Abstract
Tibial tuberosity transfer is a well-established procedure in the treatment of patellar instability and in selected cases of anterior knee pain. Several techniques have been advocated in the literature. Some of the common complications associated with this procedure have been pain and discomfort due to prominent screw heads, necessitating their removal; nonunion and delayed union of the osteotomy; and failure of fixation. Tibial fractures have also been reported in some case reports. We present our technique of tibial tuberosity transfer using two 4-mm cannulated screws for stabilization of the tuberosity fragment. We have used this technique either for isolated tibial tuberosity transfer or as part of a combined procedure along with medial patellofemoral ligament reconstruction in treating patellar instability. Using this technique, we have encountered no patients with wound problems, nonunion, delayed union, or loss of fixation and only 1 patient with a metal work problem needing a second procedure for its removal. We attribute our good outcomes to the preservation of the soft-tissue attachments to the tuberosity fragment; minimal soft-tissue dissection, which allows rapid bony consolidation of the osteotomy, which in turn allows accelerated rehabilitation; and the use of 4-mm cannulated screws for fixation of the osteotomy, minimizing the potential for metal work problems.
Patellofemoral malalignment can manifest as patellofemoral pain or acute and recurrent instability.1 Malalignment of the patellofemoral complex can be caused by deficiency of the medial patellofemoral ligament complex, trochlear dysplasia, patella alta, or an increased tibial tubercle–trochlear groove distance. Medialization of the tibial tuberosity is a powerful tool to control patellofemoral mechanics.2, 3, 4, 5 Normalization of an increased tibial tuberosity–trochlear groove distance by medialization of the tibial tuberosity is used in the treatment of recurrent patellar instability and lateral patellar overload syndromes. Hauser6 in 1938 first described tibial tuberosity transfer, popularized later by Fulkerson et al.7 There have been various modifications since its first description.8 Tibial tuberosity transfer, though considered a straightforward procedure, can lead to major and minor complications.9, 10 Our technique incorporates subtle modifications in terms of the way tibial tubercle osteotomy is performed and use of cannulated screws for fixing the osteotomy, thus minimizing the risk of complications (Table 1, Table 2).
Table 1.
Pearls and Pitfalls for Modified Technique of Tibial Tuberosity Transfer
| Pearls |
| The skin incision should be positioned either slightly medial to the tibial tuberosity (when combining tibial tuberosity transfer with MPFL reconstruction) or lateral to the tibial tuberosity (when performing isolated tibial tuberosity transfer). |
| Internal rotation of the foot facilitates proper orientation of the osteotomy. |
| The distal soft-tissue attachments of the tuberosity fragment should always be preserved. |
| To create a smooth surface, the surgeon should avoid creating a step at the proximal end of the osteotomy. |
| Releasing the fat pad from the patellar tendon undersurface facilitates medialization of the tibial tuberosity fragment. |
| The posterior cortex should only be scored by the cannulated drill. |
| The surgeon should add 4 mm to the actual measured length for the cannulated screw. |
| Pitfalls |
| Placing the incision too lateral or too medial can lead to excessive soft-tissue dissection. |
| Performing the osteotomy with the foot externally rotated can lead to the plane of the osteotomy being downsloping. |
| Severance of the distal soft-tissue attachments of the tuberosity fragment can lead to proximal migration of the fragment, leading to patella alta. |
| Breaching the posterior cortex with the cannulated drill will lead to the guidewire backing out along with the drill. |
MPFL, medial patellofemoral ligament.
Table 2.
