Abstract
POEMS syndrome is a rare hematological disorder associated with plasma cell dyscrasia characterized by polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy and skin changes. Castleman disease is a lymphoproliferative disorder that can be present in POEMS patients, which can be defined as Castleman disease variant of POEMS syndrome. Herein, we described a 24-year-old male patient diagnosed with this syndrome and also suffered from multiple cerebral infarctions. This patient showed no evidence of monoclonal gammopathy and failed to have electromyography examined. The final diagnosis was established with the help of the axillary lymph node biopsy. As a rare case of POEMS syndrome without evidence fulfilling the major mandatory diagnostic criteria and with cerebrovascular involvement, its characteristics was discussed with a brief literature review in order to facilitate further understanding of the POEMS syndrome.
Keywords: POEMS syndrome, Castleman disease, cerebral infarction, diagnosis
Introduction
POEMS syndrome, characterized by polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes, is a rare paraneoplastic syndrome associated with plasma cell dyscrasia. The pathogenesis of POEMS remains currently unknown, despite several theories such as overproduction of cytokines like Interleukin-6 (IL-6) and serum vascular endothelial growth factor (VEGF) have been proposed [1,2]. Castleman disease is a rare lymphoproliferative disorder. The disease is pathologically classified into three types: hyaline vascular disease, plasma cell disease, and mixed type. It is estimated that about 11%~30% of patients who were diagnosed with POEMS syndrome and received lymph node biopsy have evidence of concomitant Castleman disease [3].
The POEMS syndrome has an influence on the systemic vasculature, thus resulting in an inclination to thrombosis formation [4]. However, the cerebrovascular involvement associated with POEMS and Castleman disease is rare. In this report, we present a patient with Castleman disease variant of POEMS syndrome, who also suffered from multiple cerebral infarctions.
Case report
A 24-year-old male was initially admitted to our hospital with a 2-month history of fever and polyserositis. His family history was noteworthy that his mother was suffering from tuberculouspleuritis. He was diagnosed with tuberculosis in a local clinic and treated with antitubercular agent (isoniazide, rifampicin, ethambutol and pyrazinamide). After 1-month of medication, his condition worsened with newly developed symptoms of numbness of the upper extremities and blurred vision. His past medical history was unremarkable. He had no history of smoking, alcohol consumption, or drug abuse. He had a 15-kilogram weight loss during the past 2 months. Physical examination showed a thin man with a diffuse dark appearance with white nails. He had several non-tender enlarged lymph nodes, each measuring about 1.0×1.5 cm, spreading in his middle neck triangles, fossa axillaris and groin.
Laboratory tests revealed white blood cells (WBC) 10.1×109/L, hemoglobin 122 g/L, platelets 565×109/L, alanine transaminase 2 U/L, Creatinine 181 μmol/L, serum protein electrophoresis and immunofixation electrophoresis(-), Thyroid stimulating hormone (TSH) 15.930 mU/L, Free T4 2.0 pmol/L, testosterone 0 μg/L, prolactin 27.01 pg/L, serum tumor markers were within normal range. Ophthalmic fundus examination showed bilateral papilledema. Computed tomography (CT) scan of the thorax and abdomen revealed gynecomastia, polyserositis and multiple lymphadenectasis, without evidence of malignant tumor (Figure 1).
Figure 1.
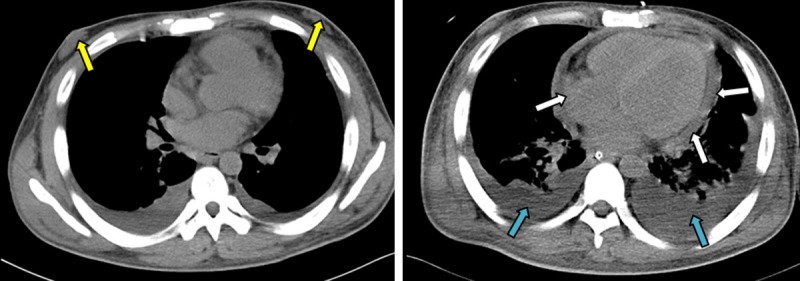
CT scan of the thorax showed gynecomastia (yellow arrow) and pleural effusion (blue arrow), pericardial effusion (white arrow).
