Abstract
Hip arthroscopy has recently become a common procedure to treat central and peripheral hip pathology. Capsulotomies are necessary in these procedures, and negotiating adequate visualization, as well as capsular preservation, is a challenge. We describe a capsular suspension technique that allows for adequate visualization of the central and peripheral compartments while facilitating preservation of the native hip capsule. This technique eliminates the need for additional personnel for retraction, potentially decreases iatrogenic hip injury, eliminates the need for excessive capsular debridement, and allows for capsular closure under minimal tension.
Hip arthroscopy is a common procedure to treat central and peripheral hip pathology, including femoroacetabular impingement and labral tears, that results in pain and disability. Capsulotomy allows for proper visualization and instrumentation in treating intracapsular pathology of the hip joint. Both basic science1, 2, 3 and clinical4, 5 data support the importance of capsular repair after capsulotomy to decrease the risk of instability, decrease revision rates, and improve sports-specific outcome scores. Although capsular repair is often the goal, excessive debridement of the capsule for visualization and access, as well as iatrogenic contact from repeated instrument placement, often leaves the capsule edges difficult to repair with physiological tension, if at all. We describe a capsular suspension technique that allows for adequate visualization of the central and peripheral compartments in the setting of a T-capsulotomy while preserving the native hip capsule for later repair. This technique eliminates the need for additional personnel for retraction, minimizes iatrogenic contact, eliminates the need for excessive capsular debridement, and allows for capsular closure under minimal tension.
Technique
A standard supine hip arthroscopy technique is used, and traction is applied to allow initial access through the central compartment. Video 1 demonstrates this technique from initial capsulotomy to capsular closure with narration. Table 1 includes all specific instrumentation used intraoperatively.
Table 1.
Specific Instrumentation Used to Perform Technique
| Suture passer: Injector; Pivot Medical (Sunnyvale, CA)/Stryker |
| Suture: Zipline; Pivot Medical/Stryker |
| Radiofrequency ablator: ArthroCare (Sunnyvale, CA)/Smith & Nephew (London, England) |
| Shaver: 4-mm Tomcat; Stryker |
| Beaver blade: Samurai; Pivot Medical |
| Cannula: Transport; Pivot Medical |
| 5-mm round burr: Pivot Medical |
Central Compartment
The technique begins with standard central-compartment access, and an anterior portal (AP) and anterolateral portal (ALP) are established. We prefer a modified AP, approximately 1 cm lateral and distal to the intersection of the horizontal line at the tip of the greater trochanter and the vertical line starting at the anterior superior iliac spine. Once both ALP and AP cannulas have been placed, the precapsular fatty tissue is identified and removed using radiofrequency (RF) ablation until the anterior portion of the capsule is visualized. By use of a beaver blade (Samurai; Stryker, Kalamazoo, MI), an interportal capsulotomy is performed through the ALP, measuring approximately 2 to 4 cm in length depending on pathomorphology. It is important to note that enough capsule must be left proximally (acetabular side) for later suspension and subsequent repair. Approximately 5 to 8 mm of capsule distal to the labrum is adequate.5 The first portion of the interportal capsulotomy is made with visualization through the AP and the beaver blade in the ALP. This cut is made from medial to lateral until the gluteus minimus muscle is seen at the lateral aspect of the capsulotomy (Fig 1A). The visualization and working portals are switched to complete the second half of the capsulotomy. Focus is placed on making a smooth, singular cut through the capsule. This medial portion of the cut traditionally ends prior to visualization of the iliopsoas but should be as extensive as needed to address the central-compartment pathology. The edges of the interportal capsulotomy are trimmed with a 4-mm shaver (Stryker) at a low speed (revolutions per minute) to avoid excessive debridement of the capsule. The goal is to achieve smooth edges to place the retraction sutures and not to decrease the amount of capsule.
