Abstract
Carcinoma of the cervix is the second to fourth most common malignancy in women. It metastasizes most often to the lungs, bones, and liver. Skin involvement originating from cervical cancer is rare, even in the terminal stages of the disease. Cutaneous metastasis of cervical cancer usually presents as cutaneous nodules, papules/plaques, maculopapular rash, and diffuse inflammatory rash. We report a rare case (only the second reported case to the best of our knowledge) of a 50-year-old woman with cutaneous metastasis in form of fungating ulcerative growth on mons pubis as presenting feature of carcinoma cervix.
Keywords: Carcinoma cervix, cutaneous metastasis, genital ulcer, vulva
What was known?
Cervical carcinoma is one of the most common malignancies in women
Cutaneous metastasis of carcinoma cervix is a rare and late stage entity
Most common modes of presentation of skin metastasis of carcinoma cervix are nodules, papules, plaques, maculopapular, and diffuse inflammatory rash.
Introduction
Carcinoma cervix is the second to fourth most common malignancy in women.[1,2] It metastasizes most often to lungs, bones and liver; but cutaneous metastasis is rare, even in terminal stages of the disease.[1,3]
We report a rare case of a 50-year-old woman with cutaneous metastasis in the form of fungating ulcerative growth on mons pubis as presenting feature of carcinoma cervix, (Level of evidence III).
Case Report
A 50-year-old postmenopausal female presented to dermatology clinic of Government Medical College with complaints of skin lesions on genitalia with pain in vulval region, and dyspareunia for 6 months; and yellowish-white foul smelling discharge per-vaginum for past 2–3 months. Neither she nor her spouse had a history suggestive of high-risk behavior or sexually transmitted infection (STI).
Cutaneous examination revealed two ulcers on mons pubis with fungating edge and deep center with slough [Figure 1]. The vulva was edematous and erythematous and was firm to woody hard and tender on palpation. Bilateral inguinal lymph nodes were palpable, soft, discrete, and nontender. There was no evidence of STI.
Figure 1.

Two fungating ulcers with deep centre containing slough on mons pubis; vulva erythematous and edematous
Per-speculum examination showed fungating growth involving cervix, and anterior vaginal wall which bled on touch and cervix was eaten up [Figure 2]. Other systemic examinations revealed no significant abnormality. Clinical differential diagnoses were carcinoma cervix Stage IIB with cutaneous metastasis; granuloma inguinale or lymphogranuloma venereum (ruptured inguinal bubo) in an immunocompromised case.
Figure 2.

Fungating growth involving cervix and anterior vaginal wall on per-speculum examination
On investigation, her hemoglobin was 9 g%; her complete blood count and urine routine-microscopy were within normal limits. Serum creatinine was 4.5 mg%, blood urea 109 mg%, serum bilirubin 0.4 mg%; and serum HIV and serum venereal disease research laboratory were negative.
Incision biopsy from cervix was suggestive of large cell keratinizing squamous cell carcinoma (SCC) [Figures 3 and 4]. Incision biopsy from the edge of the ulcer in mons pubis showed epidermal proliferation with fairly well circumscribed deeper border. The proliferation consisted of thickened branching and coalescing rete ridges. The keratinocytes showed individual cell keratinization and formation of horn pearls with incompletely keratinizing centers. The epidermal proliferation showed crowding of keratinocytes with nuclear pleomorphism and altered nuclear, cytoplasmic ratio with increased mitotic figures above the basal layer. The dermo-epidermal junction was not well-maintained. The dermis showed moderately dense lympho-histiocytic infiltrate. This was suggestive of fairly well-differentiated SCC [Figures 5 and 6].
Figure 3.
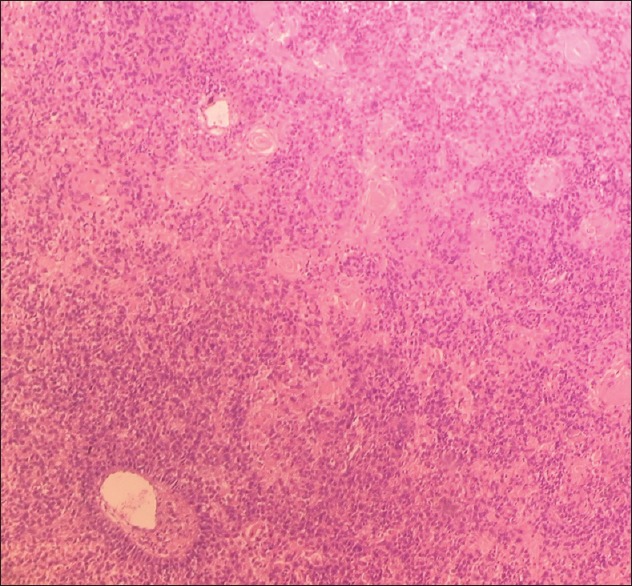
Histopathological examination of tissue specimen from cervix. (H and E, ×10)
Figure 4.
