased significantly after bed rest in both groups, indicating that HDBR significantly reduced cardiac parasympathetic activity, which is consistent with previous reports.14 Additionally, LFn/HFn as an indicator of cardiac sympathovagal balance in the TEAS group, increased more than in the control group after 4-day HDBR. These results suggest that daily TEAS treatment improves OT by enhancing cardiac performance and activating the peripheral sympathetic nervous system.
Astronauts have reduced OT on return to Earth. The precipitating event leading to syncope must be a reduction in cerebral blood flow sufficient to cause loss of consciousness. The mechanism most commonly invoked to explain OI after spaceflight is that cerebral blood flow declines secondary to hypotension.16 Many studies have suggested that spaceflight impairs cerebral autoregulation, and that this impairment contributes to OI after spaceflight, notwithstanding adequate autonomic BP control.16 17 In humans, spaceflight or simulated microgravity alters several factors involved in cerebral autoregulation such as blood volume and presumably vascular dimensions.17 We have previously shown that TEAS treatment improves OT through inhibiting the decrease in cerebral blood flow and increasing the tolerance of the brain to ischaemia.8 The principal findings of the present study are that CBFV of the right MCA during HDBR (on days 3 and 4) decreased significantly compared with values before HDBR in the control group. However, in the TEAS group, CBFV of the right MCA was not significantly changed. These factors may contribute to the maintenance of cerebrovascular function after 4-day HDBR in the TEAS group.
A number of studies have indicated that HDBR results in activation of the renin-angiotensin system (RAS), along with a decrease in autonomic function.18 This suggests that reductions in plasma volume are largely responsible for the observed changes in autonomic arterial baroreflex regulation after bed rest.19 We found that blood volume was significantly decreased after HDBR in the control group, which indicates that weightlessness could cause loss of plasma volume. However, we did not see significant changes in blood volume in the TEAS group. Therefore, daily TEAS treatment partially prevented a reduction in plasma volume after bed rest. In addition, we found that Ang II and Ald were significantly increased in the TEAS group compared with the control group. This indicates that TEAS treatment at PC6 may effectively maintain RAS activity. We therefore speculate that the sympathetic responses to TEAS treatment at PC6 may be induced both by neurohumoral activation of hormones and activation of the somatosympathetic reflex pathway. TEAS treatment ameliorated the reduction in plasma volume and thus the spontaneous arterial-cardiac baroreflex.
In conclusion, we have demonstrated that daily TEAS treatment at PC6 during 4-day HDBR produced a marked improvement in OT largely through up-regulation of both cardiac volume-regulating hormones and the peripheral sympathetic nervous system. Furthermore, TEAS partially maintained blood flow velocity in the MCA and cardiac function during simulated weightlessness. Therefore, the present study suggests that TEAS treatment could be a useful countermeasure against cardiovascular deconditioning induced by simulated microgravity. However, the efficiency of TEAS treatment for long-term simulated microgravity should be further investigated. Moreover, TEAS stimulation at PC6 may be a novel therapeutic method for the prevention or treatment of autonomic dysfunction.
Summary points.
Head-down bed rest (HDBR) simulates microgravity and provides a model for studying cardiovascular decomposition in spaceflight.
Transcutaneous electrical acupuncture stimulation (TEAS) significantly increased orthostatic tolerance compared with no treatment.
TEAS treatment reduces cardiac deconditioning induced by short-term HDBR.
Supplementary Material
Acknowledgments
We thank Dr Hui Ma, Department of Ultrasound Medicine, Xijing Hospital, for technical assistance when measuring cerebral blood flow and cardiac function.
Footnotes
Contributors: JS, YSZ and XQS: study conception and design; XTL, YCW, FS, YG and QL: collection, analysis and interpretation of data; JS, YSZ, XQS, XTL and QL: drafting the article or revising it critically for important intellectual content. All authors have read and approved the final manuscript.
Funding: This study was supported by grants from the National Natural Science Foundation of China (grant numbers 81301682, 81301681, 81171872 and 81372130).
Competing interests: None declared.
