Abstract
Cardiovascular disease deaths are increasing in low- and middle-income countries and are exacerbated by health care systems that are ill-equipped to manage chronic diseases. Global health partnerships, which have stemmed the tide of infectious diseases in low- and middle-income countries, can be similarly applied to address cardiovascular diseases. In this review, we present the experiences of an academic partnership between North American and Kenyan medical centers to improve cardiovascular health in a national public referral hospital. We highlight our stepwise approach to developing sustainable cardiovascular services using the health system strengthening World Health Organization Framework for Action. The building blocks of this framework (leadership and governance, health workforce, health service delivery, health financing, access to essential medicines, and health information system) guided our comprehensive and sustainable approach to delivering subspecialty care in a resource limited setting. Our experiences may guide the development of similar collaborations in other settings.
Keywords: cardiovascular disease, global health partnership, limited resources, sub-Saharan Africa
“If you want to walk fast, walk alone. If you want to walk far, walk together.”
-African Proverb
Although cardiovascular disease (CVD) remains the leading cause of death worldwide (1), significant gains in treatment have been made over the last 4 decades. Since the 1970s, the rate of death from CVD has declined most dramatically in high-income countries (2). Half of the decline has been attributed to the rapid dissemination of coronary care units and radical reorganization of cardiac care, centralizing acute CVD patients in 1 location in the hospital (3). Nevertheless, gains in CVD health have not been realized equitably around the globe. The Global Burden of Disease Study estimated that 80% of deaths from noncommunicable diseases, including CVD, now occur in low- and middle-income countries (1). Between 1990 and 2013, there was an 81% increase in the number of CVD deaths in sub-Saharan Africa; significantly, 70% to 80% of these deaths could have been averted with the availability of critical or specialty care (4). The epidemiological transition of CVD burden in low- and middle-income countries has garnered international attention, emboldening the World Health Organization’s “25 × 25” goal of a 25% reduction in mortality from noncommunicable diseases by 2025 (5).
Despite these recent positive trends, historically, most global health funding has not been applied to the treatment of acute or chronic CVD, but rather, to infectious disease care (6,7). Noncommunicable diseases account for 9 times the number of deaths worldwide, but receive 300 times less funding than human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) (8). In sub-Saharan Africa, the percent of total spending on HIV now exceeds the percent burden of HIV-related deaths and disability (9). In Kenya, cardiovascular and circulatory diseases constitute 8.2% of all deaths (1) and cause the highest inpatient case fatality rate (10). Cerebrovascular disease (3.9% of all deaths), ischemic heart disease (2.4%), cardiomyopathies (0.5%), hypertensive heart disease (0.5%), and rheumatic heart disease (0.3%) were the most common causes of cardiovascular and circulatory disease deaths in Kenya in 2010 (1). Nonetheless, HIV/AIDS accounts for >60% of the total health spending costs (11). As a result, only 27% of public health centers in Kenya are equipped with the necessary supplies to treat CVD, access to cardiologists is limited, and absenteeism of all levels of providers is commonplace (12).
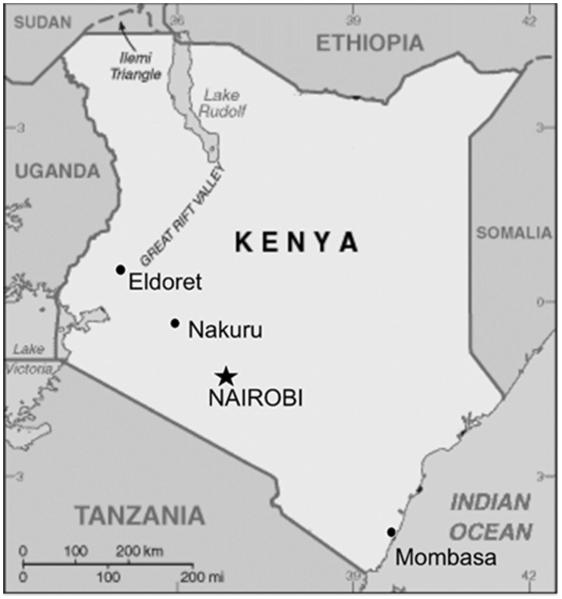
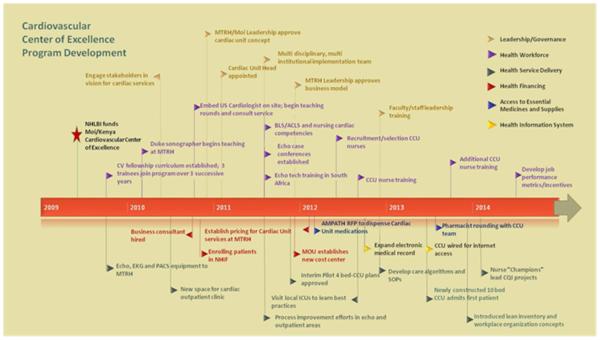
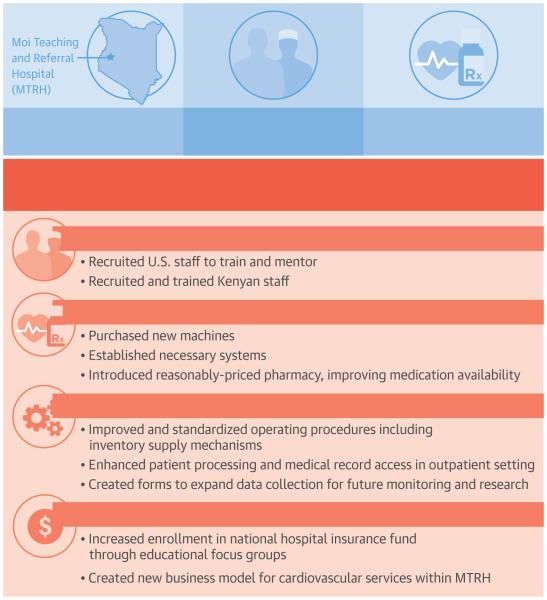
Given these observations and an opportune research investment from the National Heart, Lung and Blood Institute (NHLBI), we leveraged a long-standing multi-institutional collaboration with Moi University and Moi Teaching and Referral Hospital (MTRH) in Eldoret, Kenya (Figure 1) to ambitiously tackle the shortage of specialists and infrastructure necessary to address the rising burden of CVD. On the basis of a collective interest among academic partners and MTRH in focusing on CVD care, and using the World Health Organization’s Health Systems Strengthening Framework for Action (13), we highlight our innovative partnership and the developmental milestones that created the foundation for a sustainable model for improved CVD care in the public sector (Figure 2).
