Abstract:
The purpose of this study was to describe the design and utilization of a multi-modality life support system (MMLSS), which is used to provide extracorporeal support for cases such as left heart bypass (LHB), extracorporeal life support (ECLS), veno-venous bypass, and hypothermic resuscitation. The design of the MMLSS consisted of a mobile cart outfitted with a centrifugal pump, heater cooler, an in-line blood gas monitor, oxygen blender/flow meter, and assorted safety devices (pressure sensors and level and bubble detectors). A single disposable circuit was used for all procedures and designed to be easily modifiable to support a variety of clinical scenarios, with and without the use of an oxygenator. The system was designed for rapid deployment throughout the hospital. From January 1, 2006 to December 31, 2007, the MMLSS has been used in three LHB procedures (63 ± 72 minutes), four adult ECLS cases (57.2 ± 56.9 hours), four veno-venous bypasses (72 ± 35 minutes), and one hypothermic resuscitation (182 minutes). The MMLSS was designed to be used in patients >20 kg and could achieve flows in the range of 1-5.5 L. There were no complications associated with the device. The MMLSS is a versatile system that can be used throughout the hospital with a single disposable circuit, accommodating a diverse caseload in a safe and reproducible manner.
Keywords: extracorporeal support, portable, cardiopulmonary bypass
The utility for cardiopulmonary bypass (CPB) outside of the operating room setting is complicated by several factors related to the heart lung machine including size limitations, lack of safety devices, and the inability for a single perfusionist to provide critical support with a cardiopulmonary support system. To provide patient safety with a portable device, it should include safety features such as “arterial line filters, blood level sensors, and air bubble detectors.” (1) The size of a standard heart lung machine, with its large footprint, is an issue, as well as the need for a separate heater cooler. When designing a portable CPB machine, all of these issues should be addressed, and there entails the increased cost and complexity.
At Geisinger Medical Center (GMC), we designed the multi-modality life support system (MMLSS) to incorporate small size, safety, portability, and cost effectiveness in one device. A single disposable tubing pack is used for many types of procedures throughout various locations in the hospital including the emergency room (ER), cardiac intensive care unit (CICU), adult intensive care unit (AICU), and the operating room (OR). The size also allows a single perfusionist to mobilize the MMLSS and bring it in to the patient’s bedside or other remote places outside of the OR when it is not possible to move the patient. For example, the MMLSS has been used for extracorporeal support in cases such as left heart bypass (LHB), extracorporeal life support (ECLS), veno-venous bypass, and hypothermic resuscitation. It also can be used in other cases in which cardiopulmonary support is needed. Being able to use the MMLSS during many types of CPB support cases also makes it more cost effective. Incorporating all these aspects in the MMLSS has made it another device with the utility to provide life-saving support outside the OR in a safe and reproducible manner.
MATERIALS AND METHODS
The design of the MMLSS was built on a modified mobile cart. The cart was outfitted with a centrifugal pump (Stockert SCPC; Sorin Biomedical, Arvada, CO), heater cooler (BioCAL 340; Medtronic Cardiopulmonary, Minneapolis, MN), and Stockert level and bubble detector (Sorin Biomedical). Included are also assorted safety devices such as a Stockert Electrical remote-controlled tubing clamp (ERC; Sorin Biomedical) to reduce the potential for retrograde flow and air embolism. An in-line blood gas monitor (Terumo CDI 500; Terumo, Ann Arbor, MI) is incorporated for arterial and venous blood gas monitoring. The cart also has a CO2 tank, O2 tanks, storage area, extra long gas lines, and a vacuum regulator. The disposables for the device consist of a custom tubing pack that can be used for several clinical applications. The device was designed to accommodate various oxygenators such as the COBE Synthesis, COBE primox, COBE EOS (Sorin Biomedical), Medtronic ECMO oxygenator (Medtronic Cardiopulmonary, Minneapolis, MN), and Jostra D oxygenator (Maquet Cardiopulmonary, Hirrlingen, Germany). Procedures not requiring pulmonary support are performed without an oxygenator, but may require a heat exchanger (see Figures 1 and 2) (Medtronic biotherm heater; Medtronic Cardiopulmonary). The MMLSS was designed to be used in patients >20 kg and could achieve flows in the range of 1–.5 L.
