Abstract
This study examined psychological distress, parenting stress and family functioning in female caregivers of adolescents undergoing bariatric surgery compared to caregivers of adolescents with extreme obesity not undergoing surgery across the first post-operative year. Female caregivers of 16 adolescents undergoing RYGBP (Mage = 16.6 years; MBMI = 66.2 kg/m2; 94% recruitment) and 28 comparison adolescents who had sought behavioral weight management (Mage = 16.2 years; MBMI = 46.3 kg/m2; 90% recruitment) completed measures of psychological distress (SCL90-R), parenting stress (SIPA), and family functioning (FAD) at baseline/pre-surgery, 6- and 12-months. Caregiver and adolescent anthropometrics were obtained. At baseline, clinical cut-offs were exceeded by 29.5% of caregivers for psychological distress, 31.8% for family dysfunction, and 13.2% for parenting stress. Linear Mixed Modeling indicated that bariatric adolescents had a significantly greater BMI at baseline than comparison adolescents (t = −7.79, p < .001) with a substantial reduction by 12-months relative to the nearflat trajectory of comparisons (t = 20.32, p < .001). No significant group differences at baseline or group trajectory differences were identified for any caregiver or family variable. Initial findings suggest caregivers of adolescents with extreme obesity present with limited dysfunction and that bariatric surgery has no impact on caregiver distress, parenting stress, or family functioning across the first post-operative year. Larger samples and longer-term follow-up will allow examination of what role caregiver/family factors play in adolescent post-operative outcomes.
The early and impressive evidence for the safety, short-term efficacy, and associated psychosocial improvements of bariatric surgery for the adolescent patient1–4 will likely contribute to an increasing adolescent surgical volume over time. However, unlike adult care models, the practice of pediatric medicine proves unique due to the presence and influence of caregivers5. Accordingly, caregivers of adolescents undergoing bariatric surgery are seen as critical to providing the adolescent with emotional and instrumental social support, including the facilitation of their adherence to the post-operative medical and lifestyle regimen. However, no empirical literature to date characterizes the caregivers or families of adolescents undergoing surgical weight management or whether caregiver or family functioning changes over time following surgery.
The present study was informed by several cross-sectional studies that described families presenting to non-surgical multidisciplinary weight management programs. These studies indicated that the majority (66–90%) of female caregivers of treatment-seeking obese youth were also obese (BMI > 30 kg/m2)6–8 as well as self-reported clinical levels of psychological distress (28–50%)7–9, elevated levels of parenting stress (18%)10 and problematic family functioning7. Thus, the family environment may be characterized not only by a shared disease (obesity), but potentially, dysfunction. Furthermore, the broader pediatric literature demonstrates an association between impaired caregiver and family functioning and poorer treatment outcomes in pediatric conditions reliant on regimen adherence, lifestyle change, and/or treatment intensity (i.e., surgery)11–14. These data are concerning when applied to adolescent bariatric surgery, an intensive weight loss intervention.
In the current study, we examined levels of psychological distress, parenting stress and family dysfunction at baseline/pre-surgery for female caregivers of adolescents undergoing Roux-en-Y gastric bypass (RYGBP) as compared to comparison caregivers of adolescents with extreme obesity not undergoing surgery. We hypothesized caregiver/family functioning to be impaired for both groups at baseline, with no group differences in the number of caregivers exceeding clinical cut-offs. We also examined caregiver/family functioning over the same course of time (baseline/pre-surgery, 6- and 12-months post-operatively). Based on the expected treatment efficacy (i.e., significant adolescent BMI change following RYGBP), we hypothesized that bariatric caregivers would report differing trajectories for psychosocial distress, parenting stress, and family dysfunction, relative to the non-operative comparison group, for which little to no change in adolescent weight would be expected over time., Specifically, bariatric caregivers may experience improved psychosocial health with their child’s weight loss, or there may be an increase in parenting demands with regard to the adolescent’s medical care and lifestyle change.
