Abstract
Dry arthroscopy is attractive because it affords an unsurpassed clarity of view and minimizes swelling. The elbow is a challenging joint to assess arthroscopically; however, dry arthroscopy has some particular benefits in the elbow. The primary benefit is the quality of the tissue definition, but dry arthroscopy also increases the working time for surgery by reducing swelling and results in less postoperative discomfort for the patient. With dry arthroscopy, all joint surfaces are covered in synovial fluid, which reflects light, to provide a clearer image of the joint surfaces and depth of field. The air-fluid interface provides an uninterrupted appreciation of the synovial recesses and tissue perfusion. This article describes the technique and indications for dry elbow arthroscopy, which will allow other surgeons to reap the benefits of dry arthroscopy without the need for special equipment or changes in their basic technique.
Elbow arthroscopy is usually performed using fluid inflow regulated by gravity or a pump. With an extended surgical time, considerable soft-tissue swelling and extravasation of fluid can occur, placing neurovascular structures at risk and risking compartment syndrome.
To our knowledge, dry arthroscopy has not been described in the elbow; however, it is becoming popular in the wrist, in which both diagnostic and therapeutic procedures can be performed.1 In patients with shoulder instability, some authors advocate that initial assessment of the capsulolabral structures should be performed dry, to prevent fluid distension exaggerating the pathology.2 Dry endoscopy is routinely used in the thoracic and abdominal cavities with air insufflation. Dry endoscopy has been described for extra-articular procedures around the elbow, including ulnar nerve decompression/transposition, distal biceps repair, and olecranon bursectomy.3, 4, 5 We have developed a technique to perform dry elbow arthroscopy by application of skills developed in wrist arthroscopy and dry endoscopy. This article outlines the current indications, advantages, and technical aspects of dry elbow arthroscopy.
Surgical Technique
We routinely perform dry elbow arthroscopy in every case that would have required “wet arthroscopy” in the past.
Setup
Surgery is performed with the patient under general anesthesia, in the lateral decubitus position, with a sterile tourniquet applied. A list of required instruments is given in Table 1.
Table 1.
Equipment Required for Dry Arthroscopy of Elbow
| Equipment | Essential or Desirable |
|---|---|
| Sterile tourniquet | Desirable |
| Low-profile arm support | Essential |
| 4.0-mm cannula with 2 inlet taps | Essential |
| 30° arthroscope | Essential |
| 4.0-mm shaver with variable suction control | Essential |
| Radiofrequency ablation probe | Desirable |
| Arthroscopic retractors (right-angled retractors and mini-Homan retractors) | Essential |
| Irrigation fluid | Essential |
| Metallic narrow-bore outflow cannula | Desirable |
Procedure
The joint is insufflated with air using a 20-mL syringe through the soft spot formed by the radial head, lateral epicondyle, and olecranon. This moves the capsule and overlying neurovascular structures away from the joint as it is entered with a trocar. A proximal-superior-medial viewing portal is created 2 cm proximal to the medial epicondyle and just anterior to the medial intermuscular septum. Only the skin is incised to avoid inadvertent cutaneous nerve injury, and the joint is entered using a blunt trocar. Dissection through the joint capsule with an artery clip is avoided because this creates a large capsular perforation and allows dissipation of air into the extra-articular tissues. A 4.0-mm, 30° arthroscope (Karl Storz, Tuttlingen, Germany) is inserted. If visualization is poor but entry into the joint is confirmed by visualization of the articular cartilage, the joint is insufflated with 20 mL of room air through the inlet on the arthroscope sheath. The inlet tap is closed after insufflation to minimize air dissipation. The lateral capsule is identified, and a lateral working portal is created by an inside-out technique. Standard arthroscopic instruments are introduced through this working portal. A complete diagnostic assessment of the anterior compartment is performed, followed by treatment of intra-articular pathology as necessary.
Attention is then turned to the posterior compartment. A midline posterior viewing portal 2 cm proximal to the olecranon tip is created. A posterolateral working portal is made 2 cm lateral to the viewing portal using an outside-in technique. It can be difficult to obtain a view in the posterior compartment until the soft tissue is cleared from the olecranon fossa. This is performed using a shaver through the working portal. Once the view improves, air is used to maintain the working space as described for the anterior compartment. The posterolateral and posteromedial gutters are viewed, and the presence of instability is assessed by applying varus and valgus forces in pronation, supination, flexion, and extension. Gapping of the ulnohumeral articulation or the drive-through sign, in which the arthroscope can be “driven” into the anterior compartment, is indicative of instability (Video 1). More commonly, soft-tissue lesions such as plicae are debrided in the posterior compartment, as are posterior osteophytes that may cause impingement in extension. At the end of the procedure, the posterior and anterior compartments are thoroughly irrigated to clear any residual debris and reduce the chance of infection.