During hospitalization, the patient developed symptoms of headache and nausea, and experienced three 10-min episodes of dysarthria. Soon his condition deteriorated and showed symptoms of moter aphasia with incontinence and disorientation. Lumbar puncture showed remarkable elevated pressure of the cerebrospinal fluid (CSF), which exceeded 330 mm H2O. CSF analysis revealed slightly elevated protein of 0.86 g/L. Magnetic Resonance Imaging (MRI) of the brain revealed a medium-size focal area of cerebral infarction near the left ventricle (Figure 2A). A follow-up CT scan of the brain was performed because of disturbance of consciousness, which showed a newly emerged area of cerebral infarction near the right ventricle (Figure 2B). Further analysis of the VEGF was made, which showed a remarkably elevated value of 7046 ng/L. Histological examination of the Axillary lymph node revealed lymphoid hyperplasia and plasma cell infiltration, with interfollicular vascularisation (Figure 3A). Immunohistochemistry demonstrated that the plasma cells in the interfollicular area were CD138 positive (Figure 3B), and CD34 staining showed the interfollicular vascular hyperplasia (Figure 3C). The patient was finally diagnosed with Castleman disease variant of POEMS syndrome and immediately treated with lenalidomide (10 mg/day) and dexamethasone (20 mg per week). Despite the treatment, the patient’s condition deteriorated into recurrent epilepsy, renal failure and respiratory failure. The patient quit further therapy after 7 days of medication and died during follow-up within a week.
Figure 2.
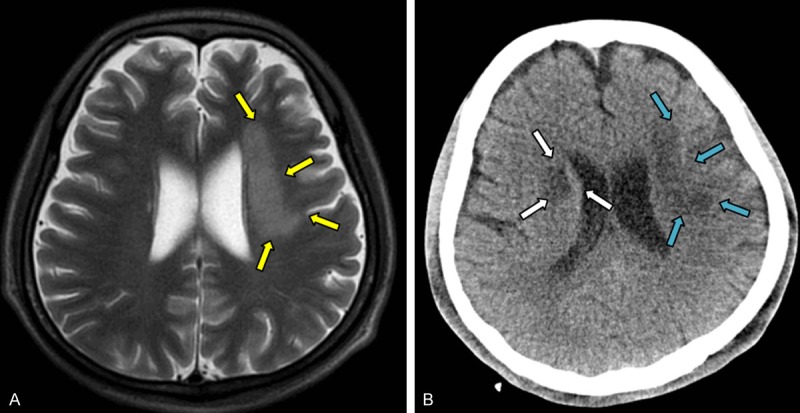
(A) MRI of the brain showed a medium-size focal area of cerebral infarction near the left ventricle (yellow arrow). (B) A follow-up CT scan of the brain showed a newly emerged area of cerebral infarction near the right ventricle (white arrow) in addition to the prior cerebral infarction area (blue arrow) (B).
Figure 3.
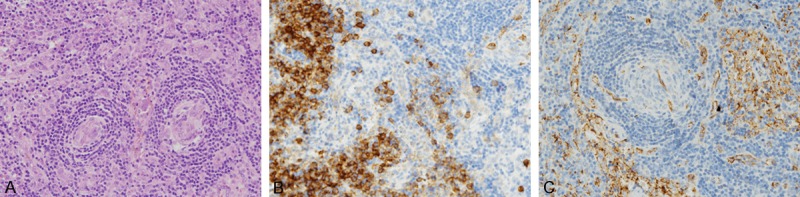
A: Histological examinations stained with hematoxylin and eosin revealed lymphoid hyperplasia and plasma cell infiltration, with interfollicular vascularization, ×20. B: Immunohistochemical staining showed that the plasma cells in the interfollicular area were CD138 positive, ×20. C: Immunohistochemical staining of CD34 showed interfollicular vascular hyperplasia, ×20.