Methods
The present investigation utilized data from a prospective, controlled, longitudinal study observing psychosocial adjustment and family functioning of adolescents undergoing RYGBP at a large Midwestern pediatric hospital, a non-operative comparison group of extremely obese adolescents (BMI ≥ 40), and their respective female caregivers. The current study examined female caregiver self-report of psychological distress, parenting stress, and family functioning at pre-surgery/baseline, and at 6- and 12- months post-surgery. We chose to focus on female caregivers because they typically serve as the health-managing parent attending surgical weight loss program appointments. Moreover, our previous work demonstrated that female and not male caregivers of treatment-seeking obese youth report greater psychological distress and family dysfunction7. Institutional Review Board approval was obtained.
Participants and Procedures
Study inclusion criteria required all participants to be 14–17 years of age, with no physical impairments unrelated to obesity, or developmental disability due to the high reading demand of the study. For the bariatric group, RYGBP candidacy was based on patient selection guidelines15, with participants only approached for study inclusion after achieving clinical and insurance approval for RYGBP. Of the 17 eligible consecutive patients, 16 (94%) adolescent/caregiver dyads agreed to participate. Adolescents underwent surgery between July 2005 and January 2007. Data were obtained at all time points for 94% of the bariatric sample, with 1 dyad completing only 2 time points. Potential comparison adolescents meeting inclusion criteria and their caregivers were either recruited consecutively when initiating treatment at a behavioral weight management clinic, or had previously initiated treatment and had recently participated in one of the first author’s other studies16, 17. Of the 31 eligible comparison families, 28 (90%) dyads agreed to participate. Data were obtained at all time points for 79% of the comparison cohort with 3 dyads completing only 2 time points.
At each time-point, caregivers completed measures independently with trained staff available for assistance. Data were primarily collected in clinical research space. To minimize burden and promote retention, follow-up data collection also occurred in locations convenient for the family (i.e., home setting) at 6- (27.5%) and 12-months (25.7%).
Measures
Caregivers completed a questionnaire assessing caregiver and family demographics, including information to determine family socioeconomic status (SES) using the Revised Duncan, an occupation-based measure of SES18, 19.Adolescent and caregiver height and weight were measured by research staff using a calibrated stadiometer and digital scale. Participants were measured in street clothing without shoes and measurements were taken in triplicate, with the means used to calculate BMI (kg/m2).
Caregiver distress was assessed with the Global Severity Index (GSI) from the Symptom Checklist-90-Revised (SCL-90-R), a 90-item self-report measure of a broad range of current psychological symptoms.20 The GSI combines information on the number and intensity of symptoms present. Psychological distress in the clinical range is indicated with a GSI total score or two primary dimension scores ≥ 63. For the current sample, internal consistency for the GSI was good (α = 0.98). Parenting stress was measured using the Parent Domain (SIPA-PD) from the Stress Index for Parents of Adolescents™ (SIPA™)21, a 112-item self-report for caregivers of youth ages 11–19 years. The SIPA-PD is calculated from 4 sub-scales: Life Restrictions, Relationship with Spouse/Partner, Social Alienation, and Incompetence/Guilt. Higher scores represent greater parenting stress, and corresponding percentile scores are categorized as: normative (< 85th percentile); borderline (85th –89th); clinically significant (90th – 94th); and clinically severe (95th–100th). The SIPA-PD is psychometrically sound, and internal consistency within the current sample was good (α = 0.92). Finally, caregiver perceptions of family functioning were assessed using General Functioning Scale of the McMaster Family Assessment Device (FAD)22, a 60-item self-report questionnaire. Within the current sample, internal consistency for this scale was good (α = 0.95).
Data Analyses
Two-tailed independent Student’s t tests compared the bariatric and comparison groups on baseline demographic variables. Instrument derived clinical cut-off scores for caregiver psychological distress, parenting stress, and family dysfunction were calculated to examine clinical elevations at baseline. Given the small sample size, Fisher’s Exact tests compared groups exceeding clinical cut-offs.
