Abstract:
Strategies to reduce blood loss and transfusion of allogeneic blood products during surgical procedures are important in modern times. The most important and well-known autologous techniques are preoperative autologous predonation, hemodilution, perioperative red cell salvage, postoperative wound blood autotransfusion, and pharmacologic modulation of the hemostatic process. At present, new developments in the preparation of preoperative autologous blood component therapy by whole blood platelet-rich plasma (PRP) and platelet-poor plasma (PPP) sequestration have evolved. This technique has been proven to reduce the number of allogeneic blood transfusions during open heart surgery and orthopedic operations. Moreover, platelet gel and fibrin sealant derived from PRP and PPP mixed with thrombin, respectively, can be exogenously applied to tissues to promote wound healing, bone growth, and tissue sealing. However, to our disappointment, not many well-designed scientific studies are available, and many anecdotic stories exist, whereas questions remain to be answered. We therefore decided to study perioperative blood management in more detail with emphasis on the application and production of autologous platelet gel and the use of fibrin sealant. This review addresses a large variety of aspects relevant to platelets, platelet-rich plasma, and the application of platelet gel. In addition, an overview of recent animal and human studies is presented.
Keywords: platelets, platelet-rich plasma, platelet gel, platelet growth factors, thrombin
Few hospitals in Europe routinely use autologous platelet gel application techniques as part of a perioperative blood management program. In the United States, an increasing number of clinicians tend to use platelet gel applications in a variety of surgical settings, for both in and out of hospital surgery. The question of why this novel and promising technique for the delivery of autologous growth factors has not yet been adopted on a broader scale needs to be addressed. The main reason may be the lack of convincing scientific data that provide information of whether or not the use of platelet-rich plasma (PRP) and platelet gels (PG) are appropriate in the clinical setting.
At Catharina Hospital (Eindhoven, Netherlands), we started to use PG techniques in 2001 with a small group of patients undergoing complicated cardiac surgical procedures and in patients undergoing spinal fusion surgery. This was carried out as an adjunct to the already existing perioperative blood management programs with apparently impressive clinical results.
The Department of Perioperative Blood Management of the Catharina Hospital performs close to 1600 blood management procedures annually, of which 60% are related to obtaining whole blood platelet to produce PRP for the use of PG procedures. While its extended use is based on positive clinical impressions and on clinical judgment, it still lacks a firm scientific basis. Therefore, clinical trials are required to answer questions on the efficacy, efficiency, and safety of the application of PRP and PG under various surgical and medical conditions.
It is clear that a good understanding of the proper preparation and use of this specific blood management technique is mandatory for clinicians to adequately evaluate results of its use and to avoid inconsistent results. Conflicting data have been reported in clinical and experimental research on the efficacy of PG treatment (1–5). To understand how this arises, it is essential to be in possession of the details of the preparation of PRP and PG. Knowledge of the following factors are of particular importance: the method of drawing blood, the quality of the PRP used, the platelet and growth factor counts, the PRP activation, whether autologous or donor PRP was used, and the overall methodology. With respect to these issues, the clinician should be aware that data may sometimes seem to be conflicting in the eventual outcome.
This review addresses a variety of aspects pertaining to the use of PG, including background on platelet activity, the pivotal role of platelets in hemostasis, soft tissue healing, and bone growth, whole blood PRP production procedure, platelet activation with thrombin, and a description of the various actions of platelet-derived growth factors (PDGFs). In addition, a discussion of the most recent clinical and experimental articles is presented with respect to these issues. Some safety issues including possible PG mitogenic effects are also addressed.
PLATELET ANATOMY AND FUNCTION
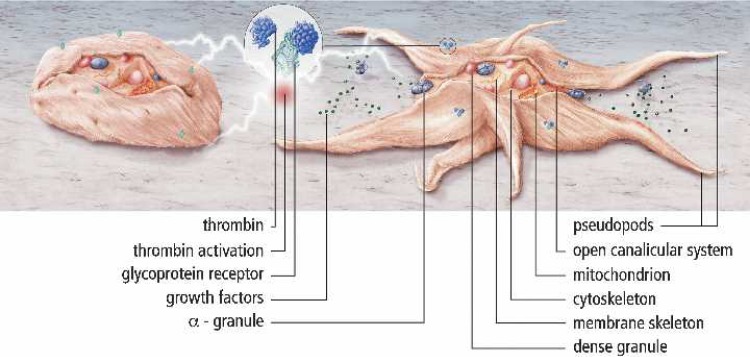
Platelets are small discoid blood cells (∼1–3 μm). The average platelet count ranges from 1.5 to 3.0 × 10−5/mL of circulating blood, and the in vivo half-life time of platelets is about 7 days. Platelets are formed from megakaryocytes and are synthesized in bone marrow by pinching off pieces of cytoplasm. Thereafter, platelets are extruded into the circulation. Platelets have a ring of contractile microtubules (cytoskeleton) around their periphery, containing actin and myosin. Inside the platelet, a number of intracellular structures are present containing glycogen, lysosomes, and two types of granules. These are known as dense granules, which contain ADP, ATP, serotonin, and calcium, and a-granules, which contain clotting factors, growth factors, and other proteins. They are equipped with an extensively invaginated membrane with an intricate canalicular system, which is in contact with the extra-cellular fluid (6). Normally, in the resting state, platelets are nonthrombogenic and require a trigger before they become a potent and an active player in hemostasis and wound healing. On activation (e.g., by thrombin), they change shape and develop pseudopodia, which promotes platelet aggregation and subsequent release of the granule content through the open canalicular system (Figure 1).
Figure 1.
Schematic overview of a resting and activated platelet. Normally platelets are in a resting, nonactivated state. On activation (e.g., by thrombin), platelets change their shape with the development of pseudopods to promote platelet aggregation and subsequent release of granule content through the open canalicular system (GP, glycoprotein).
PLATELET ACTIONS
Platelets and PG in Hemostasis
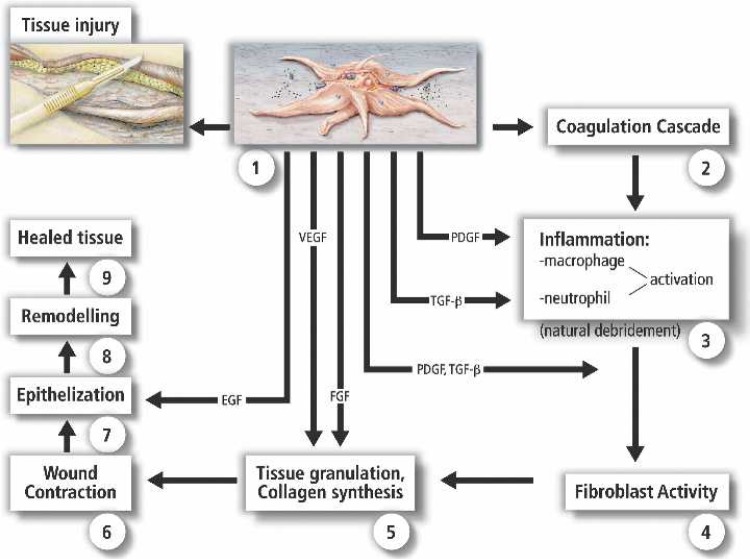
Hemostasis is a balanced interaction of platelets, vasculature, plasma clotting proteins, and low molecular weight substances. After an injury (e.g., by surgical trauma), the most important initial reactions leading to immediate blood coagulation are mainly mediated by platelets and blood vessel wall changes. In surgery, damaged blood vessel walls expose subendothelial collagen, binding von Willebrand factor in the plasma, and subsequently changing the structure so that the platelets can adhere to the blood vessel wall. This process, known as platelet adhesion, acts through the glycoprotein Ib, and IIb/IIIa receptors that are present in the platelet membrane. After this event, platelets become activated and aggregate. On activation, the platelet cytoskeleton changes from discoid to a spherical shape with protruding pseudopods, which then spread over injured tissues at the site of injury, a phenomena called platelet aggregation. After aggregation, the granular contents are released through the canalicular system. Secreted serotonin probably assists in tissue vasoconstriction. ADP promotes release of granule contents from other platelets and makes the platelets sticky, thus forming a hemostatic plug. Many other agents are able to cause platelet aggregation and also to activate phospholipase A2 present in the platelet membrane. Subsequently, as a result of the latter, membrane phospholipids release arachidonic acid, which is converted into thromboxane A2 and also causes platelet aggregation and platelet growth factor (PGF) release. Independent of thromboxane and ADP, another mechanism that causes platelet aggregation and platelet granule release is induced by the presence of thrombin. Thus, by these three mechanisms of platelet activation, the platelet plug is extended in an attempt to stop blood loss from damaged vessels. Furthermore, the coagulation system is activated by secreted and budded particles (7,8). The most well-understood platelet function, at the onset of primary hemostasis, is the formation of a platelet plug. Thereafter, secondary hemostasis is initiated with the activation of coagulation factors and the formation of a fibrin network that stabilizes the platelet plug (9). The final step is the activation of leukocytes invading the affected area with the release of cytokines, which activate the fibrinolytic system, leading ultimately to clot lysis (Figure 2). Because platelet a-granules secrete PDGFs at the wound site almost at the instant of injury, repair of injured vasculature and tissue is directly initiated with the formation of new connective tissue and revascularization. Furthermore, the temporary formation of platelet and fibrin plugs at the wound site prevents the entry of microorganisms.
Figure 2.
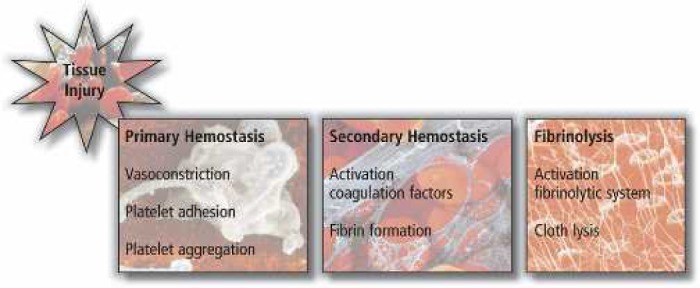
The different cascade stages in hemostasis after tissue injury.