Figure 1. Map of Kenya Showing Cities with Cardiology Expertise.
In 2009, most cardiologists in Kenya were located in and around the capitol (Nairobi) or on the coast in Mombasa. There were no adult cardiologists in Eldoret, the 5th largest city, serving 25 million people.
Figure 2. Critical Milestones in Development of the Cardiovascular Center of Excellence and the Cardiac Unit.
ACLS = advanced cardiac life support; BLS = basic life support; CCU = cardiac intensive care unit; CQI = continuous quality improvement; Duke = Duke University; ECG = electrocardiogram; echo = echocardiography; ICU = intensive care unit; Moi = Moi University; MOU = memorandum of understanding; MTRH = Moi Teaching and Referral Hospital; NHIF = National Hospital Insurance Fund; NHLBI = National Heart Lung and Blood Institute; PACS = picture archiving and communication system; RFP = revolving fund pharmacy; SOP = standard operating procedures
PROLOGUE: CARDIOVASCULAR CARE SERVICES IN WESTERN KENYA, CIRCA 2008
MTRH is the second major public referral teaching hospital in Kenya, serving approximately 25 million people. The hospital has an 800-bed inpatient capacity, a busy casualty/emergency department, medical, surgical, pediatric, maternal, and outpatient clinic facilities providing care to more than 600,000 patients annually. MTRH’s stated mission is to provide quality health care services and teaching facilities through research, training, capacity building, innovation, and participation in national health planning. Yet, in 2008, CVD patients had limited options; MTRH had only a 6-bed medical-surgical intensive care unit, and no adult cardiologists. A pediatric cardiologist ran a half-day pediatric cardiology clinic, whereas general internists staffed the adult cardiac clinic. Diagnostic equipment included 1 electrocardiogram machine, a treadmill, and an echocardiogram machine (HP Sonos 2500)—all nearing the end of life. There were no monitored beds or defibrillators outside the intensive care unit and operating rooms. There were no trained cardiac nurses and no formal training for echocardiography technicians. Even routine diagnostic tools, such as portable chest x-ray and ultrasound machines, were often unavailable, and stock-outs of medications and laboratory reagents were frequent.
THE SPARK: ACADEMIC MODEL PROVIDING ACCESS TO HEALTHCARE CONSORTIUM AND THE NHLBI’S GLOBAL HEALTH INITIATIVE
In hopes of responding to the burden of CVD, the NHLBI and the UnitedHealth Group launched the Collaborating Centers of Excellence (COE) program in 2009 to establish cardiovascular and pulmonary disease clinical research centers in low- and middle-income countries in partnership with institutions in high-income countries (14,15). Moi University School of Medicine and Duke University were funded to create 1 of the 11 NHLBI COEs (16) in Kenya. The Kenya COE was built upon a robust 22-year collaboration of academic medical centers, called the Academic Model Providing Access to Healthcare (AMPATH) Consortium (17). Each academic partner in the Consortium commits to “Lead with Care” in their area of expertise, enhancing local care through educational exchange, infrastructure development, and research collaborations. Although the backbone of AMPATH’s funding has historically come from the President’s Emergency Program for AIDS Relief (PEPFAR), funding has included other grants, philanthropy, and academic partner investment. Bidirectional institutional benefit has been significant, as impactful cutting-edge global health programs have attracted high-quality trainees and faculty. Over the years, AMPATH has expanded its focus beyond HIV to include maternal and child health, primary care, and chronic diseases. Unfortunately, despite the fact that CVD is the second leading cause of death among adults in most African countries, funding for CVD remains meager relative to HIV (18).
WARMING UP: ENSURING A SHARED VISION
Unlike other NHLBI-funded COEs, the Kenya COE did not have cardiovascular subspecialists to provide care in our catchment area. Provider incentives in the public sector were low, leaving most advanced CVD patients with limited options. Thus, while building CVD research capacity, Duke University’s Hubert Yeargan Center for Global Health committed to developing a general clinical cardiology fellowship training program and enhancing infrastructure for cardiovascular services. In addition to grant-supported activities, this undertaking required salary and travel support for U.S. cardiologists, an echocardiography technician, a nurse educator, a business consultant and a unit administrator in Kenya, and a stateside program director. Several philanthropic donors were willing to provide Duke with startup funds (>$250,000) for this major undertaking, with the understanding that future operational costs would be sustained by MTRH and the Kenyan Ministry of Health. The director of MTRH, as well as the principal of Moi University College of Health Sciences, enthusiastically embraced this concept, officially announcing the creation of a cardiovascular unit that was to cut across internal medicine, surgery, and anesthesiology.