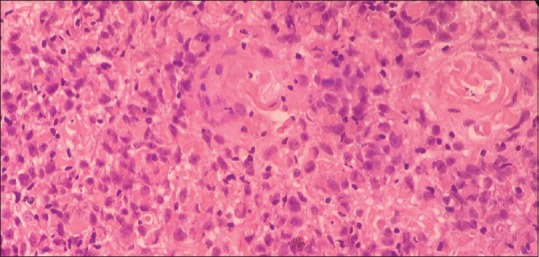
Histopathological examination of tissue specimen from cervix. (H and E, ×40)
Figure 5.
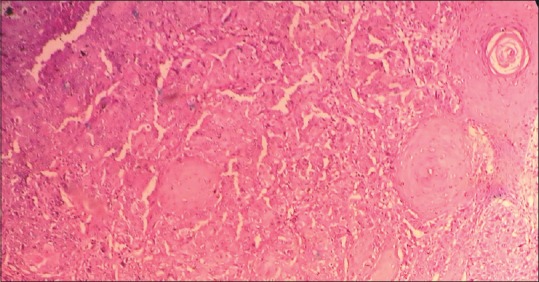
Histopathological examination of tissue specimen from edge of ulcer on mons pubis. (H and E, ×10)
Figure 6.
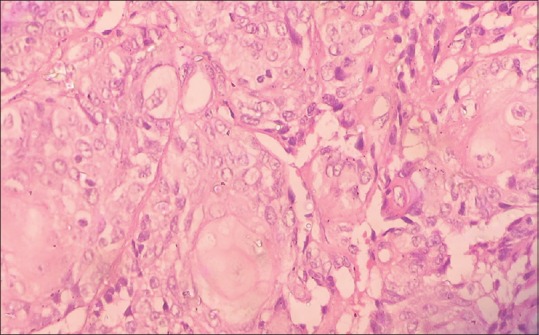
Histopathological examination of tissue specimen from edge of ulcer on mons pubis. (H and E, ×40)
Chest X-ray (posterioranterior-view), to rule out any metastasis, was normal. Ultrasonography abdomen and pelvis showed mild hydronephrosis in right kidney.
Final diagnosis was cutaneous metastasis of SCC cervix International Federation of Gynecology and Obstetrics (FIGO) clinical Stage IIIB[4] (carcinoma is Stage IIIB when tumor extends to pelvic wall and/or causes hydronephrosis or nonfunctioning kidney[4]) for which patient was admitted.
In 15 days of presentation, patient developed incontinence of urine and her serum creatinine raised to 11 mg% and blood urea to 194 mg%. Suprapubic cystostomy and radiotherapy for carcinoma was planned. But patient absconded and was lost to follow-up.