Based on the fundamental role of platelets in hemostasis, as discussed above, it may be hypothesized that exogenously applied PG would contribute to a more effective hemostatic condition of (surgical) wound surfaces, where it attaches to tissues as a solid platelet plug. Stover et al. (10) prospectively evaluated the use of PG as a dural seal-ant in patients undergoing craniotomy or thoracolumbar procedures and noted successful closure in 39 of 40 treated patients. Another therapeutic application is to use PG as a wound sealant when it is sprayed by an aerosol technique over larger wound surfaces and suture lines in patients who are at risk of postoperative wound leakage or fistula formation. Furthermore, in patients who are at risk of impaired wound healing, such as diabetics, and thus at risk for postoperative wound complications, a sprayed PG may deliver a high concentration of PGF to the wound, thus boosting and supporting the natural healing process.
Platelets and PG in Wound Healing
Wound healing is a well-orchestrated and complex series of events involving cell–cell and cell–matrix interactions, with growth factors serving as messengers to regulate the various processes involved. The “wound healing” process as a whole has to be considered from the point of view of the type of lesion, which will in turn dictate the degree of healing that can be obtained. A partial-thickness skin abrasion heals almost entirely by epithelization, whereas deep pressure chronic ulcers rely mainly on matrix synthesis, angiogenesis, fibroplasia, and wound contraction. The significant action of PDGFs in wound healing has been widely reviewed. With wounds, and also after surgical incisions, repair begins with platelet clot formation, activation of the coagulation cascade, and platelet degranulation with release of growth factors. During the first 2 days of wound healing, an inflammatory process is initiated by migration of neutrophils and subsequently macrophages to the wound site. In turn, activated macro-phages release multiple growth factors, including transforming growth factors-α and -β (TGF-α, TGF-β), PDGF, interleukin-1 (IL-1), and fibroblast growth factor (FGF) (11). Angiogenesis and fibroplasia starts shortly after day 3, followed by the beginning of collagen synthesis on days 3–5. This process leads to an early increase in wound breaking strength, which is the most important wound healing parameter of surgical wounds, followed by epithelization and the ultimate remodeling process. During the various stages of wound healing, PGF play a key role, as shown in several studies (12,13). In Figure 3, an illustration of the role of PDGFs during the different stages in the wound healing process is represented.
Figure 3.
Schematic illustration of the role of PDGFs (numbers indicate the sequence of actions) during the different stages of the wound healing process (VEGF, vascular endothelial growth factor).
Platelet Degranulation:
After tissue damage, PDGF and FGF are already being produced by the injured cells (14). Once the platelet plug is in place, platelets will start to degranulate with the release of growth factors; PDGF and TGF-β are the most important growth factors at the wound site in the start of the wound healing process. A characteristic of PGF molecules is that they are also chemotactic and mitogenic with regard to inflammatory cells (i.e., neutrophils, monocytes, and macrophages) (15).
Inflammatory Action:
Pierce et al. (16) showed that a single application of PDGF used in incisional wounds amplifies the inflammatory response with an increased wound influx of neutrophils and macrophages.
Matrix Deposition:
During the phase of matrix synthesis and matrix deposition, PGF again plays a predominant role. Mustoe et al. (17) showed, in an experimental model, that a single dose of PDGF increased the volume of tissue granulation by 200% after 7 days. With the application of TGF-β alone on wounds, it was revealed that the matrix mainly consisted of new collagen (15). Furthermore, in steroid-treated or irradiated wounds, it was shown that the application of TGF-β reversed the healing deficit with restoration of wound breaking strength (18).
Collagen Production:
Also important in wound healing is collagen production, which is initiated by the chemotactic and mitogenic actions of fibroblasts by FGF.
Epithelization:
Topically applied epidermal growth factor (EGF) leads to accelerated epithelization, as shown in a model by Nanney (19). In the beginning of the epithelization process, PDGF receptor genes were found, indi-cating that PDGF is also important during epithelization (20). During the last phase of wound healing, both FGF and PDGF increased contraction and remodeling time (21,22).
Based on the actions of the various PGF during the different stages in the wound healing cascade, the use of PG to stimulate wound repair is an interesting proposition (Figure 3). Compared to recombinant single growth factor applications, PG has the supreme advantage that it offers multiple synergistically working growth factors promoting mitogenesis of mesenchymal stem cells at the wound site (12,23–25).
Promising indications for topical PG applications might be for treatment of chronic nonhealing wounds and supportive healing after incisional wounds that occur, for example, in diabetic patients who are at risk of impaired wound healing. PG has been used successfully in wound care patients to close chronic nonhealing (diabetic) ulcera (26,27). Margolis et al. (28) showed, in a large cohort of patients, that the application of the material released from platelets was more effective than standard care methods in wound healing. The treatment was even more effective in patients with deeper wounds (28). Another interesting finding in one study was the effect of PG had on the reduction of pain, an effect that is still not understood (29). In conclusion, there is sound evidence indicating that the use of PG in patients with chronic nonhealing wounds can be useful, and there is now a need to conduct clinical trials to study its effect on wound rehabilitation and earlier functional recovery in different surgical procedures.
Platelets and PG in Bone Healing
Bone is defined as a biological tissue composed of dynamically active cells that are integrated into a rigid framework. Bone cells consist of osteoblasts, osteoclasts, osteocytes, osteoprogenitor cells, and hematopoietic components (30). The bone healing process, whether in fracture repair or any given fusion model, is a delicate balance between bone deposition, resorption, and remodeling, and is influenced by numerous biochemical, biomechanical, cellular, and pathological mechanisms. During bone healing, mature bone forming osteoblasts secrete growth factors that are also present in platelets (31). Osteoclasts, in contrast, are bone-resorbing cells, a process controlled by hormonal and cellular mechanisms. Under normal circumstances, the activity of osteoblasts and osteoclasts is in balance.
In fracture repair and bone healing (i.e., callus formation), platelets act as an exogenous source of growth factors stimulating the activity of bone cells, based on their particular relevance to bone growth (32,33). As in wound healing, bone fracture healing also incorporates the three stages of inflammation, proliferative repair, and remodeling. At bone fracture sites, platelets release PDGF, TGF-β, and EGF, providing an ideal system for the delivery of growth factors to the injury site. The richest source of TGF-β is found in platelets, bone, and cartilage. Two isoforms, TGF-β1 and TGF-β2, are present in the platelets. TGF-β1 has the greatest potential for bone repair because both chondrocytes and osteoblasts are enriched with receptors for TGF-β1. In fact, TGF-β may contribute to bone healing at all stages (34,35). It has been shown that, with a combination of PGF, TGF-β, FGF, and EGF, an optimum is created for the stimulation of differentiation and proliferation of osteoblasts to osteogenic cells (36,37). Similarly, proliferation was increased by the mitogenic action of PDGF in mesenchymal stem cell differentiation when TGF-β and EGF was added (38).
The ability of bone to heal is based on three concepts: osteogenesis, osteoinduction, and osteoconduction.
Osteogenesis is described as the ability to produce new bone and is determined by the presence of osteoprogenitor cells and osteogenic precursor cells in the area.
PGF are present in three of four stages during this bone healing process (31).
Osteoinduction is defined as the ability to stimulate stem cells to differentiate into mature cells through the stimulation by local growth factors such as PDGF and TGF-β (39,40).
Osteoconduction is determined by the presence of a scaffold that allows for vascular and cellular migration and is usually achieved by the use of autologous harvested bone (autograft), homologous graft materials (allograft), or artificial matrixes like demineralized bone (DMB), hydroxyl apatite, tricalciumphosphate, and collagen (41). In the regulation and stimulation of these biochemical and cellular processes, PDGF plays a dominant role with regard to mitogenesis, chemotaxis, and stem cell differentiation. Recently, PRP has been successfully applied by subcutaneous administration in a diabetic femur fracture model. PRP normalized the early cellular proliferation and chondrogenesis, while improving the late mechanical strength (42).
Bone grafts are widely used to overcome bone continuity defects and to enhance a variety of fusions. For this reason, they are often used as a supportive tool in fracture repair and for the treatment of fractures. It can be hypothesized that mixing PRP and thrombin (PG), along with sequestered autologous bone graft materials, might create a bioengineered graft (Figure 4). The result is a bone graft enriched with a high concentration of platelets releasing growth factors. Because of the viscous nature of PG, the bone chips will stick together, thus avoiding migration of bone particles.
Figure 4.
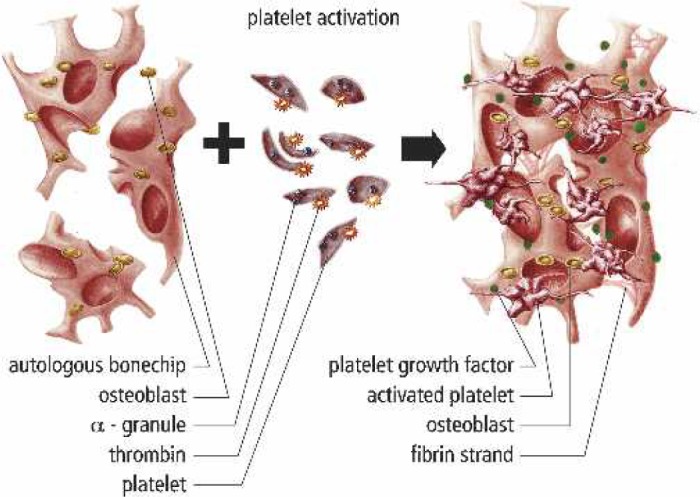
Graphical representation of a bioengineered bone graft with PG. Sequestered autologous bone chips are mixed with PRP and thrombin. The result is a bone graft that is enriched with a high concentration of platelets releasing their growth factors. Because of the viscous PG, the bone chips will stick together, thus avoiding migration of bone particles.
This may be a promising technique that could support and promote bone growth and accelerate fracture healing, particularly in patients who are at risk of the development of nonunions. The mixture of PG with bone grafts might also be an attractive alternative in the treatment of fractures, spinal fusion, and bone tissue engineering strategies.
PREPARATION OF PRP
PRP is perioperatively prepared from a unit of autologous whole blood by means of extracorporeal blood processing techniques. PRP can be prepared either through standard blood banking techniques or through point-of-care devices, including blood cell savers/separators or table top devices. The preparation of PRP by blood banks, through discontinuous plasmapheresis methods, should be limited because of higher production costs and delayed availability of PRP, compared to bedside devices. Furthermore, blood bank–prepared PRP is out of reach of the clinician and demands a highly controlled logistic system to avoid product mismatch before application to the patient.