Surgical Steps for Modified Technique of Tibial Tuberosity Transfer
| 1. Position the patient supine with the operative knee held in 45° of flexion by a foot roll and side support. |
| 2. Make a vertical skin incision slightly lateral or medial to the tibial tuberosity prominence. |
| 3. Make a stab incision at the inferolateral border of the patella, and extend it proximally by 1 cm. |
| 4. Using a blade, mark the line of osteotomy, which is just anterior to the anterolateral-compartment muscles. |
| 5. Internally rotate the leg, and perform the osteotomy with an oscillating saw, starting proximally and angling the blade upward at the distal extent. |
| 6. Elevate the tuberosity fragment with an osteotome, taking care to maintain the distal soft-tissue attachments. |
| 7. Release the patellar tendon from the fat pad. |
| 8. With the knee in extension, medialize the tuberosity fragment. |
| 9. Pass 2 parallel guidewires for 4-mm cannulated screws under image guidance. |
| 10. Measure the length, and add 4 mm to it. |
| 11. Pass the cannulated drill over the guidewires until the posterior tibial cortex is scored but not breached. |
| 12. Pass the cannulated screws over the guidewires with a washer. |
Surgical Technique
The patient is positioned supine on the operating table, and general anesthesia is instituted. A tourniquet is applied to the ipsilateral proximal thigh; side support and a foot roll are used to hold the knee in approximately 45° of flexion (Fig 1, Video 1). A self-adherent waterproof U-drape (Steri-Drape, 120 cm × 130 cm; 3M Health Care, St. Paul, MN) is applied just proximal to the tourniquet to seal off the tourniquet area. A single dose of prophylactic antibiotic is administered at the time of induction. The surgeon positions himself or herself on the same side as the operative knee. The surgical area is prepared and draped in standard surgical fashion. The image intensifier is positioned on the side opposite the operative limb. A longitudinal skin incision of approximately 6 to 7 cm is made over the tibial tuberosity, with a tendency to keep it just slightly lateral to the tuberosity prominence (Fig 2) when performing an isolated tibial tuberosity transfer or slightly medial when performing a combined tibial tuberosity transfer and medial patellofemoral ligament reconstruction. The skin and subcutaneous tissues are undermined minimally to expose the lateral edge of the patellar tendon and lateral aspect of the tibial tuberosity. A small incision is made at the inferolateral border of the patella (Fig 3) and extended in a proximal direction by 1 cm. The distal line of the osteotomy is marked by sharp dissection with a blade just anterior to the anterior-compartment muscles (Fig 3). The foot is brought into internal rotation, and the osteotomy progresses in the same oblique plane (as seen from an axial view) as the tibial tuberosity. Internal rotation of the foot allows for easier orientation of the blade and subsequent osteotomy to prevent the distal aspect of the blade from veering toward the internal surface of the proximal anteromedial tibial cortex and sliding along it. The lateral edge of the patellar tendon helps identify the lateral-most edge of the tuberosity, which is where the osteotomy is begun. The tibial tuberosity osteotomy is carried out using an oscillating blade (De Soutter blade, 46 × 15 × 0.9 mm; De Soutter Medical, Aylesbury, England) (Fig 4, Video 1). This is performed from the lateral side alone. At the distal end, the saw blade is angled slightly upward to exit the anterior cortex (Fig 4, Video 1). The osteotomy is completed using the saw; however, at no point are the soft tissues distally or medially dissected or severed. A half-inch Lambotte osteotome is used to break off some of the bony bridges that have not been addressed with the saw blade (Fig 5, Video 1). It is important to note proximally that the osteotomy does not create a step with the anterior tibial slope, and the transition here should remain as smooth as possible.
Fig 1.
A left knee, side view, after preparation and positioning in approximately 45° of flexion.
Fig 2.
A vertical skin incision is made either just medial to the tuberosity prominence (for a combined medial patellofemoral ligament and tibial tuberosity transfer) or lateral to the tuberosity prominence (for isolated tibial tuberosity transfer).
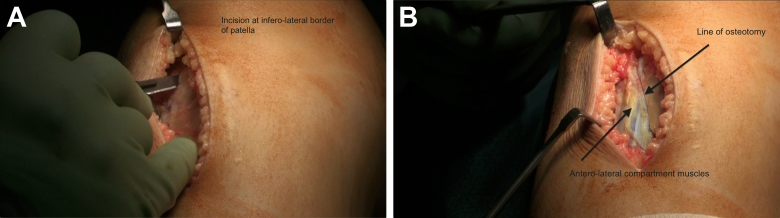
Fig 3.
The line of osteotomy is marked, starting at the inferolateral border of the patella and extending distally, just anterior to the anterolateral-compartment muscles, with a blade.
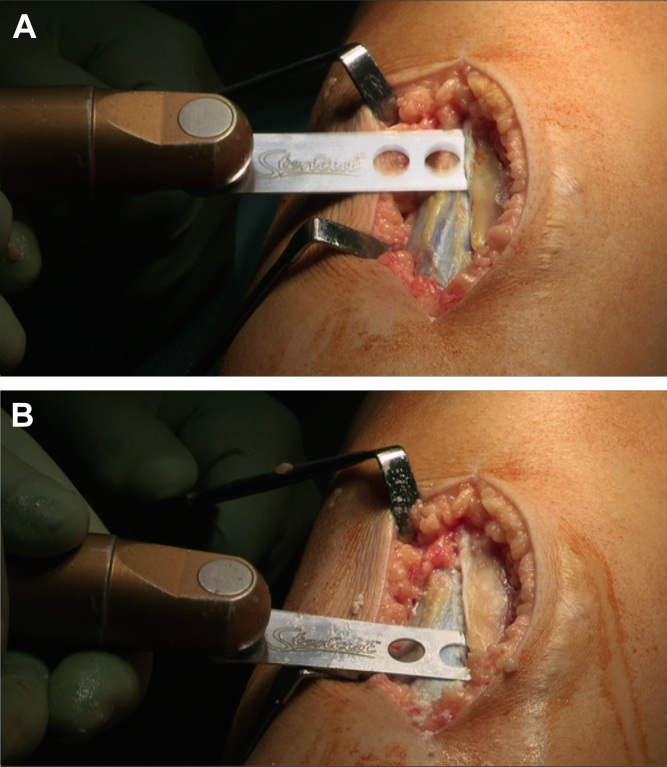
Fig 4.