Discussion
POEMS syndrome is a rare disorder characterized by polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes. The diagnostic criteria of POEMS syndrome include major mandatory criteria, other major criteria and minor criteria [5]. To be specific, major mandatory criteria include polyneuropathy and monoclonal gammopathy, both of which must be present for the diagnosis. Other major criteria include Castleman disease, sclerotic bone lesions and VEGF elevation. Minor criteria include organomegaly (splenomegaly, hepatomegaly, or lymphadenopathy), extravascular volume overload (edema, pleural effusion, or ascites), endocrinopathy (adrenal, thyroid, pituitary, gonadal), skin changes (hyperpigmentation, glomeruloid hemangiomata, white nails), papilledema and thrombocytosis. Only if one or more of each major and minor criteria is presented as an addition to the major mandatory criteria can a diagnosis be established. Our patient fulfilled 2 major criteria and 6 minor criteria. However, as to major mandatory criteria, he showed negative results of serum protein electrophoresis and immunofixation electrophoresis, namely there was no present evidence of monoclonal gammopathy. Moreover, although the patient experienced numbness of extremities that may indicate the existence of peripheral neuropathy, his condition deteriorated so fast that it was impossible for him to have the electromyography examined. When we synthesized all the symptoms and test results, a diagnosis of POEMS syndrome was highly suspicious. But for patients without any evidence of the major mandatory criteria, is it possible to establish the final diagnosis?
The concept of Castleman disease variant of POEMS syndrome, which was described by Dispenzieri et al. [5] in 2014, was a key to the final diagnosis of our patient. Castleman disease is a rare lymphoproliferative disorder, the diagnosis of which is mostly dependent on pathological findings. In a retrospective study of 99 patients with POEMS syndrome [6], 25 of 43 biopsied lymph nodes were pathologically diagnosed with Castleman disease, 84% of which was hyaline vascular type. It was then demonstrated that only those with peripheral neuropathy and monoclonal gammopathy could be termed as standard POEMS syndrome. Those patients without both of the above major mandatory criteria but with pathologically diagnosed Castleman disease could be classified as Castleman disease variant of POEMS syndrome if they have other POEMS features [5]. In the case of our patient, the pathological finding, on which the final diagnosis depended, was of vital importance. The biopsy of Axillary lymph node of our patients revealed lymphoid hyperplasia and plasma cell infiltration. The mantle zone was broad and composed of concentric rings of small lymphocytes (so-called ‘onion skin’), which was commonly seen in Hyaline-vascular variant of Castleman disease. Moreover, the interfollicular vascularization was another typical manifestation of Castleman disease (Figure 3A). Thus, our patient was pathologically diagnosed with Castleman disease and met the diagnostic criteria of Castleman disease variant of POEMS syndrome.
Besides symptoms commonly seen in POEMS syndrome, our patient also had multiple cerebral infarctions. Considering that this patient was a 24-year-old man without any commonly seen stroke risk factors such as hypertension, hyperlipidemia or smoking, the infarction was most likely the result of POEMS syndrome. In fact, since systemic vasculature is affected in this syndrome, occurrence of ischemic organ injury should not be surprising. But the majority of the case reports describe thrombotic events in the coronary and lower limb arteries, and cerebrovascular involvement is less frequently seen [4]. Previously published case reports of cerebrovascular event in patients with POEMS syndrome are summarized in Table 1. In a retrospective study in Mayo Clinic [7], 19 out of 208 POEMS patients developed cerebral infarction, none of which occurred after successful treatment of this syndrome. Moreover, researchers also found out that thrombocytosis and evidence of plasma cell proliferation on bone marrow biopsy rather than traditional stroke risk factor were associated with an increased risk of stroke. In another retrospective study [6], 4 patients diagnosed with POEMS syndrome suffered from cerebral infarction, and none of these patients received any therapy for this syndrome. In this context, we can come to the conclusion that an early diagnosis and timely therapy of POEMS syndrome is crucial to a better prognosis.
Table 1.