Figure 1.

MMLSS during thoracoabdominal aneurism surgery providing left heart bypass support.
Figure 2.
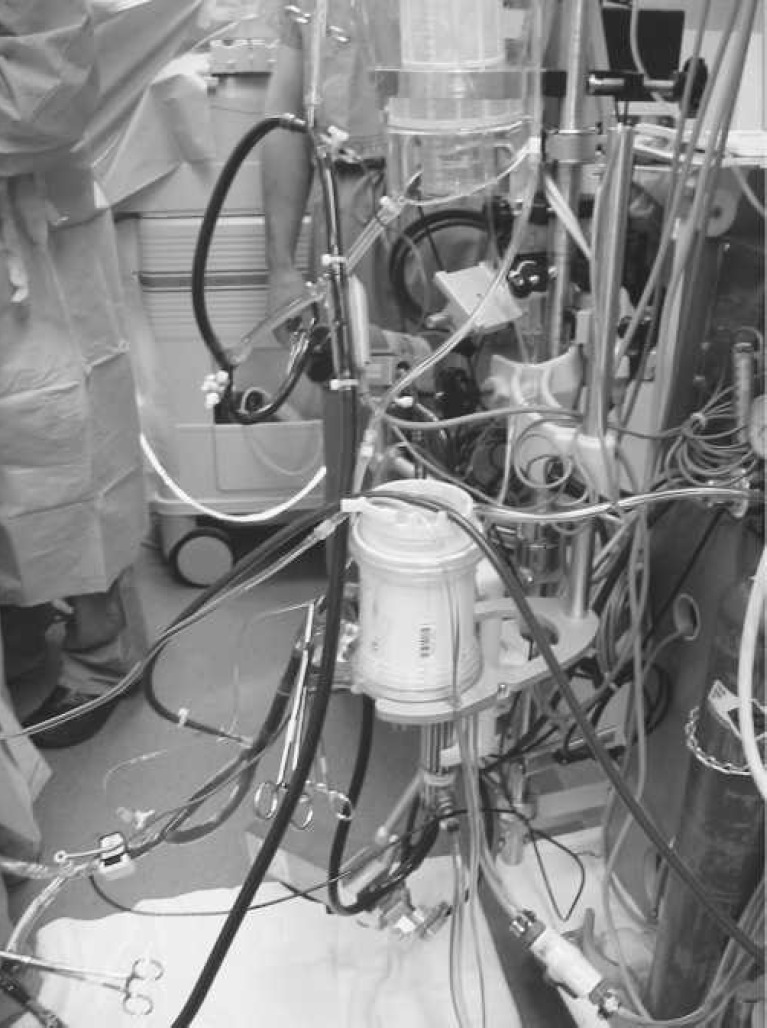
MMLSS during thoracoabdominal aneurism surgery providing left heart bypass support.
RESULTS
From January 1, 2006 to December 31, 2007, the MMLSS has been used in three LHB procedures (63 ± 72 minutes) that were all done in the operating room. There were four adult ECMO cases (57.2 ± 56.9 hours) all done in the adult intensive care and cardiac intensive care units at the patient’s bedside. Four veno-venous bypasses (72 ± 35 minutes) for orthotopic liver transplant patients were all done in the operating room. One hypothermic resuscitation (182 minutes) was performed in the emergency room. There were no complications associated with the device.
