Abstract
Hip arthroscopy serves as both a diagnostic and therapeutic tool for the management of various conditions that afflict the hip. This article reviews the basics of hip arthroscopy by demonstrating supine patient positioning, fluoroscopic evaluation of the hip under anesthesia, and sterile preparation and draping. Careful attention to detail during the operating theater setup ensures adequate access to the various compartments of the hip to facilitate the diagnosis of disease and treatment with minimally invasive arthroscopy. Furthermore, having a routine method for patient positioning and operative setup improves patient safety, as well as operative efficiency, as the operative team becomes familiar with the surgeon's standard approach to hip arthroscopy cases.
Hip arthroscopy is gaining more popularity as both a diagnostic and therapeutic procedure performed by orthopaedic surgeons.1, 2, 3 The number of arthroscopic hip procedures has increased 6-fold based on the number of reported hip arthroscopies performed by American Board of Orthopaedic Surgery Part II examinees over the 5-year period from 2006 through 2010.4 Indications for hip arthroscopy have also expanded since Burman's first description of the procedure in 1931.5 Modern hip arthroscopy can address focal chondromalacia, labral tears, septic arthritis, synovial chondromatosis, hip instability, osteochondritis dissecans, femoroacetabular impingement, ischiofemoral impingement, removal of loose bodies, ligamentum teres injuries, and snapping hip syndrome, as well as other hip diseases.6, 7, 8, 9, 10
This article and Video 1 review the operating theater setup for hip arthroscopy, in particular supine patient positioning, positioning of the arms, application of traction, dynamic fluoroscopic evaluation of the hip under anesthesia, and sterile preparation and draping. Proper positioning of the patient on the operating table allows for efficient access to the deep-seated hip joint and facilitates surgical intervention during arthroscopy.
Surgical Technique
The patient is brought to the operating theater and transferred to the operating table after appropriate patient identification and safety measures, such as marking of the patient in the preoperative holding room by the surgeon (Table 1). Time-out procedures are performed to ensure patient safety. Typically, general anesthesia with paralysis is induced to facilitate relaxation, and regional methods of anesthesia, such as spinal, epidural, or lumbar plexus blocks, may be used concomitantly for adjuvant postoperative pain control. Hip arthroscopy has been described with the patient in both the lateral position and the supine position; however, at our institution, we prefer supine positioning for hip arthroscopy and will focus on this positioning method in this article and in Video 1. Our anesthesia colleagues also prefer supine patient positioning to facilitate intraoperative anesthetic care during hip arthroscopy. In addition, the anesthesia team is made aware preoperatively of our preference to keep the mean arterial pressure lower than or equal to about 65 mm Hg, when this can be safely accomplished based on various patient factors. Keeping the mean arterial pressure lower than the arthroscopic pump pressure and using epinephrine in the arthroscopic irrigation solution aid in intraoperative arthroscopic visualization. The anesthesia team maintains normothermia throughout the case using warmed intravenous saline solution and the Bair Hugger warming system (3M, St Paul, MN).11, 12 Warmed arthroscopic solution may also be protective against intraoperative hypothermia, but this option is not used at our institution.13
Table 1.
Potential Pearls and Pitfalls for Supine Positioning for Hip Arthroscopy
| Positioning pearls |