Discussion
Cutaneous metastasis to cervical carcinoma is rare (0.01–2%).[3] In an Indian study by Ayyamperumal et al. on 750 internal malignancy patients with 35% women, cervical carcinoma was third most common malignancy (16.66%) among women but no case of cutaneous metastasis was observed.[5] Skin metastasis is found in 0.8% in Stage I, in Stage II (1.2%), Stage III (1.2%) and Stage IV carcinoma cervix cases (4.8%). Most commonly involved sites on the skin are an abdominal wall, vulva, anterior chest wall and lower extremity.[2,6] After an extensive literature search, only one other case presenting with multiple genital ulcers subsequently proven to be cutaneous metastasis to SCC cervix was reported.[7]
Agrawal et al. reviewed 47 cases documented in Medline and EMBASE database from 1996 to 2008 of cervical cancer with cutaneous metastasis; histopathological patterns found were SCC (63.8%), adenocarcinoma (10.6%), and poorly or undifferentiated carcinoma (4.2%)[1] (while others observed adenocarcinoma and undifferentiated carcinoma cervix have higher incidence of skin metastasis than SCC[2,6]). At the time of presentation, the average age was 52 years (23–79 years) and most common FIGO clinical stage was Stage IIIB. Average interval between diagnosis and appearance of cutaneous metastasis based on stage was 37.6 months (Stage I), 20.8 months (Stage II), 24.9 months (Stage III) and 3.4 months (stage IV). Most frequent presenting cutaneous symptoms were cutaneous nodules (55.3%), plaques (10.6%), maculopapular rash (8.5%), and diffuse inflammatory rash (4.2%).[1]
Primarily, cervical carcinoma spreads through a direct local extension to paracervical tissue and pelvic organs (viz., vagina, pelvic wall, urinary bladder, and rectum) and lymphatic embolization.[1,4] Hematogenous dissemination and distant metastasis are rare. The probable mechanism of cutaneous metastasis is an alteration of the lymphatic flow. The deep lymphatic pathways are obstructed by tumor resulting in shunting of the lymphatic flow to the cutaneous lymphatics.[1,6]
Skin metastasis is usually associated with generalized dissemination, locoregional recurrence, and rapidly progressive disease process that signals poor prognosis[8,9] (average reported survival 3[8]–8.5[2,6] months). There is no effective treatment. Only palliative treatment can be given in the form of extirpation of skin lesion, followed by radiotherapy or chemotherapy.[1,6]
Conclusion
The present case is rare and unique. The mode of presentation was two fungating ulcers on mons pubis with comparatively silent FIGO Stage III B carcinoma cervix. This is the second such case reported to the best of our knowledge. This led the patient to approach dermatology rather than gynecology outpatient department and the lesions unless thoroughly checked could easily be misdiagnosed as sexually transmitted genital ulcer disease. This was typically a case of late diagnosis due to delayed presentation. Lack of awareness on patient's side and private nature of disease prevented the early diagnosis of the disease which is a fairly common occurrence in our country.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
What is new?
Ulcer as a presenting feature of skin metastasis of cervical carcinoma is a rare phenomenon
Fungating vulval ulcer being the mode of presentation of otherwise comparatively silent carcinoma cervix is unusual; and thus should be kept among differential diagnoses in genital ulcer diseases.
References
- 1.Agrawal A, Yau A, Magliocco A, Chu P. Cutaneous metastatic disease in cervical cancer: A case report. J Obstet Gynaecol Can. 2010;32:467. doi: 10.1016/S1701-2163(16)34501-7. [DOI] [PubMed] [Google Scholar]
- 2.Behtash N, Mehrdad N, Shamshirsaz A, Hashemi R, Amouzegar Hashemi F. Umblical metastasis in cervical cancer. Arch Gynecol Obstet. 2008;278:489–91. doi: 10.1007/s00404-008-0617-4. [DOI] [PubMed] [Google Scholar]
- 3.Behtash N, Ghaemmaghami F, Yarandi F, Ardalan FA, Khanafshar N. Cutaneous metastasis from carcinoma of the cervix at the drain site. Gynecol Oncol. 2002;85:209–11. doi: 10.1006/gyno.2001.6559. [DOI] [PubMed] [Google Scholar]
- 4.Benedet JL, Hacker NF, Ngan HY. Staging Classifications and clinical practice guidelines of gynaecologic cancers. 2003. [Last accessed on 2014 Oct 10]. pp. 38–39. [WWW document] Available from: http://www.igcs.org/files/TreatmentResources/FIGO_IGCS_staging.pdf .
- 5.Ayyamperumal A, Tharini G, Ravindran V, Parveen B. Cutaneous manifestations of internal malignancy. Indian J Dermatol. 2012;57:260–4. doi: 10.4103/0019-5154.97657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Imachi M, Tsukamoto N, Kinoshita S, Nakano H. Skin metastasis from carcinoma of the uterine cervix. Gynecol Oncol. 1993;48:349–54. doi: 10.1006/gyno.1993.1061. [DOI] [PubMed] [Google Scholar]
- 7.Vasuki S, Durgalakshmi J, Latha J. Cutaneous metastases presenting as genital ulcer disease. Indian J Sex Transm Dis. 2014;35:43–5. doi: 10.4103/2589-0557.132422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khurana R, Singh S. Isolated cutaneous metastasis to thigh from cancer cervix – Fourteen years after curative radiotherapy. Internet J Gynecol Obstet. 2009;11:1. [Google Scholar]
- 9.Grabiec M, Małgorzata W, Andrzej M. Multiple skin metastases to vulva from carcinoma of the cervical stump. Ginekol Pol. 2010;81:140–3. [PubMed] [Google Scholar]