DISCUSSION
The use of these devices for patients with acute respiratory distress syndrome (ARDS) as rescue therapy shows that with early institution, it is lifesaving and beneficial for patients that have reversible respiratory failure that are non-responders to conventional mechanical intervention (2). Another use for mobile CPB devices is resuscitation from accidental hypothermia. Coronary artery bypass (CAB) is recommended for patients who have a core temperature of <25°C (3). The use of these devices in venovenous bypass for liver transplant patients helps prevent systemic hypotension in these surgeries (4). The repair of thoracoabdominal aortic aneurysms is another surgical procedure that warrants the use of these devices, especially in the treatment of type I and type II aneurysms to help prevent spinal cord ischemia (5). This circuit also allows for quick alterations to accommodate the need for oxygenation or conversion to full bypass support by the simple manipulation of clamps as does the BICIRUIT system by Bisleri et al. (6) When converting from LHB to full bypass with circulatory arrest, the need may arise for cerebral perfusion, which our system accommodates as would a full-size system (7).
Studies are being done at the University of Pennsylvania Center for Resuscitation Science on how CPB can be used to treat patients that have had a massive myocardial infarction with circulatory collapse. The researchers realized that the standard emergency room procedure for treating these patients may be inappropriate. Standard protocol is to flood these patients with oxygen and resuscitate them, but instead “we should aim to reduce oxygen uptake, slow metabolism, and adjust the blood chemistry for gradual and safe reperfusion” (8). Their work coincides with what Athanasuleas et al. (9) are doing at the Norwood Clinic and Kemp-Carraway Heart Institute in Birmingham, Alabama. Their study showed that CPB support and controlled cardioplegic administration to induce a state of suspended animation of the heart with correction of the underlying cardiac pathology and controlled reperfusion offers hope for cardiac arrest patients.
CONCLUSION
In conclusion, having a device like the MMLSS in our hospital has been an important tool in saving the lives of patients that would not have had other options. Because of its design, it meets all of the needs of having a small footprint, necessary safety devices, maneuverability, and cost effectiveness.
REFERENCES
- 1.Palanzo DA.. Perfusion safety: Defining the problem. Perfusion. 2005;20:195–203. [DOI] [PubMed] [Google Scholar]
- 2.Madershahian N, Wittwer T, Strauch J, et al. Application of ECMO in multitrauma patients with ARDS as rescue therapy. J Card Surg. 2007;22:180–4. [DOI] [PubMed] [Google Scholar]
- 3.Vretenar DF, Urschel JD, Parrott JCW, Unruh HW.. Cardiopulmonary bypass resuscitation for accidental hypothermia. Ann Thorac Surg. 1994;58:895–8. [DOI] [PubMed] [Google Scholar]
- 4.Kaufman RD, Khoury GF.. Hemodynamic changes with initiation of veno-venous bypass in orthotopic liver transplant patients. Am J Anesthesiol. 1995;22:184–8. [PubMed] [Google Scholar]
- 5.Coselli JS.. The use of left heart bypass in the repair of thoracoabdominal aortic aneurysms: Current techniques and results. Semin Thorac Cardiovasc Surg. 2003;15:326–32. [DOI] [PubMed] [Google Scholar]
- 6.Bisleri G, Giancarlo T, Alberto N, et al. The Bicircuit system: Innovative perfusional options for surgical treatment of the thoracic aorta. Ann Thorac Surg. 2005;79:678–81. [DOI] [PubMed] [Google Scholar]
- 7.Guan Y, Yang J, Wan C, et al. Cardiopulmonary bypass for thoracic aortic aneurysm: A report on 488 cases. J Extra Corpor Technol. 2004;36:22–7. [PubMed] [Google Scholar]
- 8.Adler J.. To treat the dead, the new science of resuscitation is changing the way doctors think about heart attacks-and death itself. Newsweek. May 7, 2007. [Google Scholar]
- 9.Athanasuleas CL, Buckberg GD, Allen BS, Beyersdorf F, Kirch MM.. Sudden cardiac death: Directing the scope of resuscitation towards the heart and brain. Resuscitation. 2006;70:44–51. [DOI] [PubMed] [Google Scholar]


