Abstract
A 52-year-old Hispanic woman presented to the emergency department, reporting worsening sharp lower right quadrant abdominal pain for 3 days. CT of the abdomen and pelvis showed evidence of inflammation in the peritoneal soft tissues adjacent to an enlarged and thick-walled appendix, an appendicolith, no abscess formation and a slightly thickened caecum consistent with acute appendicitis. During laparoscopic appendectomy, the caecum was noted to be firm, raising suspicion of malignancy. Surgical oncology team was consulted and open laparotomy with right hemicolectomy was performed. Pathology reported that the ileocaecal mass was not a malignancy but was, rather, actinomycosis. The patient was discharged after 10 days of intravenous antibiotics in the hospital, with the diagnosis of abdominal actinomycosis. Although the original clinical and radiological findings in this case were highly suggestive of acute appendicitis, abdominal actinomycosis should be in the differential for right lower quadrant pain as it may be treated non-operatively.
Background
There are a number of disorders associated with masses in the ileocaecal region. One of the most common causes is acute appendicitis—a surgical emergency. Each year, thousands of appendectomies are performed in the USA. Other typical causes of ileocaecal masses include infection, inflammation, neoplasm and drug related. The most common causes include acute appendicitis, colon cancer and Crohn's disease. This case report describes a rare cause of an ileocaecal mass, actinomycosis.
Abdominal actinomycosis is a rare cause of ileocaecal lesions. It is often a diagnosis of exclusion, and is not made until more common causes such as colon cancer, carcinoid tumours or Crohn's disease are excluded. Actinomycosis is most common in middle-aged men, making our case even more unusual, as it was present in a middle-aged woman.
Actinomyces, a Gram-positive filamentous anaerobe, is part of the normal flora of the oral cavity, gastrointestinal tract and vagina. The most common cause of human actinomycosis is Actinomyces israelii. Actinomyces remains commensal and rarely causes infection in the absence of necrotic tissue. However, when pathological, it causes a chronic granulomatous disease, actinomycosis. Because Actinomyces does not cause invasive infection without necrotic tissue, it is most common after trauma. Common causes of trauma leading to actinomycosis include cholecystectomy, abdominal surgery, dental procedures and intrauterine device use.
The majority of actinomycosis cases are extra-abdominal, with 50% of cases being cervicofacial. Only 20% of actinomycosis cases consist of abdominal infection. Abdominal actinomycosis is typically localised to the appendix and ileocaecal region. The infection very rarely disseminates and generally spreads contiguously. Actinomyces is a slow-growing anaerobe. Owing to this fact, patients with previous cholecystectomy have been found to have abdominal actinomycosis many years after surgery. Abdominal actinomycosis can be chronic and indolent or can manifest as palpable masses, fistulas and draining sinus tracts.
A major clinical dilemma is being able to diagnose abdominal actinomycosis preoperatively. Clinical manifestations are vague and non-specific, consisting of symptoms such as fatigue, fever, weight loss and abdominal pain. Only 10% of abdominal actinomycosis cases are diagnosed preoperative, usually due to more obvious signs such as a palpable mass, sinus tracts and fistulas. Actinomyces can be identified by the formation of Sulfur Granules or clusters of filamentous branching Gram-positive rods. While indicative of actinomycosis, Sulfur Granules are not pathognomonic. Currently, most diagnosed cases of abdominal actinomycosis are made postoperatively and confirmed by pathology.
Diagnosis is difficult to make solely on radiological findings due to the non-specific nature of the disease. CT-guided percutaneous aspiration can help make a diagnosis of abdominal actinomycosis if Sulfur Granules and cultures are positive. The gold standard for diagnosis is pus positive for Sulfur Granules and culture of Actinomyces. Colonoscopic findings can vary from normal mucosa to thickened, inflamed or ulcerated mucosa. A button-like nodular lesion and inverted appendiceal orifice can also be seen on colonoscopy. However, the differential diagnosis of these findings includes Crohn's disease, Carcinoid tumours and other neoplasms, as well as actinomycosis. Biopsy of lesions suspicious for malignancy can occasionally yield a preoperative histologic diagnosis of abdominal actinomycosis.
Treatment usually involves resection, as the diagnosis of abdominal actinomycosis is usually not made preoperatively. However, medical therapy with antibiotics can be used if a preoperative diagnosis is made. The antibiotic of choice is intravenous penicillin G. Intravenous penicillin for 3–6 weeks followed by 6–12 months of oral therapy is recommended. Tetracycline, erythromycin and clindamycin are alternatives.
Case presentation
A 52-year-old Hispanic woman presented to the emergency department, with worsening sharp lower right quadrant abdominal pain for 3 days. There was no radiating pain. There were no alleviating or aggravating factors. Review of systems was positive for nausea. All other reviews of systems were negative. On physical examination, the abdomen was soft and non-distended. There was moderate tenderness in the right lower quadrant and positive rebound tenderness. Bowel sounds were present and normal. Pertinent medical history included a cholecystectomy. Pertinent social history included no history of tobacco, alcohol or drug use.