Growth curve analysis examined change over time and possible differences between caregiver groups for psychological distress, parenting stress, family functioning, and adolescent BMI. The growth curves were specified within the context of linear mixed models (LMM) with random effects for intercepts and slopes23. Each LMM had parameters for group intercept differences and group trajectory differences. Graphs of mean values suggested a possible nonlinear relationship. Given there were only three time points, the transformation log(month+1) was used in all analyses as this provides for nonlinear but monotonic growth curves with fewer parameters than a quadratic polynomial model24. We assumed the random effects have a joint-normal distribution with zero means, the random error has a normal distribution with zero mean, and the random error and random effects are independent. Group was dummy coded as 0 = bariatric and 1 = comparison. Each model was fit separately for each response variable using restricted maximum likelihood estimation. The multi-parameter null hypothesis was tested first based on a likelihood ratio chi-squared statistic.
Results
Baseline demographic and anthropometric data are presented in Table 1. Adolescents were primarily female, with the comparison group having a higher percentage of African American adolescents (57.1%) relative to the bariatric group (18.8%). No significant group differences were identified for caregiver or family demographic variables. For bariatric caregivers, 6.7% were classified as overweight (BMI ≥ 25 kg/m2; n = 1), 40.0% obese (n = 6), and 46.7% extremely obese (n = 7). For comparison caregivers, 10.7% were classified as overweight (n = 3), 46.4% obese (n = 13), and 39.3% extremely obese (n = 11).
Table 1.
Caregiver, Adolescent, and Family Demographic Characteristics at Pre-surgery/Baseline.
| Bariatric (n=16) | Comparison (n=28) | ||||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | % | Range | Mean (SD) | % | Range | ||
| Caregivers | Agea | 46.3 (4.7) | 32.0–59.0 | 40.4 (6.0) | 31.0–50.0 | ||
| Educationa | 13.2 (2.7) | 8–18 | 13.4 (1.7) | 10–16 | |||
| BMI (kg/m2) | 40.6(11.1) | 22.7–65.8 | 39.0 (9.0) | 20.6–65.1 | |||
| Adolescents | Agea | 16.6 (1.2) | 14.4–18.4 | 16.2 (1.2) | 13.7–17.9 | ||
| BMI (kg/m2) | 66.2 (12.0) | 48.6–88.8 | 46.3 (4.7) | 39.4–57.8 | |||
| Gender | 69% female | 64% female | |||||
| Family | Single Parent | 37.5% (n=6) | 42.9% (n=12) | ||||
| Children in household | 2.1 (0.8) | 1–3 | 2.3 (1.3) | 1–7 | |||
| SESb | 44.7 (23.9) | 15.0–87.9 | 38.5 (19.6) | 15.0–83.7 | |||
Note.
Age and education are in years;
Socioeconomic status; Based upon Duncan TSEI2 for head of household, a measure of occupational attainment.
Means and standard deviations for all outcome variables across time are provided in Table 2. Using Fisher’s Exact Tests, no significant differences in number of caregivers exceeding clinical cut-offs were identified at baseline between groups for psychological distress (12.5% bariatric, 39.3% comparison, p = .09); family dysfunction (25.0% bariatric, 35.7% comparison, p = .52); or parenting stress (16.7% bariatric, 11.5% comparison, p = .64).
Table 2.
Adolescent BMI, Caregiver Adjustment and Family Functioning Means and Standard Deviations at Baseline/Pre-Surgery (T1) and at 6 Months (T2) and 12 Months (T3) Post-Surgery.
|
Bariatric (n=16) M±SD |
Comparison (n=28) M±SD |
|||||
|---|---|---|---|---|---|---|
| Scale/Timepoint | T1 | T2 | T3 | T1 | T2 | T3 |
| Adolescent BMI | 66.24±12.0 | 45.82±9.9 | 41.11±9.6 | 46.25±4.7 | 47.09±4.9 | 46.45±4.7 |
| Psychological Distressa | ||||||
| Global Severity Index | 53.25±9.5 | 49.94±12.0 | 52.40±12.4 | 55.96±12.4 | 54.33±11.2 | 54.52±13.4 |
| Parenting Stressb | ||||||
| Parent Domain | 53.33±24.9 | 50.00±21.5 | 45.31±20.8 | 54.15±22.8 | 52.50±24.0 | 50.87±23.9 |
| Family Functioningc | ||||||
| General Functioning | 1.58±0.4 | 1.64±0.6 | 1.65±0.5 | 1.84±0.5 | 1.81±0.4 | 1.82±0.5 |
Note.