THE ROAD MAP: A MODEL FOR DEVELOPMENT OF CARDIOVASCULAR CARE
In order to strengthen MTRH’s cardiac services and to invest our resources into something of lasting value, we adopted the World Health Organization Framework for Action (13) as a roadmap for development. The building blocks of the Framework include: leadership and governance; health workforce; health service delivery; health financing; access to essential medicines and supplies; and health information system. These building blocks describe essential and interdependent functions necessary for the optimal performance of a health system; therefore, they guided us in setting appropriate substantive and comprehensive milestones needed to develop sustainable capacity for high-quality cardiovascular services (Figure 2).
LEADERSHIP AND GOVERNANCE
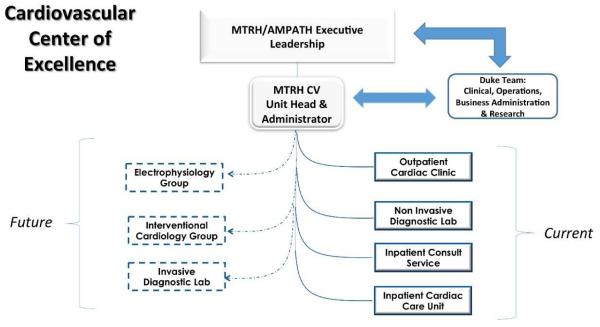
Our vision for the Kenya COE had its foundation in AMPATH’s model of “leading with care,” which promotes a strong health service delivery backbone that enables an even more robust training and research agenda (19). AMPATH’s long-standing model of twinning Kenyan and North American partners promoted a bilateral commitment of time, personnel, and financial resources as the basis for collaboration. An early priority included forming a multinational multidisciplinary implementation team made up of Kenyan and American colleagues to engage stakeholders in vision setting, with an emphasis on establishing a governance structure, accountability, and transparency at the individual and organizational levels. We hired a Masters of Business Administration (MBA) graduate as a business consultant to assist with developing a “semiautonomous” organizational structure (Figure 3) and a financial cost center for MTRH’s cardiac services, charting a new course for how subspecialty services could become sustainable in the long term. The consultant provided leadership training for key clinical and administrative staff while crafting a Memorandum of Understanding between Duke University and MTRH; this agreement formalized plans for developing a leadership team composed of operations and clinical staff. This team would be responsible for: continuous improvement in clinical services; financial plans for managing revenue, expenses, and operating budgets; clinical guidelines for implementing consistent standards and staff performance expectations; and forecasting plans for capital equipment and long-term planning needs.
Figure 3. MTRH Cardiac Unit Organizational Structure as Outlined in a Memorandum of Understanding between Duke and Moi Universities.
MTRH and AMPATH Leadership administer the MTRH Cardiac Unit, with Duke as lead collaborator and adviser. The Cardiac Unit includes a pediatric and adult outpatient clinic, noninvasive cardiac diagnostic unit, inpatient consult service, and cardiac care unit. Expansion goals include electrophysiology, interventional, and invasive diagnostic services. AMPATH = Academic Model Providing Access to Healthcare; CV = cardiovascular; MTRH = Moi Teaching and Referral Hospital
HEALTH WORKFORCE
Training the cardiac workforce began with a focus on the outpatient and diagnostic settings, while developing the more robust capacity required for a specialized cardiac inpatient unit (Figure 2). We conducted most training in Kenya because we believed that in addition to reducing costs, on-site training would foster staff retention. We produced a clinical curriculum in general cardiology for the physician workforce and hired a senior U.S. cardiologist willing to spend the majority of each year in Kenya as Clinical Lead. Assisted by a Duke Cardiology fellow (who later joined the Duke faculty) and a junior faculty member from Icahn School of Medicine at Mount Sinai, the outpatient clinic became a robust teaching and consulting service for cardiology fellows. The clinical service evolved to include daily morning report, weekly grand rounds, and a 24/7 on-call schedule. Three Kenyan cardiology fellows were recruited over 3 successive years, joined by medical officers (similar to U.S. intern graduates) and registrars (similar to U.S. residents).
Skill development and upgrading equipment for the cardiovascular diagnostic unit (CDU) were emphasized as early priorities. Despite the fact that the CDU was busy, performing approximately 3,900 echocardiograms per year in 2009 (20), CDU technicians lacked formal training. Furthermore, there was no technology available to digitally acquire images for review and interpretation offline. With assistance from the medical device industry, we acquired new portable echocardiography machines, a picture archiving and communication system, and established weekly echocardiography didactic sessions. Duke sent a sonographer to Eldoret for several months a year to provide training for the diagnostic staff, which was further supplemented by experiences in Cape Town, South Africa. One technician underwent additional echocardiography training at Duke and passed the Cardiovascular Credentialing International examination.
Nursing instruction initially included basic and advanced cardiac life support and basic cardiac competencies for staff in the outpatient and inpatient settings. However, with the construction of a cardiac care unit (CCU), focus shifted to building the unit’s workforce. MTRH and Duke jointly designed job descriptions, recruited, interviewed, and trained staff in a 6-week course taught primarily by our cardiology fellows. Training was supplemented by rotations in other MTRH specialty units and in-service instruction by equipment vendors. Most nursing staff rotate regularly throughout the hospital; however, MTRH committed to permanently assigning trained staff to the unit. Two MTRH nurse educators were sent to Duke for supplemental training and a Duke cardiac nurse made visits to MTRH to continue training. All of the trained fellows, echocardiography technicians, and CCU nurses remain on staff at MTRH. Of 3 medical officers, 1 was matched at Duke for an internal medicine residency, and another was accepted into registrar training at Nairobi University.