Ethics approval: This study was approved by the Medical Ethical Committee of Fourth Military Medical University.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Platts SH, Martin DS, Stenger MB, et al. Cardiovascular adaptations to long-duration head-down bed rest. Aviat Space Environ Med 2009;80:A29–36. 10.3357/ASEM.BR03.2009 [DOI] [PubMed] [Google Scholar]
- 2.Hargens AR, Bhattacharya R, Schneider SM. Space physiology VI: exercise, artificial gravity, and countermeasure development for prolonged space flight. Eur J Appl Physiol 2013;113:2183–92. 10.1007/s00421-012-2523-5 [DOI] [PubMed] [Google Scholar]
- 3.Clement G, Pavy-Le TA. Centrifugation as a countermeasure during actual and simulated microgravity: a review. Eur J Appl Physiol 2004;92:235–48. 10.1007/s00421-004-1118-1 [DOI] [PubMed] [Google Scholar]
- 4.Syuu Y, Matsubara H, Hosogi S, et al. Pressor effect of electroacupuncture on hemorrhagic hypotension. Am J Physiol Regul Integr Comp Physiol 2003;285:R1446–52. 10.1152/ajpregu.00243.2003 [DOI] [PubMed] [Google Scholar]
- 5.Li Z, Wang C, Mak AF, et al. Effects of acupuncture on heart rate variability in normal subjects under fatigue and non-fatigue state. Eur J Appl Physiol 2005;94:633–40. 10.1007/s00421-005-1362-z [DOI] [PubMed] [Google Scholar]
- 6.Syuu Y, Matsubara H, Kiyooka T, et al. Cardiovascular beneficial effects of electroacupuncture at Neiguan (PC-6) acupoint in anesthetized open-chest dog. Jpn J Physiol 2001;51:231–8. 10.2170/jjphysiol.51.231 [DOI] [PubMed] [Google Scholar]
- 7.Yin S, Cao Y, Zhang J. Treatment of primary hypotension by electroacupuncture at Neiguan and Gongsun—a report of 100 cases. J Tradit Chin Med 2004;24:193. [PubMed] [Google Scholar]
- 8.Sun J, Sang H, Yang C, et al. Electroacupuncture improves orthostatic tolerance in healthy individuals via improving cardiac function and activating the sympathetic system. Europace 2013;15:127–34. 10.1093/europace/eus220 [DOI] [PubMed] [Google Scholar]
- 9.Van Beaumont W. Evaluation of hemoconcentration from hematocrit measurements. J Appl Physiol 1972;32:712–13. [DOI] [PubMed] [Google Scholar]
- 10.Hargens AR, Richardson S. Cardiovascular adaptations, fluid shifts, and countermeasures related to space flight. Respir Physiol Neurobiol 2009;169(Suppl 1):S30–3. 10.1016/j.resp.2009.07.005 [DOI] [PubMed] [Google Scholar]
- 11.Yang CB, Wang YC, Gao Y, et al. Artificial gravity with ergometric exercise preserves the cardiac, but not cerebrovascular, functions during 4 days of head-down bed rest. Cytokine 2011;56:648–55. 10.1016/j.cyto.2011.09.004 [DOI] [PubMed] [Google Scholar]
- 12.Longhurst JC. Electroacupuncture treatment of arrhythmias in myocardial ischemia. Am J Physiol Heart Circ Physiol 2007;292:H2032–4. 10.1152/ajpheart.00071.2007 [DOI] [PubMed] [Google Scholar]
- 13.Yang L, Yang J, Wang Q, et al. Cardioprotective effects of electroacupuncture pretreatment on patients undergoing heart valve replacement surgery: a randomized controlled trial. Ann Thorac Surg 2010;89:781–6. 10.1016/j.athoracsur.2009.12.003 [DOI] [PubMed] [Google Scholar]
- 14.Hirayanagi K, Iwase S, Kamiya A, et al. Functional changes in autonomic nervous system and baroreceptor reflex induced by 14 days of 6 degrees head-down bed rest. Eur J Appl Physiol 2004;92:160–7. 10.1007/s00421-004-1067-8 [DOI] [PubMed] [Google Scholar]
- 15.Li P, Ayannusi O, Reid C, et al. Inhibitory effect of electroacupuncture (EA) on the pressor response induced by exercise stress. Clin Auton Res 2004;14:182–8. [DOI] [PubMed] [Google Scholar]
- 16.Iwasaki K, Levine BD, Zhang R, et al. Human cerebral autoregulation before, during and after spaceflight. J Physiol 2007;579:799–810. 10.1113/jphysiol.2006.119636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levine BD, Pawelczyk JA, Ertl AC, et al. Human muscle sympathetic neural and haemodynamic responses to tilt following spaceflight. J Physiol 2002;538:331–40. 10.1113/jphysiol.2001.012575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grenon SM, Hurwitz S, Xiao X, et al. Readaptation from simulated microgravity as a stimulus for improved orthostatic tolerance: role of the renal, cardioendocrine, and cardiovascular systems. J Investig Med 2005;53:82–91. [DOI] [PubMed] [Google Scholar]
- 19.Iwasaki K, Shiozawa T, Kamiya A, et al. Hypergravity exercise against bed rest induced changes in cardiac autonomic control. Eur J Appl Physiol 2005;94:285–91. 10.1007/s00421-004-1308-x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.