Two different point-of-care blood centrifugation machines were introduced to the market recently that achieve optimal blood separation for the production of PRP. With cell savers/separators, larger predonation blood volumes (250 to >500 mL of whole blood) can be obtained, resulting in a PRP volume ranging from 20 to >50 mL. Tabletop centrifuges have been used to manufacture smaller volumes of PRP from lesser amounts of whole blood (50–150 mL). The choice for either system is mainly dependent on the type of surgical procedure and the anticipated need for the amount of PG. It seems reasonable that cell savers are used when both red cell salvage and PG application are both indicated. In contrast, tabletop devices are used when only small amounts of PG are required during minimal blood loss surgical procedures. In Table 1, an overview of the currently available cell saver/separator devices is shown, and in Table 2, an overview of tabletop systems is shown.
Table 1.
Overview of currently available cell-saver/separator PRP devices.
| Device Name | Manufacturer | Characteristics | Flow | Bowl Size (mL) |
|---|---|---|---|---|
| Brat 2 | Cobe, Cardiovascular Inc, Arvada, CO, USA | Baylor bowl | Discontinuous | 55, 125, 175, 225, 240 |
| Compact A | Sorin Group, Mirandola, Italy | Latham bowl | Discontinuous | 55, 125, 175, 225 |
| Electa | Sorin Group, Mirandola, Italy | Latham bowl | Discontinuous | 55, 125, 175, 225 |
| Fresenius CATS | Fresenius Kabi AG, Bad Homburg, Germany | Separation chamber | Continuous | N/A |
| Haemonetics CS 5 Plus | Haemonetics Corporation, Braintree, MS, USA | Latham bowl | Discontinuous | 70, 125, 225 |
| Sequestra 1000 | Medtronic Inc., Minneapolis, MN, USA | Latham bowl | Discontinuous | 125, 225 |
Table 2.
Overview of currently available tabletop PRP devices.
| Device Name | Manufacturer | Characteristics | Components | PRP Volume | RPM |
|---|---|---|---|---|---|
| Angel | Sorin Group, Mirandola, Italy | Variable chamber disk | RBC, PPP, PRP | 5–18 mL | Max 4000 |
| GPS II | Biomet, Warsaw, IN, USA | Container + buoy | PPP, PRP | 5–6 mL | 3200 |
| Magellan | Medtronic Inc, Minneapolis, MN, USA | Chamber | RBC, PPP, PRP | 1–8 mL | Max 4000 |
| Secquire | PPAI Medical, Fort Myers, FL, USA | Container | RBC, PPP, PRP | 7 mL | 3500 |
| Symphony II | dePuy Inc, Raynham, MS, USA | Two chambers | PPP, PRP | 7 mL | Fixed two step |
| Vivostat | Vivolution A/S, Birkeroed, Denmark | Preparation chamber | PRF, FS | 5–7 mL | N/A |
RBC, red blood cells; PPP, platelet poor plasma; PRP, platelet rich plasma; PRF, platelet rich fibrin; FS, fibrin scalant; N/A, not applicable.
PRP Preparation Methodology
In the clinical standard setting, blood is drawn from the median cubital vein. When a cell saver is used to manufacture PRP, autologous whole blood is collected into standard donor bags filled by gravity, not exceeding the maximum allowable predonation volume in relation to the citrate volume in the blood bag. When tabletop devices are used, the blood is carefully collected by aspiration techniques into syringes, avoiding “negative pulling” to fill the syringes quickly. The use of a needle diameter larger than 17 gauge avoids trauma to the platelets during the blood draw. The autologous predonated blood is collected in sufficient amounts of anticoagulation citrate dextrose-A solution (ACD-A). In general, a ratio of 1 mL of ACD-A to 7–8 mL of whole blood should be maintained. The aspirated blood is gently agitated to thoroughly mix the anticoagulant with the blood.
Currently, most cell savers use a Latham (tapered) bowl instead of a Baylor (straight) bowl, ranging in volume between 50 and 225 mL. Furthermore, continuous autotransfusion systems, not using a bowl, can also be used to prepare PRP.
These sequester the whole blood in a semiautomatic controlled operating mode by centrifugation at 5600 rpm, separating the platelet-poor plasma (PPP) from the buffy coat layer and erythrocytes. The PPP volume is separately collected in a blood bag. Thereafter, centrifugation is slowed down to 2400 rpm to obtain the buffy coat layer consisting of PRP and leukocytes, which is collected in a separate blood bag or syringe. After this procedure, the erythrocytes are also separately collected in a blood bag. The collected PPP and erythrocytes are reinfused during surgery at a time determined by the anesthesiologist. The collected PRP is used to prepare PG for application to tissues.
With tabletop devices, a similar protocol of high-and low-speed centrifugation is followed. Depending on the brand of tabletop device, one may collect all blood components separately or collect only PRP. In those cases where no retransfusion of blood components is feasible, the PPP and erythrocytes are discarded.
Regardless of the type of PRP preparation method, the aim of working with whole blood is to prepare PRP with a platelet count in excess of the baseline platelet count values at the patient’s bedside.
PRP Activation
Alpha granules of the nonactivated platelets in the PRP contain PGF and are thus nonfunctional, because they are not released or in contact with the tissue. To initiate the release of these growth factors, platelets must be activated. Thrombin, the most potent platelet activator, will induce immediate PGF release from the PRP in a dose-dependent fashion (43,44). In the United States, commercially available thrombin, derived from bovine plasma, is used as a “gold standard,” despite the fact that bovine thrombin has been associated some years ago with the development of antibodies to clotting factors V, XI, and thrombin, which had occasionally lead to life-threatening coagulopathies (45). Alternatively, PRP can be activated by autologous thrombin, produced with commercially available thrombin production kits, which either use autologous whole blood sequestered PPP or PRP (Table 3). Recently, Tsay et al. (46) reported that the use of a synthetic peptide that mimics thrombin known as peptide-6 SFLLRN (TRAP). Activation with TRAP results in a more sustained release of the PGF with less PG retraction and higher PDGF-AB and TFG-β concentrations. The mechanism of this sustained release phenomenon is unclear, but it may possibly be useful in the development and maturation of platelet-enriched bone grafts and also in tissue healing.
Table 3.
Autologous thrombin processing kits.
| Autologous Thrombin Kit Manufacturer |
Required Volume Product |
Thrombin Volume |
Activator Reagent | Thrombin Activity |
Ratio AT:PRP |
|---|---|---|---|---|---|
| ActivAT, Dideco, Mirandola, Italy | 12 mL PPP | 5–6 mL | Ethanol 17%, glass beads, calcium chloride 10% | 50 IU | 1:10 |
| Magellan, Medtronic, Minneapolis, MN | 3 mL WB | 2.5 mL | Glass fiber, calcium chloride 10% | 10–15 IU | 1:4 |
| Petri dish, Catharina Hospital | Variable PPP/PRP | Variable | Glass Petri dish, calcium chloride 10% | 10–15 IU | 1:4 |
| Thrombin Assessing Device, Thermogenesis, Rancho Cordova, CA | 9.5–10.5 mL PPP | 8 mL | Ethanol 18.8%, ceramic beads, calcium chloride 10% | 40–50 IU | 1:3 |
The ratio AT:PRP refers to the manufacturer’s proposed ratio for mixing PRP with thrombin to produce PG.
PPP, platelet poor plasma; WB, whole blood; PRP, platelet rich plasma; AT, autologus thrombin; UB, international units.
Mixing PRP with thrombin and calcium chloride to antagonize the anticoagulative effect of the citrate present in the predonation blood bag will result in the activation of the platelet concentrate with the development of the viscous PG solution. Thereafter, the PG can be exogenously applied with a syringe or as a solid clotted jelly mass applied to soft tissues, bone, or synthetic bone.
From a surgical point of view, an “ideal” PG procedure is often defined as a procedure forming a platelet coagulum within 10 seconds. However, the formation of the coagulum is merely a function of the activated fibrinogen concentration, rather that the number of platelets.
PG Growth Factors
PGFs of the PG are peptides that promote cell proliferation, differentiation, chemotaxis, and induce the migration of various cells. Therefore, they play an important role in healing processes, as shown in several studies (47,48). We can classify growth factors into two groups: morphometric and mitogenic. The morphometric growth factors, involved in bone growth, can turn undifferentiated multipotent mesenchymal stem cells (MSCs) into immature and mature osteoprogenitor cells through the presence of the so called bone morphogenic proteins (BMPs) (49). These BMP growth factors belong to the TGF-β super family, a growth factor that is also present in PRP.
Most of the PGF in the PRP have mitogenic actions that increase the population of healing cells by mitogenesis. However, the action depends on the presence of further differentiated MSCs.
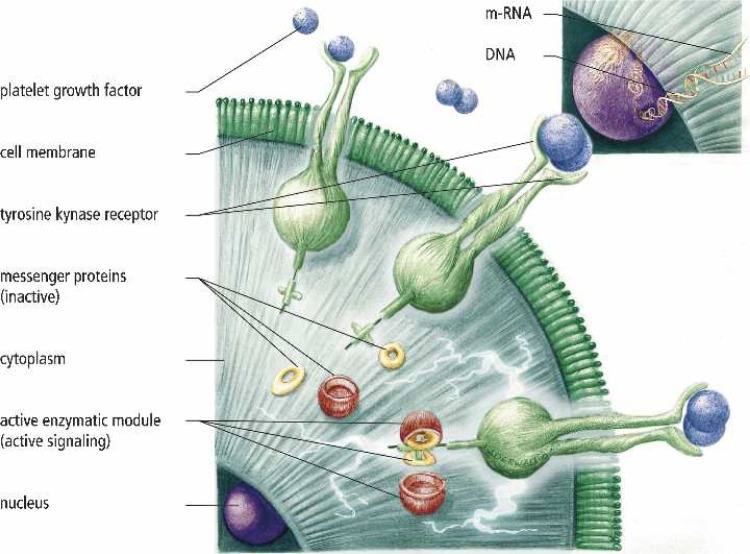
PGF Receptor Binding
After PG has been applied to tissues and the clot has retracted and degranulated, PGF will be deposited in the extracellular matrix. Thereafter, during matrix degradation, growth factors are released that interact and bind with the platelet tyrosine kinase receptor (TKR), present in the cell membranes of tissue cells (ligand–receptor interaction). The actual binding site is on the outer surface of the cell membrane. The TKR is a membrane spanning protein that extends into the cytoplasm of the cell. After growth factor interaction with the external part of the TKR, activation of (inactive) messenger proteins in the cytoplasm occurs. The activated TKR cytoplasmic tail now serves as a binding site for the messenger proteins. An activated protein is generated through a signalling cascade that is capable of entering the cell nucleus, where it triggers the genes responsible for controlling cell division. Subsequently, transcription of mRNA is induced, producing a biological response that initiates the cascades that induce tissue repair and regeneration (Figure 5) (50,51).