HEALTH SERVICE DELIVERY
Hiring a business consultant early in the process allowed us to critically evaluate health service delivery in tandem with developing the workforce. We conducted extensive evaluations of patient flow and medical record access, which ultimately led to reductions in wait time. We made several visits to local mission, private, and public hospitals to glean insight into the best critical care practices for the region, remaining mindful of financial viability and areas for potential collaboration. Prior to constructing the permanent 10-bed CCU, we piloted a 4-bed unit in a space renovated by Moi University, as proof-of-concept for financial and operational management. Nurses, pharmacists, and physicians jointly developed standard operating procedures, clinical care algorithms, patient flow sheets, and order sets. Nursing “champions” were identified to lead continuous quality improvement efforts and an administrator was identified to assist with operational process enhancements, budgeting, financial forecasting, and procurement. A regular stock control system was established and training was conducted to organize the workplace. MBA graduates were brought in to assist with short-term quality projects. Checklists and alert cards were established to flag problems in the system.
HEALTH FINANCING
The business model underpinning the COE sustainability plan evolved from several key strategic decisions. First, unlike private facilities that can turn patients away if they lack the ability to pay, MTRH allows admission to the CCU, regardless of financial circumstances. We anticipated attracting a diverse payer mix that could subsidize indigent care because MTRH’s CCU would be the only specialized cardiac unit in western Kenya. Secondly, a concerted effort was made to enroll all clinic patients in Kenya’s National Hospital Insurance Fund (NHIF) to cover future hospitalization costs. NHIF is the primary hospital insurance provider in Kenya. Although enrollment in NHIF is compulsory for salaried employees through graduated payroll deductions, 83% of the Kenyan workforce is made up of “informal” (not on tax payrolls) laborers (21), who comprise the majority of patients seen at MTRH. Therefore, we worked with social workers to run weekly NHIF education talks at outpatient clinics so that registration could be made on site. For a fee of 160 KES/month (~$2/month), NHIF covers the enrollee, spouse, and an unlimited number of children. Beneficiaries receive comprehensive hospital coverage with no overall limit on the amount of benefits received (22). Thirdly, a separate cost center, managed by MTRH’s Cardiac Unit Head, was established from CDU cash revenue, to build an “operating reserve” that could be more responsive to supply chain issues for cardiac medicines and supplies. Revenue and expenses from all other cardiac inpatient and outpatient services flow through the hospital’s main accounting structure.
During the planning phase, the implementation team and MTRH’s financial administration set a budget and pricing for cardiac services. The Hock Family Foundation provided $250,000 for construction of the permanent 10-bed CCU and initial capital investment costs for cardiac monitors, supplies, and essential cardiac medications; MTRH purchased beds.
Our preliminary data suggest that subspecialty cardiac services are sustainable in the public sector. In its 22 months of operation, fewer than 5% of patients admitted to the CCU had their fees waived, 35% were insured (primarily through the NHIF), and 60% paid out-of-pocket. Total monthly revenue (approximately USD $14,843) exceeds monthly expenses (approximately USD $10,939). These data include all operating expenses and service and maintenance agreements, but do not include salaries (paid for through the Kenyan Ministry of Health) or new capital equipment purchases covered by the central administration. As a government hospital, general operating expenses (less salaries) are managed through hospital operations. Nonetheless, these preliminary data suggest that long-term sustainability is possible.
ACCESS TO ESSENTIAL MEDICINES AND SUPPLIES
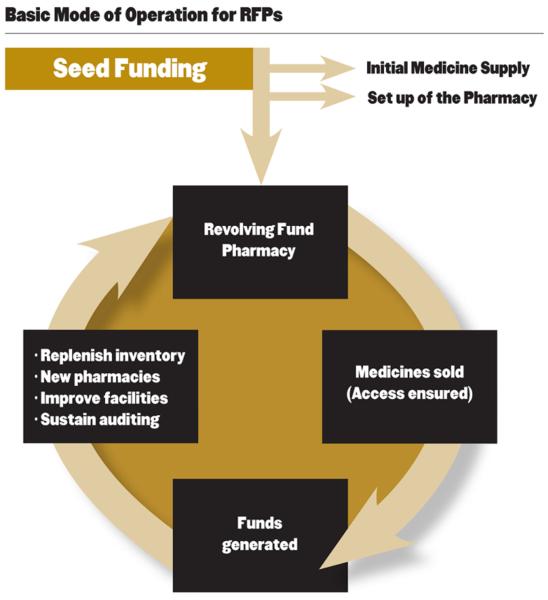
One of the challenges in our early efforts was ensuring that patients would have uninterrupted access to critical medications. National Kenyan evaluations of health care system performance have found that some basic essential medications are only available 66% of the time, with drastic variations in availability between facilities (23). To combat this, AMPATH partners from MTRH and the Purdue University College of Pharmacy introduced revolving fund pharmacies (RFP) (Figure 4) (24,25), which are intended to be a second-line option when a medication is out of stock at the government pharmacy. Situated at the MTRH campus, 25 rural satellite dispensaries, and 2 subdistrict hospitals, these RFPs charge slightly more than government pharmacies; profits from this markup charge (5% to 10%) are used to restock the pharmacy. Although the RFP’s partner with the Ministry of Health in the inpatient and outpatient setting, they operate semi-independently to avoid many of the limitations of governmental procurement policies. The RFP provides patients with uninterrupted access to reasonably priced medications and ensures that the Cardiac Unit can accommodate an expanding patient volume, without incurring losses. With the many challenges associated with supply chain management in low- and middle-income countries (e.g., inflexibility of the government supply chain, rigid tendering system, among others), the RFP has been a crucial solution to enhance quality of care. The key aspects of the RFP are affordable prices, flexibility of the formulary, more stringent inventory management, and selecting suppliers that perform industry-standard quality checks prior to delivery. This backup RFP supply chain system has helped to improve medication availability from ~60% to >94%. Through the RFP, we have been able to provide previously unavailable cardiovascular medications, such as diltiazem, norepinephrine, nitroprusside, dobutamine, dopamine, amiodarone, and nitroglycerin. The Purdue University College of Pharmacy also provides clinical training for an MTRH full-time clinical pharmacist who rounds in the CCU daily, in addition to developing infrastructure for and high-quality inpatient and outpatient anticoagulation monitoring (26).