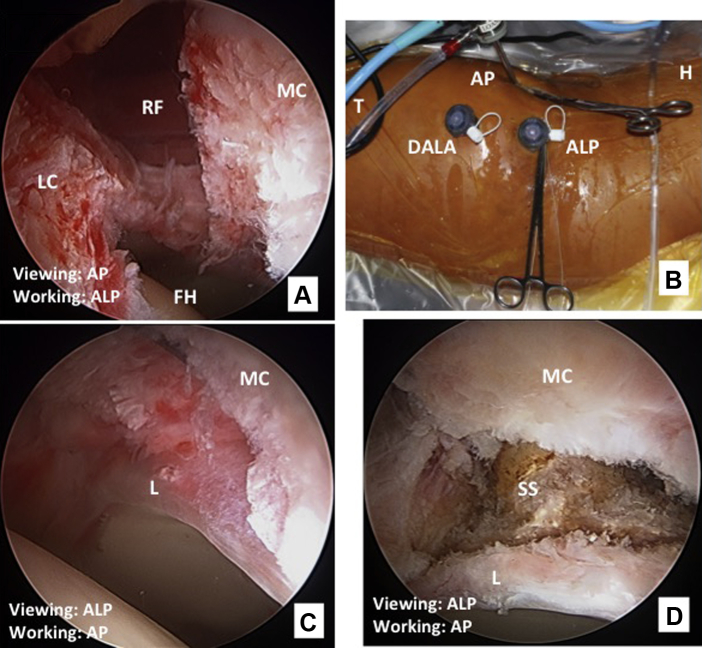
Fig 1.
(A) Central-compartment capsulotomy in a left hip, showing the reflected head of the rectus femoris in the medial aspect of the capsulotomy. Visualization is performed through the anterior portal (AP) and working through the anterolateral portal (ALP). (B) Portal and suspension clamp setup in a left hip with the patient in the supine position. The cephalad (H) aspect of the patient is on the right, and the caudad (T) aspect is on the left. The camera is viewing from the AP with a clamp suspending the medial capsule (MC). Another clamp is on the ALP suspending the lateral capsule (LC), and the distal anterolateral (DALA) portal is the most distal portal. (C) Visualization of the central compartment with the ALP as the viewing portal, showing a clear view of the labrum (L) with a retracted medial capsule; the lateral capsule is outside the viewing field. (D) Visualization of subspine (SS) from ALP with the medial capsule suspended and the labrum inferiorly. (FH, femoral head; RF, rectus muscle.)
The suspension technique begins at the medial portion of the proximal capsule. By use of the AP as the working portal, a suture-shuttling device of the surgeon's choice is used to pass a horizontal mattress suture. The short side of the suture within the suture-shuttling device is placed on the medial side because the mattress stitch limbs will be passed medially to laterally (Table 2). Performing the mattress stitch while moving away from the short side of the suture will prevent crossover of the stitch that compromises the retraction of the capsule and retrieval of the second part of the mattress stitch. The surgeon must be sure to have enough slack when passing the second limb of the mattress stitch to ensure that the suture-shuttling device can grab and pass the suture through the tissue. Once both limbs of the mattress stitch have been passed, the cannula is removed. The 2 free ends of suture are then drawn out of the AP and snapped in tension against the skin with a medium-sized clamp (Fig 1B). Selection of a clamp that is too small will result in inadequate retraction, with the clamp being pulled into the portal site. The tension of the clamp against the skin controls and suspends the capsule upward, allowing for central-compartment visualization. This creates capsular suspension for the medial portion of the proximal capsule while allowing for future manipulation or tightening of the capsular retraction if necessary. The cannula may or may not be placed back into the portal site based on the surgeon's preference. The same technique is used to place a mattress stitch in the lateral portion of the proximal capsule. In summary, 2 horizontal mattress stitches are used to suspend the proximal capsule. The central compartment can now be visualized, and the proximal capsule is well controlled to allow access to the acetabular rim and subspinous region while still preserving the capsule for repair (Fig 1 C and D).
Table 2.