Figure 5.
Diagram showing the mechanism by which PGF binds to the tyrosine kinase receptor. Extracellular PGF receptor binding results in intracellular signalling transmission to the cell nucleus.
Growth factors seem to have three different modes of action. They may act in a paracrine manner, where the growth factors are secreted by one cell stimulating a neighboring second cell. Second, they can act in an autocrine manner, where the cell releases factors act on itself, increasing its own activity. Third, in an endocrine manner, where growth factors may influence a cell that is different in phenotype from the original cell and is located at a remote anatomical site. Because of the unique modes of action, growth factors are capable of inducing effects on multiple cell types and may therefore provoke a series of cellular functions in different tissues (52,53).
The next paragraph gives some background information on two of the most well-described factors and on a recently evaluated growth factor present in PRP. In Table 4, a synopsis of the most well-known PRP growth factors is provided along with a description of the source and specific function, (16,54–63).
Table 4.
Synopsis of growth factors present in PRP.
| Growth Factor | Source | Function | Reference |
|---|---|---|---|
| Transforming Growth Factor-beta, TGF-β | Platelets, extracellular matrix of bone, cartilage matrix, activated TH1 cells and natural killer cells, macrophages/monocytes and neutrophils | Stimulates undifferentiated mesenchymal cell proliferation; regulates endothelial, fibroblastic and osteoblastic mitogenesis; regulates collagen synthesis and collagenase secretion; regulates mitogenic effects of other growth factors; stimulates endothelial chemotaxis and angiogenesis; inhibits macrophage and lymphocyte proliferation | 16, 53 |
| Basic Fibroblast Growth Factor, bFGF | Platelets, macrophages, mesenchymal cells, chondrocytes, osteoblasts | Promotes growth and differentiation of chondrocytes and osteoblasts; mitogenetic for mesenchymal cells, chondrocytes and osteoblasts | 54, 55 |
| Platelet Derived Growth Factor, PDGFa-b | Platelets, osteoblasts, endothelial cells, macrophages, monocytes, smooth muscle cells | Mitogenetic for mesenchymal cells and osteoblasts; stimulates chemotaxis and mitogenesis in fibroblast/glial/smooth muscle cells; regulates collagenase secretion and collagen synthesis; stimulates macrophage and neutrophil chemotaxis | 16, 56 |
| Epidermal Growth Factor, EGF | Platelets, macrophages, monocytes | Stimulates endothelial chemotaxis/angiogenesis; regulates collagenase secretion; stimulates epithelial/mesenchymal mitogenesis | 57, 58 |
| Vascular Endothelial Growth Factor, VEGF | Platelets, endothelial cells | Increases angiogenesis and vessel permeability, stimulates mitogenesis for endothelial cells | 59, 60 |
| Connective Tissue Growth Factor, CTGF | Platelets through endocytosis from extracellular environment in bone marrow | Promotes angiogenesis, cartilage regeneration, fibrosis and platelet adhesion | 61, 62 |
PDGF
PDGF is a glycoprotein with a molecular weight of ap-proximately 30 kd and with two disulphide-bonded polypeptides, referred to as A and B chains. There are three isoforms, PDGF-AA, -BB, and -AB (57,59). PDGF is not only found in the dense α-granules of the platelet but is also synthesized and secreted by macrophages and the endothelium. PDGF seems to be the first growth factor present in a wound and initiates connective tissue healing through the promotion of collagen and protein synthesis. Furthermore, PDGF enhances the proliferation of bone cells and increases bone regeneration through osteoblastic mitogenesis. After the adhesion of PG to wound sites, PDGF will emerge from the degranulating platelets, and receptor activation will be initiated as described above (52,64,65). The most specific function of PDGF includes mitogenesis (attraction of cells to the wound site), angiogenesis (endothelial mitosis into functioning capillaries), and macrophage activation (biological wound debridement and a secondary source of growth factors). Bowen-Pope et al. (66) studied the production of PDGF and concluded that there are approximately 0.06 ng of PDGF per 106 platelets or about 1200 molecules per platelet. Therefore, one might assume that PG with a platelet count in excess of 3-to 5-fold the baseline level would have a profound effect on both wound healing and bone regeneration.
TGF-β
TGF-β is the name given to a group of proteins of molecular weight approximately 25 kd that are involved in the formation and development of many tissues (67). TGF-β is part of a super family to which BMP also belong. In humans, three subtypes of TGF-β are present, but TGF-β1 and TGF-β2 seem to be the most important with regard to general connective tissue repair and bone regeneration (68,69). TGF-β is found predominantly in platelets, which account for 95% of the total, while some is also found in macrophages in a latent form. TGF-β has an inhibitory effect on cell growth of many tissues, except for MSCs, where proliferation is enhanced. The other functions of TGF-β are to promote chemotaxis and mitogenesis of fibroblasts and osteoblastic precursor cells, which will later differentiate into mature osteoblasts, and also to stimulate osteoblast deposition at the collagen matrix of the tissue wound healing and bone matrix regions (70). TGF-β acts both in an autocrine and paracrine fashion, making it a growth factor with long-term healing and bone regeneration capabilities (71). Some concern on the use of TGF-β has been muted by Dieudonne et al. (72), who studied its the effect of on osteoclastic bone resorption in an experimental setting. They concluded that low concentrations have a stimulatory effect on bone cell proliferation, whereas at higher concentrations, proliferation is suppressed.
In PRP, both PDGF and TGF-β are present, implying that a mixture of combinations of growth factors will always be present at tissue sites. This unavoidable effect seems to be beneficial toward tissue healing because various results are reported on the synergistic effect of different growth factors (23,24,50).
Connective Tissue Growth Factor
Very recently, Kubota et al. (62) described a new PGF known as connective tissue growth factor (CTGF). Platelets adhere to CTGF at injured tissue wound sites, where it is overexpressed along with the platelet coagulation process. In their experiments, they showed that nonactivated platelets contain considerable amounts of CTGF that is released by activated PRP. It was also shown that the CTGF content in platelets is more than 20-fold higher than any other PGF and that CTGF endorses angiogenetic activity, cartilage regeneration, and fibrosis. Cicha et al. (63) showed that CTGF is expressed in bone marrow cells, but not by platelet-producing megakaryocytes, suggesting that the total amount of CTGF in platelets is the result of endocytosis from the extracellular environment in bone marrow. CTGF might be considered as an important member of the PGF family.
PG STUDIES
Animal Studies
There is a large variety of animal studies on PG research in the literature. Table 5 shows some of the more recent experimental studies (2,73–94). The results tend to be confusing, and the reader might conclude that the animal data on PG studies is conflicting. One concern is that a variety of different animal species has been used, and often no information of platelet counts or growth factor numbers in the PRP is provided. Furthermore, methods showing PRP was produced are sometimes lacking. Some investigators even used damaged platelets, whereas others did not activate the PRP at all, as most clinicians would do in a clinical setting to release PGF. Also, “true” autologous PRP is not always achieved in small animals. It is therefore not surprising that Ranly et al. (93) observed a reduced osteoinductivity when human PRP in combination with demineralized bone was mixed and implanted in mice. In summary the different protocols used in these studies makes it difficult to draw conclusions. Therefore, the “no” treatment effect and negative outcome of the use of PG in animal studies should be interpreted with caution.
Table 5.
Summary of animal studies with the use of autologous platelet gel.
| Reference | Year | Study Animal | Medical Area | N | Outcome Effect |
|---|---|---|---|---|---|
| 73 | 01 | Rabbit | M-F: bone | 20 | + |
| 74 | 02 | Dog | M-F: peri-implant | 12 | + |
| 2 | 02 | Rabbit | Cranial: defect | 15 | − |
| 75 | 02 | Goat | M-F: bone | 28 | + |
| 76 | 02 | Dog | M-F: bone defect | 12 | |
| 77 | 03 | Mini pig | M-F: sinus graft | 12 | +/− |
| 78 | 03 | Sheep | M-F: bone | 12 | +/− |
| 79 | 03 | Pig | Bone implants | 15 | +/− |
| 80 | 03 | Mini pig | Dental implants | 12 | + |
| 81 | 04 | Rabbit | Cranial: defect | 15 | +/− |
| 82 | 04 | Dog | M-F: soft tissue | 8 | − |
| 83 | 04 | Goat | M-F: bone | 28 | + |
| 84 | 04 | Pig | SS: bone | 10 | − |
| 85 | 04 | Rabbit | M-F: bone | 10 | + |
| 86 | 04 | Rabbit | M-F: bone | 24 | + |
| 87 | 05 | Rabbit | Cranial: defect | 15 | − |
| 88 | 05 | Rabbit | M-F: sinus | 12 | − |
| 89 | 05 | Goat | M-F: bone | 6 | + |
| 90 | 05 | Sheep | M-F: bone | 10 | − |
| 91 | 05 | Dog | M-F: bone | 10 | + |
| 92 | 05 | Rat | M-F: bone | 30 | − |
| 93 | 05 | Mouse | OS: muscle | 30 | − |
| 94 | 05 | Rabbit | WC: implants | ? | + |
M-F, maxillofacial surgery; WC, wound care; SS, spinal surgery; OS, orthopaedic surgery; +, authors conclude a positive effect of PG treatment; +/−, means, respectively, a positive, doubtful, and negative effect of PG treatment; ?, animal numbers where not mentioned.
