Abstract
Objective
To examine the correlation between HIV prevalence and male circumcision and other foreskin cutting practices across the four regions of Papua New Guinea (PNG).
Design
An ecological substudy using unique data from an interdisciplinary research programme to evaluate the acceptability, sociocultural context and public health impact of male circumcision for HIV prevention in PNG.
Methods
Published data describing (a) self-reported circumcision status by region from the ‘Acceptability and Feasibility of Male Circumcision for HIV prevention in PNG’ study and (b) HIV prevalence by region from PNG National Department of Health were used to correlate male circumcision and other foreskin cutting practices and HIV prevalence. Maps were constructed to visually represent variations across the four regions of PNG.
Results
Regions of PNG with the highest HIV prevalence had the lowest prevalence of male circumcision and other forms of foreskin cutting and vice versa. Male circumcision and dorsal longitudinal cuts were strongly associated with HIV prevalence and able to explain 99% of the observed geographical variability in HIV prevalence in PNG (p<0.01).
Conclusions
The regional prevalence of HIV infection in PNG appears to be closely correlated with the regional distribution of male circumcision and dorsal longitudinal foreskin cuts. Further research is warranted to investigate causality of this correlation as well as the potential of dorsal longitudinal cuts to confer protection against HIV acquisition in heterosexual men.
Keywords: HIV, CIRCUMCISION, EPIDEMIOLOGY (GENERAL), PUBLIC HEALTH
Introduction
Male circumcision has been conclusively shown to reduce the risk of heterosexual HIV acquisition in men by around 60%.1–4 Epidemiological evidence from countries with heterosexually driven epidemics indicates that populations with relatively high prevalence of male circumcision have relatively low prevalence of HIV.5 Within-country variations have also been described.6
Papua New Guinea (PNG) has the highest prevalence of HIV, syphilis and other sexually transmitted infections among Asia-Pacific countries.7 The HIV epidemic in PNG is primarily linked to heterosexual transmission, and over half of all reported HIV diagnoses come from just three of its 22 provinces.8 PNG has an estimated general adult HIV prevalence of 0.6%–0.8%, but there are significant variations in prevalence by geographical region and in different subpopulations.8 HIV prevalence of 12%–17% has been observed among women and men who sell and/or exchange sex, and antenatal prevalence of around 2% is reported in several Highland provinces.8 PNG is an extremely diverse nation of seven million people who live in locations ranging from remote coral atolls to mountain-top villages to cosmopolitan provincial towns and cities. PNG has over 800 mutually unintelligible local languages with people from different cultural groups conversing in English or PNG's lingua franca Tok Pisin (PNG Pidgin). Accordingly, there are myriad sociocultural practices across the country, including a wide variety of penile modification practices.9 10 These modifications include the complete removal of the foreskin (male circumcision), several variations of longitudinal foreskin cutting, insertion of objects under the penile skin, injection of fluids along the penile shaft and/or a combination of these practices.11–14
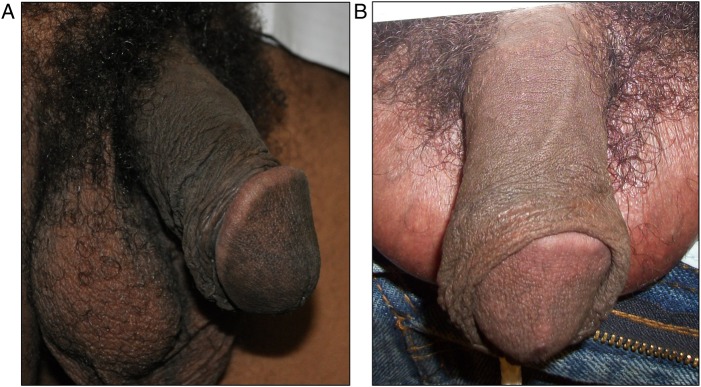
In earlier research by our group,11–15 we observed high prevalence of the dorsal longitudinal cut among men in PNG. Dorsal longitudinal cuts resulted in the complete exposure of these the glans and inner foreskin in 63% of men, with the final appearance closely resembling that of medical circumcision (figure 1).11 We have previously postulated12–14 that the dorsal longitudinal cut may confer some degree of protection against HIV acquisition in men in a similar way to full removal of the foreskin. This is because the lateral retraction and eversion of the foreskin that follows a full-length dorsal longitudinal cut closely resembles medical circumcision.11
Figure 1.