Description of Portal Use and Suture Technique in Capsular Suspension
| Area of Treatment (in Chronologic Order) | Portal Suture Inserted | Portal Suture Retrieved | Suture Construct | Type of Tension Placed |
|---|---|---|---|---|
| Medial proximal limb | AP | AP | Mattress | Tight |
| Lateral proximal limb | ALP | ALP | Mattress | Tight |
| Lateral leaflet, distal capsule | DALA | ALP | Mattress | Tight |
| Medial leaflet, distal capsule | DALA | DALA | Single or mattress | Relaxed |
| Accessory lateral leaflet, lateral to apex | ALP | ALP | Single | Tight |
ALP, anterolateral portal; AP, anterior portal; DALA, distal anterolateral portal.
Once both the medial and lateral aspects of the proximal capsule have been suspended, a shaver is introduced through the AP to clean up the edges of the capsule. It is then used to “peel” the undersurface of the proximal capsule back, working from the labrum to the anterior inferior iliac spine. This is achieved using RF ablation and a shaver device. After the inferior capsule has been released, proximal capsular suspension can be retightened to maintain adequate retraction and visualization. At this point, pathology within the central compartment can be addressed.
Peripheral Compartment
To address peripheral-compartment pathology, axial traction is relaxed as the hip is placed in slight flexion and neutral rotation. We prefer to use a distal anterolateral (DALA) portal that is typically in line with the ALP and 4 cm distal. This portal is used during central-compartment arthroscopy to place suture anchors and is the primary working portal during peripheral-compartment arthroscopy. Through the DALA portal, RF ablation is used to clear precapsular fat and visualize the interval between the iliocapsularis muscle and gluteus minimus. By use of the beaver blade, a T-capsulotomy is extended perpendicular from the interportal capsulotomy to the intertrochanteric line as previously described.6 Once again, focus is placed on making a single, smooth, longitudinal “T” cut in the capsule. This creates a 180° view of the peripheral compartment allowing for femoral osteochondroplasty.
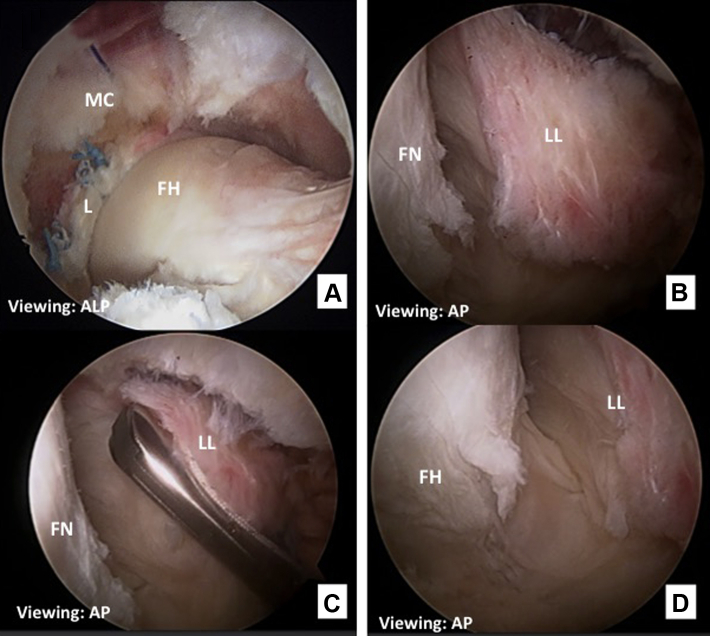
Capsular suspension is achieved with the suture-shuttling device inserted through the DALA portal with visualization through the AP. The first limb of the mattress construct is placed at the distal aspect of the lateral leaflet, with the second limb placed near the proximal corner or apex of the lateral leaflet. Again, the short side of the suture should be distal when passing the first limb of the mattress construct to prevent crossing of the suture. Both suture limbs are then retrieved through the ALP and placed in tension with the same capsular suspension technique as the central compartment (Fig 2A). With attention turned toward the medial leaflet, the suture-shuttling device is inserted through the DALA portal and grasps the leaflet at midcapsulotomy. Without passing the suture, the medial leaflet is grasped and pulled back, with the surgeon noting the amount of exposure. If the surgeon believes that exposure of the peripheral compartment is adequate, a single suture may be passed at this level and retrieved out the DALA portal for capsular suspension. If exposure is deemed inadequate, a mattress construct can be passed in the same fashion as the lateral capsule. Approximately 90% of the time, only a single suture is necessary. The medial leaflet is retracted under less tension than the aforementioned capsular leaflets to allow for mobility of surgical instruments during femoral osteochondroplasty. On occasion, after both the lateral and medial leaflets are suspended, the proximal portion of the lateral leaflet obstructs proper visualization (Fig 2B). If this is the case, a single additional retraction suture may be placed and retrieved through the ALP (Fig 2C), just lateral to the apex of the lateral leaflet, to achieve better visualization (Fig 2D).
