Abstract
Introduction
In 2002, the Mount Sinai Center for Occupational and Environmental Medicine, with support from the National Institute for Occupational Safety and Health (NIOSH), began coordinating the World Trade Center (WTC) Worker and Volunteer Medical Screening Program (MSP) to monitor the health of qualified WTC responders. Enrolled participants were offered a clinical examination; interviewed to collect medical, mental health, and exposure information; and requested to complete a self-administered medical questionnaire. The objective of this study was to better understand work-related injuries and illnesses sustained on-site by WTC responders.
Methods
A descriptive analysis of select data from the MSP self-administered medical questionnaire was conducted. Data collected July 2002 through April 2004 from MSP participants enrolled at the Mount Sinai clinic were reviewed using univariate statistical techniques.
Results
Records from 7,810 participants were analyzed, with most participants associated with either the construction industry (n = 2,623, 34%) or law enforcement (n = 2,036, 26%). Approximately a third of the participants (n = 2,486, 32%) reported at least one injury or illness requiring medical treatment that was sustained during WTC work/volunteer activities. Of the total 4,768 injuries/illnesses reported by these participants, respiratory complaints were most common (n = 1,350, 28%), followed by traumatic injuries excluding eye injuries (n = 961, 20%), eye injuries/ailments (n = 709, 15%), chest pain (n = 375, 8%), headaches (n = 359, 8%), skin conditions (n = 178, 4%), and digestive system conditions (n = 163, 3%). Participants reported that 36% of injuries/illnesses were treated off-site and 29% were treated on-site, with the remaining not specifying treatment location. Off-site treatment was prevalent for respiratory complaints, psychological stress, and chest pain. On-site treatment was predominate for eye injuries/ailments and traumatic injuries excluding eye injuries.
Conclusion
Study results underscore the need for rapid deployment of personal protective equipment for disaster responders and medical care stations mobilized near disaster work-sites. Additionally, the results, many of which are comparable to findings from previous WTC studies where data were collected in real-time, indicate that a screening program such as the MSP may be effective in retrospectively providing general information on disaster responder demographics and work-related injuries and illnesses.
Keywords: emergency responders, emergency response volunteers, emergency response workers, World Trade Center, World Trade Center Worker and Volunteer Medical Screening Program
Introduction
In the days, weeks, and months following the September 11, 2001 attack, responders to the World Trade Center (WTC) site performed rescue, recovery, cleanup, and restoration operations. Due to the massive scale, these operations continued long-term, combining efforts of workers who belonged to diverse organizations. Volunteers providing support services also played a critical role, particularly during the first months. These workers and volunteers were exposed to numerous health and safety hazards.
One program monitoring WTC responder health was initiated in 2002 by the Mount Sinai Center for Occupational and Environmental Medicine with support from the National Institute for Occupational Safety and Health (NIOSH). Mount Sinai served as the coordinating entity for the program, called the WTC Worker and Volunteer Medical Screening Program* (MSP). Potential MSP participants, who self-identified following various outreach efforts, were screened to determine eligibility. To qualify, an individual must have worked and/or volunteered as part of WTC operations south of Canal Street in Manhattan, on the barge-loading piers in Manhattan, or in the Staten Island landfill for at least 24 hours during September 11–30, 2001 or for at least 80 hours between September 11 and December 31, 2001. WTC responders employed by the Office of the Chief Medical Examiner were eligible with no minimum hour requirements. Firefighters and Emergency Medical Services workers, collectively known as rescue workers, employed by the Fire Department of New York City (FDNY) did not participate because they had a separate program.1
Qualified MSP participants were offered a standardized clinical examination; interviewed by trained health care practitioners for medical, mental health, and exposure-assessment questionnaires; and asked to complete a self-administered medical questionnaire. Several studies using aggregated MSP data have been conducted to better understand WTC responder health burdens including respiratory2 and mental health3 issues.