(A) Dorsal longitudinal foreskin cut causing complete exposure of the glans: lateral retraction and eversion of foreskin that results in appearance similar to medical circumcision, but with redundant skin at the sides and undersurface of the penile shaft. (B) Dorsal longitudinal foreskin cut causing partial exposure of the glans: partial retraction of foreskin that results in appearance of a ‘short’ foreskin.
We conducted an ecological study to compare geographical variations in HIV prevalence with the prevalence of male circumcision and dorsal longitudinal cut in different regions in PNG. This was done in order to make inferences in regard to the potential impact of these practices on the HIV epidemic in this setting.
Methods
Self-reported male circumcision status data from the ‘Acceptability and Feasibility of Male Circumcision for HIV prevention in PNG’ study were collated and disaggregated by province and region. A detailed description of the field study design, methodology and data have previously been published.11 13 15 16 In brief, an observational cross-sectional study was conducted among men in four locations in the period between July 2010 and February 2011: two ‘rural development’ communities (Higaturu Oil Palms, Popondetta, Oro Province, and Porgera Joint Venture, Porgera, Enga Province) and two institutes of higher education (Pacific Adventist University, Port Moresby, National Capital District, and Divine Word University, Madang, Madang Province). These sites enabled access to men from a wide variety of sociocultural, religious and educational backgrounds from each of the country's four geographical regions. Following the completion of informed consent procedures, participants were asked to complete a self-administered questionnaire to capture demographic and sexual behavioural information; and to review a seven-level classification figure of penile foreskin cutting that included photographs with a written description. Questionnaires were in both English and Tok Pisin, and participants chose the language that best suited them. For each of the seven types of cut, men were asked to circle the number beside the picture that most closely resembled their own foreskin. Participants having poor levels of literacy were assisted in completion of the questionnaire by a trained interviewer. Participants could choose to have assistance in either English or Tok Pisin.
HIV surveillance data from the PNG National Department of Health in the same period (2010)17 were collated and disaggregated by province and region. Foreskin cutting data and HIV prevalence data were entered into an Excel spreadsheet, and subsequently analysed by linear regression analysis using SPSS V.19.0 (IBM software, USA). Tabulated data were used to construct maps indicating variations in HIV prevalence and foreskin cutting in each of PNG's four regions (Southern, Highlands, Momase and New Guinea Islands) using MapInfo Professional V.12.0 (Pitney Bowes Software, USA).
Ethics
Ethical approval was granted by the Human Research Ethics Committees of Pacific Adventist University, Divine Word University, James Cook University (Australia) and the PNG National AIDS Council. Endorsement was also provided by the Provincial AIDS Committees of the National Capital District, and Enga, Oro and Madang Provinces.
Results
The prevalence of male circumcision (ie, complete removal of the foreskin) varied from 8%–9% in the Southern and Highlands Regions to 13% in Momase and 23% in New Guinea Islands (table 1). The prevalence of dorsal longitudinal cut of the penile foreskin varied from 42% in the Southern Region, 45% in Highlands, 50% in New Guinea Islands and 58% in Momase Region. The proportion of men reporting no foreskin cut was, therefore, 50%, 46%, 29% and 27% in Southern, Highlands, Momase and New Guinea Islands Regions, respectively. The National Department of Health estimated that adult HIV prevalence in 2010 (the time of the above study) was 1.17%, 1.02%, 0.63% and 0.61% in Southern, Highlands, Momase and New Guinea Islands, respectively (table 1, figure 2).
Table 1.
HIV prevalence and foreskin cutting by region
| HIV prevalence (%) | No foreskin cut (%) | Circumcision (full removal) (%) | Dorsal longitudinal cut (%) | |
|---|---|---|---|---|
| New Guinea Islands | 0.61 | 26.5 | 23.1 | 50 |
| Momase | 0.63 | 28.8 | 13.1 | 58.2 |
| Highlands | 1.02 | 46.1 | 9.2 | 44.6 |
| Southern | 1.17 | 50.4 | 7.5 | 42.1 |
Figure 2.
