Abstract:
In recent years, a steady decline in the number of perfusion education programs in the United States has been noted. At the same time, there has been a parallel decline in the number of students graduated from perfusion educational programs in the United States. Also, as noted by several authors, there has been an increase in demand for perfusion graduates. The decline in programs and graduates has also been noted in anesthesia and surgical residency programs. The shift is caused by a combination of economic and clinical factors. First, decreased reimbursement has led to reallocation of hospital resources. Second, the original enthusiasm for beating heart coronary artery bypass surgery was grossly overestimated and has led to further reallocation of hospital resources and denigration of cardiopulmonary bypass. This paper describes two models of perfusion education programs: serial perfusion education model (SPEM) and the distributed perfusion education model (DPEM). Arguments are presented that the SPEM has some serious limitations and challenges for long-term economic survival. The authors feel the DPEM along with dependence on tuition funding can survive the current clinical and economic conditions and allow the profession to adapt to changes in scope of practice.
Keywords: perfusion education, distributed perfusion educational model, serial educational model
Significant changes have occurred in the practice of medicine, medical economics, and medical education during the past 20 years. These changes are reflected in the practice of perfusion. The Information Age has impacted both the practice of medicine and education of medical professionals (1). Perfusion has seen a decline in the number of educational programs and a decrease in the total number of students who graduate from perfusion programs and enter the work force (2–4). An understanding of the problem becomes evident if you “follow the money.”
EVOLUTION OF PERFUSION AND PERFUSION EDUCATION
During the 1960s, perfusionists were typically technicians or nurses who received on-the-job training. Many of the early surgical programs were also associated with medical educational and research efforts. “Pump techs,” as this early group of perfusionists were called, possessed a wide variability in both education and abilities. Many of the “pump techs” possessed academic degrees in nursing, physiology, chemistry, and even veterinary medicine. The early leadership of perfusion societies, national certification, and research came from this group. These perfusionists formed the American Association of Pump Oxygenator Technicians in 1964 to establish standards of practice and provide continuing medical education for this fledgling field of study. Medical literature specific to cardiopulmonary bypass for perfusionists was nonexistent in the early 60s. The book Heart-Lung Bypass by Galletti and Brecher, published in 1962, was the first standard reference for perfusion. The American Society of Extra-Corporeal Technology (AmSECT) was formed from the American Association of Pump Oxygenator Technicians in 1967. In 1972, the first certification examinations were given. The certification responsibilities were finally shifted from AmSECT to the newly created American Board of Cardiovascular Perfusion (ABCP) in 1975.
The accreditation process began with AmSECT establishing the standards for perfusion educational programs in the 1970s. The process evolved as the ABCP began to accredit perfusion programs, although the ABCP recognized that certifying students from programs they had previously accredited created a conflict of interest. Therefore, in 1976, responsibility for accreditation of perfusion educational programs was moved to the Committee on Allied Health Education and Accreditation (CAHEA) with the formation of the Joint Review Committee for Perfusion Education (JRC-PE). In 1980, the JRC-PE published the first series of Essentials and Guidelines, finalizing the transition from ABCP accreditation to CAHEA accreditation. Today, the Commission on Accreditation of Allied Health Education Programs (CAAHEP) has replaced CAHEA as the overseer of allied health accreditation, and the Accreditation Committee-Perfusion Education (AC-PE) has replaced the JRC-PE as the group directly responsible for accreditation of perfusion educational programs. Effective November 2002, perfusion educational programs had to meet specific outcome-based objectives to remain accredited. Before that date, continuing accreditation was process based. Principally, the school completed an exhaustive self-study document, followed by an AC-PE site-visit of the program. The objectives of the outcome-based process are (a) a pass rate of 70% on the ABCP certification examination, (b) a class retention rate of 70%, and (c) a job placement rate of 80% (2).
SERIAL PERFUSION EDUCATION MODEL: THE FIRST EDUCATIONAL MODEL
Formal perfusion educational programs initially followed a serial perfusion educational model (SPEM). In these programs, the relationship between didactic and clinical education occurred naturally in the same institution, usually the hospital. Didactic and clinical educators were usually used by the hospital. The health care facilities provided the majority of income for the educational program, thus off-setting program expenses. The program faculty was paid primarily as perfusion health care providers and secondarily as perfusion educators. Surgeons were clearly the leaders of the program. The surgeons brought significant amounts of revenue to the hospital and had clout with the hospital administration. Everyone, including the hospital, had positive margins, and business was good. Surgeons were generally supportive of perfusion education.
