Abstract
The major component of car washer fluid is a methanol. Intracranial hemorrhage is a rare but lethal complication in methanol poisoning. We report a case of massive bilateral basal ganglia hematoma in a 32-year-old man with methanol poisoning. He drank car washer solution twice time (about 500 ml), and was admitted to a territorial hospital 10 hours post-ingestion for depressed mental status, lower blood pressure, and high anion gap metabolic acidosis. Computed tomographic (CT) scan showed lesions in both putamen and cerebral deep white matter. Twenty-one days after methanol exposure, he suddenly developed cardiorespiratory arrest. In autopsy, external examination revealed moderate cerebral edema, but no evidence of herniation. Coronal sections of the brain showed softening and about 34 g hematoma in the bilateral putamen and 3rd ventricles. The toxic effect of methanol on the visual system has been noted in the absence of neurologic manifestations; however, there have also been a report of concomitant brain in Korea.
Keywords: Methanol poisoning, intoxication, car washer fluid, autopsy, intracranial hemorrhage
Introduction
Methanol poisoning is rare, can occur when someone drinks alcohol (ethanol) to the mistaken. It is oxidized to formaldehyde in the liver and eventually becomes formic acid. Formic acid is six times more toxic than methanol and causes weakness, nausea, vomiting, headache, abdominal pain, dyspnea and cyanosis. Symptoms usually begin within 30 minutes, sometimes may appear after a day. In severe cases of poisoning, coma, convulsion, hypothermia occurs due to metabolic acidosis and definitely blindness before death. Despite survivors can be blinded because formic acid is characteristically toxic to retinal cells [1]. For the present case, after drinking a car washer fluid twice (about 500 ml), 32-year-old man became worse after about 10 hours and received first aid in a coma. At the time of admission he was accompanied by severe metabolic acidosis with high anion gap. Computed tomographic (CT) scan of brain showed hemorrhagic lesions in both putamen and brain edema. About twenty days after treatment in intensive care unit he died. In case of death associated with various poisoning including methanol, serum drug level is important associated with a lethal dose and the cause of death can be determined based on this in many cases. However, as this case, if additional cause of death is found by the autopsy, it is necessary to clarify the causal relationship considering the relevance of the drug and eliminate the additional controversy. So we report a case of methanol poisoning and review autopsy findings and information on the situation before and after the death. Furthermore we will consider appropriate response to the event of a similar emergency or autopsy.
Case report
Outline of the events
A 32-year-old man was seen to keep retching about 11 pm. In the words of witness, he drank car washer solution by mistake confusing alcohol. Soon after he complained of severe pain in the head and abdomen and was transported to the hospital. According to the medical records at the time of admission in local hospital, he drank washer solution twice time (about 500 ml). He was drowsy mental state with low blood pressure (90/60). Arterial blood gas analysis result was metabolic acidosis state (pH 6.99, pCO2 25, pO2 148, HCO3 6.2 mEq) and blood tests revealed high anion gap; 49. After intubation he was transported to a tertiary hospital, treatment with continuous renal replacement therapy (CRRT) and intravenous fomepizole was began. But there was no response to the neurological examination with unconscious state. CT scan of brain revealed acute intracerebral hemorrhage in both putamen and moderate edema (Figure 1). Acute hemorrhage was also suspected in falx and tentorial area. He received treatment in the intensive care unit, but he died after about twenty days.
Figure 1.

Computed tomographic (CT) scan showed lesions in both putamen and edema.
Autopsy findings
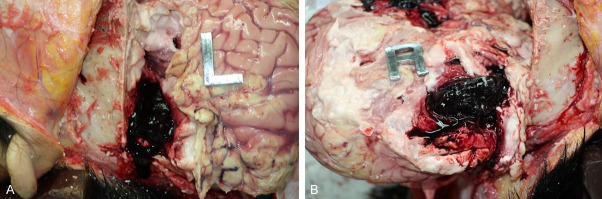
The person who died was 175 cm tall and weighed 55.7 kg. Lividity was formed as a moderate on the back of the body with dark red. There was no particular finding in the face and neck. Epidermal deprivation and contusion were observed in the range of 4.0×1.5 cm in the left elbow and epidermal deprivation in the range of 4.0×3.5 cm in the right elbow. Blisters with each size of 4.0×2.0 cm, 2.0×1.0 cm were observed in the outer and inner right wrist. In the right calf, 7.0×4.0 cm sized scar was found. There was no special finding in both feet other than needle marks. There was no special finding on the scalp, skull and meninges. But in the brain, high degree of softening with edema, about 34 g hematoma in the bilateral putamen and 3rd ventricles were observed (Figure 2A, 2B). There was no fracture in the base of skull. We observed the pus in the airway and right subclavian subcutaneous bleeding caused by a subcutaneous injection. We did not see any other special findings in the chest and abdomen. The weight of the heart was about 388 g and heart blood was a mix of dark red blood. Coronary atherosclerosis blocking 20-30% of the left coronary artery lumen was examined. A few petechial hemorrhages in outer membrane, pus in the main bronchus in the lung and fatty liver findings were observed. The results of blood and stomach contents showed that poison, methanol, surfactant contained in the washer were not detected.
Figure 2.
In autopsy, brain showed softening and about 34 g hematoma in the bilateral putamen and 3rd ventricle (A, B).