WTC responder safety is another area warranting attention. Three studies that considered injuries as well as illnesses found that WTC responders experienced respiratory ailments, traumatic injuries, and eye ailments.4–6 Each study examined a slightly different population, and each had certain limitations. The study by Berríos-Torres et al4 had a reference period limited to the first months of WTC operations, and focused on select categories of rescue and recovery workers. With a similar reference period, the Perritt et al study5 focused only on Disaster Medical Assistance Team (DMAT) patients, and did not address work-relatedness. The third study had an 11-month reference period, and focused entirely on FDNY rescue workers.6
With an expanded reference period, information on injuries and illnesses, and a population that includes workers and volunteers, this article complements the previous WTC responder studies through an analysis of data from the MSP self-administered medical questionnaire. The objective of this study is to better understand work-related injuries and illnesses sustained on-site by WTC responders. The data were collected from July 2002 through April 2004 from MSP participants who were examined at the Mount Sinai clinic, provided written informed consent, agreed explicitly to permit data aggregation for research purposes, and provided Health Insurance Portability and Accountability Act (HIPAA) authorization.
Methods
Following study approval by the Mount Sinai School of Medicine Institutional Review Board, NIOSH received completely de-identified participant record data collected from the injury/illness module of the MSP self-administered medical questionnaire. Each record contained the following participant-reported information: dichotomized response to the question, “Did you have an injury or illness for which you received first aid or other medical treatment during your WTC work/volunteering;” total number of separate, medically treated injuries/illnesses; details on the four most severe injuries/illnesses (categorical data for type of injury/illness, categorical data for body part affected, narrative text describing the circumstances surrounding the injury/illness, and categorical data for treatment location); and narrative text describing any other WTC activity-related injuries/illnesses. Additional participant record data from other MSP components were also provided including age, gender, narrative text describing usual trade or profession (i.e., trade/profession on September 10, 2001), narrative text describing WTC work/volunteer activities, and labor union membership.
Information on usual trade or profession, WTC work/volunteer activities, and labor union membership was used by the authors to code each participant record with a variable describing the industry with which the participant was most likely associated during WTC work and/or volunteer activities. The codes were collapsed into three broad industry categories: “construction,” “law enforcement,” and “all other.”
Using information on type of injury/illness, body part affected, and narrative text, injuries and illnesses were coded according to the Occupational Injury and Illness Classification System (OIICS), which was developed by the Bureau of Labor Statistics7 and is commonly used for research on work-related injuries. Physicians, who worked under NIOSH contract and were OIICS-trained, coded each reported injury/illness with two OIICS variables: “nature” to describe the physical characteristics of the injury/illness and “body part” affected. Since participants could report up to four detailed injuries/illnesses and provide a description for other injuries/illnesses, OIICS coding resulted in each participant record containing up to five “nature” codes and five corresponding “body part” codes.
Categorical responses for the treatment location, reported for each detailed injury/illness (up to four per participant record), were collapsed by the authors from nine categories to three. The new categories were: (1) “on-site professional medical treatment,” which were reported as “WTC triage site” or “DMAT station;” (2) “off-site professional medical treatment,” reported as “emergency department,” “doctor office,” “hospital,” “other clinic,” or “USNS Comfort**;” and (3) “other unspecified treatment,” reported as “other medical” or “did not receive treatment.” The questionnaire instructed participants to report only injuries and illnesses requiring first aid or medical treatment. Although some participants reported that they “did not receive treatment” for an injury/illness, the narrative text often suggested that first aid was administered. Therefore, a reported injury/illness was never determined to be out-of-scope based on the treatment location response.
SAS 9.2 (SAS Institute, Cary, North Carolina, USA) was used for analysis of frequencies and cross-tabulations.8 Prevalence distributions for variables in select cross-tabulations were tested using the chi-square (χ2) statistic with the appropriate degrees of freedom (d.f.). Because MSP participants were not statistically sampled, nor were their reported data validated, tests of associations were not considered.
Results
A total of 7,810 participant records were analyzed. Demographic characteristics of these participants are shown in Table 1. The majority of participants were male (n = 6,728, 86%). Ages ranged from young adults (n = 12 for <21 years) to seniors (n = 16 for >70 years), and averaged 42 years. Participants were predominantly associated with either the construction industry (n = 2,623, 34%) or law enforcement (n = 2,036, 26%).
Table 1.