| Perform a safety time-out before surgical positioning per institutional protocol. |
| Position patients the same way every time to avoid variability. |
| Ensure that operating room staff know and understand equipment preferences. |
| Place instruments in a similar position to avoid case-to-case variability. |
| Positioning pitfalls |
| Excessive continuous traction can lead to lateral femoral cutaneous nerve neurapraxia, as can inappropriate portal placement. |
| A known risk, due to inadequate perineal post padding, is pudendal nerve neurapraxia. |
| Hip flexion >20° may result in sciatic nerve injury. |
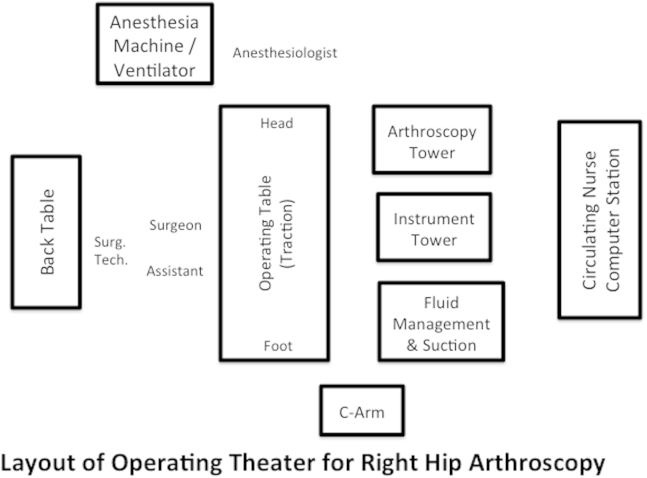
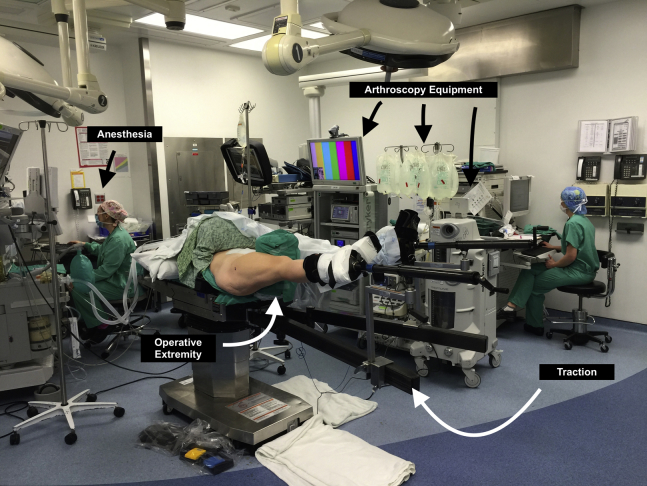
The operating theater setup is shown in Figure 1. The arthroscopic monitors, fluid management system, fluoroscopy/C-arm (OEC Fluoro Scanner; GE Healthcare, Salt Lake City, UT), operating device units such as radiofrequency, and arthroscopic shaver stations should be positioned on the contralateral side, or opposite the surgical side. The surgeon, surgical assistant, and surgical technologist, along with the back primary instrument table and Mayo stand, are positioned on the ipsilateral, operative side. There should be sufficient room for the circulating nurse to access the foot of the fracture table. Intraoperative manipulation of the operative extremity with the addition or subtraction of traction, limb abduction and adduction, and flexion and extension of the hip is necessary for gaining access to the various portions of the intra-articular and extra-articular hip joint.
Fig 1.
Operative theater setup for right-sided hip arthroscopy. The locations of various instruments and equipment in the operating theater are shown. The surgeon, assistants, and instrumentation are located on the operative (right) side of the patient. The arthroscopy tower and associated equipment are located on the contralateral (left) side of the patient. (Surg Tech, surgical technologist.)
After general anesthesia is induced, a Foley catheter is placed to decompress and relax the bladder during traction and hip manipulation. The Foley catheter is secured to the patient's abdomen and taken off the head of the operative table so that the anesthesiologist may monitor urine output. Ocular lubrication, additional intravenous access, and placement of additional monitors, as well as other protective anesthesia measures, can be undertaken at this time. A radiofrequency grounding pad is also placed at this time on the operative side of the abdomen. A compression stocking is placed on the contralateral lower extremity to prevent deep vein thrombosis.
Next, the patient's bilateral feet and ankles are placed into commercially available foam-padded boots (Philippon Hip; Bledsoe, Grand Prairie, TX) (Fig 2, Table 2). After the foam-padded boots are secured, with care taken to ensure that no wrinkles are present, the patient is brought down on the standard fracture table (Amsco Orthovision; Steris, Le Haillan, France) or standard operating table with traction attachment and lateralized to the ipsilateral, operative side to facilitate full access to the operative hip. Movement of the patient is coordinated with the anesthesia staff to ensure that the endotracheal tube is secure and with the nursing and operative room staff, as well as the surgeon, to ensure the safety of the patient and the surgical operating room team. The patient's buttocks will need to be positioned at the edge of the table to facilitate application of traction against a well-padded commercially available post (Bledsoe [padding] and Amsco Orthovision [post]) that is positioned toward the operative side, which is placed after initial positioning is performed (Fig 3). More details regarding the post and application of traction will be reviewed later in this article.
Fig 2.