Figure 4. RFP Concept.
After the provision of seed funding, patient revenue is reinvested in the RFP to replenish medications and to expand the formulary, ensuring a continuous supply of vital medications. RFP = revolving fund pharmacy.
HEALTH INFORMATION SYSTEM
One of AMPATH’s most compelling successes in the outpatient HIV care program has been its open-access electronic medical record system and unique patient identification numbers (27). Leveraging this resource, we developed CVD-focused outpatient encounter forms to expand the dataset, as a rich repository for future monitoring, evaluation, and research. Eventually, we hope to translate that technology to MTRH. During CCU construction, we prospectively wired the new building with internet capabilities; however, funding for broader installation throughout the hospital and the ongoing high cost of internet access remain significant deterrents to maximizing its potential.
EXPERIENCE TO DATE
CLINICAL
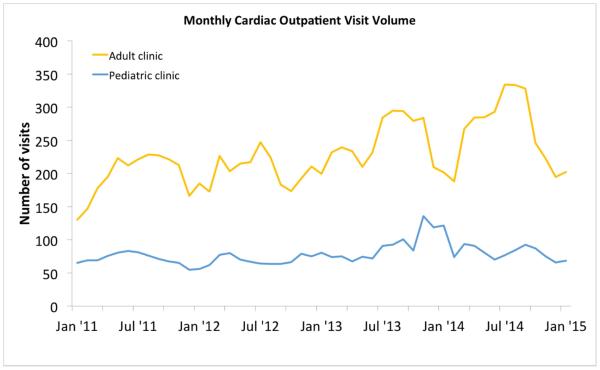
In the first year of operation, the CCU admitted 180 patients. This number increased to 276 in year 2. Readmissions accounted for 14% of all admissions. Occupancy rates have varied seasonally, averaging 61%. Most CCU patients (87%) were adults ≥18 years of age. Females slightly outnumbered males (54% vs. 46%). The average age of adult patients was 59 years and the average length of stay was 6.0 days. The most common primary admitting diagnoses were: heart failure (206 of 456 admissions, 20%); rheumatic heart disease complications (14%); hypertensive urgency/emergency (9%); cardiogenic shock (5%); and acute coronary syndromes (5%) (Table 1). Most patients were discharged to another inpatient ward (42%) while 28% were discharged directly home. Mortality in the CCU was 30%, driven largely by late presentation of disease, dearth of local and national surgical options, and financial constraints of patients presenting in the public hospital. Inpatient cardiovascular mortality rates prior to opening the CCU are unknown. The cardiac clinic, which is staffed by 4 to 5 clinicians and supervisors, has grown consistently in volume since 2011, and now averages 80 patients per weekly session (Figure 5). Compared with 2009, echocardiogram volume has grown by 149%. Most echocardiograms are now acquired digitally using state-of-the-art equipment (i.e., Philips CX50, GE Vividq) for review, analysis, and teaching offline.
Table 1.
MTRH CCU Patient Characteristics
| Time Period | ||
|---|---|---|
| Characteristics | Year 1 (February 2013– January 2014) |
Year 2 (February 2014– January 2015) |
| Total number of admissions | 180 | 276 |
| Number of unique patients admitted | 162 | 238 |
| Adult patients, n (%) | 154 (86%) | 243 (88%) |
| Pediatric patients, n (%) | 26 (14%) | 33 (12%) |
| Female, n (%) | 97 (54%) | 150 (54%) |
| Average age of adult patients, yrs | 66.8 | 42 |
| Average age of pediatric patients, yrs | 11.2 | 12.6 |
| Average length of stay, days | 5.9 | 6.0 |
| Disposition | ||
| Discharge to another inpatient ward | 95 (53%) | 95 (34%) |
| Discharge to home | 25 (14%) | 103 (37%) |
| Deceased | 60 (33%) | 78 (28%) |
| Most common admission diagnoses of 456 admissions, n (%) |
||
| Heart failure | 206 (20%) | |
| Rheumatic heart disease complications | 63 (14%) | |
| Hypertensive diseases | 42 (9%) | |
| Cardiogenic shock | 22 (5%) | |
| Acute coronary syndromes | 21 (5%) | |
CCU = cardiac care unit; MTRH = Moi Teaching and Referral Hospital
Figure 5. Trends in Cardiac Outpatient Clinic Volume.
Three-month running average for the adult and pediatric cardiac outpatient clinics from January 2011 to January 2015. Clinic volumes decreased seasonally in December and January.