Demographic characteristics of studied participants (N = 7,810) in the World Trade Center (WTC) Worker and Volunteer Medical Screening Program, and distributions and rates by demographic characteristic for participants reporting at least one injury/illness (n = 2,486) sustained during WTC work/volunteer activities
| Characteristic | Total Participants (N = 7,810) | Percent* of Total | Participants Reporting an Injury/Illness (n = 2,486) | Injury/Illness Reporting Rate per 100 |
|---|---|---|---|---|
| Gender | ||||
| Male | 6,728 | 86 | 2,082 | 31 |
| Female | 1,082 | 14 | 404 | 37 |
| Age (years) | ||||
| <25 | 118 | 2 | 37 | 31 |
| 25–34 | 1,582 | 20 | 494 | 31 |
| 35–44 | 3,376 | 43 | 1,150 | 34 |
| 45–54 | 1,946 | 25 | 604 | 31 |
| 55–64 | 720 | 9 | 180 | 25 |
| >64 | 65 | 1 | 19 | 29 |
| Unknown | 3 | 0 | 2 | – |
| Industry Association | ||||
| Construction | 2,623 | 34 | 806 | 31 |
| Law Enforcement | 2,036 | 26 | 675 | 33 |
| All Other | 2,892 | 37 | 911 | 32 |
| Unknown | 259 | 3 | 94 | – |
| Total | 7,810 | 100 | 2,486 | 32 |
May not sum to totals due to rounding
Of the 7,810 participants, 2,486 reported at least one injury or illness requiring medical treatment was sustained during WTC work/volunteer activities. Demographic characteristics of these 2,486 participants are also shown in Table 1. By gender, females were more likely than males to report an injury/illness (37 reports per 100 females compared to 31 per 100 males; χ2 = 17.6, d.f. = 1, P <.0001). A comparison by age shows relative consistency in the rate of reporting at least one injury/illness, with the exception of the lower rate for those aged 55–64 years (25 reports per 100; χ2 = 24.3, d.f. = 5, P = .0002). Minimal variation was found in an industry association comparison (χ2 = 3.2, d.f. = 2, P = .2036), with rates ranging from 31 reports per 100 participants associated with the construction industry to 33 reports per 100 participants associated with law enforcement.
Examining the total number of reported injuries/illnesses on each participant record allowed for further characterization of WTC responder burden. For every 100 participants, 16 reported that one injury/illness requiring medical treatment was sustained during WTC activities, eight reported two injuries/illnesses, four reported three injuries/illnesses, and four reported more than three injuries/illnesses. These rates for all participants were comparable to corresponding rates for both female and male participants. Rate comparability also held across age groups and industry association groups, with one notable exception. The rate for reporting more than three injuries/illnesses was relatively high for participants <25 years of age. For every 100 participants within this group, eight reported more than three injuries/illnesses, twice the corresponding rate for all participants.
A total of 4,768 injuries and illnesses requiring medical treatment were reportedly sustained by participants during WTC work/volunteer activities. Distributions of these injuries/illnesses by nature are shown in Table 2. Respiratory system complaints were the most common, accounting for over a quarter of all injuries/illnesses (n = 1,350, 28%). Of these, 321 (24%) were upper respiratory complaints, which were primarily sinus/nasal congestion and acute infections such as the common cold, and 290 (21%) were chronic obstructive pulmonary conditions, which were primarily reports of asthma. Reports of coughing, shortness of breath, lung ailments due to smoke and/or dust, and other ill-defined respiratory system ailments were captured under “Respiratory system: Other,” which accounted for 739 (55%) of all respiratory system complaints. In addition to respiratory system conditions, the following injury/illness categories each accounted for over 10% of the total: traumatic injuries excluding eye injuries (n = 961, 20%); and eye injuries/ailments (n = 709, 15%).
Table 2.