Human Clinical Studies
Autologous PRP was first used in cardiac surgery by Ferrari et al. in 1987 (95), as an autologous transfusion component after an open heart operation, to avoid homologous blood product transfusion. Later, in the early 1990s, PG was used as a byproduct of the sequestration procedure, as an alternative to fibrin sealant for the control of hemostasis in cardiac surgery (96,97). Since that time, an increasing number of institutions have used PG for optimization of soft tissue healing and bone regeneration. However, many case reports or small uncontrolled cases have been presented, but only a few have been published (1,3,98). The majority of these clinical studies showed a significantly improved effect on soft tissue healing and bone regeneration when PG was used. Strikingly, in most studies, data were obtained in oral and maxillofacial surgery, wound care, and cosmetic surgery, mainly because of the availability of histological specimens under these treatment conditions. Advocates of PG cite that it has a beneficial effect on tissue healing and bone growth and seems to reduce the incidence of infections and postoperative blood loss (28,99–104). Nevertheless, there are also clinical and experimental data that do not show any effect of PG applications. In Table 6, we summarize a series of 28 clinical human in vivo studies concerning autologous PG application that have been published in peer-reviewed journals (1,3–5,27–29,98–118). However, we ex-cluded abstracts presented at meetings, data obtained from in vitro studies, and results obtained with recombinant (single) growth factors. In seven studies, no positive effect of PG was shown. Three of those seven studies were in the maxillofacial field, including in total only nine patients (three patients per study). In the study by Froum et al. (1), the results obtained were from only three patients. Moreover, they all were treated with different bone graft materials and synthetic membranes in combination with PG. Shanaman et al. (3) also included only three patients in their study, so that no statistical analysis was possible. Furthermore, the conclusions drawn by these authors are only based on very limited data. The four other studies were conducted as spine surgery, where the PRP was concentrated with the a so-called autologous growth factor filter (AGF filter; Biomet, Warsaw, IN) (4,5,107,112). Kevy and Jacobson (119) observed in an in vitro study that the use of the AGF filter resulted in a significant activation of platelets in the concentrated PRP and in an unintentional release of PGF before the PG was applied to the tissue. They concluded that platelets were fragmented and bound to the hollow fibers because of repetitive passage of the PRP through the microporous fiber of the AGF filter. Therefore, the end product of use of the AGF filter is merely a platelet releasate rather than a viable concentrated PRP, normally containing nonactivated platelets until the moment of platelet activation and tissue application.
Table 6.
Summary of clinical studies with the use of autologous platelet gel.
| Reference | Year | Study Type | Medical Field | Patients in Study | Outcome Effect |
|---|---|---|---|---|---|
| 105 | 90 | PR | WC | 32 | + |
| 99 | 98 | PR | M-F | 88 | + |
| 106 | 99 | Case | M-F | 20 | + |
| 107 | 99 | R-case | SS* | 19 | +/− |
| 98 | 01 | Case | M-F | 3 | − |
| 108 | 01 | Case | ES | 121 | + |
| 100 | 01 | Case | CS | 20 | + |
| 28 | 01 | R-case | WC | 26.599 | + |
| 109 | 01 | Case | M-F | 3 | + |
| 110 | 01 | PR-B | CS | 8 | + |
| 3 | 01 | Case | M-F | 3 | − |
| 111 | 02 | Case | CS | 20 | + |
| 1 | 02 | Case | M-F | 3 | − |
| 102 | 02 | Case | M-F | 5 | + |
| 101 | 02 | Case | CS | 14 | + |
| 4 | 03 | Case | SS* | 57 | − |
| 112 | 04 | P-contr | SS* | 84 | − |
| 29 | 04 | Case | WC | 24 | + |
| 113 | 04 | Case-contr | M-F | 5 | + |
| 27 | 04 | Case | WC | 22 | + |
| 114 | 05 | PR | M-F | 18 | + |
| 5 | 05 | R-contr | SS* | 152 | − |
| 103 | 05 | R | CTS | 30 | + |
| 115 | 05 | Case | M-F | 8 | + |
| 116 | 05 | P-contr-B | M-F | 10 | + |
| 117 | 05 | PR | OS | 10 | + |
| 118 | 05 | Case-contr | M-F | 20 | + |
| 104 | 06 | PR | OS | 164 | + |
PR, prospective randomized; case, consecutive cases; R-case, retrospective case study consecutive cases; PR-B, prospective randomized blinded; case-contr, case study with patient being his/her own control; P-contr, prospective study with controls; R-contr, retrospective study with control patients; P-control-B, prospective consecutive study, single blinded; M-F, maxillo-facial surgery; WC, wound care; SS, spinal surgery; CS, cosmetic surgery; ES, eye surgery; OS, orthopaedic surgery; CTS, cardio thoracic surgery.
+, +/− means a positive, doubtful, and negative effect of PG treatment, respectively.
It is of concern that, based these considerations, several authors review the applications and results PRP and PG with human clinical and animal outcome data side-by-side (120–122). From a scientific point of view, human and animal trials should to be discussed and reviewed separately. Thus, any conclusions drawn from these reviews should be addressed with caution, especially because there are often no growth factor analysis determination kits available for some animal species. The differences in results obtained in humans vs. animals may therefore be caused by the great dissimilarity in species, because PG is a very sensitive autologous biological product and demands specific tissue receptor cells.
WHAT QUANTITY OF PLATELETS ARE REQUIRED TO ACHIEVE A POSITIVE EFFECT AFTER PG APPLICATION?
The question of the actual quantity of platelets required is often put forward by clinicians who need to know the minimal therapeutic level of the platelets in the PRP that would result in a significant improvement, using PG compared with standard treatments. At present, not many data are available to answer this question directly, and only indirect information exists. In 1998, Marx et al. (99) performed the first study showing a significant improvement in mandibular continuity defects when PRP was mixed with autogenous bone grafts. Their PRP contained three to four times higher platelet count compared with baseline values, although the average PRP platelet count found in their patients was just below 8 × 105/μL, a number that is lower than in most other studies. Nevertheless, they observed a significantly faster radiographic maturation and histomorphometrically denser bone regeneration. Nowadays, the latest separation devices produce PRP platelet counts in excess of 6–10 times the baseline platelet count values. Manufacturers tend to interpret a high platelet concentration as a quality performance indicator of their separation devices, regardless of the fact that these high concentrations may not be necessary or might even contribute to a negative outcome. Weibrich et al. (86) observed an advantageous effect with platelet concentrations of approximately 106/μL. Furthermore, they state that higher concentrations might have a paradoxically inhibitory effect.
Haynesworth et al. (123) studied the response of PRP on cellular mechanisms of adult human MSCs (ahMSCs) in vitro. In soft tissue and bone healing, ahMSCs are essential components for the repair processes (124,125). It was shown that release of PRP PGF stimulates the migration and proliferation of ahMSCs in a PRP concentration-dependent manner. A significant cellular response occurred with a 4-to 5-fold increase of platelet count compared with the baseline platelet count. In another study, Liu et al. (126) showed that the fibroblast proliferation and type I collagen production were augmented by a 4-to 5-fold increase in the PRP platelet count.
With these studies, it was shown that a PRP platelet count of approximately 106/μL is likely, which is in the therapeutically effective range, because in most patients, a whole blood platelet count between 1.5 and 3 × 105/μLis found. A PRP platelet count with a four to five times higher baseline value seems to be adequate to achieve significant outcome using a PG application.
SAFETY ISSUES
Patients who are considered to be candidates for a PG application must undergo a minor hematological evaluation to exclude blood disorders or platelet dysfunction. The authors feel the following are relative contraindications for PG application: a platelet count less than 105/μL, a hemoglobin level less than 10 g/dL, presence of a tumor in the wound bed or metastatic disease, and other active infections. PRP preparation and PG production is safely executed by certified perfusionists or other health care professionals who have been trained in proper aseptic pheresis and transfusion techniques, complying with generally accepted safety requirements. Any concerns of immunogenic reactions or disease transmission such as HIV and hepatitis that exist with homologous blood products are eliminated because PRP is produced from autologous blood.
As discussed earlier, the use of bovine thrombin should be decrease, because there are high quality and safer alternatives available for activating PRP.
To our knowledge, no wound infections after PG applications have been reported, although the preparation of PG demands many processing steps, and thus theoretically, there is the possibility of contamination (119).
Some of the commercial available autologous thrombin kits require the use of ethanol. The safety of using a small amount of ethanol in the PG on nerves was studied in an animal model by de Somer et al. (127). It was concluded that the myelin sheaths were normal in appearance, with no axonal swelling and no collagen necrosis caused by the ethanol.
Despite the fact that PGF has mitogenic properties, there is no evidence that the growth factors in PG promote tumor growth or that they are involved in carcinogenesis (128,129). Furthermore, Scott and Pawson (130) showed that growth factors act on cell membranes and not on the cell nucleus and that PGF activates normal rather than abnormal gene expression. However, the effect of PG during tumor surgery should be studied before using it under these circumstances.
CONCLUSIONS
Platelets are unique blood elements initiating hemostasis and healing processes. Therefore, the potential of autologous PG growth factor applications are numerous. PRP contains a high concentration of platelets, which can be activated to form PG and to release PGF for therapeutic use. Data from human and animal studies provide both direct and indirect evidence that PGF plays a considerable role in tissue regenerative processes. Nevertheless, some uncertainty is present, and some clinicians remain skeptical of the clinical benefits of PG and are uncertain about the ideal biological setting (e.g., percentage of vital bone cells, volume of PRP) for the application of the PG. Therefore, randomized controlled trials are required to study the potential of the use of PG and to provide material for sound clinical decision-making in the near future.
ACKNOWLEDGMENTS
The authors thank J. Derwall and E. Lemmens en I. van Hezik from www.dlgraphics.nl, Kerkrade, The Netherlands, for preparation of the illustrations.