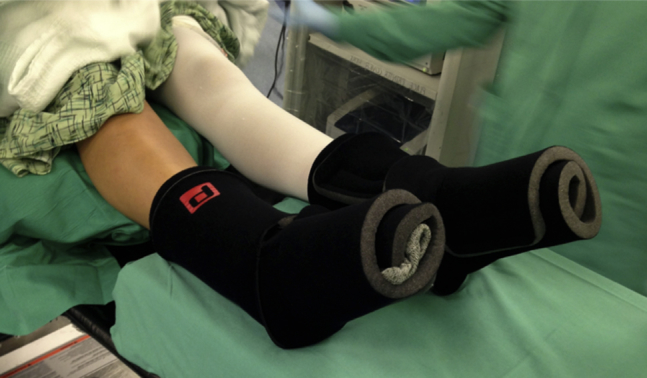
Bilateral feet after placement of commercially available foam-padded boots for right hip arthroscopy. The contralateral (left) leg is depicted with a compression hose to prevent deep vein thrombosis. The ipsilateral, operative (right) leg does not have a compression hose. Care is taken to avoid wrinkles while applying the foam-padded boots to prevent decubitus ulcers.
Table 2.
Quick Reference for Hip Arthroscopy Procedure Setup
| Recommendations | |
|---|---|
| Padding of bony prominences | Foam padding, feet and ankles in traction boots, and blankets placed on ipsilateral arm |
| Ipsilateral upper extremity | Placement across patient's body (flexion <90°), with pulse oximetry, papoose wrapping, and safety belt |
| Contralateral upper extremity | Arm board (shoulder abducted <60°, elbow flexion <20°) and IV access |
| Perineal post | Lateralized to operative side—contact with medial thigh (check for genital compression) |
| Foot and ankle | Traction boots |
| Fluoroscopy | 45° lateral Dunn view, ROM, and vacuum crescent sign |
| Operative hip | 15° of flexion and 0° of adduction before application of traction |
| Ipsilateral foot | Internal rotation of 10°-15° |
| Contralateral lower extremity | Delicate countertraction (10-20 lb [4.5-9 kg]) |
IV, intravenous; ROM, range of motion.
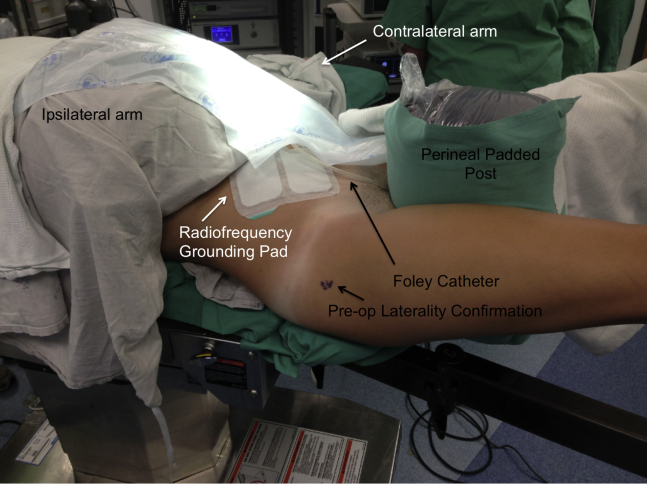
Fig 3.
Positioning of operative right hip after placement into traction boots and positioning of perineal padded post for right hip arthroscopy. The arms have been positioned so that the ipsilateral (right) arm is placed over the patient and is well padded, and a papoose wrapping has been applied. The contralateral (left) arm is placed on a standard arm board. The perfusion of both upper extremities is confirmed after positioning. The positioning of the Foley catheter and the radiofrequency grounding pad is also shown.
The upper extremity ipsilateral to the operative side is positioned away from the operative field by bringing it across the patient's body. We allow for our anesthesia colleagues to ensure that placement of their monitors and intravenous access are adequate throughout the positioning of the upper extremities. The ipsilateral arm is brought over folded blankets and foam padding. The ipsilateral upper extremity is not flexed past 90° at the elbow to prevent ischemia and to facilitate circulation. A pulse oximeter is placed on the ipsilateral upper extremity to monitor oxygen saturation to the upper extremity. Then, a draw sheet is folded, with care taken to ensure that there are no wrinkles in the papoose wrapping, and the arm and patient are secured with a safety belt to fix the upper extremity and patient to the operative table. The contralateral upper extremity is positioned on an arm board with padding of the bony prominences and peripheral nerves. In addition, we recommend abduction of the contralateral shoulder of no more than 60° and contralateral elbow flexion of 20°. By allowing the contralateral arm to be free, the anesthesia team is able to gain access to the extremity during the operative procedure throughout the case (Fig 3). Before further positioning is performed, we confirm adequate intravenous flow into the upper extremities.