Distributions by nature of injury or illness (n = 4,768) among studied participants (N = 7,810) in the World Trade Center Worker and Volunteer Medical Screening Program
| Nature of Injury or Illness | Number | Percent* |
|---|---|---|
| Respiratory system | 1,350 | 28 |
| Upper respiratory complaint | 321 | 7 |
| Chronic obstructive pulmonary condition | 290 | 6 |
| Other | 739 | 15 |
| Traumatic injuries, excluding eye injuries | 961 | 20 |
| Cut, laceration, puncture | 183 | 4 |
| Sprain, strain, tear | 140 | 3 |
| Abrasion, blister, contusion | 138 | 3 |
| Soreness, pain, hurt, excluding back injury | 106 | 2 |
| Burn | 69 | 1 |
| Fracture, dislocation | 64 | 1 |
| Other | 261 | 5 |
| Eye | 709 | 15 |
| Ailment, illness | 429 | 9 |
| Traumatic injury | 280 | 6 |
| Chest pain | 375 | 8 |
| Headache | 359 | 8 |
| Skin | 178 | 4 |
| Digestive system | 163 | 3 |
| Psychological stress | 89 | 2 |
| Other ailment, illness, complaint | 559 | 12 |
| Non-classifiable | 25 | 1 |
| Total | 4,768 | 100 |
May not sum to totals due to rounding
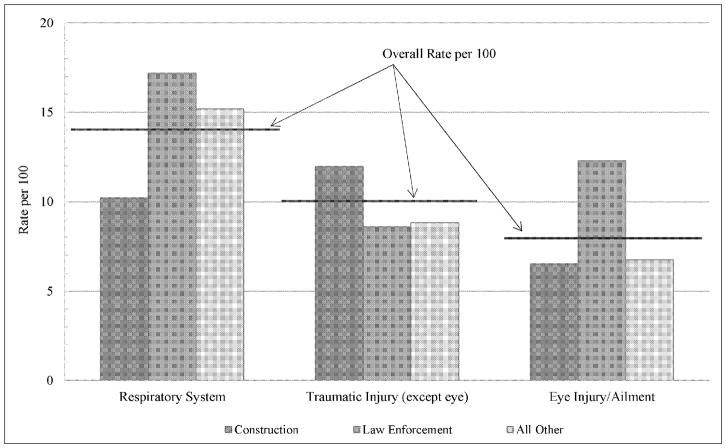
Prevalence rates for these three primary injury/illness categories were further analyzed to identify potential differences by gender, age, and industry association. Overall, for every 100 participants, 14 reported one or more respiratory system conditions; 10 reported one or more traumatic injuries excluding eye injuries; and eight reported one or more eye injuries/ailments. The corresponding rates for male participants were virtually identical to those for all participants. The female rate for a traumatic injury was also comparable; however, females were more likely than males to report a respiratory system condition (18 reports per 100 females; χ2 = 13.6, d.f. = 1, P = .0002), and were slightly less likely to report an eye injury/ailment (6 reports per 100 females; χ2 = 4.1, d.f. = 1, P = .0419). By age group (<35 years, 35–44 years, 45–54 years, and >54 years), the rates for participants in the 35–44 year group were higher than the corresponding rates for all participants and across all other age groups; and the rates for participants in the >54 year group were lower than the corresponding rates for all participants and across all other age groups. Per 100 participants, 15 in the 35–44 year group and 10 in the >54 year group reported a respiratory system condition (χ2 = 18.6, d.f. = 3, P = .0003); 11 in the 35–44 year group and eight in the >54 year group reported a traumatic injury excluding an eye injury (χ2 = 11.4, d.f. = 3, P = .0096); and 10 in the 35–44 year group and five in the >54 year group reported an eye injury/ailment (χ2 = 25.6, d.f. = 3, P <.0001). Rate variation was also pronounced in an industry association comparison. Figure 1 shows the overall rates for the three primary injury/illness categories, as well as the rates for each of the three industry groups. In the respiratory system category (χ2 = 51.7, d.f. = 2, P <.0001), participants associated with law enforcement were more likely to report a condition (17 reports per 100 law enforcement participants), while participants associated with construction were less likely (10 reports per 100 construction participants). For the traumatic injury category excluding eye injury (χ2 = 20.4, d.f. = 2, P <.0001), participants associated with construction were more likely to report a condition (12 reports per 100 construction participants). Within the last category, eye injury/ailment (χ2 = 63.3, d.f. = 2, P <.0001), participants associated with law enforcement were more likely to report a condition (12 reports per 100 law enforcement participants).
Figure 1.