REFERENCES
- 1.Froum SJ, Wallace SS, Tarnow DP, et al. Effect of platelet rich plasma on bone growth and osseointegration in human maxillary sinus grafts: Three bilateral case reports. Int J Periodont Restor Dent. 2002;22:45–49. [PubMed] [Google Scholar]
- 2.Aghaloo TL, Moy PK, Freymiller EG.. Investigations of platelet rich plasma in rabbit cranial defects. A pilot study. J Oral Maxillofac Surg. 2002;60:1176–81. [DOI] [PubMed] [Google Scholar]
- 3.Shanaman R, Filstein MR, Danesh-Meyer MJ.. Localized ridge augmentation using GBR and platelet rich plasma: Three case reports. Int J Periodont Restor Dent. 2001;21:343–55. [PubMed] [Google Scholar]
- 4.Weiner BK, Walker M.. Efficacy of autologous growth factors in lumbar intertransverse fusions. Spine. 2003;28:1968–71. [DOI] [PubMed] [Google Scholar]
- 5.Carreon LY, Glassman SD, Anekstein Y, Puno RM.. Platelet gel (AGF) fails to increase fusion rates in instrumented posterolateral fusions. Spine. 2005;30:243–7. [DOI] [PubMed] [Google Scholar]
- 6.Zucker-Franklin C.. Megakaryocytes and platelets. In: Zucker-Franklin D, Greaves MF, Grossi CE, Marmont AM, eds. Atlas of Blood Cells. Philadelphia, PA: Lea & Febiger; 1998; 621 [Google Scholar]
- 7.Sixma JJ, Sakariassen KS, Beeser-Visser NH, et al. Adhesion of platelets to human artery subendothelium: Effects of factor VIII-von Willebrand factor of various multimerc composition. Blood. 1984;63:128–39. [PubMed] [Google Scholar]
- 8.Fox JEB.. The platelet cytoskeleton. In: Verstraete M, Vermylen J, Lijnen R, Arnout J, eds. Thrombosis and Haemostasis. Leuven, Belgium: Leuven University Press; 1987; 175. [Google Scholar]
- 9.Dhall TZ, Shah GA, Ferguson IA, et al. Fibrin network structure: modification by platelets. Thromb Haemostas. 1983;49:42–6. [PubMed] [Google Scholar]
- 10.Stover EP, Siegel LC, Hood PA, et al. Intraoperatively prepared platelet gel as an alternative to fibrin glue in dermal wound repair. Transfusion. 1996;36(suppl):S46. [Google Scholar]
- 11.McGrath MH.. Peptide growth factors and wound healing. Clin Plast Surg. 1990;17:421–32. [PubMed] [Google Scholar]
- 12.Hunt TK.. Basic principles of wound healing. J Trauma. 1990;30:S122–8. [DOI] [PubMed] [Google Scholar]
- 13.Robson MC.. Growth factors as wound healing agents. Curr Opin Biotechnol. 1991;2:863–7. [DOI] [PubMed] [Google Scholar]
- 14.McNeil PL.. Cell wounding and healing. Am Sci. 1991;79:222–35. [Google Scholar]
- 15.Cromack DT, Pierce GF, Mustoe TA.. TGF-β and PDGF medicated tissue repair: Identifying mechanisms of action using impaired and normal models of wound healing. In: Barbul A, Caldwell M, Eagl-stein W, Hunt T, Marshall D, Pines E, Skower G, eds. Clinical and Experimental Approaches to Dermal and Epidermal Repair: Normal and Chronic Wounds. New York: Wiley Liss; 1991; 359–73. [Google Scholar]
- 16.Pierce GF, Mustoe TA, Altrock BW, Deuel TF, Thomason A.. Role of platelet-derived growth factor in wound healing. J Cell Biochem. 1991;45:319–26. [DOI] [PubMed] [Google Scholar]
- 17.Mustoe TA, Pierce GF, Morisima C, Deuel TF.. Growth factor induced acceleration of tissue repair through direct and inductive activities in a rabbit dermal ulcer model. J Clin Invest. 1991;87:694–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cromack DT, Porras-Reyes B, Mustoe TA.. Current concepts in wound healing: growth factor and macrophage interaction. J Trauma. 1990;30:S129–33. [DOI] [PubMed] [Google Scholar]
- 19.Nanney LB.. epidermal and dermal effects of epidermal growth factor during wound repair. J Invest Dermatol. 1990;94:624–9. [DOI] [PubMed] [Google Scholar]
- 20.Antoniades HN, Galanopoulos T, Neville-Golden J, Kiritsy CP, Lynch SE.. Injury induces in vivo expression of platelet-derived growth factor (PDGF) and PDGF receptor mRNAs in skin epidermal cells and PDGF mRNA in connective tissue fibroblasts. Proc Natl Acad Sci USA. 1991;88:565–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stenberg BD, Phillips LG, Hokanson JA, Heggers JF, Robson MC.. Effects of bFGF on the inhibition of contraction caused by bacteria. J Surg Res. 1991;50:47–50. [DOI] [PubMed] [Google Scholar]
- 22.Sprugel KH, Greenhalgh DG, Murray MJ, Ross R.. Platelet derived growth factor and impaired wound healing. In: Barbul A, Caldwell M, Eaglstein W, Hunt T, Marshall D, Pines E, Skower G, eds. Clinical and Experimental Approaches to Dermal and Epidermal Repair: Normal and Chronic Wounds. New York: Wiley Liss; 1991; 327–40. [PubMed] [Google Scholar]
- 23.Lynch SE, Nixon JC, Colvin RB, Antoniades HN.. Role of platelet-derived growth factor in wound healing: synergistic effects with other growth factors. Proc Natl Acad Sci USA. 1987;84:7696–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brown RL, Breeden MP, Greenhalg DG.. PDGF and TGF-alpha act synergistically to improve wound healing in the genetically diabetic mouse. J Surg Res. 1994;56:562–70. [DOI] [PubMed] [Google Scholar]
- 25.Kells AF, Coats SR, Schwartz HS, Hoover RL.. TGF-beta and PDGF act synergistically in affecting the growth of human osteoblast-enriched cultures. Connect Tissue Res. 1995;31:117–24. [DOI] [PubMed] [Google Scholar]
- 26.Mazzuco L, Medici D, Serra M, et al. The use of autologous platelet gel to treat difficult-to-heal wounds: a pilot study. Transfusion. 2004;44:1013–8. [DOI] [PubMed] [Google Scholar]
- 27.Henderson JL, Cupp CL, Ross EV, et al. The effects of autologous platelet gel on wound healing. Ear Nose Throat J. 2003;82:598–602. [PubMed] [Google Scholar]
- 28.Margolis DJ, Kantor J, Santanna J, Strom BL, Berlin JA.. Effectiveness of platelet releasate for the treatment of diabetic neuropathic foot ulcers. Diabetes Care. 2001;24:483–8. [DOI] [PubMed] [Google Scholar]
- 29.Crovetti G, Martinelli G, Issi M, et al. Platelet gel for healing cutaneous chronic wounds. Transfus Apher Sci. 2004;30:145–51. [DOI] [PubMed] [Google Scholar]
- 30.Canalis E, McCarthy TL, Centrella M.. Growth factors and cytokines in bone cell metabolism. Annu Rev Med. 1991;42:17–24. [DOI] [PubMed] [Google Scholar]
- 31.Slater M, Patava J, Kingham K, Mason RS.. Involvement of platelets in stimulating osteogenic activity. J Orthop Res. 1995;13:655–63. [DOI] [PubMed] [Google Scholar]
- 32.Bolander ME.. Regulation of fracture repair by growth factors. Proc Soc Exp Biol Med. 1992;200:165–70. [DOI] [PubMed] [Google Scholar]
- 33.Thiede MA, Smock SL, Petersen DN, Grasser WA, Nishimoto SK, Thompson DD.. Production of osteocalcin by platelets: a potentially important link of platelet action in bone turnover. J Bone Miner Res. 1993;8:S147–51. [Google Scholar]
- 34.Robey PG, Young KC, Flanders KC, et al. Osteoblasts synthesize and respond to transforming growth factor-type beta (TGF-beta) in vitro. J Cell Biol. 1987;105:457–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bourquie WT, Gross M, Hall BK.. Expression of four growth factors during frcture repair. Int J Dev Biol. 1993;37:573–9. [PubMed] [Google Scholar]
- 36.Kasperk CH, Wergedal JE, Mohan S, Long DL, Lau KH, Baylink DJ.. Interaction of growth factors present in bone matrix with bone cells: effects on DNA synthesis and alkaline phosphatise. Growth Factors. 1990;3:147–58. [DOI] [PubMed] [Google Scholar]
- 37.Katagiri T, Lee T, Takeshima H, Suda H, Omura S.. Transforming growth factor-beta modiulates proliferation and differentiation of mouse clonal osteoblastic MC3T3-E1 cells depending on their maturation stages. Bone Miner. 1990;11:285–93. [DOI] [PubMed] [Google Scholar]
- 38.Piche JE, Graves DT.. Study of the growth factor requirements of human bone-derived cells: a comparison with human fibroblasts. Bone. 1989;10:131–8. [DOI] [PubMed] [Google Scholar]
- 39.Kalfas IH.. Principles of bone healing. Neurosurg Focus. 2001;10:1–8. [DOI] [PubMed] [Google Scholar]
- 40.Solheim E.. Growth factors in bone. Int. Orthop. 1998;22:410–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Helm GA.. Bone graft substitutes for the promotion of spinal arthrodesis. Clin Neurosurg. 2005;52:250–255. [PubMed] [Google Scholar]
- 42.Gandhi A, Dumas C, O’Conner JP, Parsons JR, Lin SS.. The effects of local platelet delivery on diabetic fracture healing. Bone. 2006;38:540–6. [DOI] [PubMed] [Google Scholar]
- 43.Lacoste E, Martineau I, Gagnon G.. Platelet concentrates: effects of calcium and thrombin on endothelial cell proliferation and growth factor release. J Periodontol. 2003;74:1498–507. [DOI] [PubMed] [Google Scholar]
- 44.Chouhan VD, De La Cadena RA, Nagaswani C, Weisel JW, Kajani M, Rao AK.. Simultaneous occurrence of human antibodies directed against fibrinogen, thrombin, and factor V following exposure to bovine thrombin: effects on blood coagulation, protein C activation and platelet function. Thromb Haemost. 1997;77:343–9. [PubMed] [Google Scholar]
- 45.Zehnder JL, Leung LLK.. Development of antibodies to thrombin and factor V with recurrent bleeding in a patient exposed to topical bovine thrombin. Blood. 1990;76:2011–6. [PubMed] [Google Scholar]