Attention is then turned toward final positioning adjustment and traction application (Table 3). The perineal post is placed in a lateralized position toward the operative side with the perineum against the padded post, with contact of the medial thigh of the operative hip allowing for controlled lateralization of the femur. The use of a commercially available oversized perineal post that ranges in diameter from 9 to 12 cm is preferred because such posts have been associated with a lower risk of pudendal neurapraxia (Figs 3 and 4).14, 15 After the post is placed and the patient is moved into position against the post, the genitalia and scrotum should be checked to ensure that they are not compressed. The bilateral padded feet and ankles can then be placed in the traction boots and secured with Velcro straps and tape. The pelvis and torso are stabilized by application of gentle countertraction of about 10 to 20 lb (4.5 to 9 kg) on the contralateral lower extremity. Then, the operative extremity is tested in the traction boot by bringing it into full flexion, extension, abduction, and adduction.
Table 3.
Traction Tips
| Place the operative hip in 15° of flexion and 0° of adduction before application of traction. |
| Monitor the amount of total traction time. |
| Grossly apply manual traction. |
| Typically, use 25-50 lb (11-23 kg) to achieve adequate joint distraction. |
| Apply gentle countertraction on the contralateral extremity. |
Fig 4.
Positioning of patient in traction before sterile preparation and draping for right hip arthroscopy. The operative hip is positioned at 15° of flexion and 0° of adduction before the application of traction. Internal rotation of the foot to 10° to 15° positions the femoral neck more parallel to the operative horizon.
The C-arm fluoroscopic machine is brought into the operative field, and a 45° lateral Dunn view is obtained. The operative leg is taken through a range of motion under fluoroscopy. These dynamic hip assessments aid in the surgical planning for femoroacetabular impingement resection and osteoplasty during arthroscopic surgery. The operative hip is positioned at 15° of flexion and 0° of adduction before the application of traction. Internal rotation of the foot to 10° to 15° positions the femoral neck more parallel to the operative horizon (Fig 4). We avoid excessive hip flexion during positioning and application of traction to relieve pressure on the sciatic nerve.
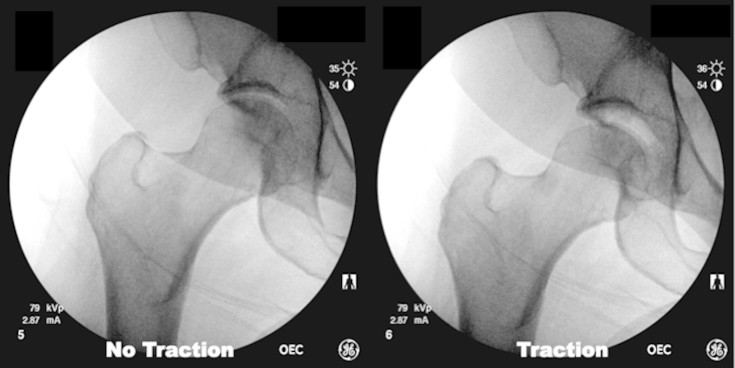
With adequate muscle paralysis, traction should be gently applied under fluoroscopic guidance. Carefully monitoring the amount of total traction time is critical to avoid adverse events related to excessive and lengthy traction times. The amount of traction force required is patient specific and dependent on the patient's pathologic condition—typically, arthritic joints require more traction—but most patients require from 25 to 50 lb (11 to 23 kg) to achieve adequate joint distraction to gain access to the central hip compartment. Manual traction is grossly applied by locking the boot into the sliding rail, followed by fine traction through the rotating handle attached to the boot. Providing gross traction first ensures that the amount of distraction does not exceed the limitations of the traction device. The appearance of a vacuum crescent sign under fluoroscopy confirms that traction is adequate (Fig 5). If the surgeon is unable to attain the vacuum crescent sign and bony distraction, 2 options are available. The patient can be prepared and draped sterilely, and the joint can then be vented with a spinal needle to break the suction seal of the femoroacetabular joint. Alternatively, the surgeon can continue to add gentle traction until the crescent sign appears by relaxation through physiological creep and ligamentotaxis. Of note, we have found that bony distraction of the hip joint without a vacuum crescent sign is indicative of 3 specific pathologic conditions: hemarthrosis, synovial chondromatosis, and pigmented villonodular synovitis. Traction is then maintained during sterile preparation and draping of the operative field.
Fig 5.
Fluoroscopic views of the right hip before and after application of traction, confirming adequate distraction of the hip joint through the appearance of the crescent sign. If the surgeon is unable to attain the vacuum crescent sign, the joint can be vented with a spinal needle to break the suction seal or the surgeon can continue to add gentle traction until the crescent sign appears.