Technical Pearls
Technical pearls are summarized in Table 2.
Table 2.
Pearls and Pitfalls of Procedure
| Reason | |
|---|---|
| Pearls | |
| Do not use artery clip to open capsule | Allows air to dissipate into soft tissues |
| Use low-pressure air to insufflate joint | Expands working space safely |
| Use intermittent low-pressure suction | Prevents collapse of working space |
| Point shaver blade away from camera | Prevents coating of camera with debris |
| Use irrigation with radiofrequency probe | Avoids heating of chondral surfaces |
| Use retractors liberally | Helps maintain safe working space |
| Use intermittent irrigation and suction | Efficiently clears bony debris |
| Irrigate joint at end of procedure | Minimizes infection risk |
| Pitfalls | |
| Avoid performing aggressive suction | Collapses working space and draws in neurovascular structures |
| Avoid making multiple passes when entering joint | Allows air to dissipate into soft tissues |
| Avoid using air insufflation in acute fractures | May predispose to air embolus due to exposed vascular surfaces |
Maintaining Working Space
To maintain safe visualization during elbow arthroscopy, it is necessary to keep the anterior soft tissues away from the bony structures. We achieve this by manual air insufflation, using a 20-mL syringe to maintain capsular distension. When entering the joint, we use a blunt trocar immediately after the skin incision and advance it through the capsule in one motion. This minimizes the size of the capsular perforation and air escape into the soft tissues. After injecting air through the 3-way valve on the arthroscope, we turn the valve off to minimize slow loss of air. Suction is necessary to clear debris and blood on occasion, but it must be used carefully. Uncontrolled suction results in collapse of the joint and loss of visualization; however, low-pressure intermittent suction is beneficial.
We frequently use retractors. These are either standard right-angled retractors or flat retractors, such as mini-Hohmann retractors (Innomed, Savannah, GA). No specific or custom equipment is required. The retractors are inserted either through the viewing portal alongside the arthroscope or through an accessory portal. The assistant retracts the capsule manually, which maintains the working space.
Maintaining Visualization
Aside from collapse of the joint space, visualization can be affected by condensation (fogging) of the arthroscope and by blood and debris adhering to the end of the arthroscope. If present, fogging settles as the case proceeds. This is due to an initial temperature mismatch between the joint and arthroscope. Wiping the lens with an alcohol swab or immersing the arthroscope in warm saline solution before starting the procedure minimizes fogging. Blood, debris, and condensation on the lens can also be removed by wiping the lens on the intra-articular soft tissues, which avoids removal of the arthroscope. To reduce contamination of the lens, shavers or burrs should be pointed away from the lens when in use. Short bursts of irrigation and suction on the shaver are very useful to rapidly clear the visual field and maintain a dry environment.
Using Radiofrequency Probes
A common concern with dry arthroscopy is the use of radiofrequency devices or cautery. If used, we recommend a low setting and short pulses of activity. This should be accompanied by frequent irrigation and suction to prevent overheating of the cartilage. When radiofrequency probes are used in a dry environment, smoke generation occurs. If excessive, opening the valve on the arthroscope and balloting the soft tissues will dissipate the smoke. These maneuvers act as a bellows to pump smoke out of the joint.
Discussion
We now routinely perform all elbow arthroscopies dry. Depending on the technical demands of the procedure, we do use fluid in the latter part of the case, although the need for this is decreasing with experience. We have not had any postoperative complications related to using a dry technique.
Advantages of Dry Arthroscopy
Tissue Definition
The key benefit of dry arthroscopy is the quality of tissue definition. Figure 1 shows the view achieved during a diagnostic arthroscopy. Subtle areas of synovitis and chondral damage, as well as partial ligament tears, are more obvious when dry. This is because the articular surfaces remain coated with synovial fluid, which reflects light at the air-fluid interface. This provides greater detail of the tissue surface. With wet arthroscopy, fluid also coats the articular surfaces but there is no air-fluid interface to reflect light. This means the finer detail is not appreciated. Figure 2 shows comparative views of dry and wet arthroscopy during diagnostic and therapeutic arthroscopy.