With the foot internally rotated, osteotomy is performed using an oscillating saw, and at the distal end, the saw blade is angled upward to exit the anterior cortex.
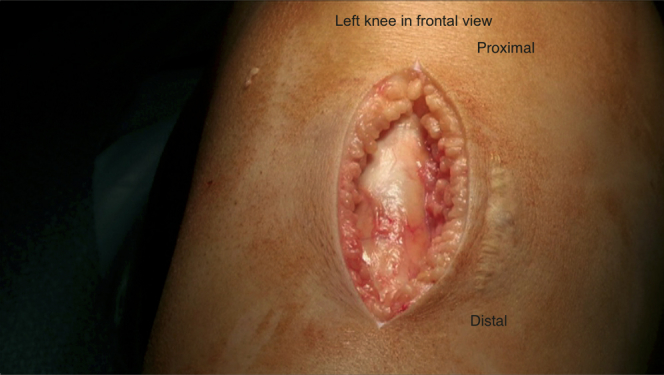
Fig 5.

The surgeon uses an osteotome to elevate the tuberosity fragment, gently maintaining the soft-tissue attachments distally.
The tuberosity is gently elevated. The osteotomy in its proximal portion can be medialized up to 12 mm, and the osteotomy plane will naturally allow for some anteriorization. To facilitate medialization and to achieve biomechanical offloading of the lateral patellofemoral joint, the distal undersurface of the patellar tendon needs to be released from the Hoffa pad (Video 1). This is best performed with the knee in extension; its effect is certainly more appreciably noticed in this position. Along with this, an extra synovial inferolateral release is performed. This is performed through the same incision under direct vision. The soft-tissue sleeve distally, which is where the patellar tendon fibers meet the periosteum of the tibial crest, provides soft-tissue stability to the osteotomy and should be preserved when possible. Once the desired medialization of the tuberosity is achieved, 2 guidewires (1.25 mm; Synthes, Oberdorf, Switzerland) are placed parallel to the posterior tibial slope of the proximal tibia and parallel to each other (Fig 6, Video 1). The position of the guidewires is checked under the image intensifier. The cannulated drill is advanced over the guidewire. Drilling is stopped once the far cortex is reached, with care taken not to penetrate the far cortex. The osteotomy is secured with two 4.0-mm cannulated screws (Synthes) with washers (Video 1). This is performed under image intensifier control. We release the tourniquet at this stage, check for bleeders, and secure hemostasis. We infiltrate the subcutaneous tissues with an appropriate volume of local anesthetic. Skin closure is performed with No. 3-0 Monocryl subcuticular sutures (Ethicon, Somerville, NJ).
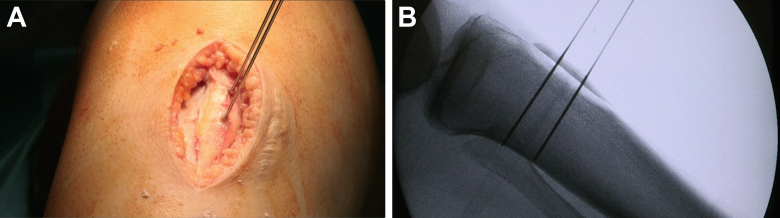
Fig 6.
The tuberosity fragment is medialized and held in position by two 4-mm cannulated screw guidewires placed in a parallel manner.
Discussion
Tibial tuberosity medialization is a well-established surgical strategy in the management of patellofemoral instability and patellofemoral lateral pain syndrome. For patellofemoral instability, distal realignment by medialization of the tibial tuberosity is usually combined with proximal soft-tissue surgery in the form of either a lateral release and medial reefing or reconstruction of the medial patellofemoral ligament.11 Tibial tuberosity transfer, although a straightforward procedure, can result in major complications such as proximal tibial fractures.9, 10 Koeter et al.9 reported that 29 of the 60 patients (48%) in their series needed removal of screws because of symptoms from prominent screws. Warner et al.12 compared the fixation strengths of two 4.5-mm screws and three 3.5-mm screws and concluded that both fixation methods are comparable in terms of failure strength but smaller, 3.5-mm screws may reduce the need for hardware removal related to prominence and soft-tissue irritation. In our series of 25 patients (27 knees, 2 bilateral) with a minimum follow-up period of 18 months, we have seen no major complications and only 1 patient with problems with the screws used for fixation of the osteotomy. Two patients had hypersensitive scars. We attribute our low complication rate to the minimally invasive nature of our technique, preserving the soft-tissue attachments to the tubercle fragment, and the use of 4-mm partially threaded cannulated screws, which are low profile but give stable fixation, allowing accelerated rehabilitation.