Fig 2.
(A) Peripheral compartment in a left hip viewed through the anterolateral portal (ALP) after labral repair and before osteochondroplasty within this compartment. The femoral head (FH) is inferior, the medial capsule (MC) is suspended, and the labrum (L) has been repaired. (B) Proximal portion of the lateral leaflet of the peripheral-compartment obstructing visualization after placement of 1 medial and 1 lateral suspension suture, with visualization through the anterior portal (AP). (C) Placement of the second stitch in the lateral capsule, viewing from the AP. (D) Suspension of the lateral capsule with visualization of a cam lesion, as well as the lateral synovial folds about the lateral limb of the capsule. (FN, femoral neck; LL, lateral limb.)
After use of 2 or 3 sutures for adequate exposure of the peripheral compartment, the ALP is used as the working portal for addressing peripheral-compartment pathologies (Fig 3). Typically, the medial leaflet is more mobile, and the burr can be brought through the ALP to reach the farthest lateral portions of cam lesions.
Fig 3.
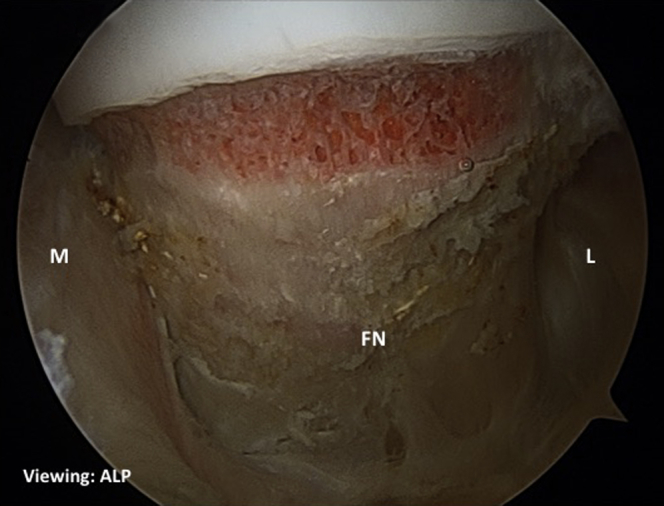
Peripheral compartment in a left femur viewed through the anterolateral portal (ALP) with initiation of osteochondroplasty, with excellent visualization of the cam lesion, as well as the medial (M) and lateral (L) base of the femoral neck (FN).
Capsule Repair
When the surgeon is repairing the capsule, all traction is released from capsular suspension and the sutures are removed. Although existing sutures can be used, we find that efficient use of a suture-shuttling device allows the sutures to be replaced more quickly than using existing sutures—the time savings primarily results from reducing the risk of suture entanglement. In addition, passing new sutures allows for optimal placement to maximize the quality of the closure. The longitudinal T-capsulotomy incision is repaired first, with placement of 3 evenly spaced sutures, all through the DALA portal with visualization through the AP. The surgeon places the distal-most stitch first, loading the suture's short side medially and passing through the medial leaflet first and then through lateral leaflet. A standard arthroscopic knot-tying technique is used to secure the suture. The midlongitudinal suture is placed and tied in similar fashion. The third suture is placed through the apex of the medial leaflet and then lateral leaflet. To ensure complete closure of the capsule, the suture should be passed fully through the deep (articular) surface of the capsule (Fig 2D).