RESEARCH
During clinical training, COE cardiology fellows engaged in research training and conducted projects supported by the NHLBI. These projects addressed locally relevant cardiovascular issues, including hypertension in rural populations (28), peripheral arterial disease among diabetics, and task shifting the use of hand-held cardiac ultrasound (29). Moreover, a number of Kenyan and North American trainees and faculty received numerous awards from Fogarty International Center of the National Institutes of Health, the Fulbright Program, and the Doris Duke Foundation to work with the COE, resulting in >30 scientific presentations and manuscripts (30–34). Sixteen trainees have completed a 6-month individually mentored online course in clinical research methodology offered by Duke, and 1 trainee completed the Fogarty International Center’s distance-based international research coordinator training. In addition to the impact on cardiovascular health care delivery in Eldoret, the development of the Cardiac Unit has also been of value to U.S.-based institutions, with regard to their research and educational missions.
LESSONS LEARNED: CHALLENGES, OPPORTUNITIES, AND FUTURE DIRECTIONS
Ambitious endeavors, like the introduction of subspecialty cardiac services to the Kenyan public sector, are simultaneously fraught with challenges and opportunities. The early years marked tireless efforts to train clinical faculty and staff while establishing an administrative framework and business model. There has undoubtedly been significant progress, but many challenges remain.
PARTNERSHIPS
Relationships are key. Duke joined the AMPATH Consortium in 2005, yet as a relatively new member, building trust over time was critical to bridge cross-cultural expectations and minimize miscommunication. While e-mail and conference calls were a supplemental means of communication, they were not substitutes for face-to-face meetings. Charting a shared vision and engaging stakeholders of Duke, Moi, and MTRH at all levels (not just at the senior leadership level) was essential to introduce change, particularly because institutional politics and competing priorities for limited resources were significant challenges to innovation. Although it was important to be adaptive, it was equally important to delay progress or change course when something was not working well.
WORKFORCE DEVELOPMENT
Developing a subspecialty workforce from scratch meant expanding beyond training physicians, to training paraprofessionals and administrative support personnel. In resource-constrained environments, there is constant tension between taking time to teach versus providing care; assigning registrars and medical officers to the service was essential to create a “deeper bench” to manage growing patient volumes. Trainees must have dedicated time for instruction. Unlike the U.S. system, where residents and fellows receive salary support, trainees are uncompensated and expected to pay fees. As a result, private practice (or moonlighting) is common, even during normal business operations, detracting from rigorous clinical instruction. Developing mechanisms to compensate clinicians during subspecialty training is essential to create a top-notch training program.
Even with a strict time commitment, training is only the first step. Mentors and educators need to work side by side with trainees over extended periods of time to adapt desired behavior, implement procedural changes, and ensure accountability. In light of the statistics on absenteeism referred to earlier (12), an absolute prerequisite for delivering quality care for all level of providers is closer oversight of approved time off by management to ensure adequate patient coverage. Furthermore, leadership development is equally critical to clinical training because without solid leadership, technical capacity-building efforts have limited impact.
Perhaps the most important lesson learned is that a subspecialty fellowship training program is feasible in low- and middle-income countries. This program has yielded the first Kenyan cardiologists recognized by the Kenyan Medical Practitioners and Dentists Board who were trained almost exclusively in Kenya (COA, FAB).
BUSINESS AND OPERATIONAL MODEL
Investing resources to create a viable business and operational model is an essential component of health system strengthening. We have demonstrated that subspecialty services have the potential to be financially viable in the public sector, particularly with a separate cost center generating a more consistent and reliable funding stream; nevertheless, this model has yet to be fully actualized. Recent modifications to our model may produce better results in the future, but only time will tell. As a result, equipment is still lacking, which jeopardizes the quality of care, workforce development and retention, and patient outcomes. The development of accredited training programs has the potential to bolster the cardiac services business model as an income-generating mechanism.
POLICY IMPLICATIONS
There is still significant misalignment between financial remuneration and budgetary allocation of resources for subspecialty care in Kenya. Local efforts to address the critical shortage of subspecialty providers and infrastructure will have limited value without greater resources from the Kenyan Ministry of Health and Education and increased allocation of Kenya’s gross domestic product to health care budgets (35). Referral hospitals are major teaching centers that can help to retain physician experts who may seek employment elsewhere if the tools to practice their craft are absent. Interim tax relief for donated medical equipment and supplies could help to address acute shortages. While the NHIF will eventually transform into a more comprehensive universal health insurance plan, challenges remain, with delayed reimbursements to hospitals and reassessment of rates for specialized services. Information technology innovation and greater efficiencies in the procurement and tendering processes for supplies and medications remain vastly untapped opportunities to exponentially improve care.
FUTURE DIRECTIONS
Despite the many accomplishments of the past 5 years, much work remains. Our collaboration is committed to supporting ongoing efforts, yet new sources of funding will need to be identified and greater responsibility for expansion of services and educational programing will have to be undertaken by Moi University and MTRH. Workforce development will continue to be a high priority for all types of providers. The Cardiology Fellowship curriculum is being submitted for formal adoption by Moi University; if successfully inaugurated, this program will be the first cardiology fellowship training program in Kenya. Embedding a full-time nurse educator in the CCU remains a high priority, as well as credentialing all echocardiography staff. Significant internal and external pressures exist to develop interventional capabilities to care for the huge population suffering sequelae of rheumatic and congenital heart disease. Nonetheless, establishing adequate training and infrastructure prior to advancing to later stages of development will be crucial to ensure good patient outcomes. Fully outfitting the cardiac unit with equipment, while building the technical capacity of MTRH’s ancillary services (i.e., laboratory, radiology, among others), will be equally important to patient outcomes.