Caregiver distress based on Symptom Checklist-90-Revised; T-scores are reported in the table but all analyses were completed using raw scores;
Stress Index for Parents of Adolescents; Percentile scores are reported in the table but all analyses were completed using raw scores;
McMaster Family Assessment Device.
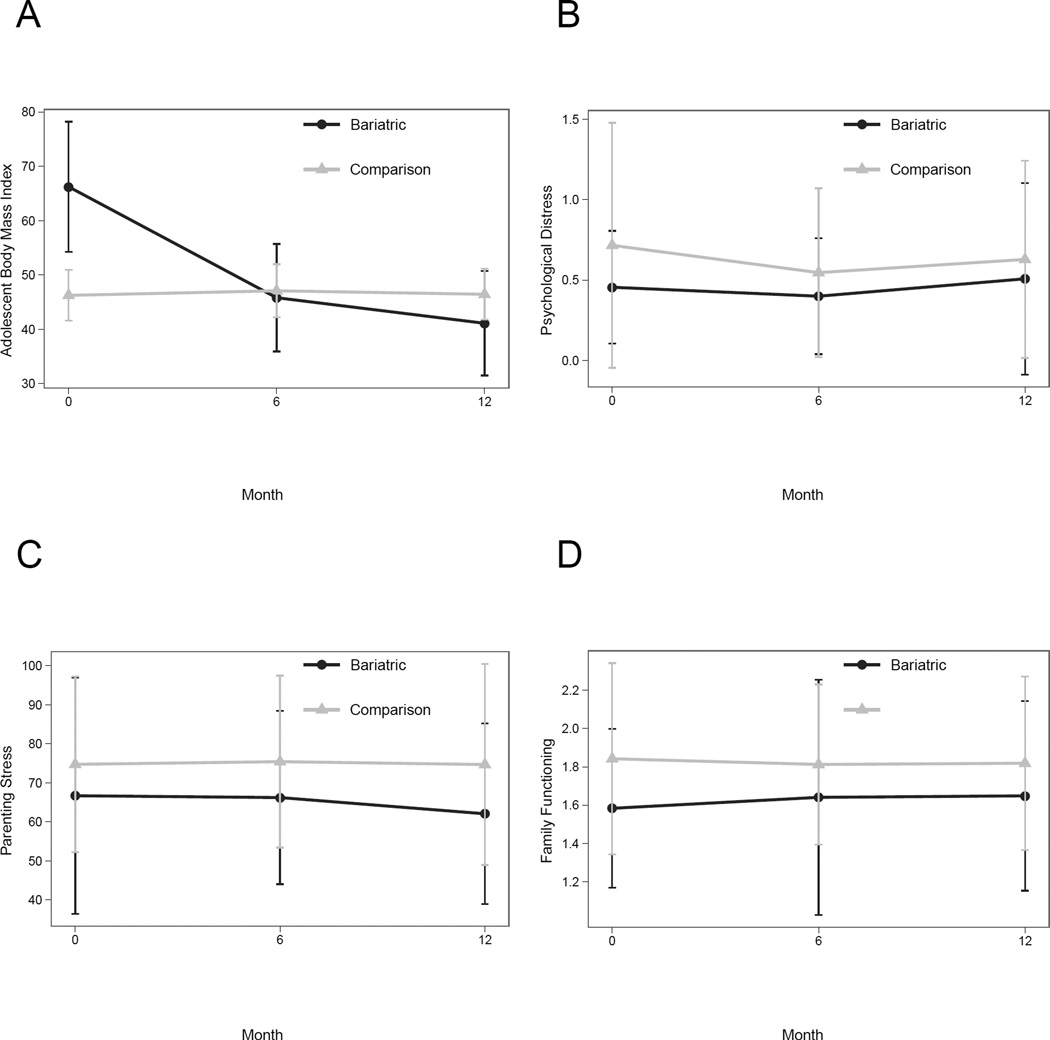
As expected, weight trajectories differed for bariatric adolescents relative to comparisons (Figure 1). For bariatric adolescents, the mean change in BMI from baseline to 12-months was −25.1 kg/m2 (n=15), representing a mean BMI loss of 38%; for comparison adolescents, the mean BMI change was +0.20 kg/m2 (n=23). LMM analysis demonstrated the omnibus test of global treatment effect was statistically significant, χ2(2) = 105.81, p < .0001. Bariatric adolescents had a significantly greater BMI at baseline than comparison adolescents (t = −7.79, p < .001) with a significant group by time interaction effect (t = 20.32, p < .001). This indicates the bariatric group had a strong nonlinear decrease in BMI over time, with a rapid deceleration from baseline to 6-months and a slower deceleration from 6- to 12-months, relative to the near flat trajectory of the comparison group.