- 46.Tsay RC, Burke A, Eisig SB, Lu HH, Landesberger R.. Differential growth factor retention by platelet-rich plasma composites. J Oral Maxillofac Surg. 2005;63:521–8. [DOI] [PubMed] [Google Scholar]
- 47.Giannoble WV.. Periodontal tissue engineering by growth factors. Bone. 1996;S19:S23–37. [DOI] [PubMed] [Google Scholar]
- 48.Giannoble WV, Hernandez RA, Finkelman RA, et al. Comparitive effects of platelet-derived growth factor-BB and insulin-like growth factor I, individually and in combination, on periodontal regeneration in Macaca fascicularis. J Periodontal Res. 1996;31:301–12. [DOI] [PubMed] [Google Scholar]
- 49.Hock JM, Canalis E.. Platelet-derived growth factor enhances bone cell replication, but not differentiated function of osteoblasts. Endocrinology. 1994;134:301–12. [DOI] [PubMed] [Google Scholar]
- 50.Schliephake H.. Bone growth factors in maxillofacial skeletal reconstruction. Int J Oral Maxillofac Surg. 2002;31:469–84. [DOI] [PubMed] [Google Scholar]
- 51.Antoniades HN, Williams LT.. Human platelet-derived growth factor: structure and functions. Fed Proc. 1983;81:2396–400. [PubMed] [Google Scholar]
- 52.Trippel SB, Coutts RD, Einhorn TA, Mundy GR, Rosenfeld RG.. Growth factors as theurapeutic agents. J Bone Joint Surg Am. 1996;78:1272–86. [Google Scholar]
- 53.Bames GL, Kostenuik PJ, Gerstenfeld LC, Einhorn TA.. Growth factor regulation of fracture repair. J Bone Miner Res. 1999;14:1805–15. [DOI] [PubMed] [Google Scholar]
- 54.Rosier RN, O’Keefe RJ, Hicks DG.. The potential role of trans-forming growth factor beta in fracture healing. Clin Orthop. 1998;(355 Suppl):S294–300. [DOI] [PubMed] [Google Scholar]
- 55.Wang JS.. Basic fibroblastic growth factor for stimulation of bone formation in osteoinductive or conductive implants. Acta Orthop Scand. 1996;269:1–33. [DOI] [PubMed] [Google Scholar]
- 56.Friesel RE, Maciag T.. Molecular mechanisms of angiogenesis: fibroblast growth factor signal transduction. FASEB J. 1995;9:919–25. [DOI] [PubMed] [Google Scholar]
- 57.Canalis E, McCarthy TL, Centrella M.. Effects of platelet-derived growth factor on bone formation in vitro. J Cell Physiol. 1989;140:530–7. [DOI] [PubMed] [Google Scholar]
- 58.Steenfos HH.. Growth factors and wound healing. Scand J Plast Reconstr Hand Surg. 1994;28:95–105. [DOI] [PubMed] [Google Scholar]
- 59.Martin P, Hopkinson-Woolley J, McClusky J.. Growth factors and cutaneous wound repair. Prog Growth Factor Res. 1992;4:25–44. [DOI] [PubMed] [Google Scholar]
- 60.Rhee JS, Black M, Schubert U, et al. The functional role of blood platelet components in angiogenesis. Thromb Haemost. 2004;92:394–402. [DOI] [PubMed] [Google Scholar]
- 61.Hom DB, Maisel RH.. Angiogenic growth factors: Their effects and potential in soft tissue wound healing. Ann Otol Rhinol Laryngol. 1992;101:349–54. [DOI] [PubMed] [Google Scholar]
- 62.Kubota S, Kawata K, Yanagita T, Doi H, Kitoh T, Takigawa M.. Abundant retention and release of connective tissue growth factor (CTGF/CCN2) by platelets. J Biochem (Tokyo). 2004;136:279–82. [DOI] [PubMed] [Google Scholar]
- 63.Cicha I, Garlichs CD, Daniel WG, Goppelt-Struebe M.. Activated human platelets release connective tissue growth factor. Thromb Haemost. 2004;91:755–60. [DOI] [PubMed] [Google Scholar]
- 64.Lieberman JR, Daluiski A, Einhorn TA.. The role of growth factors in the repair of bone. J Bone Joint Surg Am. 2002;84:1032–44. [DOI] [PubMed] [Google Scholar]
- 65.Heldin CH, Miyazono K, ten Dijke P.. TGF-beta signalling from cell membrane to nucleus through SMAD proteins. Nature. 1997;390:465–71. [DOI] [PubMed] [Google Scholar]
- 66.Bowen-Pope DF, Vogel A, Ross R.. Production of platelet-derived growth factor-like molecules reduced expression of platelet-derived growth factor receptors accompany transformation by a wide spec-trum of agents. Proc Natl Acad Sci USA. 1984;81:2396–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gao J, Symons AL, Bartold PM.. Expression of transforming growth factor-beta 1 (TGF-1) in the developing periodontium of rats. J Dent Res. 1998;77:1708–16. [DOI] [PubMed] [Google Scholar]
- 68.Roberts AB, Spron MB.. Physiological actions and clinical applications of transforming growth factor –beta (TGF-beta). Growth Factors. 1993;8:1–9. [DOI] [PubMed] [Google Scholar]
- 69.Miyazono K, ten Dijke P, Ichiyo H, Heldin CH.. Receptors for transforming growth factor-bata. Adv Immunol. 1994;55:181–220. [PubMed] [Google Scholar]
- 70.Mohan S, Baylink DJ.. Bone growth factors. Clin Orthop Rel Res. 1991;263:30–43. [PubMed] [Google Scholar]
- 71.Beck LS, De Guzman L, Lee WP, Yvette XU, Siegel MW, Amento EP.. One systemic administration of transforming growth factor-beta 1 reverses age or glucocorticoid-impaired wound healing. J Clin Invest. 1993;92:2841–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dieudonne SC, Foo P, van Zoeken EJ, Burger EH.. Inhibiting and stimulating effects of TGF-1 on osteoclastic bone resorption in fetal mouse bone organ cultures. J Bone Miner Res. 1991;6:479–87. [DOI] [PubMed] [Google Scholar]
- 73.Kim ES, Park EJ, Choung PH.. Platelet concentration and its effect on bone formation in calvarial defects: an experimental study in rabbits. J Prosthet Dent. 2001;86:428–33. [DOI] [PubMed] [Google Scholar]
- 74.Kim SG, Chung CH, Kim YK, Park JC, Lim SC.. Use of particulate dentin-plaster of Paris combination with/without platelet-rich plasma in the treatment of bone defect around implants. Int J Oral Maxillofac Surg. 2002;17:86–94. [PubMed] [Google Scholar]
- 75.Fennis JP, Stoelinga PJ. Jansen JA.. Mandibular reconstruction: a clinical and radiographic animal study on the use of autogenous scaffolds and platelet-rich plasma. Int J Oral Maxillofac Implants. 2002;31:281–6. [DOI] [PubMed] [Google Scholar]
- 76.Kim SG, Kim WK, Park JC, Kim HJ.. A comparative study of osseointegration of Avana implants in demineralised freeze-dried bone alone or with platelet-rich plasma. J Oral Maxillofac Surg. 2002;60:1018–25. [DOI] [PubMed] [Google Scholar]
- 77.Furst G, Gruber R, Tangl S, et al. Sinus grafting with autogenous platelet-rich plasma and bovine hydroxyapetite. A histomorphometric study in minipigs. Clin Oral Implants Res. 2003;14:500–8. [DOI] [PubMed] [Google Scholar]
- 78.Jakse N, Tangl S, Gilli R, et al. Influence of PRP on autogenous sinus grafts. An experimental study on sheep. Clin Oral Implants Res. 2003;14:578–83. [DOI] [PubMed] [Google Scholar]
- 79.Schegel KA, Kloss FR, Kessler P, Schultze-Mosgau S, Nkenke E, Wiltfang J.. Bone conditioning to enhance implant osseointegration: an experimental study in pigs. Int J Oral Maxillofac Implants. 2003;18:505–11. [PubMed] [Google Scholar]
- 80.Zechner W, Tangl S, Tepper G, et al. Influence of platelet-rich plasma on osseous healing of dental implants: a histologic and his-tomorphometric study in minipigs. Int J Oral Maxillofac Implants. 2003;18:15–22. [PubMed] [Google Scholar]
- 81.Aghaloo TL, Moy PK, Freymiller EG.. Evaluation of platelet-rich plasma in combination with anorganic bovine bone in the rabbit cranium: a pilot study. Int J Oral Maxillofac Implants. 2004;19:59–65. [PubMed] [Google Scholar]
- 82.Choi BH, Im CJ, Huh JY, Suh JJ, Lee SH.. Effects of platelet-rich plasma on bone regeneration in autogenous bone graft. Int J Oral Maxillofac Surg. 2004;33:56–9. [DOI] [PubMed] [Google Scholar]
- 83.Fennis JP, Stoelinga PJ, Jansen JA.. Mandibular reconstruction: a histological and histomorphometric study on the use of autogenous scaffolds, particulate cortico-cancellous bone grafts and platelet rich plasma in goats. Int J Oral Maxillofac Surg. 2004;33:48–55. [DOI] [PubMed] [Google Scholar]
- 84.Li H, Zou X, Xue Q, Egund N, Lind M, Bunger C.. Anterior lumbar interbody fusion with carbon fiber cage loaded with bioceramics and platelet-rich plasma. An experimental study on pigs. Eur Spine J. 2004;13:354–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Yazawa M, Ogata H, Kimura A, Nakajima T, Mori T, Watanabe N.. Basic studies on the bone formation ability by platelet rich plasma in rabbits. J Craniofac Surg. 2004;15:439–46. [DOI] [PubMed] [Google Scholar]
- 86.Weibrich G, Hansen T, Kleis W, Buch R, Hitzler WE.. Effect of platelet concentration in platelet-rich plasma on peri-implant bone regeneration. Bone. 2004;34:665–71. [DOI] [PubMed] [Google Scholar]
- 87.Aghaloo TL, Moy PK, Freymiller EG.. Evaluation of platelet-rich plasma in combination with freeze-dried bone in the rabbit cranium. A pilot study. Clin Oral Implants Res. 2005;16:250–7. [DOI] [PubMed] [Google Scholar]
- 88.Butterfield KJ, Bennett J, Gronowicz G, Adams D.. Effects of platelet-rich plasma with autogenous bone graft for maxillary sinus augmentation in a rabbit model. J Oral Maxillofac Surg. 2005;63:370–6. [DOI] [PubMed] [Google Scholar]