CONCLUSIONS
The MTRH Cardiac Unit is still a case study in progress. By adapting the World Health Organization Framework for Action, we have demonstrated how a multinational public and private partnership can deliver robust cardiac services in a low- and middle-income country. Successes in clinical training, infrastructure development, leadership training, and business model development have yielded important, clinically relevant results, and plans for expansion are in place. We believe that our approach to developing this program can potentially be implemented in other resource-limited settings.
Central Illustration. Developing Sustainable Cardiovascular Services at Public Hospitals in Kenya.
Acknowledgments
The authors acknowledge the important contributions from people from Academic Model Providing Access to Healthcare leadership; Moi University School of Medicine; Moi Teaching and Referral Hospital (nursing leadership, Cardiac Care Unit nurses, Cardiovascular Diagnostic Unit, medical records, pharmacy, engineers, critical care educators, human resources); Purdue University College of Pharmacy; Duke Hubert Yeargan Center for Global Health, volunteer faculty mentors: Jim Bengston, Moe Bishara, John Burks, Jonathan Ward, and William E. Wilkinson; Duke Global Health Institute; Duke University Cooperative Cardiovascular Society; Duke Cardiac Care Unit Nurse Clinicians and Managers; Duke University Medical Center and Philips and GE Healthcare; and Erin Hanley for her editorial contributions to this paper; Ms. Hanley did not receive compensation for her contributions, apart from her employment at the institution from where this paper was generated.
Funding sources: The work described here was funded by NHLBI contract #HHSN268200900031C, the Hock Family Foundation, the Hubert Yeargan Center for Global Health, the Ruth Lilly Foundation, and NHLBI/FIC grant #K01TW008407.
ABBREVIATIONS
- AIDS
acquired immunodeficiency syndrome
- AMPATH
Academic Model Providing Access to Healthcare
- CCU
Cardiac Care Unit
- CDU
Cardiovascular Diagnostic Unit
- COE
Centers of Excellence
- CVD
cardiovascular disease
- HIV
human immunodeficiency virus
- MTRH
Moi Teaching and Referral Hospital
- NHLBI
National Heart, Lung and Blood Institute
Footnotes
Disclosures: All authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mirzaei M, Truswell AS, Taylor R, et al. Coronary heart disease epidemics: not all the same. Heart. 2009;95:740–6. doi: 10.1136/hrt.2008.154856. [DOI] [PubMed] [Google Scholar]
- 3.Braunwald E. Shattuck lecture--cardiovascular medicine at the turn of the millennium: triumphs, concerns, and opportunities. N Engl J Med. 1997;337:1360–9. doi: 10.1056/NEJM199711063371906. [DOI] [PubMed] [Google Scholar]
- 4.Murthy S, Adhikari NK. Global health care of the critically ill in low-resource settings. Ann Am Thorac Soc. 2013;10:509–13. doi: 10.1513/AnnalsATS.201307-246OT. [DOI] [PubMed] [Google Scholar]
- 5.Hunter DJ, Reddy KS. Noncommunicable diseases. N Engl J Med. 2013;369:1336–43. doi: 10.1056/NEJMra1109345. [DOI] [PubMed] [Google Scholar]
- 6.Ali MK, Rabadán-Diehl C, Flanigan J, Blanchard C, Narayan KM, Engelgau M. Systems and capacity to address noncommunicable diseases in low- and middle-income countries. Sci Transl Med. 2013;5:181cm4. doi: 10.1126/scitranslmed.3005121. [DOI] [PubMed] [Google Scholar]
- 7.Kruk ME, Nigenda G, Knaul FM. Redesigning primary care to tackle the global epidemic of noncommunicable disease. Am J Public Health. 2015;105:431–7. doi: 10.2105/AJPH.2014.302392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sridhar D, Batniji R. Misfinancing global health: a case for transparency in disbursements and decision making. Lancet. 2008;372:1185–91. doi: 10.1016/S0140-6736(08)61485-3. [DOI] [PubMed] [Google Scholar]
- 9.Amico P, Aran C, Avila C. HIV spending as a share of total health expenditure: an analysis of regional variation in a multi-country study. PLoS One. 2010;5:e12997. doi: 10.1371/journal.pone.0012997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Etyang AO, Munge K, Bunyasi EW, et al. Burden of disease in adults admitted to hospital in a rural region of coastal Kenya: an analysis of data from linked clinical and demographic surveillance systems. Lancet Glob Health. 2014;2:e216–24. doi: 10.1016/S2214-109X(14)70023-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reidpath DD, Allotey P. The burden is great and the money little: Changing chronic disease management in low- and middle-income countries. J Glob Health. 2012;2:020301. doi: 10.7189/jogh.02.020301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Institute for Health Metrics and Evaluation (IHME) Health Service Provision in Kenya: Assessing Facility Capacity, Costs of Care, and Patient Perspectives. IHME; Seattle, WA: 2014. [Google Scholar]
- 13.World Health Organization Everybody's Business: Strengthening Health Systems to Improve Health Outcomes. WHO’s Framework for Action. 2007 World Health Organization web site. Available at: http://www.who.int/healthsystems/strategy/everybodys_business.pdf. Accessed September 30, 2015.