Figure 1.
Group Differences (± one standard error) for Adolescent Body Mass Index(A), Caregiver Psychological Distress (B), Parenting Stress (C), and Family Functioning (D) Across the First Post-operative Year.
LMM analyses examined change in caregiver and family functioning over time for groups of caregivers (see Figure 1). The multi-parameter chi-squared test of group effects for each outcome variable indicated no significant differences between groups at baseline or group trajectory differences over time, with essentially flat trajectories for all variables for both groups: psychological distress (χ2(2) = 1.79, p = .41), parenting stress (χ2(2) = 1.89, p = .39), and family functioning (χ2(2) = 3.02, p = .22).
Discussion
The present study provides important preliminary insight into the families of adolescents with extreme obesity undergoing weight loss surgery. Findings suggest caregivers of adolescents with extreme obesity present with limited dysfunction and that bariatric surgery has no significant impact on caregiver psychosocial status or perception of family functioning across the first post-operative year. Based on the extant pediatric obesity literature, we did not anticipate the low levels of caregiver and family dysfunction reported. While not statistically significant, only a small percentage of bariatric caregivers (12.5%) met criteria for “caseness” for psychological distress relative to comparison caregivers (39.3%) at baseline, suggesting less impairment for female caregivers whose adolescents undergo choose bariatric surgery.
As anticipated, the overwhelming majority (86%) of female caregivers were obese themselves, if not extremely obese (47% BMI > 40 kg/m2). While the adult literature has demonstrated a strong family history for extreme obesity among adult family members25, the present data speak to a multi-generational trend for obesity to progress to extreme levels by adolescence. Interestingly, post hoc analyses for the current study revealed that, of those caregivers who were not extremely obese at the time of their adolescent’s surgery, 25% had undergone bariatric surgery within the previous 3 years, with another caregiver undergoing bariatric surgery between the adolescent’s 6- and 12-month post-operative visits. Thus, bariatric surgery may emerge as a family weight loss tool. While it is accepted that there is a genetic component in a family’s transmission of obesity, there is also an undeniable environmental component that maintains adolescent obesity (e.g., food availability within the home, family meal structure/planning, cultural preferences, engagement in exercise)26, 27. Thus, without considerable change at the family level, an adolescent must function within a family environment that has contributed to their pre-surgery health and psychosocial impairment. Having a caregiver who has also undergone bariatric surgery may present unique benefits and/or challenges for the adolescent patient.
A major strength of the current study is our prospective, longitudinal and controlled design. Although representative of our clinical population and surgical volume during the study time period, these data represent a single adolescent bariatric program. In addition, it remains unknown whether these caregiver and family characteristics are unique to families who seek weight management treatment for their extremely obese adolescent as compared to those not accessing care. Replication of these findings utilizing a larger sample drawn from multiple clinical sites is ongoing through the Teen-Longitudinal Assessment of Bariatric Surgery (Teen-LABS) Consortium28 and associated ancillary studies. This work includes follow-up to the 24-month post-operative time-point and will be adequately powered to examine interactions with family demographics (e.g., single-parent status, SES) and caregiver weight and bariatric surgery history, as well as expand the focus to include additional family contexts (e.g., social support, caregiver presence and connectedness, abuse and neglect) which may account for individual variation in adolescent BMI and psychosocial change post-surgery.