DISTRIBUTED PERFUSION EDUCATION MODEL
As described by Riley et al. (5), the distributed perfusion education model (DPEM) is university based. Perfusion students are enrolled in the university setting for their didactic education. After the didactic training, the students move on to their clinical training that is provided by one or more clinical affiliation sites where the students interact with a variety of preceptors. During this period, the students may also be enrolled in Internet-based didactic courses and virtual classrooms, which are usually moderated by faculty members (5). The distributed piece of this model deals with the program’s access to multiple clinical affiliation sites located both locally and at a distance from the didactic program.
FACTORS INFLUENCING THE DECLINE OF THE SPEM
The number of perfusion education programs has declined dramatically over the past 11 years (Figure 1). The SPEM based programs compose the largest percentage of the programs that have closed (6). The biggest influence on the decline of the SPEM-based perfusion education programs has been the increased pressure placed by Congress, which enacted legislation called Diagnostic Related Groups (DRG) in 1983. Hospitals and other providers were paid by the federal government based on categorizing patients into a specific primary and secondary diagnosis. Hospitals and other providers were given incentives to keep the cost down. This was the beginning of “managed health care.” The providers and hospitals could earn a profit only if their costs were less than the amount of the DRG reimbursement. In reality, the health care system would be rewarded only if they rationed health care. For instance, new mothers and babies were encouraged to leave the hospital within 24 hours even though it increased morbidity and mortality rates.
Figure 1.
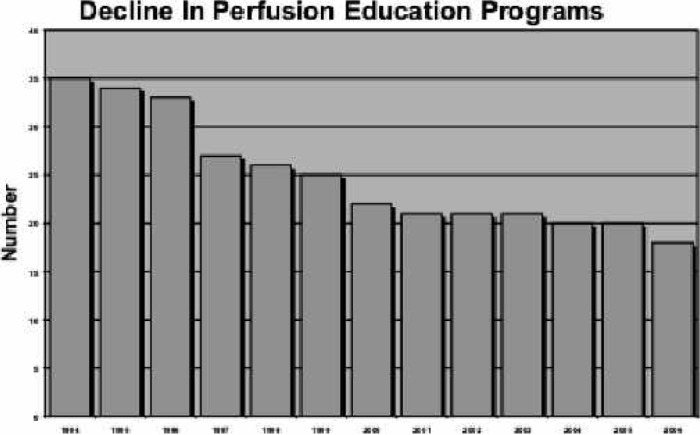
Decline in the number of perfusion educational programs from 1994 through 2005. Data from AC-PE web site.
“Fast Track” became the catch phrase in health care and cardiac surgery. Anesthesia patients were fast tracked to reduce patient recovery time, and ultimately, patient costs. Reducing the length of hospital stay became an overall goal in hospital practice. Health Maintenance Organizations used the Medicare reimbursement schedules as a means of reducing payments and enhancing revenue for their organizations. Many hospitals could not survive the newly imposed payment plan, and as a result, were sold or reorganized. Under the DRG payment system, only those hospitals and other health care providers providing the least expensive health care benefited. Initially, little concern was paid to quality. Hospitals concerns were focused on economic survival.
Elimination of education programs was another cost-cutting initiative. Nursing, medical and surgical residencies, and allied health programs were eliminated in the hospital-based educational programs. University hospitals were not exempt from the negative effects of drastically reduced income. When faced with economic survival or educational programs, the hospital administrators inevitably favored survival. Perfusion education programs were among the programs eliminated or placed on austerity measures by hospital administrations.
Another economic reality in the decline of SPEM per-fusion programs has been the dramatic growth in interventional cardiology. Interventional technology and procedure growth has shown considerable increases since the early 1980s, when the balloon angioplasty procedure became a treatment modality. As of 2001, this market represented 14.4 billion dollars with an average margin of 15.7%. Furthermore, the average length of stay was 2.9 days for these patients (7). Hospitals initiated new marketing techniques extolling the virtues of these less invasive procedures for patients with coronary artery disease, and the battle was on among the hospitals in a competitive geographic market. Hospitals were strongly encouraged by patients who observed the advertising to provide these new technology interventions.
Other factors have also had a negative impact on the SPEM (Table 1). There have been financial reductions in the cardiovascular manufacturer’s support of perfusion education because of the consolidation of the industry. The total impact of “beating heart surgery” on perfusion education has yet to be quantified, but it has had a negative impact on the emotional state of the profession and the public’s perception of the profession’s viability.