Laboratory tests at the time of admission included white cell count 12 100/μL; mostly neutrophils 9 100/μL. The patient was afebrile with a temperature of 37.6°C. Pertinent imaging included a CT of the abdomen and pelvis, in the emergency department. The diagnosis made after CT was acute appendicitis (figure 1). General surgery was then consulted. After evaluation by the surgeon, the patient was admitted and taken to the operating room for a laparoscopic appendectomy.
Figure 1.
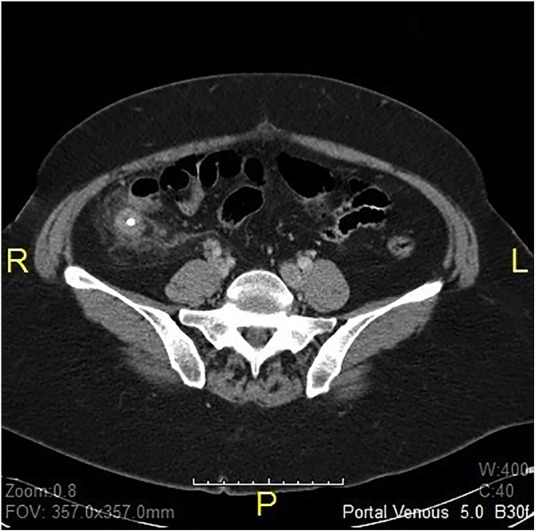
Abdomen/pelvis CT: there is inflammation in the peritoneal soft tissues adjacent to an enlarged and thick-walled appendix. An appendicolith is also seen. The findings are consistent with acute appendicitis. No abscess formation is seen. There is slight thickening of the caecum, consistent with inflammatory change.
The operation began as a laparoscopic appendectomy but after dissection and visualisation of the appendix, it was noted that the appendix was non-mobile. Furthermore, the surgeon noted that the caecum felt quite firm, raising suspicion of malignancy. No evidence of metastatic disease was seen on laparoscopic examination. On open laparotomy, the surgical oncologist decided that the mass was suspicious for malignancy, and proceeded with right hemicolectomy. A specimen containing the ascending colon, caecum, appendix and distal ileum was sent to pathology.
The pathology report was negative for malignancy or benign neoplasm. However, the report did note abscesses in the caecum and appendiceal orifice, with Gram-positive filamentous bacteria suggestive of actinomycetes (figure 2). An area of acute and organising abscess arising in the caecum, surrounding the appendiceal orifice and involving the base of the appendix, was noted by pathology. There was also marked oedema of the surrounding pericolic tissues with degenerative cellular changes within the muscularis and subserosal fat necrosis. Distal margins were viable and without significant inflammation or evidence of malignancy.
Figure 2.
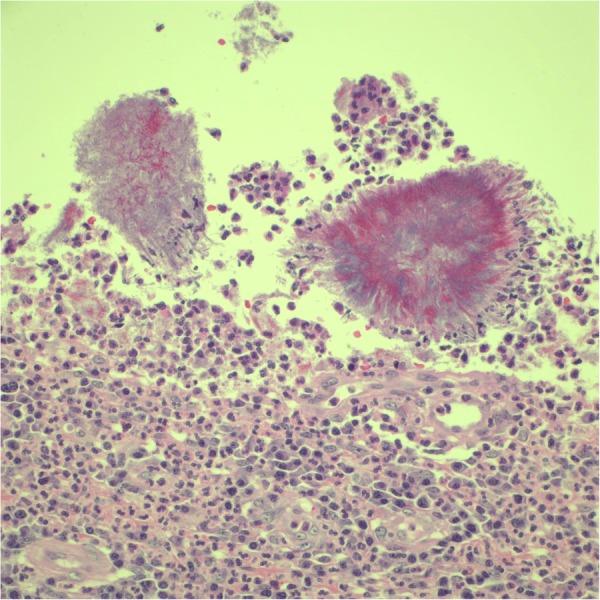
Histology: Actinomyces and Sulfur Granule—Gram-positive filamentous bacteria.
The diagnosis of abdominal actinomycosis was made and infectious disease was consulted. Infectious disease concurred with the diagnosis of gastrointestinal actinomycosis and recommended intravenous Unasyn (ampicillin and sulbactam). A 4-week intravenous course of Unasyn therapy was prescribed. This was to be followed by 6–12 months of oral antibiotics per infectious disease.