According to the autopsy findings and analysis about poison, methanol and surfactant, we made the following conclusions. Even though the person who died had no specific findings on the scalp and skull, hematoma in the right and left ventricles, intracerebral hemorrhage in both putamen, extensive brain edema and softening were observed. These findings reminded of non-traumatic intracerebral hemorrhage. Focal inflammation and pus in the lung were thought to be difficult to cause of death. There was no past history of stroke or vascular disorder in the dead and he had no presymptoms of cerebral hemorrhage. During routine day he drank car washer solution and was taken to the tertiary hospital in a coma due to brain hemorrhage and edema. Judging from these facts, the point of cerebral hemorrhage was shortly after drinking washer fluid.
Discussion
The main component of washer fluid is water and methanol. There are reports that can be lead to death in case of massive aspiration of methanol due to both putamen hemorrhage [2]. Acute putaminal hemorrhage is relatively rare complication and can be seen in methanol, carbon monoxide, ethylene glycol poisoning [3]. However, acute putaminal hemorrhage accompanied by visual loss and optic atrophy is known for its unique complications that appear only on methanol poisoning [4]. It is still unclear why hemorrhagic lesions especially well involve putamen in methanol poisoning. Maybe accumulation of formic acid in the putamen is one of the causes [5]. Visual disturbance that appear with bleeding is known to be based on the formic acid [1]. Another symptom from methanol intoxication is metabolic acidosis with high anion gap and osmolal gap which can be also seen in diabetic ketoacidosis, alcoholic ketoacidosis, chronic renal failure, multiple organ failure [6]. Symptoms of intoxication may attack at any time within 40 minutes to 72 hours and the incubation period is usually 12-24 hours [6].
For the present case, he drank car washer solution by mistake confusing alcohol and after visiting the local hospital, fell into a coma, was transported to a tertiary hospital to receive emergency treatment and it took about 10 hours. When he arrived at the tertiary hospital he was in comatous mental state, so CT scan was performed and it showed bilateral putaminal hemorrhage. In this process, test on blood methanol concentration was not carried out. And component of the washer solution, methanol or surfactant was not detected due to the first-aid treatment and long hospital stay. But considering he had no hypertension or vascular disorder in the past and no presymptoms like headache or nausea before methanol drinking, synthetically it seems to be no doubt that he died from cerebral hemorrhage due to methanol poisoning.
According to the literature, even low concentrations of serum methanol (<20 mg/dL), possibility of severe poisoning can’t be ruled out. Minimum capacity to cause blindness and death is 8 g (10 mL, 100 %) and 10 g (30 mL, 40%) respectively [6]. Mostly in case of ingestion a capacity of 40 g or 1 g/kg, if the treatment is not performed, it causes fatal poisoning. If the treatment is made in a short time patients can survive without sequelae [6].
In most cases of poisoning, the situation or blood test is often helpful and treatment is about complications of high frequency. Even in this case, the purpose of the aid was a relatively common complication of methanol poisoning, metabolic acidosis. Motivation in brain CT was mental change. However, even if rare, early reminding of the fact that brain hemorrhage can occur during severe methanol poisoning is helpful to cope with emergency. Likewise, when a patient suspected methanol poisoning that just arrived at the emergency room, we should not simply write a death certificate with methanol poisoning even higher methanol concentration in the blood and keep in mind the possibility of other complications. Since most organs including brain are examined in autopsy, it is not difficult to know the presence or absence of cerebral hemorrhage. Nevertheless, starting to work considering the possibility of various complications can lead to the exact cause of death. Surely it is critical role of autopsy to determine whether definitive cause of death is associated with chronic disease of the dead or result of poisoning.
Acknowledgements
This study was supported by a grant from the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (Kim HS, NRF-2013R1A1A2007621).
Disclosure of conflict of interest
None.
References
- 1.Kang DY, Kang HW, Kwak JS. A textbook of Legal Medicine. Korea: Jeong Mun Kag; 2012. p. 200. [Google Scholar]
- 2.Permpalung N, Cheungpasitporn W, Chongnarungsin D, Hodgdon TM. Bilateral putaminal hemorrhages: serious complication of methanol intoxication. N Am J Med Sci. 2013;5:623–624. doi: 10.4103/1947-2714.120804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharma P, Eesa M, Scott JN. Toxic and acquired metabolic encephalopathies: MRI appearance. AJR Am J Roentgenol. 2009;193:879–886. doi: 10.2214/AJR.08.2257. [DOI] [PubMed] [Google Scholar]
- 4.Singh P, Paliwal VK, Neyaz Z, Kanaujia V. Methanol toxicity presenting as haemorrhagic putaminal necrosis and optic atrophy. Pract Neurol. 2013;13:204–205. doi: 10.1136/practneurol-2012-000500. [DOI] [PubMed] [Google Scholar]
- 5.Beltz EE, Mullins ME. Hyperintensity of the basal ganglia and cortex on FLAIR and diffusion-weighted imaging: self-assessment module. AJR Am J Roentgenol. 2010;195(Suppl):S9–11. doi: 10.2214/AJR.10.7261. [DOI] [PubMed] [Google Scholar]
- 6.Kim GW, Youn SG, Jeong YS, Choi SC. Clinical Toxicology. Korea: Koonja; 2006. pp. 600–7. [Google Scholar]