Table 1. Changes that caused the shift in economies for perfusion education programs.
| • Increase in invasive cardiology procedures | |
| • Fast track anesthesia | |
| • Length of stay | |
| • “You have to cut your costs to a minimum” | |
| • Advent of minimally invasive procedures | |
| • Cardiovascular manufacturers | |
| • Merged and sold | |
| • Many went out of business | |
| • Economic support for perfusion societies decreased | |
| • Advent of beating heart surgery | |
DECLINING NUMBER OF PERFUSION EDUCATIONAL PROGRAMS AND PERFUSION GRADUATES
As seen in Figure 1, in 1994, there were 35 perfusion educational institutions in the United States. Today, according to the CAAHEP web site, there are 20 active perfusion educational programs, representing a decrease of 43% since 1994. Furthermore, the number of graduating perfusion students has witnessed a decline from 224 in 1992 to 122 in 2003 (Figure 2). This dramatic decrease represents a reduction of 46%. To add to this precarious situation, there has been much discussion concerning the aging perfusionist. Searles et al. (3) predict that 575 perfusionists will retire during the next 5 years.
Figure 2.
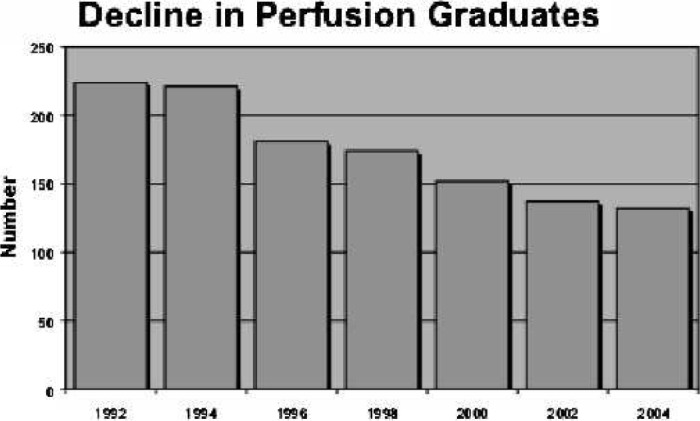
Decline in the number of perfusion graduates from 1992 through 2004. Data from AC-PE web site.
SUMMARY
A steady decline in the number of perfusion education programs in the United States has been noted. There also has been a decline in the number of graduating perfusion students while there has been an increase in the demand. These decreases are because of a combination of economic and clinical factors: reimbursement reduction, increased enthusiasm for interventional cardiology, decreased financial support from cardiovascular manufacturers, negative impact on the profession’s emotional state by “beating heart surgery,” and negative impact on public’s perception of cardiac surgery associated with “beating heart surgery.”
The perfusion educational programs most affected by these economic realities follow the SPEM because of the above-mentioned economic and clinical factors. The per-fusion educational programs least affected follow the DPEM. DPEM is the model of the future because the model is tuition driven. Because funding comes from tuition payments, program existence is not as dependent on changes in hospital priorities, decreasing clinical revenues, and subsidization by soft money. Also, because the program is distributed across an educational institution with multiple clinical sites, the risks are distributed if one of the clinical sites becomes inactive. In fact, loss of key program personnel or loss of key surgical support at a clinical site will not have as great an impact on the program’s success in contrast with the SPEM.
The authors feel the DPEM, along with dependence on tuition funding, can survive the current clinical and economic conditions and allow the profession to adapt to changes in scope of practice.
REFERENCES
- 1.Gorman PJ, Meier AH, Rawn C, Krummel TM.. The future of medical education is no longer blood and guts, it is bits and bytes. Am J Surg. 2000;180:353–6. [DOI] [PubMed] [Google Scholar]
- 2.Toomasian JM, Searles B, Kurusz M.. The evolution of perfusion education in America. Perfusion. 2003;18:257–65. [DOI] [PubMed] [Google Scholar]
- 3.Searles B, Darling EM, Riley JB, et al. . Supply and demand of the perfusion graduate. Part 1 and Part 2. AmSECT 42nd International Conference, Poster Session 2004. [Google Scholar]
- 4.Hall EF.. Mapping the literature of perfusion. Bull Med Libr Assoc. 1999;87:305–11. [PMC free article] [PubMed] [Google Scholar]
- 5.Riley JB, Austin JW, Holt DW, Searles BE, Darling EM.. Internet-based virtual classroom and educational management software enhance student’s didactic and clinical experiences in perfusion education programs. J Extra Corpor Technol. 2004;36:235–9. [PubMed] [Google Scholar]
- 6.Plunkett PF.. Perfusion education in the USA. Perfusion. 1997;12: 233–41. [DOI] [PubMed] [Google Scholar]
- 7.Cardiovascular Roundtable Analysis. Future of Cardiac Services. Sollucient LLC. 2003. [Google Scholar]