Prevalence rates for respiratory system complaints, traumatic injuries excluding eye injuries, and eye injuries/ailments by industry association for participants in the World Trade Center Worker and Volunteer Medical Screening Program
Further analysis of the 961 traumatic injuries, which exclude those to the eye, showed that most affected the upper extremities (n = 255, 26%), lower extremities (n = 239, 25%), and trunk (n = 171, 18%). The upper extremity body parts affected were primarily hands and fingers (n = 152, 60%) that were reportedly cut, lacerated, or punctured (n = 82, 54% of hand/finger injuries). The lower extremity body parts affected were evenly distributed across the following: knees (n = 71, 30%) that were sprained, strained, or torn (n = 32, 45% of knee injuries); feet and toes (n = 69, 29%) injured by abrasions, blisters, or contusions (n = 27, 39% of foot/toe injuries); and legs excluding knees (n = 63, 26%) that had cuts, lacerations, or punctures (n = 26, 41% of leg injuries). Trunk injuries primarily affected the back (n = 62, 36%), and were reported as pain (n = 39, 63% of back injuries).
Details regarding treatment location were requested for 4,437 injuries/illnesses. Participants reported that 1,617 (36%) of these were treated off-site and 1,295 (29%) were treated on-site, with the remaining injury/illness reports either missing the treatment location information (n = 814, 18%) or indicating other unspecified treatment locations (n = 711, 16%). Females preferentially sought off-site treatment, with 40% of injuries/illnesses treated off-site compared to 22% on-site; whereas males comparably sought treatment off- and on-site (36% of injuries/illnesses treated off-site compared to 31% on-site). A review of treatment location by age revealed patterns similar to those for all participants. More than a third of injuries/illnesses within each age group were treated off-site (35% to 39% range across age groups) and less than a third were treated on-site (24% to 31% range across age groups), with the remaining either missing the location information or indicating other unspecified treatment locations. One notable result was identified in reviewing treatment location by industry association. As opposed to other industry groups, participants associated with the construction industry reported receiving more treatments on-site (33%) than off-site (26%). Variation in treatment location by type of injury/illness was also evident. On-site treatment was predominant for eye injuries/ailments (56%) and traumatic injuries excluding eye injuries (41%). Off-site treatment was prevalent for all other types of injuries/illnesses, with the highest percentages seen for the following: respiratory system (49%), psychological stress (48%), and chest pain (43%).
Discussion
This study, which includes some previously unavailable findings, provides unique insight into the WTC responder population by describing medically treated injuries and illnesses sustained on-site during WTC activities. Rate variations by age are of interest, particularly the lower rates seen for the older age groups. Without additional details on these workers, e.g., information on exposures or worker tasks, it is not clear why this older group of responders would have lower rates.
The treatment location findings, not previously available, are also of interest. Not surprisingly, MSP participants associated with the construction industry, who were likely working in or near the restricted perimeter and had ready access to the on-site medical care stations, more frequently sought on-site treatment. This was not true for participants associated with law enforcement, who more frequently sought off-site treatment. Potential factors contributing to the higher percentage of off-site treatment for these participants include: departmental guidelines, which may have required personnel to seek off-site treatment for work-related injuries/illnesses; the slightly lower rates of traumatic injuries, which were more often treated on-site; and the average rates of latent and chronic illnesses, which were more often treated off-site.
This study and two previous studies, Berríos-Torres et al4 and Perritt et al,5 that focused on injuries and illnesses associated with WTC rescue and recovery activities share many similar findings including demographic characteristics of the population, which were predominately male (86% versus 78% Perritt et al and 89% Berríos-Torres et al), averaged around 40 years old (42 years versus 39 years Perritt et al. and Berríos-Torres et al), and primarily associated with construction (34% versus 41% Berríos-Torres et al) and law enforcement (26% versus 31% Berríos-Torres et al). Additionally, all three studies showed that the two leading complaints for WTC responders were respiratory system ailments (28% versus 22% Perritt et al and 16% Berríos-Torres et al) and traumatic injuries excluding those to the eye (20% versus 29% Perritt et al and 27% Berríos-Torres et al under musculoskeletal with skin blisters and skin burns included).