Summary of previously published case reports of cerebrovascular event in patients with POEMS syndrome
| Sex | Age | Cerebrovascular event | Extra-cerebrovascular event | Reference |
|---|---|---|---|---|
| M | 49 | Left frontal parietal and occipital area infarction | None | [9] |
| M | 46 | Right parietal occipital area infarction | None | [9] |
| F | 54 | Recurrent stroke | None | [10] |
| M | 61 | Recurrent stroke | None | [11] |
| M | 41 | Right frontal parietal infarction | Occlusion of superior mesenteric and left renal arteries | [12] |
| F | 53 | Amaurosis | Stenosis of left subclavian and superior mesenteric arteries | [13] |
| F | 63 | Amaurosis | Pulmonary embolism | [14] |
| F | 42 | Large right MCA stroke | None | [15] |
| M | 42 | Left ACA/MCA and MCA/PCA watershed area infarction | None | [16] |
| F | 48 | Bilateral PCA territory infarction | Gangrene of left foot | [16] |
| F | 52 | Left MCA/PCA watershed area infarction | None | [16] |
| M | 49 | Left subcortical infarct; bilateral stenosis of first segment of MCA | None | [4] |
| F | 50 | Bilateral BG infarction; bilateral stenosis of first segment of MCA | None | [4] |
| M | 59 | Recurrent stroke | Myocardial infarction, foot gangrene | [17] |
| F | 32 | Recurrent stroke | None | [18] |
Supportive care is of great benefits for POEMS syndrome, which includes administration of diuretics for extravascular volume overload and hormone replacement therapy with thyroxine or prednisone. However, treatment of diffuse plasma cell infiltrates is irreplaceable. Autologous peripheral blood stem cell transplantation (PBSCT) is the first-line treatment for patients younger than 65 years old with normal organ function, while melphalan/dexamethasone (MDex) or lenalidomide/dexamethasone (LDex) therapy is a better option for older patients with severe organ dysfunction [3,8]. Our patient was in such a severe condition that autologous PBSCT was not feasible. Thus, LDex therapy was chosen. Unfortunately, our patient quit further treatment due to economic reasons, and rendered it impossible to obtain follow-up data.
Conclusion
POEMS syndrome co-existed with Castleman disease is rarely seen. In this report, we describe a patient diagnosed with this syndrome, who also developed multiple cerebral infarctions. The final diagnosis was made with the help of pathological findings of Castleman disease. Unfortunately, the intrinsic links between POEMS syndrome and cerebral infarction is currently unknown. We believe that it is an intriguing area for further investigation.
Disclosure of conflict of interest
None.
References
- 1.Scarlato M, Previtali SC, Carpo M, Pareyson D, Briani C, Del Bo R, Nobile-Orazio E, Quattrini A, Comi GP. Polyneuropathy in POEMS syndrome: role of angiogenic factors in the pathogenesis. Brain. 2005;128:1911–1920. doi: 10.1093/brain/awh519. [DOI] [PubMed] [Google Scholar]
- 2.Sekiguchi Y, Misawa S, Shibuya K, Nasu S, Mitsuma S, Iwai Y, Beppu M, Sawai S, Ito S, Hirano S, Nakaseko C, Kuwabara S. Ambiguous effects of anti-VEGF monoclonal antibody (bevacizumab) for POEMS syndrome. J Neurol Neurosurg Psychiatry. 2013;84:1346–1348. doi: 10.1136/jnnp-2012-304874. [DOI] [PubMed] [Google Scholar]
- 3.Li J, Zhou DB. New advances in the diagnosis and treatment of POEMS syndrome. Br J Haematol. 2013;161:303–315. doi: 10.1111/bjh.12236. [DOI] [PubMed] [Google Scholar]