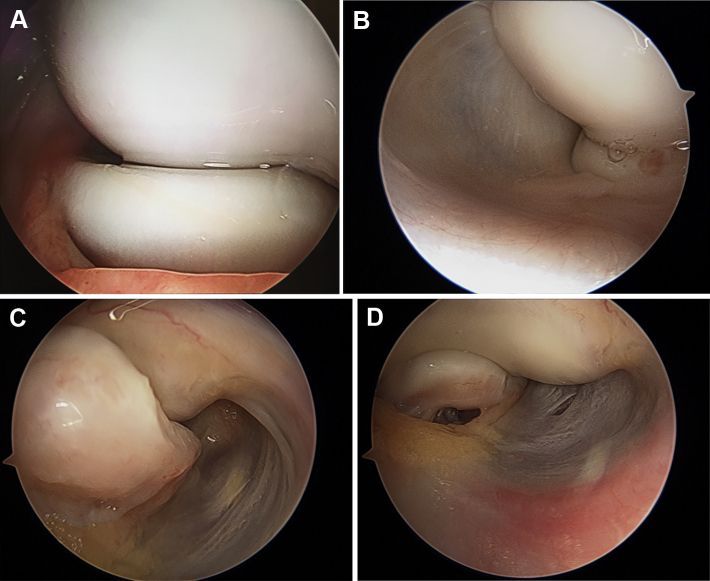
Fig 1.
Dry diagnostic arthroscopy of anterior compartment. (A) Radiocapitellar articulation viewed from anteromedial portal. The articular surfaces are coated in synovial fluid. Light reflects more readily at the air–synovial fluid interface to give a clear, vibrant image. (B) Lateral capsule and radiocapitellar joint viewed from anteromedial portal. Air distension expands the working space and tensions the capsule, which can be seen clearly. Bubbles on the surface of the synovial fluid can be seen from the air distension. (C) Medial capsule and coronoid process viewed from anterolateral portal with elbow flexed. The hammock-like anatomy of the capsule is displayed, as is the bony detail of the coronoid process and trochlea. (D) Panoramic view of anteromedial aspect of joint with elbow extended. The vascular markings of the capsule are seen with clarity that cannot be achieved when using air distension.
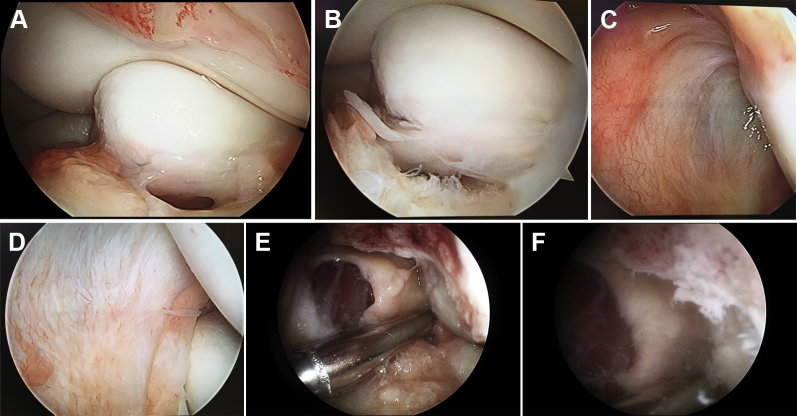
Fig 2.
Comparative views of dry and wet arthroscopy. (A) Dry and (B) wet views of coronoid process and trochlea. In the dry view, the articular surface is clear and vibrant, whereas in the wet view, it is dull in comparison. (C) Dry and (D) wet views of lateral capsule. During dry arthroscopy, the striations and detail of the capsule are superior and the light can be seen reflecting off of the soft tissues coated in synovial fluid. (E) Dry and (F) wet views of osteocapsular release of anterior compartment. In the dry view, the muscle, capsule, bone, and articular cartilage all look crisp and clear, whereas in the wet view, the image is cloudy because of debris floating in the fluid.
Reduced Intra-articular Pressure
Wet arthroscopy distends the soft tissues and compresses the capillary vessels. Dry arthroscopy does not compress these vessels, allowing a greater appreciation of synovitis, which can be underestimated when wet. During wet arthroscopy, extensive synovitis may obscure visualization because of the fluid effect (Fig 3).
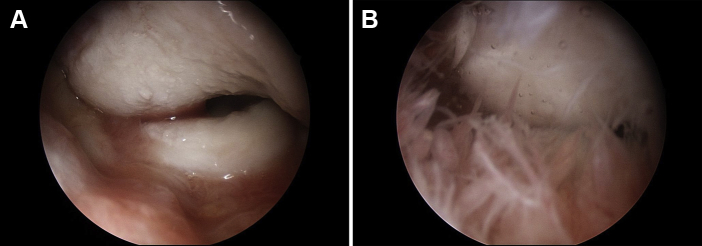
Fig 3.
Images from a patient with osteoarthritis of the elbow and anterior compartment synovitis. (A) When dry, the synovitis is visible but not obstructive; (B) however, with fluid distension, the synovitic tissue floats up and obscures the view.