The advantages of our technique include the following: Hamstring grafts can be taken through the same skin incision if one is performing a medial patellofemoral ligament reconstruction at the same time; due to the plane of the osteotomy, medialization and anteriorization of the tuberosity are achieved simultaneously; and maintenance of the distal soft-tissue attachments to the tuberosity fragment will prevent inadvertent proximal or distal migration. Moreover, because the screws used are cannulated, temporary stabilization of the tuberosity fragment is provided by the guidewires for the screws, and the smaller diameter and profile of the 4-mm cannulated screws, as compared with large fragment screws, decrease the risk of splitting the tuberosity fragment, as well as irritation from prominent screw heads. The main limitation of this technique is that because the distal soft-tissue attachments are preserved, the tuberosity fragment cannot be brought down if one wishes to correct patella alta.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Tibial tuberosity transfer in a left knee, with the patient lying supine, with 4-mm cannulated screws used for tuberosity fragment fixation.
References
- 1.Insall J. “Chondromalaciae patellae” patellar malalignment syndrome. Orthop Clin North Am. 1979;10:117–127. [PubMed] [Google Scholar]
- 2.Fulkerson J.P. Anteromedialization of the tibial tuberosity for patellofemoral malalignment. Clin Orthop Relat Res. 1983;(177):176–181. [PubMed] [Google Scholar]
- 3.Trillat A., Dejour H., Couette A. Diagnosis and treatment of recurrent dislocations of the patella. Rev Chir Orthop Reparatrice Appar Mot. 1964;50:813–824. [in French] [PubMed] [Google Scholar]
- 4.Caton J.H., Dejour D. Tibial tubercle osteotomy in patello-femoral instability and in patellar height abnormality. Int Orthop. 2010;34:305–309. doi: 10.1007/s00264-009-0929-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lane J., Karnatzikos G., Gobbi A. Elmslie-Trillat procedure: A distal-based procedure for patellar stabilization. In: Gobbi A., Espregueira Mendes J., Nakamura N., editors. The patellofemoral joint: State of the art in evaluation and management. Springer; New York: 2014. pp. 155–160. [Google Scholar]
- 6.Hauser E.D.W. Total tendon transplant for slipping patella. Surg Gynecol Obstet. 1938;66:199–214. [Google Scholar]
- 7.Fulkerson J.P., Becker G.J., Meaney J.A. Anteromedial tubercle transfer without bone graft. Am J Sports Med. 1990;18:490–496. doi: 10.1177/036354659001800508. [DOI] [PubMed] [Google Scholar]
- 8.Servien E., Verdonk P., Neyret P. Tibial tuberosity transfer for episodic patellar dislocation. Sports Med Arthrosc. 2007;15:61–67. doi: 10.1097/JSA.0b013e3180479464. [DOI] [PubMed] [Google Scholar]
- 9.Koeter S., Diks M.J.F., Anderson P.G., Wymenga A.B. A modified tibial tubercle osteotomy for patellar maltracking. J Bone Joint Surg Br. 2007;89:180–185. doi: 10.1302/0301-620X.89B2.18358. [DOI] [PubMed] [Google Scholar]
- 10.Luhmann S.J., Fuhrop S., O’Donnell J.C., Gordon J.E. Tibial fractures after tibial tubercle osteotomies for patellar instability: A comparison of three osteotomy configurations. J Child Orthop. 2011;5:19–26. doi: 10.1007/s11832-010-0311-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang C.J., Chan Y.S., Chen H.H. Factors affecting the outcome of distal realignment for patellofemoral disorders of the knee. Knee. 2005;12:195–200. doi: 10.1016/j.knee.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 12.Warner B.T., Kamath G.V., Spang J.T., Weinhold P.S., Creighton R.A. Comparison of fixation methods after anteromedialization osteotomy of the tibial tubercle for patellar instability. Arthroscopy. 2013;29:1628–1634. doi: 10.1016/j.arthro.2013.06.020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tibial tuberosity transfer in a left knee, with the patient lying supine, with 4-mm cannulated screws used for tuberosity fragment fixation.