Conclusion
An adolescents’ health and well-being is significantly impacted by their interactions within the contexts of their daily lives (e.g., family, peers).29, 30 To fully understand the impact of adolescent bariatric surgery on their physical and psychosocial health, we must examine an adolescent’s interactions within these age-salient contexts. The present data provide evidence of the short-term effectiveness of RYGBP for significant weight loss which parallels our previous research demonstrating significant psychosocial improvement over the same time4. In the context of these considerable changes for the adolescent, the present data suggest that caregiver and family functioning does not change over time or with adolescent surgical weight loss. As demand increases for adolescent surgical programs and additional surgical procedures (e.g., laparoscopic adjustable gastric band, sleeve gastrectomy), the pre- and post-operative care of adolescents will be informed by understanding which, if any, caregiver or family factors would improve (or sustain) adolescent weight loss and psychosocial outcomes.
Acknowledgements
This research was funded by a grant from the National Institutes of Health awarded to the M.H.Z. (R03 DK0788901). We thank Christina Ramey, Lindsay Wilson, Kate Grampp, Ashley Morgenthal, and Faye Riestenberg for assistance with data collection and participant retention efforts.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Inge TH, Jenkins TM, Zeller MH, et al. Baseline BMI is a strong predictor of nadir BMI following adolescent gastric bypass. J Ped. 2010;156:103–108e101. doi: 10.1016/j.jpeds.2009.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sugerman HJ, Sugerman EL, DeMaria EJ, et al. Bariatric surgery for severely obese adolescents. J Gastrointest Surg. 2003;7:102–107. doi: 10.1016/S1091-255X(02)00125-7. [DOI] [PubMed] [Google Scholar]
- 3.O'Brien PE, Sawyer SM, Laurie C, et al. Laparoscopic adjustable gastric banding in severely obese adolescents: A randomized trial. JAMA. 2010;303:519–536. doi: 10.1001/jama.2010.81. [DOI] [PubMed] [Google Scholar]
- 4.Zeller MH, Modi AC, Noll JG, Long JD, Inge TH. Psychosocial functioning improves following adolescent bariatric surgery. Obesity. 2009;17:885–890. doi: 10.1038/oby.2008.644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Academy of Pediatrics. Family Pediatrics: Report of the Task Force on the Family. Pediatrics. 2003;111:1541–1571. [PubMed] [Google Scholar]
- 6.Modi AC, Guilfoyle SM, Zeller MH. Impaired health-related quality of life in caregivers of youth seeking obesity treatment. J Pediatr Psychol. 2009;34:147–155. doi: 10.1093/jpepsy/jsn070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeller MH, Reiter-Purtill J, Modi AC, Gutzwiller J, Vannatta K, Davies WH. Controlled study of critical parent and family factors in the obesigenic environment. Obesity. 2007;15:126–136. doi: 10.1038/oby.2007.517. [DOI] [PubMed] [Google Scholar]
- 8.Janicke DM, Marciel KK, Ingerski LM, et al. Impact of psychosocial factors on quality of life in overweight youth. Obesity. 2007;15:1799–1807. doi: 10.1038/oby.2007.214. [DOI] [PubMed] [Google Scholar]
- 9.Zeller MH, Saelens BE, Roehrig H, Kirk S, Daniels S. Psychological adjustment of obese youth presenting for weight management treatment. Obes Res. 2004;12:1576–1586. doi: 10.1038/oby.2004.197. [DOI] [PubMed] [Google Scholar]
- 10.Guilfoyle SM, Zeller MH, Modi AC. Parenting stress impacts obesity-specific health-related quality of life in a pediatric obesity treatment-seeking sample. J Dev Behav Pediatr. 2010;31:17–25. doi: 10.1097/DBP.0b013e3181c73641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duke DC, Geffken GR, Lewin AB, Williams LB, Storch EA, Silverstein JH. Glycemic Control in Youth with Type 1 Diabetes: Family Predictors and Mediators. J Pediatr Psychol. 2008;33:719–727. doi: 10.1093/jpepsy/jsn012. [DOI] [PubMed] [Google Scholar]