Differential diagnosis
Based on the initial clinical and radiological findings of leucocytosis, right lower quadrant abdominal pain, appendicolith and appendiceal inflammation, the initial diagnosis was acute appendicitis. However, on finding a mass lesion at the ileocaecal junction, the differential diagnosis included malignancy, Crohn's disease and abdominal actinomycosis. The treatment of malignancy, Crohn's disease and abdominal actinomycosis can include surgical resection and anastomoses. However, conservative medical treatment can be used for Crohn's disease and abdominal actinomycosis if the diagnosis is made preoperatively. Actinomycosis can be treated with long-term antibiotic therapy, specifically penicillin.
Treatment
Treatment of abdominal actinomycosis depends on whether the diagnosis is made preoperatively or postoperatively. The recommended nonsurgical treatment for abdominal actinomycosis is intravenous penicillin G for 2–6 weeks followed by oral penicillin or amoxicillin for 6–12 months. For those allergic to penicillin, alternatives include tetracycline, erythromycin or clindamycin. Surgery is reserved for patients who do not respond to initial antibiotic therapy or for patients in whom there is severe spread of the disease as noted by fistulas, necrosis or abscesses. Surgery is also indicated if malignancy cannot be ruled out. Postsurgical treatment includes long-term penicillin therapy. Mortality is extremely rare and favourable outcomes are seen in 90% of cases treated with combined medical and surgical therapy.
Outcome and follow-up
The patient made a full recovery from surgery. She will need follow-up with both surgical oncology and infectious disease for medical management of abdominal actinomycosis. Treatment with oral Unasyn—ampicillin and sulbactam—for 6–12 months should be sufficient to treat the actinomycosis infection. Appropriate measures reduce mortality rates to <10%, and also lower the risk of reoccurrences.
Discussion
This case represents a typical presentation of abdominal actinomycosis infection that was confounded by it mimicking acute appendicitis and malignancy. As with many other cases, the true diagnosis was not made until after pathological studies were completed.1 Typically, abdominal actinomycosis is low on the differential list because it is not common and mimics many other diseases. In this case, the rapid onset and CT findings were highly suspicious for acute appendicitis. However, once the laparoscopic appendectomy had begun, the surgeon suspected a malignancy and changed the procedure into an open laparotomy. Intersurgical diagnosis was made as likely neoplasm, which was finally changed to actinomycosis on completion of pathological studies. Similar cases are presented in the current literature. Karateke et al2 described three cases of abdominal actinomycosis that were diagnosed postoperatively. The first case was described as an internal abdominal wall mass, the second case as an acute abdomen with suspicion of malignancy, and the third case was an acute appendicitis. These three cases highlight the variability in the presentation of actinomycosis infections as well as the common postoperative diagnosis. Ferrari et al3 also described a case of large bowel actinomycosis infection that was diagnosed preoperatively as suspected perforation secondary to diverticulitis and then postoperatively by pathology. Treatment typically consists of surgical resection followed by high-dose intravenous penicillin for approximately 4 weeks. After the course of intravenous antibiotics is completed, transition should be made to oral antibiotic treatment, which is typically penicillin or amoxicillin. This treatment should last for 6–12 months.4 Although abdominal actinomycosis is a rare cause of bowel dysfunction, it is important to recognise and properly treat it, to prevent recurrence. Clinical diagnosis is extremely difficult, and this disease process shows the importance of good pathological studies.
Learning points.
Abdominal actinomycosis should be in the differential diagnosis for right lower quadrant abdominal pain. Other causes include malignancy, Crohn's disease, acute appendicitis or tuberculosis.
Less than 10% of abdominal actinomycosis cases are diagnosed preoperatively.
A preoperative diagnosis allows for non-surgical medical management, which is typically long-term intravenous penicillin.
Abdominal actinomycosis can cause mechanical bowel obstruction due to mass effect.
Acknowledgments
The authors would like to thank Dr Dan Galvan for his contribution to this case and to the care of the patient in the index operation of acute appendicitis. He was the Primary General Surgeon. They would also like to thank Dr Saju Joseph for his contribution and collaboration.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Harris LA, Decosse JJ, Dannenberg A. Abdominal actinomycosis: evaluation by computed tomography. Am J Gastroenterol 1989;84:198–201. [PubMed] [Google Scholar]
- 2.Karateke F, Ozyazici S, Menekşe E et al. Unusual presentations of actinomycosis; anterior abdominal wall and appendix: report of three cases. Balkan Med J 2013;30:315–17. 10.5152/balkanmedj.2012.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferrari TC, Couto CA, Murta-Oliveira C et al. Actinomycosis of the colon: a rare form of presentation. Scand J Gastroenterol 2000;35:108–9. 10.1080/003655200750024623 [DOI] [PubMed] [Google Scholar]
- 4.Hamid D, Baldauf JJ, Cuenin C et al. Treatment strategy for pelvic actinomycosis: case report and review of literature. Eur J Obstet Gynecol Reprod Biol 2000;89:197–200. 10.1016/S0301-2115(99)00173-6 [DOI] [PubMed] [Google Scholar]