However, differing from the two previous studies, the two leading complaints in this study were in reverse order, with respiratory system ailments exceeding traumatic injuries. A possible explanation is that MSP participants continue to experience WTC-related respiratory symptoms, as noted in a companion study by Herbert et al,2 which may enable recall of on-site respiratory ailments. Most traumatic injuries experienced during WTC activities have fully healed, especially the less severe, decreasing the potential for recall.
The type of respiratory system condition reported in this study also differed from the two previous studies. Although exact comparisons are complicated by different classification schemes, this study identified a higher percentage of chronic obstructive pulmonary conditions, predominately asthma, which was not mentioned in the previous findings. Possible explanations relate to questionnaire design and data administration for this study. Respiratory system conditions were the most challenging to classify and code. Frequently, the injury/illness category selected by the MSP participant did not correspond with narrative text. It may be that participants had difficulty matching their respiratory condition with one of the three pre-specified respiratory-related injury/illness categories, namely “asthma,” “congestion,” and “lung (smoke/dust).” If a match was not evident, e.g., the participant experienced shortness of breath, the most convenient choice was likely selected. Because “asthma” appeared at the top of the alphabetized categories and could have been considered a reasonable choice for breathing troubles, participants may have disproportionally selected “asthma” for conditions that were not clinically asthma. Regardless of the complications involved in analyzing respiratory conditions, this study is consistent with the previous two studies and several others in identifying respiratory system ailments as a leading condition that affected WTC responders on-site.4–6,9–11
Also consistent with numerous previous studies, eye injuries/ailments were among the leading conditions affecting responders working/volunteering on-site.4–6,11 Although direct comparisons across the various studies are complicated by different classification schemes and reference periods, the percentages ranged from 14% of WTC rescue and recovery workers and volunteers reporting incident and persistent eye irritation11 to 8% of MSP participants in this study retrospectively reporting eye injuries/ailments resulting from on-site WTC activities.
It is also intriguing, from a methodological perspective, that the results at the highest level within the injury/illness categories are quite comparable between this retrospective study and two studies where data were collected in real-time, Berríos-Torres et al4 and Perritt et al.5 Retrospective self-reports are highly susceptible to recall bias, making the results more prone to underestimation.12 Further research is needed to determine whether the comparability is simply an anomaly associated with the WTC tragedy, for which the magnitude, intensity, and response was unprecedented, or if it carries over to research conducted for other disaster response efforts.
As would be expected, demographic characteristics of the population in this study are very comparable to those from previous MSP studies, Herbert et al2 and Stellman et al.3 The majority of participants were male (86% versus 87% Herbert et al and Stellman et al), around 42 years old (average of 42 years versus median of 42 years Herbert et al), and associated with construction (34% versus 34% Herbert et al) and law enforcement (26% versus 29% Herbert et al). Furthermore, the respiratory illness findings in this study corroborated the results of the MSP study by Herbert et al,2 both indicating that respiratory issues were the primary concern for WTC responders.
Limitations
Study results are subject to at least three limitations. First, respondent recall bias was a concern. MSP participants were asked to report incidents that occurred up to 31 months prior, which is a lengthy time interval that is considered a major determinate for recall. Conservative estimates are likely for injuries and illnesses that generally are considered less severe and were less publicized in WTC-response reports, and overestimates are likely for injuries and illnesses that were highly publicized. Second, data quality was a major concern since these data were collected via a self-administered questionnaire, were collected separately from the medical examination data, and were not validated or reviewed during the data collection period. Inconsistencies within a participant report were common, and data quality generally deteriorated with each additional injury/illness reported by a participant, with the third and fourth injuries/illnesses having the most inconsistencies and fewest narrative details. Furthermore, it was not possible to distinguish if a reported injury/illness was a condition strictly from the past or a condition currently being experienced. As an aside, many federal agencies have recommended developing standardized, worker safety and health data collection tools to address data quality issues and provide the means for systematic analyses of worker burden for future disaster response efforts. The third limitation is that the results cannot be extended to the entire WTC responder population, and caution must be used in comparing prevalence rates across industry association groups. Statistical sampling methods were not used in selecting MSP participants, FDNY rescue workers are not MSP participants, and reliable statistics on size and composition of the WTC responder population are not available, all of which compromise the ability to generalize results and accurately compare rates.