We have noticed that fluid distension causes the capsule to become capacious, whereas air will not over-distend it. This may alter the surgeon's perception of capsular and ligamentous laxity, although this entity is difficult to quantify.
Swelling
Dry surgery results in less swelling. With wet arthroscopy, there is progressive swelling, which limits the “working time” for safe surgery. The swelling compromises visualization and can lead to extravasation. With dry arthroscopy, there is no swelling or extravasation, and it therefore increases the safe working time. This is particularly valuable for surgeons in the early part of their learning curve for elbow arthroscopy, when swelling and time are limiting factors.
Conversion to Open Surgery
Conversion to open surgery is easier after dry arthroscopy. The fluid extravasation accompanying wet arthroscopy compromises the soft tissues and makes it more difficult to identify the anatomic planes during dissection.
Rehabilitation
In our experience, reduced postoperative swelling after dry arthroscopy translates into patients having less pain and allows quicker mobilization and rehabilitation postoperatively.
The advantages and disadvantages of dry and wet arthroscopy are compared in Table 3. There are some potential concerns with air distension, which must be respected, such as the risk of an air embolus. Positive-pressure gas distension was the initial method of joint distension during the early years of arthroscopy, without a significant incidence of air emboli. Air emboli are rare, given the number of arthroscopic and endoscopic procedures performed on a daily basis. In particular, abdominal and thoracic endoscopy is performed with greater volumes of gas, without a tourniquet and in a field in which a greater number of veins are exposed. The minimum volume of air required to cause a minor, asymptomatic air embolus is 50 mL.6 Thus, by never injecting greater than 20 mL at a time, the risk is minimized. Finally, in the lateral position, the elbow does not lie significantly above the level of the heart, which means the air within the joint is not under greater pressure than the venous pressure. In view of the serious nature of air emboli, we advise that mechanical air insufflation should not be used for this procedure.
Table 3.
Advantages of Dry and Wet Arthroscopy
| Dry arthroscopy |
| Better tissue definition (joint surfaces, synovial reflections, and perfusion) |
| Decreased risk of swelling, fluid extravasation, and compartment syndrome |
| Easier conversion to open surgery |
| Retention of external landmarks |
| “Truer” understanding of tissues and their pathology |
| Less postoperative swelling and discomfort |
| Less expensive |
| Wet arthroscopy |
| Familiar technique |
| Sustained fluid distension and visualization of joint |
| Continuous irrigation of debris |
| Cooling effect to joint |
| Floating of synovium and loose bodies (this can be a disadvantage) |
Dry arthroscopy of the elbow is new, but there is considerable evidence from the wrist of its superiority over wet arthroscopy. On the basis of our experience, we would urge other surgeons to try this technique because they will find the improved tissue definition valuable to their practice and pathoanatomic understanding of intra-articular elbow conditions.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Compilation of diagnostic and therapeutic dry arthroscopy. A full dry diagnostic arthroscopy is shown, in addition to a dry assessment of stability in a patient with chronic global instability, as well as a dry osteocapsular release in a patient with osteoarthritis.
References
- 1.del Piñal F., García-Bernal F.J., Pisani D., Regalado J., Ayala H., Studer A. Dry arthroscopy of the wrist: Surgical technique. J Hand Surg Am. 2007;32:119–123. doi: 10.1016/j.jhsa.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 2.Rupenian P. Dry arthroscopy of the shoulder. Arthrosc Tech. 2013;2:e437–e440. doi: 10.1016/j.eats.2013.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morse L.P., McGuire D.T., Bain G.I. Endoscopic ulnar nerve release and transposition. Tech Hand Up Extrem Surg. 2014;18:10–14. doi: 10.1097/BTH.0000000000000030. [DOI] [PubMed] [Google Scholar]
- 4.Eames M.H., Bain G.I. Distal biceps tendon endoscopy and anterior elbow arthroscopy portal. Tech Shoulder Elbow Surg. 2006;7:139–142. [Google Scholar]
- 5.Tu C.G., McGuire D.T., Morse L.P., Bain G.I. Olecranon extrabursal endoscopic bursectomy. Tech Hand Up Extrem Surg. 2013;17:173–175. doi: 10.1097/BTH.0b013e31829c0535. [DOI] [PubMed] [Google Scholar]
- 6.Young T.J., Rossberg M.I., Hutchins G.M. Volume of air in a lethal venous air embolism. Anesthesiology. 2001:94360–94361. doi: 10.1097/00000542-200102000-00031. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Compilation of diagnostic and therapeutic dry arthroscopy. A full dry diagnostic arthroscopy is shown, in addition to a dry assessment of stability in a patient with chronic global instability, as well as a dry osteocapsular release in a patient with osteoarthritis.