Once the longitudinal T-capsulotomy has been adequately repaired, attention is directed toward closure of the interportal capsulotomy. We prefer to continue to view through the AP but switch to working through the ALP. The ALP cannula is carefully placed in the interval between the gluteus minimus and iliocapsularis muscle, under the gluteus minimus. This is in contrast to the typical initial placement of the ALP during central-compartment arthroscopy. Working through this interval is important because it prevents incorporation of the gluteus minimus muscle within the suture construct. Furthermore, working through this portal allows access to both the medial and lateral portions of the interportal capsulotomy. By use of RF, the interval between the capsule and the rectus femoris is developed. It is important to not capture the rectus tendon in the repair of the medial limb of the interportal capsulotomy. The 2 interportal capsulotomy sutures are placed evenly between the T cut and the edges of the initial capsulotomy. The lateral limb is closed first, followed by the medial limb. Five single-stitch sutures are used to close the full T-capsulotomy.
Discussion
Interest in capsule repair is growing, as is the evidence to support capsule repair.5, 7 As the data encouraging complete capsular repair increase,4, 5 so does the need for intraoperative preservation of the capsule. The presented capsular suspension technique is safe, reproducible, and beneficial on many levels (Table 3). This technique requires approximately 10 minutes of setup and eliminates the need for extra-personnel retraction throughout the case. There are several pearls to help avoid possible difficulties (Table 3). Benefits include adequate visualization and capsule preservation. This capsular suspension technique limits the need for excessive capsular debridement for visualization and potentially decreases iatrogenic damage to the capsule edges by removing the capsule from the working area. Substantial capsular debridement in the setting of insufficient retraction often necessitates nonanatomic over-tightening of the repaired capsule, resulting in constraint of the hip joint.5 Release of the undersurface of the proximal capsule to the anterior inferior iliac spine in conjunction with capsular suspension likely contributes to avoiding over-tightening on repair. Furthermore, the tension on the proximal capsule provided by the suspension sutures allows peeling back of the proximal capsule from the acetabular rim and subspinous region, allowing for subspine decompression if necessary while still allowing capsular closure. Advantages and risks involved with this technique are delineated in Table 4.
Table 3.
Technical Pearls and Benefits to Capsular Suspension Technique
| Technical pearls |
| The surgeon should leave adequate proximal capsule with the interportal capsulotomy for repair (5-8 mm distal to labrum). |
| Using untied mattress stitches for capsular suspension will reduce the total number of sutures used. |
| For interportal capsulotomy repair, the surgeon must ensure that the ALP cannula is inserted at the interval between the ICM and the gluteus minimus to avoid incorporating the gluteus minimus in the stitch and to allow access to the entire interportal capsulotomy from the ALP. |
| Developing the plane between the rectus femoris and capsule will prevent incorporation of muscle and/or tendon into capsule repair. |
| Benefits of technique |
| Offers improved visualization of the central and peripheral compartments |
| Enables preservation of the clean, native capsule edge, decreasing the need for excessive debridement and incidence of iatrogenic damage |
| Helps prevent over-tightening and subsequent stiffness by protecting the native edges of the capsule and removing them from the working area during treatment of central- and peripheral-compartment pathology |
| Allows exposure of the acetabular rim and subspinous region—as a result of suspension and retraction of the proximal capsule—while preserving the capsule for repair |
| Avoids the potential problem of an inadequate capsule for repair due to debridement for visualization or iatrogenic damage |
| Allows for peripheral-compartment access without the need for an assistant |
ALP, anterolateral portal; ICM, iliocapsularis muscle.
Table 4.