- 4.Garcia T, Dafer R, Hocker S, Schneck M, Barton K, Biller J. Recurrent strokes in two patients with POEMS syndrome and Castleman’s disease. J Stroke Cerebrovasc Dis. 2007;16:278–284. doi: 10.1016/j.jstrokecerebrovasdis.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 5.Dispenzieri A. POEMS syndrome: 2014 update on diagnosis, risk-stratification, and management. Am J Hematol. 2014;89:214–223. doi: 10.1002/ajh.23644. [DOI] [PubMed] [Google Scholar]
- 6.Li J, Zhou DB, Huang Z, Jiao L, Duan MH, Zhang W, Zhao YQ, Shen T. Clinical characteristics and long-term outcome of patients with POEMS syndrome in China. Ann Hematol. 2011;90:819–826. doi: 10.1007/s00277-010-1149-0. [DOI] [PubMed] [Google Scholar]
- 7.Dupont S, Dispenzieri A, Mauermann M. Cerebral infarction in POEMS syndrome: incidence, risk factors, and imaging characteristics. Neurology. 2009;73:1308–1312. doi: 10.1212/WNL.0b013e3181bd136b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Royer B, Merlusca L, Abraham J, Musset L, Haroche J, Choquet S, Leleu X, Sebban C, Decaux O, Galicier L, Roussel M, Recher C, Banos A, Guichard I, Brisseau JM, Godmer P, Hermine O, Deplanque G, Facon T, Asli B, Leblond V, Fermand JP, Marolleau JP, Jaccard A. Efficacy of lenalidomide in POEMS syndrome: a retrospective study of 20 patients. Am J Hematol. 2013;88:207–212. doi: 10.1002/ajh.23374. [DOI] [PubMed] [Google Scholar]
- 9.Dacci P, Lessi F, Dalla Bella E, Morbin M, Briani C, Lauria G. Ischemic stroke as clinical onset of POEMS syndrome. J Neurol. 2013;260:3178–3181. doi: 10.1007/s00415-013-7180-z. [DOI] [PubMed] [Google Scholar]
- 10.Sommer B, Schaumberg J. Therapeutic challenges in a patient with POEMS syndrome and recurrent stroke: presentation of a case and review of the literature. Acta Neurol Belg. 2012;112:9–13. doi: 10.1007/s13760-012-0012-6. [DOI] [PubMed] [Google Scholar]
- 11.Wu SF, Zhou GQ, Zhu ZF. A case of POEMS syndrome patient with main clinical manifestation of multiple acute cerebral infarction. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2013;25:753. [PubMed] [Google Scholar]
- 12.Lee MR, Choi HJ, Lee EB, Baek HJ. POEMS syndrome complicated by extensive arterial thromboses. Clin Rheumatol. 2007;26:1989–1992. doi: 10.1007/s10067-007-0607-0. [DOI] [PubMed] [Google Scholar]
- 13.Lesprit P, Authier FJ, Gherardi R. Acute arterial obliteration: a new feature of the POEMS syndrome? Medicine. 1996;75:226–232. doi: 10.1097/00005792-199607000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Erro ME, Lacruz F, Aymerich N. Acute carotid obliteration: a new vascular manifestation in POEMS syndrome. Eur J Neurol. 2003;10:383–384. doi: 10.1046/j.1468-1331.2003.00600.x. [DOI] [PubMed] [Google Scholar]
- 15.Huang J, Wang L, Zhou W. Hyalinc vascular Castleman disease associated with POEMS syndrome and cerebral infarction. Ann Hematol. 2007;86:59–61. doi: 10.1007/s00277-006-0188-z. [DOI] [PubMed] [Google Scholar]
- 16.Kang K, Chu K, Kim DE, Jeong SW, Lee JW, Roh JK. POEMS syndrome associated with ischemic stroke. Arch Neurol. 2003;60:745–749. doi: 10.1001/archneur.60.5.745. [DOI] [PubMed] [Google Scholar]
- 17.Forster A, Muri R. [Recurrent cerebrovascular insult--manifestation of POEMS syndrome?] . Schweiz Med Wochenschr. 1998;128:1059–1064. [PubMed] [Google Scholar]
- 18.Rossler M, Kiessling B, Klotz JM, Langohr HD. Recurrent cerebral ischemias due to cerebral vasculitis within the framework of incomplete POEMS syndrome with Castleman disease. Nervenarzt. 2004;75:790–794. doi: 10.1007/s00115-004-1683-x. [DOI] [PubMed] [Google Scholar]