- 89.Fennis JP, Stoelinga PJ, Merkx MA, Jansen JA.. Reconstruction of the mandible with a poly (D,L-lactide) scaffold, autogenous corticocancellous bone graft, and autogenous platelet-rich plasma: An animal experiment. Tissue Eng. 2005;11:1045–53. [DOI] [PubMed] [Google Scholar]
- 90.Grageda E, Lozada JL, Boyne PJ, Caplanis N, McMillan PJ.. Bone formation the maxillary sinus by using platelet-rich plasma: an experimental study in sheep. J Oral Implantol. 2005;31:2–17. [DOI] [PubMed] [Google Scholar]
- 91.Kovacs K, Velich N, Huszar T, Fenyves B, Suba Z, Szabo G.. Histomorphometric and densitometric evaluation of the effects of platelet-rich plasma on the remodeling of beta-tricalcium phosphate in beagle dogs. J Craniofac Surg. 2005;6:150–4. [DOI] [PubMed] [Google Scholar]
- 92.Pryor ME, Polimeni G, Koo KT, et al. Analysis of rat calvaria defects implanted with a platelet-rich plasma preparation: histologic and histometric observations. J Clin Periodontol. 2005;32:966–72. [DOI] [PubMed] [Google Scholar]
- 93.Ranly DM, McMillan J, Keller T, et al. Platelet-derived growth factors inhibits demineralized bone matrix-induced intramuscular cartilage and bone formation. A study of immunocompromised mice. J Bone Joint Surg Am. 2005;87:2052–64. [DOI] [PubMed] [Google Scholar]
- 94.Sclafani AP, Romo T III, Ukrainsky G, et al. Modulation of wound response and soft tissue ingrowth in synthetic and allogeneic implants with platelet concentrate. Arch Facial Plast Surg. 2005;7:163–9. [DOI] [PubMed] [Google Scholar]
- 95.Ferrari M, Zia S, Valbonesi M, et al. A new technique for hemodi-lution, preparation of autologous platelet-rich plasma and intraoperative blood salvage in cardiac surgery. Int J Artif Org. 1987;10:47–50. [PubMed] [Google Scholar]
- 96.Tawes RL, Sydorak GR, DuVall TB.. Autologous fibrin glue: The last step in operative hemostasis. Am J Surg. 1994;168:120–2. [DOI] [PubMed] [Google Scholar]
- 97.Oz MC, Jeevanandam V, Smith CR, et al. Autologous fibrin glue from intraoperatively collected platelet-rich plasma. Ann Thorac Surg. 1992;53:530–1. [DOI] [PubMed] [Google Scholar]
- 98.Anitua E.. The use of plasma-rich growth factors (PRGF) in oral surgery. Pract Proced Aesthet Dent. 2001;13:487–93. [PubMed] [Google Scholar]
- 99.Marx RE, Carlson ER, Eichstaedt RM, et al. Platelet-rich-plasma: growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:638–46. [DOI] [PubMed] [Google Scholar]
- 100.Man D, Plosker H, Winland-Brown JE.. The use of autologous platelet-rich plasma (platelet gel) and autologous platelet-poor plasma (fibrin glue) in cosmetic surgery. Plast Reconstr Surg. 2001;107:229–37. [DOI] [PubMed] [Google Scholar]
- 101.Valbonesi M, Giannini G, Migliori F, Dalla Costa R, Galli A.. The role of autologous fibrin-platelet glue in plastic surgery: a preliminary report. Int J Artif Organs. 2002;25:334–8. [DOI] [PubMed] [Google Scholar]
- 102.Robiony M, Polini F, Costa F, Politi M.. Osteogenesis distraction and platelet-rich plasma for bone restoration of the severely atrophic mandible: preliminary results. J Oral Maxillofac Surg. 2002;60:630–5. [DOI] [PubMed] [Google Scholar]
- 103.Englert SJ, Estep TH, Ellis-Stoll CC.. Autologous platelet gel applications during cardiovascular surgery: effect on wound healing. J Extra Corpor Technol. 2005;37:148–52. [PMC free article] [PubMed] [Google Scholar]
- 104.Everts PAM, Devilee RJJ, Brown-Mahoney CH.. Platelet gel and fibrin sealant reduce allogenic blood transfusions and in total knee arthroplasty. Acta Anaesth Scand. 2006;50:539–599. [DOI] [PubMed] [Google Scholar]
- 105.Knighton DR, Cirisi K, Fiegel VD, Schumerth S, Butler E, Cerra F.. Stimulation of repair in chronic, non healing, cutaneous ulcers using platelet-derived wound healing formula. Surg Gynecol Obstet. 1990;170:56–60. [PubMed] [Google Scholar]
- 106.Anitua E.. Plasma rich in growth factors: preliminary results of use in the preparation of future sites for implants. Int J Oral Maxillofac Implants. 1999;14:529–35. [PubMed] [Google Scholar]
- 107.Lowery GL, Kulkarni S, Pennisi AE.. Use of autologous growth factors in lumbal spinal fusion. Bone. 1999;(25 Suppl):S47–50. [DOI] [PubMed] [Google Scholar]
- 108.Blumenkranz MS, Ohana E, Shaikh S, et al. Adjuvant methods in macular hole surgery: intraoperative plasma-thrombin mixture and postoperative fluid-gas exchange. Ophthalmic Surg Lasers. 2001;32:198–207. [PubMed] [Google Scholar]
- 109.Pertrungaro PS.. Using platelet-rich plasma to accelerate soft tissue maturation in esthetic periodontal surgery. Compend Contin Educ Dent. 2001;22:729–34. [PubMed] [Google Scholar]
- 110.Powell DM, Chang E, Farrior EH.. Recovery from deep-plane rhytidectomy following unilateral wound treatment with autologous platelet gel: a pilot study. Arch Facial Plast Surg. 2001;3:245–50. [DOI] [PubMed] [Google Scholar]
- 111.Adler SC, Kent KJ.. Enhancing wound healing with growth factors. Facial Plast Surg Clin North Am. 2002;10:129–46. [DOI] [PubMed] [Google Scholar]
- 112.Castro FP Jr.. Role of activated growth factors in lumbar spinal fusions. J Spinal Disord Tech. 2004;17:380–4. [DOI] [PubMed] [Google Scholar]
- 113.Giannini G, Mauro V, Agostino T, Gianfranco B.. Use of autologous fibrin-platelet glue and bone fragments in maxillofacial surgery. Transfus Apher Sci. 2004;30:139–44. [DOI] [PubMed] [Google Scholar]
- 114.Camargo PM, Lekovic V, Weinlaender M, Vasilic N, Madzarevic M, Kenney EB.. A reentry study on the use of bovine porous bone mineral, GTR, and platelet-rich plasma in the regenerative treatment of intrabony defects in humans. Int J Periodontics Restorative Dent. 2005;25:49–59. [PubMed] [Google Scholar]
- 115.Merkx MA, Fennis JP, Verhagen CM, Stoelinga PJ.. Reconstruction of the mandible using preshaped 2.3 mm titanium plates, autogenous particulate cortico-cancellous bone grafts and platelet rich plasma: a report on eight patients. Int J Oral Maxillofac Surg. 2004;33:733–9. [DOI] [PubMed] [Google Scholar]
- 116.Kassolis JD, Reynolds MA.. Evaluation of the adjunctive benefits of platelet-rich plasma in subantral sinus augmentation. J Craniofac Surg. 2005;16:280–7. [DOI] [PubMed] [Google Scholar]
- 117.Savarino L, Cenni E, Tarabusi C, et al. Evaluation of bone healing enhancement by lyophilized bone grafts supplemented with platelet gel: A standardized methodology in patients with tibial osteotomy for genu varus. J Biomed Mater Res B Appl Biomater. 2006;76:364–72. [DOI] [PubMed] [Google Scholar]
- 118.Steigmann M, Garg AK.. A comparative study of bilateral sinus lifts performed with platelet-rich plasma alone versus alloplastic graft material reconstituted with blood. Implant Dent. 2005;14:261–6. [DOI] [PubMed] [Google Scholar]
- 119.Kevy SV, Jacobson MS.. Comparison of methods for point of care preparation of autologous platelet gel. J Extra Corpor Technol. 2004;36:28–35. [PubMed] [Google Scholar]
- 120.Freymiller EG, Aghaloo TL.. Platelet rich plasma: ready or not? J Oral Maxillofac Surg. 2004;62:484–8. [DOI] [PubMed] [Google Scholar]
- 121.Sanchez AR, Sheridan PJ, Kupp LI.. Is platelet rich plasma the perfect enhancement factor? A current review. Int J Oral Maxillofac Surg. 2003;18:93–103. [PubMed] [Google Scholar]
- 122.Marx RE.. Platelet rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004;62:489–96. [DOI] [PubMed] [Google Scholar]
- 123.Haynesworth SE, Kadiyala S, Liang LN, et al. Mitogenic stimulation of human mesenchymal stem cells by platelet release suggest a mechanism for enhancement of bone repair by platelet concentrates. Presented at the 48th Annual Meeting of the Orthopedic Research Society, Dallas, TX, February 2002. [Google Scholar]
- 124.Nakagawa H, Akita S, Fukui M, Fujii T, Akino K.. Human mesenchymal stem cells successfully improve skin-substitute wound healing. Br J Dermatol. 2005;153:29–36. [DOI] [PubMed] [Google Scholar]
- 125.Caplan AI.. Review: mesenchymal stem cells: cell-based reconstructive therapy in orthopedics. Tissue Eng. 2005;7:1198–211. [DOI] [PubMed] [Google Scholar]
- 126.Liu Y, Kalem A, Risto O, Wahlstrom O.. Fibroblast proliferation due to exposure to a platelet concentrate in vitro is pH dependent. Wound Repair Regen. 2002;5:336–340. [DOI] [PubMed] [Google Scholar]
- 127.De Somer F, De Brauwer V, Vandekerckhove M, Ducatelle R, Uyttendaele D, Van Nooten G.. Can autologous thrombin with a rest fraction of ethanol be used safely for activation of concentrated autologous platelets applied on nerves? Eur Spine J. 2006;15:501–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Landesberger R, Moses M, Karpatkin M.. Risks of using platelet rich plasma. J Oral Maxillofac Surg. 1998;56:1116–7. [DOI] [PubMed] [Google Scholar]
- 129.Martinez-Gonzales JM, Cano-Sanchez J, Gonzalo-Lafuente JC, Campo-Trapero J, Esparza-Gomez G, Seoane J.. Do ambulatory-use platelet-rich plasma (PRP) concentrates present risks? Med Oral. 2002;7:375–90. [PubMed] [Google Scholar]
- 130.Scott JD, Pawson T.. Cell communication: The inside story. Sci Am. 2000;282:72. [DOI] [PubMed] [Google Scholar]