Prevalence of HIV, male circumcision (full removal of the foreskin) and dorsal longitudinal foreskin cut across the four regions of Papua New Guinea.
Foreskin cutting (circumcision or dorsal longitudinal cut) was strongly and significantly associated with lower HIV prevalence (coefficient of determination, r2=0.9923; p=0.004), accounting for more than 99% of the observed geographical variability in HIV prevalence.
The median lifetime number of female sexual partners varied significantly across the four regions (NGI 5, Momase 5, Highlands 6, Southern 8; p<0.05), but there was no significant difference observed in other risk factors for HIV acquisition such as condom use at last sex (NGI 36.7%, Momase 37.6%, Highlands 32.2%, Southern 30.2%; p=0.513) or homosexual anal sex across the regions (NGI 4.3%, Momase 4.0%, Highlands 4.9%, Southern 3.7%; p=0.901).
Discussion
The geographical distribution of HIV infection in PNG mirrors the distribution of foreskin cutting (circumcision or dorsal longitudinal cut): regions having the highest prevalence of male circumcision or dorsal longitudinal cut had the lowest prevalence of HIV. No statistically significant geographical variation was observed in other risk factors for HIV acquisition, except median lifetime number of female sexual partners.
This finding supports our hypothesis that dorsal longitudinal cut may confer a similar level of protection as male circumcision against HIV acquisition in men.11–14 Our earlier finding that men with a dorsal longitudinal cut had a significantly lower incidence of syphilis compared with men without a foreskin cut12 further supports our hypothesis, and is consistent with research in other settings, which indicates that male circumcision is protective against syphilis and Herpes simplex virus type 2.18 Our earlier study was, however, underpowered to detect a difference in HIV prevalence or incidence among men with a foreskin cut compared with those without.12
Caution is warranted in the direct (causal) interpretation of our current findings. As in any ecological study, there is a risk of ecological fallacy, that is, to interpret an association as causal when, in fact, it is due to uncontrolled confounding and the differing impact of bias on the independent datasets being compared. Ecological studies are, however, extremely valuable for generating hypotheses that can then be investigated in more detailed epidemiological research conducted among individuals. Ongoing clinical, immunohistological and epidemiological research by our group is investigating the association and mechanisms by which alternative forms of foreskin cutting such as the dorsal longitudinal cut may protect men against HIV infection in this setting.19 20 This research will provide further evidence on the potential role that these forms of foreskin cutting may have in future culturally sensitive HIV prevention programmes in countries such as PNG, where such practices are common, and where, for logistical and cultural reasons, it may be problematic to effectively implement male circumcision programmes at a population level.
Key messages.
Alternative forms of penile foreskin cutting may be associated with reduced HIV infection risk in Papua New Guinea.
Regions of Papua New Guinea with the highest HIV prevalence had the lowest prevalences of male circumcision and other forms of foreskin cutting.
Male circumcision and dorsal longitudinal cuts were strongly associated with HIV infection and able to explain 99% of the observed geographical variability in HIV prevalence.
Further research is warranted to confirm whether the dorsal longitudinal foreskin cut may confer protection against HIV in this setting.
Footnotes
Handling editor Jackie A Cassell
Contributors: JMK and WJHM conceived of the study and provided overall guidance. RM, GCK, DJM and AJV conducted the analyses, and prepared the first draft of the manuscript. RT coordinated fieldwork and data management for the ‘Acceptability and Feasibility of Male Circumcision for HIV prevention in PNG’ study and provided cultural guidance and interpretation of results. DJM and AJV finalised the manuscript based on comments from other authors. All authors reviewed and approved the final version of the manuscript.
Funding: This research was funded by the National Health and Medical Research Council, Australia (Project Grant 601003), and the Australian Agency for International Development (Australian Development Research Award 44743).
Competing interests: None declared.