Conclusion
In developing conclusions for this study, two areas of consideration emerged. First, this study underscores the need to implement key recommendations provided in emergency preparedness guidelines13–14 including planning for rapid deployment of (1) appropriate personal protective equipment for responders and (2) medical care stations mobilized appropriately near responder worksite(s). The second area relates to conclusions regarding the methods used for this study. To better understand the burden of a particular disaster or to prepare for future disasters, a screening program such as the MSP may be effective in retrospectively providing insight on the responder population demographics and general information on responder work-related injuries and illnesses.
Abbreviations
- DMAT
Disaster Medical Assistance Team
- FDNY
Fire Department of New York City
- HIPAA
Health Insurance Portability and Accountability Act
- MSP
Medical Screening Program
- NIOSH
National Institute for Occupational Safety and Health
- OIICS
Occupational Injury and Illness Classification System
- WTC
World Trade Center
Footnotes
This program has continued and is currently known as the World Trade Center Medical Monitoring and Treatment Program.
USNS Comfort is a hospital ship operated by the US Navy.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
References
- 1.New York City Fire Department: Bureau of Health Services (BHS) World Trade Center (WTC) [Accessed October 14, 2011];Medical Monitoring and Treatment Program. www.nyc.gov/html/fdny/html/units/bhs/wtcmm.
- 2.Herbert R, Moline J, Skloot G, et al. The World Trade Center disaster and the health of workers: five-year assessment of a unique medical screening program. Environ Health Perspect. 2006;114:1853–1858. doi: 10.1289/ehp.9592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stellman JM, Smith RP, Katz CL, et al. Enduring mental health morbidity and social function impairment in World Trade Center rescue, recovery, and cleanup workers: the psychological dimension of an environmental health disaster. Environ Health Perspect. 2008;116:1248–1253. doi: 10.1289/ehp.11164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berríos-Torres SI, Greenko JA, Phillips M, et al. World Trade Center rescue worker injury and illness surveillance, New York, 2001. Am J Prev Med. 2003;25:79–87. doi: 10.1016/s0749-3797(03)00110-7. [DOI] [PubMed] [Google Scholar]
- 5.Perritt KR, Boal WL The Helix Group Inc. Injuries and illnesses treated at the World Trade Center, 14 September-20 November 2001. Prehosp Disaster Med. 2005;20:177–183. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Injuries and illnesses among New York City Fire Department rescue workers after responding to the World Trade Center attacks. MMWR. 2002;51(Special Issue):1–5. [PubMed] [Google Scholar]
- 7.Bureau of Labor Statistics. [Accessed October 14, 2011];Occupational Injury and Illness Classification Manual. 2007 Sep; www.bls.gov/iif/oshoiics.htm.
- 8.SAS. SAS Version 9.2. Cary, NC: SAS Institute Inc; 2007. [Google Scholar]
- 9.Levin S, Herbert R, Skloot G, et al. Health effects of World Trade Center site workers. Am J Ind Med. 2002;42:545–547. doi: 10.1002/ajim.10154. [DOI] [PubMed] [Google Scholar]
- 10.Spadafora R. Firefighter safety and health issues at the World Trade Center site. Am J Ind Med. 2002;42:532–538. doi: 10.1002/ajim.10153. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. MMWR; Physical health status of World Trade Center rescue and recovery workers and volunteers; New York City. July 2002–August 2004; 2004. pp. 807–812. [PubMed] [Google Scholar]
- 12.Andersen LP, Mikkelsen KL. Recall of occupational injuries: a comparison of questionnaire and diary data. Saf Sci. 2008;46:255–260. [Google Scholar]
- 13.Jackson BA, Peterson DJ, Bartis JT, et al. Protecting Emergency Responders: Lessons Learned from Terrorist Attacks. Santa Monica, CA: RAND Science and Technology Policy Institute; 2002. [Google Scholar]
- 14.Jackson BA, Baker JC, Ridgely MS, et al. Protecting Emergency Responders, Volume 3: Safety Management in Disaster and Terrorism Response. Cincinnati, OH: US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2004. [Google Scholar]