We prefer the use of prepackaged stick sterile preparation (DuraPrep Surgical Solution; 3M). Then, the sterile field is isolated and draped with adhesive sterile rectangular sheets. If the patient is allergic to iodine, a sticky, clear, adhesive sheet is first applied to the operative field (Steri-Drape Incise Drape; 3M). A sterile “shower-curtain” clear drape with an arthroscopic fluid collection pocket and associated drain is then used (Steri-Drape with Isolation Drape and Incise Film and Pouch; 3M). A final sterile drape is placed on the patient's upper body and used as a curtain isolating the anesthesia staff from the surgical field.
Discussion
Hip arthroscopy is valuable for the diagnosis of various hip disorders and allows for operative therapeutic intervention. Several steps are critical in patient positioning. The upper extremities should be positioned away from the surgical field but still permit adequate perfusion and intravenous access. The surgeon should be comfortable with fracture table operation and aware of potential pressure injuries that result from improper positioning. One of the most significant injuries is pudendal nerve palsy from excessive pressure from the perineal post. Preoperative fluoroscopic evaluation ensures that adequate distraction is possible before preparation and draping of the extremity. During final surgical sterile preparation and draping, care should be taken to isolate the surgical field while maintaining a sufficient field for access to all joint compartments.
The vacuum force between the femoral head and acetabulum related to the labral seal has been described as between 120 and 200 N, with distraction forces of 200 lb (90 kg) necessary for initial distraction.16, 17 Venting the joint or injecting normal saline solution with joint distention can aid in breaking the suction seal and facilitate distraction across the hip joint; in some instances these forces are reduced to 50 lb (23 kg).18, 19 The complications related to excessive traction force or the duration of the applied traction are well documented and include, but are not limited to, pudendal neurapraxia, sciatic nerve injury, lower-extremity skin compromise, and genital injury.9, 10, 20, 21, 22, 23
Optimal surgical outcomes after hip arthroscopy hinge on many factors, including safe, reproducible positioning of the patient on the operating table for optimal surgical intervention. Proper patient positioning requires the assistance and skilled expertise of the entire operating room team, including the surgeon, surgical assistants, nursing staff, surgical technologists, and anesthesia staff. A surgical team that is acquainted with the positioning and sterile preparation for hip arthroscopy will aid in the efficiency of the operative procedure and minimize risk to the patient.
Footnotes
The authors report the following potential conflict of interest or source of funding: S.M. receives support from Wake Forest Innovations Spark Award for development of rotator cuff repair device, and Orthopaedic Research and Education Foundation Resident Clinician Scientist Award. A.J.S. receives support from Smith & Nephew Endoscopy, Bauerfeind, and Johnson & Johnson.
Supplementary Data
Supine patient positioning for arthroscopy of right hip: operating room setup and padding of feet and ipsilateral arm for positioning on fracture table, dynamic fluoroscopic assessment, application of traction, and finally, sterile preparation and draping.
References
- 1.Colvin A.C., Harrast J., Harner C. Trends in hip arthroscopy. J Bone Joint Surg Am. 2012;94:e23. doi: 10.2106/JBJS.J.01886. [DOI] [PubMed] [Google Scholar]
- 2.Larson C.M., Stone R.M. Current concepts and trends for operative treatment of FAI: Hip arthroscopy. Curr Rev Musculoskelet Med. 2013;6:242–249. doi: 10.1007/s12178-013-9170-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Montgomery S.R., Ngo S.S., Hobson T. Trends and demographics in hip arthroscopy in the United States. Arthroscopy. 2013;29:661–665. doi: 10.1016/j.arthro.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Bozic K.J., Chan V., Valone F.H., III, Feeley B.T., Vail T.P. Trends in hip arthroscopy utilization in the United States. J Arthroplasty. 2013;28(suppl):140–143. doi: 10.1016/j.arth.2013.02.039. [DOI] [PubMed] [Google Scholar]