- 12.Lewin AB, Heidgerken AD, Geffken GR, et al. The relation between family factors and metabolic control: The role of diabetes adherence. J Pediatr Psychol. 2006;31:174–183. doi: 10.1093/jpepsy/jsj004. [DOI] [PubMed] [Google Scholar]
- 13.Gerson AC, Furth SL, Neu AM, Fivush BA. Assessing associations between medication adherence and potentially modifiable psychosocial variables in pediatric kidney transplant recipients and their families. Pediatric Transplantation. 2004;8:543–550. doi: 10.1111/j.1399-3046.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- 14.Stone D, Banerjee M, Dupuis J, Leleszi J, Allasio D, Singh TP. Association of parental pretransplant psychosocial assessment with post-transplant morbidity in pediatric heart transplant recipients. Pediatric Transplantation. 2006;10:602–607. doi: 10.1111/j.1399-3046.2006.00543.x. [DOI] [PubMed] [Google Scholar]
- 15.Inge TH, Krebs NF, Garcia VF, et al. Bariatric surgery for severely overweight adolescents: Concerns and recommendations. Pediatrics. 2004;114:217–223. doi: 10.1542/peds.114.1.217. [DOI] [PubMed] [Google Scholar]
- 16.Zeller MH, Modi AC. Predictors of health-related quality of life in obese youth. Obes Res. 2006;14:122–130. doi: 10.1038/oby.2006.15. [DOI] [PubMed] [Google Scholar]
- 17.Kolotkin RL, Zeller MH, Modi AC, et al. Assessing weight-related quality of life in adolescents. Obesity. 2006;14:448–457. doi: 10.1038/oby.2006.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stevens G, Featherman DL. A revised socioeconomic index of occupational status. Soc Sci Res. 1981;10:364–395. [Google Scholar]
- 19.Nakao K, Treas J. The 1989 Socioeconomic Index of Occupations: Construction from the 1989 Occupational Prestige Scores. Chicago: University of Chicago, National Opinion Research Center; 1992. [Google Scholar]
- 20.Derogatis LR. SCL-90-R: Administration, scoring, and procedures. Towson (MD): Clinical Psychometric Research; 1983. [Google Scholar]
- 21.Sheras PL, Abidin RR. Stress Index for Parents of Adolescents (SIPA) Odessa, FL: Psychological Assessment Resources, Inc.; 1998. [Google Scholar]
- 22.Epstein N, Baldwin L, Bishop D. The McMaster Family Assessment Device. Journal of Marital and Family Therapy. 1983;9:171–180. [Google Scholar]
- 23.Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. New York: Wiley; 2004. [Google Scholar]
- 24.Long JD, Ryoo J. Using fractional polynomials to model non-linear trends in longitudinal data. British Journal of Mathematical and Statistical Psychology. doi: 10.1348/000711009X431509. (in press). [DOI] [PubMed] [Google Scholar]
- 25.Crerand CE, Wadden TA, Sarwer DB, et al. A comparison of weight histories in women with class III vs. class I–II obesity. Surg Obes Relat Dis. 2006;2:165–170. doi: 10.1016/j.soard.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 26.Kral TVE, Faith MS. Influences on child eating and weight development form a behavioral genetics perspective. J Pediatr Psychol. 2009;34:596–605. doi: 10.1093/jpepsy/jsn037. [DOI] [PubMed] [Google Scholar]
- 27.Golan M, Crow S. Parents are key players in the prevention and treatment of weight-related problems. Nutr Rev. 2004;62:39–50. doi: 10.1111/j.1753-4887.2004.tb00005.x. [DOI] [PubMed] [Google Scholar]
- 28.Inge TH, Zeller MH, Harmon C, et al. Teen-Longitudinal Assessment of Bariatric Surgery: methodological features of the first prospective multicenter study of adolescent bariatric surgery. J Pediatr Surg. 2007;42:1969–1971. doi: 10.1016/j.jpedsurg.2007.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Call KT, Riedel AA, Hein K, McLoyd V, Petersen A, Kipke M. Adolescent health and well-being in the twenty-first century: A global perspective. J Res Adolescence. 2002;12:69–98. [Google Scholar]
- 30.Eccles JS, Lord SE, Roeser RW, Barber BL, Jozefowicz DMH. The association of school transitions in early adolescence with developmental trajectories through high school. In: Schulenberg J, Maggs JM, Hurrelmann K, editors. Health risks and developmental transitions during adolescence. Cambridge, U.K.: Cambridge University Press; 1997. pp. 283–320. [Google Scholar]