- 14.Nabel EG, Stevens S, Smith R. Combating chronic disease in developing countries. Lancet. 2009;373:2004–6. doi: 10.1016/S0140-6736(09)61074-6. [DOI] [PubMed] [Google Scholar]
- 15.UnitedHealth Group/National Heart, Lung, and Blood Institute Centres of Excellence A global research network for non-communicable diseases. Lancet. 2014;383:1446–7. doi: 10.1016/S0140-6736(13)61808-5. [DOI] [PubMed] [Google Scholar]
- 16.Bloomfield GS, Kimaiyo S, Carter EJ, et al. Chronic noncommunicable cardiovascular and pulmonary disease in sub-Saharan Africa: an academic model for countering the epidemic. Am Heart J. 2011;161:842–7. doi: 10.1016/j.ahj.2010.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Einterz RM, Kimaiyo S, Mengech HN, et al. Responding to the HIV pandemic: the power of an academic medical partnership. Acad Med. 2007;82:812–8. doi: 10.1097/ACM.0b013e3180cc29f1. [DOI] [PubMed] [Google Scholar]
- 18.Gaziano TA, Reddy KS, Paccaud F, et al. Cardiovascular disease. In: Jamison DT, Breman JG, Measham AR, et al., editors. Disease Priorities in Developing Countries. 2nd World Bank; Washington, DC: 2006. pp. 645–62. [Google Scholar]
- 19.Inui TS, Nyandiko WM, Kimaiyo SN, et al. AMPATH: living proof that no one has to die from HIV. J Gen Intern Med. 2007;22:1745–50. doi: 10.1007/s11606-007-0437-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koech MM, Barasa FA. Rheumatic heart disease: an echocardiographic profile at the MTRH, Eldoret, Kenya. Cardiovasc J Afr. 2011;22:S9. [Google Scholar]
- 21.Chuma J, Okungu V. Viewing the Kenyan health system through an equity lens: implications for universal coverage. Int J Equity Health. 2011;10:22. doi: 10.1186/1475-9276-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Hospital Insurance Fund Center for Health Market Innovations web site. 2015 Available at: http://healthmarketinnovations.org/program/national-hospital-insurance-fund-nhif. Accessed September 30, 2015.
- 23.Cameron A, Ewen M, Ross-Degnan D, et al. Medicine prices, availability, and affordability in 36 developing and middle-income countries: a secondary analysis. Lancet. 2009;373:240–9. doi: 10.1016/S0140-6736(08)61762-6. [DOI] [PubMed] [Google Scholar]
- 24.Pastakia S, Manji I, Jakait B. Community based approaches to reduce medication stockouts: Kenya; Presented at: Geneva Health Forum; Geneva. 2012. Available at: http://ghf.g2hp.net/2011/12/11/community-based-approaches-to-reduce-medication-stockouts-in-kenya/. Accessed October 5, 2015. [Google Scholar]
- 25.World Health Organization Chapter 13: Revolving drug funds and user fees. 2012 World Health Organization web site. Available at: http://apps.who.int/medicinedocs/documents/s19589en/s19589en.pdf. Accessed September 30, 2015.
- 26.Manji I, Pastakia SD, Do AN, et al. Performance outcomes of a pharmacist-managed anticoagulation clinic in the rural, resource-constrained setting of Eldoret, Kenya. J Thromb Haemost. 2011;9:2215–20. doi: 10.1111/j.1538-7836.2011.04503.x. [DOI] [PubMed] [Google Scholar]
- 27.Tierney WM, Rotich JK, Hannan TJ, et al. The AMPATH medical record system: creating, implementing, and sustaining an electronic medical record system to support HIV/AIDS care in western Kenya. Stud Health Technol Inform. 2007;129:372–6. [PubMed] [Google Scholar]
- 28.Akwanalo CO, Kimaiyo S, Delong AK, et al. The prevalence of undiagnosed hypertension, diabetes, and target organ damage in a rural community in Western Kenya; Paper presented at: European Society of Cardiology Congress; Barcelona, Spain. 2014. August 30–September 3. [Google Scholar]
- 29.Barasa AF, Delong A, Kimaiyo S, et al. Utility of hand-held echocardiography among clinical officers in patients referred for routine echocardiography at Moi Teaching and Referral Hospital, Kenya; Paper presented at: NHLBI-UnitedHealth Global Health Program 9th and Final Semi-Annual Steering Committee Meeting; Bethesda, MD. Apr 13-14, 2014. [Google Scholar]
- 30.Park PH, Wambui CK, Atieno S, et al. Improving diabetes management and cardiovascular risk factors through peer-led self-management support groups in Western Kenya. Diabetes Care. 2015;38:e110–1. doi: 10.2337/dc15-0353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bloomfield G, Agarwal A, Menya D, et al. Traditional cookstove replacement and resultant health effects in Kenya: baseline results of a pilot echocardiographic study; Paper presented at: NHLBI/UnitedHealth Centers of Excellence Steering Committee Meeting; Bethesda, MD. Apr 13-16, 2014. [Google Scholar]
- 32.Vedanthan R, Kamano JH, Naanyu V, et al. Optimizing linkage and retention to hypertension care in rural Kenya (LARK hypertension study): study protocol for a randomized controlled trial. Trials. 2014:15–143. doi: 10.1186/1745-6215-15-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bloomfield GS, Temu TM, Akwanalo CO, et al. Genetic mutations in African patients with atrial fibrillation: rationale and design of the Study of Genetics of Atrial Fibrillation in an African Population (SIGNAL) Am Heart J. 2015;170:455–464. doi: 10.1016/j.ahj.2015.06.008. e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vedanthan R, Kamano JH, Horowitz CR, et al. Nurse management of hypertension in rural western Kenya: implementation research to optimize delivery. Ann Glob Health. 2014;80:5–12. doi: 10.1016/j.aogh.2013.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mbacke CS. African leadership for sustainable health policy and systems research. BMC Health Serv Res. 2013;13(Suppl 2):S15. doi: 10.1186/1472-6963-13-S2-S15. [DOI] [PMC free article] [PubMed] [Google Scholar]