Ethics approval: James Cook University Human Ethics Research Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Auvert B, Taljaard D, Lagarde E, et al. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med 2005;2:e298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet 2007;369:643–56. [DOI] [PubMed] [Google Scholar]
- 3.Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet 2007;369:657–66. [DOI] [PubMed] [Google Scholar]
- 4.WHO/UNAIDS. Press Release: WHO and UNAIDS announce Recommendations from Expert Meeting on Male Circumcision for HIV Prevention. Geneva: World Health Organization (WHO) and the Joint United Nations Programme on HIV/AIDS (UNAIDS), 2007. [Google Scholar]
- 5.Moses S, Bradley JE, Nagelkerke NJ, et al. Geographical patterns of male circumcision practices in Africa: association with HIV seroprevalence. Int J Epidemiol 1990;19:693–7. [DOI] [PubMed] [Google Scholar]
- 6.Jansen HA, Morison L, Mosha F, et al. Geographical variations in the prevalence of HIV and other sexually transmitted infections in rural Tanzania. Int J STD AIDS 2003;14:274–80. [DOI] [PubMed] [Google Scholar]
- 7.Vallely A, Page A, Dias S, et al. The prevalence of sexually transmitted infections in Papua New Guinea: a systematic review and meta-analysis. PLoS ONE 2010;5:e15586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.NAC. Papua New Guinea 2013 HIV/AIDS estimations and projections. Port Moresby: National AIDS Council, Government of Papua New Guinea, 2013. [Google Scholar]
- 9.Manineng C, MacLaren D. Medically assisted circumcision: a safer option for initiation rites. Med J Aust 2014;201:610–11. [DOI] [PubMed] [Google Scholar]
- 10.Buchanan H, Frank R, Couch M, et al. The Re-Making of men and penile modification. In: Manderson L. eds. Technologies of sexuality, identity and sexual health. London: Routledge Press, 2012. [Google Scholar]
- 11.MacLaren D, Tommbe R, Mafile OT, et al. Foreskin cutting beliefs and practices and the acceptability of male circumcision for HIV prevention in Papua New Guinea. BMC Public Health 2013;13:818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vallely A, Ryan CE, Allen J, et al. High prevalence and incidence of HIV, sexually transmissible infections and penile foreskin cutting among sexual health clinic attendees in Papua New Guinea. Sex Health 2014;11:58–66. [DOI] [PubMed] [Google Scholar]
- 13.Vallely A, MacLaren D, Kaleva W, et al. Male circumcision for HIV prevention in Papua New Guinea: summary of research evidence and recommendations for public health policy following a National Policy Forum. PNG Med J 2011;54:91–108. [PubMed] [Google Scholar]
- 14.Hill PS, Tynan A, Law G, et al. A typology of penile cutting in Papua New Guinea: results of a modified Delphi study among sexual health specialists. AIDS Care 2012;24:77–86. [DOI] [PubMed] [Google Scholar]
- 15.Tommbe R, MacLaren D, Redman-MacLaren M, et al. Researching male circumcision for HIV prevention in Papua New Guinea: a process that incorporates science, faith and culture. Health Res Policy Syst 2013;11:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jayathunge P, McBride WJ, MacLaren D, et al. Men in Papua New Guinea Accurately Report Their Circumcision Status. PLoS ONE 2015;10:e0123429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National AIDS Council of Papua New Guinea. 2010 HIV Estimates. Port Moresby: National AIDS Council, Government of Papua New Guinea, 2011. [Google Scholar]
- 18.Mugo N, Dadabhai SS, Bunnell R, et al. Prevalence of herpes simplex virus type 2 infection, human immunodeficiency virus/herpes simplex virus type 2 coinfection, and associated risk factors in a national, population-based survey in Kenya. Sex Transm Dis 2011;38:1059–66. [DOI] [PubMed] [Google Scholar]
- 19.Gray R, Vallely A, Wilson D, et al. The impact of male circumcision on the HIV epidemic in Papua New Guinea: a country with extensive foreskin cutting practices. PLoS ONE 2014;9:e104531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vallely A, MacLaren D, David M, et al. Dorsal longitudinal slit of the penile foreskin may protect men against HIV acquisition in Papua New Guinea. Presentation at 8th International AIDS Society Conference on HIV Pathogenesis, Treatment and Prevention; Vancouver, Canada, 19–22 July 2015. [Google Scholar]