Potential Risks and Benefits of Capsular Suspension Technique for Hip Arthroscopy
| Potential advantages |
| Elimination of the need for additional personnel for retraction |
| Protection of the post-arthrotomy capsular edges from iatrogenic injury to facilitate later tension-free repair |
| Increased visualization within the central and peripheral compartments |
| Decreasing skin-to-joint distance, allowing for arthroscopy in larger individuals |
| Potential disadvantages/risks |
| Additional surgical time |
| Difficulty negotiating portals with tension sutures |
| Tension suture tangling |
NOTE. Capsular suspension has several advantages, as well as risks, as summarized in this table. Because of the recent adoption of the described technique, the frequency of complications resulting from this technique cannot be reported because no such data are available in the literature yet.
Summary
Safe and effective hip arthroscopy necessitates capsulotomies. Increasing evidence shows the critical role of the iliofemoral ligament in normal hip biomechanics. Closure of the capsule can lead to improved clinical outcomes4; however, there is often difficulty in creating proper visualization while still leaving enough capsule to be adequately repaired, particularly when concomitant subspine decompression is indicated. We propose a simple capsular suspension technique that allows for reliable retraction of the capsule while preserving the native capsule edge for an anatomic repair after treatment of central- and peripheral-compartment pathology.
Footnotes
The authors report the following potential conflict of interest or source of funding: S.N. receives support from Stryker and Ossur. S.H.C. receives support from Blue Belt Technologies and Stryker. R.C.M. receives support from Stryker, Smith & Nephew, KNG Health Consulting, Duke Orthopaedic Surgery, and forMD.
Supplementary Data
Arthroscopic labral repair and femoral osteochondroplasty in the left hip of a 35-year-old female patient. Visualization and working portals are delineated in the lower right corner. (ALP, anterolateral portal; AP, anterior portal; DALA, distal anterolateral portal.)
References
- 1.Bowman K.F., Jr., Fox J., Sekiya J.K. A clinically relevant review of hip biomechanics. Arthroscopy. 2010;26:1118–1129. doi: 10.1016/j.arthro.2010.01.027. [DOI] [PubMed] [Google Scholar]
- 2.Myers C.A., Register B.C., Lertwanich P. Role of the acetabular labrum and the iliofemoral ligament in hip stability: An in vitro biplane fluoroscopy study. Am J Sports Med. 2011;39:85S–91S. doi: 10.1177/0363546511412161. (suppl) [DOI] [PubMed] [Google Scholar]
- 3.Hughes A.W., Clark D., Carlino W., Gosling O., Spencer R.F. Capsule repair may reduce dislocation following hip hemiarthroplasty through a direct lateral approach: A cadaver study. Bone Joint J. 2015;97-B:141–144. doi: 10.1302/0301-620X.97B1.34038. [DOI] [PubMed] [Google Scholar]
- 4.Frank R.M., Lee S., Bush-Joseph C.A., Kelly B.T., Salata M.J., Nho S.J. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: A comparative matched-pair analysis. Am J Sports Med. 2014;42:2634–2642. doi: 10.1177/0363546514548017. [DOI] [PubMed] [Google Scholar]
- 5.Harris J.D., Slikker W., III, Gupta A.K., McCormick F.M., Nho S.J. Routine complete capsular closure during hip arthroscopy. Arthrosc Tech. 2013;2:e89–e94. doi: 10.1016/j.eats.2012.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suslak A.G., Mather R.C., III, Kelly B.T., Nho S.J. Improved arthroscopic visualization of peripheral compartment. Arthrosc Tech. 2012;1:e57–e62. doi: 10.1016/j.eats.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chow R.M., Engasser W.M., Krych A.J., Levy B.A. Arthroscopic capsular repair in the treatment of femoroacetabular impingement. Arthrosc Tech. 2013;3:e27–e30. doi: 10.1016/j.eats.2013.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic labral repair and femoral osteochondroplasty in the left hip of a 35-year-old female patient. Visualization and working portals are delineated in the lower right corner. (ALP, anterolateral portal; AP, anterior portal; DALA, distal anterolateral portal.)