- 5.Burman M.S. Arthroscopy or the direct visualization of joints: An experimental cadaver study. 1931. Clin Orthop Relat Res. 2001;(390):5–9. doi: 10.1097/00003086-200109000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Howse E.A., Wooster B.M., Mannava S., Perry B., Stubbs A.J. Arthroscopic treatment of slipped capital femoral epiphysis screw impingement and concomitant hip pathology. Arthrosc Tech. 2014;3:e515–e517. doi: 10.1016/j.eats.2014.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stabile K.J., Neumann J.A., Mannava S., Howse E.A., Stubbs A.J. Arthroscopic treatment of bucket-handle labral tear and acetabular fracture. Arthrosc Tech. 2014;3:e283–e287. doi: 10.1016/j.eats.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stubbs A.J., Andersen J.S., Mannava S. Arthroscopic hip labral repair: The Iberian suture technique. Arthrosc Tech. 2014;3:e351–e354. doi: 10.1016/j.eats.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shetty V.D., Villar R.N. Hip arthroscopy: Current concepts and review of literature. Br J Sports Med. 2007;41:64–68. doi: 10.1136/bjsm.2006.027755. (discussion 68) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kowalczuk M., Bhandari M., Farrokhyar F. Complications following hip arthroscopy: A systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1669–1675. doi: 10.1007/s00167-012-2184-2. [DOI] [PubMed] [Google Scholar]
- 11.Sardesai A., Hujazi I., Khanduja V. Surgical access warming blanket to prevent hypothermia after hip arthroscopy. Arthroscopy. 2012;28:1045–1046. doi: 10.1016/j.arthro.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 12.Parodi D., Tobar C., Valderrama J. Hip arthroscopy and hypothermia. Arthroscopy. 2012;28:924–928. doi: 10.1016/j.arthro.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 13.Parodi D., Valderrama J., Tobar C. Effect of warmed irrigation solution on core body temperature during hip arthroscopy for femoroacetabular impingement. Arthroscopy. 2014;30:36–41. doi: 10.1016/j.arthro.2013.08.035. [DOI] [PubMed] [Google Scholar]
- 14.Kong K.F., Chien P., Wong J.W., Yip D.K. Peroneal padding: An alternative to a peroneal post in hip arthroscopy. Arthroscopy. 2003;19:1027–1029. doi: 10.1016/j.arthro.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 15.Byrd J.W. Hip arthroscopy utilizing the supine position. Arthroscopy. 1994;10:275–280. doi: 10.1016/s0749-8063(05)80111-2. [DOI] [PubMed] [Google Scholar]
- 16.Dienst M., Seil R., Godde S. Effects of traction, distension, and joint position on distraction of the hip joint: An experimental study in cadavers. Arthroscopy. 2002;18:865–871. doi: 10.1053/jars.2002.36120. [DOI] [PubMed] [Google Scholar]
- 17.Byrd J.W., Chern K.Y. Traction versus distension for distraction of the joint during hip arthroscopy. Arthroscopy. 1997;13:346–349. doi: 10.1016/s0749-8063(97)90032-3. [DOI] [PubMed] [Google Scholar]
- 18.McCarthy J.C. Hip arthroscopy: Applications and technique. J Am Acad Orthop Surg. 1995;3:115–122. doi: 10.5435/00124635-199505000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Eriksson E., Arvidsson I., Arvidsson H. Diagnostic and operative arthroscopy of the hip. Orthopedics. 1986;9:169–176. doi: 10.3928/0147-7447-19860201-07. [DOI] [PubMed] [Google Scholar]
- 20.Gupta A., Redmond J.M., Hammarstedt J.E., Schwindel L., Domb B.G. Safety measures in hip arthroscopy and their efficacy in minimizing complications: A systematic review of the evidence. Arthroscopy. 2014;30:1342–1348. doi: 10.1016/j.arthro.2014.04.103. [DOI] [PubMed] [Google Scholar]
- 21.Harris J.D., McCormick F.M., Abrams G.D. Complications and reoperations during and after hip arthroscopy: A systematic review of 92 studies and more than 6,000 patients. Arthroscopy. 2013;29:589–595. doi: 10.1016/j.arthro.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 22.Dippmann C., Thorborg K., Kraemer O., Winge S., Hölmich P. Symptoms of nerve dysfunction after hip arthroscopy: An under-reported complication? Arthroscopy. 2014;30:202–207. doi: 10.1016/j.arthro.2013.11.014. [DOI] [PubMed] [Google Scholar]
- 23.Telleria J.J., Safran M.R., Harris A.H., Gardi J.N., Glick J.M. Risk of sciatic nerve traction injury during hip arthroscopy—Is it the amount or duration? An intraoperative nerve monitoring study. J Bone Joint Surg Am. 2012;94:2025–2032. doi: 10.2106/JBJS.K.01597. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supine patient positioning for arthroscopy of right hip: operating room setup and padding of feet and ipsilateral arm for positioning on fracture table, dynamic fluoroscopic assessment, application of traction, and finally, sterile preparation and draping.