Abstract
Leukemia cutis (LC) is a nonspecific word used for cutaneous infiltration of leukemia, which is a rare presentation of acute lymphoblastic leukemia (ALL), and always a harbinger of poor prognosis. We report a case of LC in a 5-year-old boy with a past medical history of ALL (L1) presented with multiple asymptomatic oval or annular red patches and plaques on his thighs, buttocks and back waist, and part of them were scaling lesions. A biopsy was performed and histopathological examination showed that medium-sized atypical cells with round to oval contours, scant cytoplasm, and finely dispersed chromatin infiltrated into the dermis and subcutis, and the perivascular and periadnexal areas were involved. Immunophenotyping showed that the atypical cells were positive for CD45, CD3ε, CD99, and Ki67 (about 70%). Considering the patient's medical history and the histopathology, the patient was diagnosed with LC.
Keywords: Acute lymphoblastic leukemia, leukemia cutis, leukemid
What was known?
Leukemia cutis (LC) is the infiltration of neoplastic leukocytes or their precursors into the epidermis, the dermis, or the subcutis, resulting in clinically cutaneous lesions. And the most common presentations are nodules, papules, and plaques
LC is rare in acute lymphoblastic leukemia, and the incidence is ranged from 1% to 3%.
Introduction
Leukemia cutis (LC) is the infiltration of neoplastic leukocytes or their precursors into the epidermis, the dermis, or the subcutis, resulting in clinically cutaneous lesions. It can occur in any type of leukemia, and is rare in ALL (1–3%). The clinic features of LC include papules, nodules, plaques, ulcers, vesicles, and swellings.[1,2] And the distributions of LC are most commonly involved in extremities and trunk. Because of the variable and nonspecificity of cutaneous presentation of LC, a biopsy is necessary. Herein, we report a case of LC of ALL for its rarity.
Case Report
A 5-year-old boy came to our clinic for evaluation with lesions on his buttocks, thighs, and back waist. One month ago, he was presented with erythema on his buttocks and thighs, which were neither itchy nor tender. In the next 1 month, the erythema gradually enlarged and spread to the back waist, and part of them developed into plaques. The patient had a history of ALL (L1) and received allogenic bone marrow transplantation 10 months ago.
On cutaneous examination, he was found to have multiple oval or annular red patches and plaques scattered on his buttocks, thighs, back waist and part of them were scaling lesions. The lesions were sharply demarcated and ranged between 1 and 3 cm in diameter [Figure 1]. Considering his history of ALL (L1), a biopsy was performed immediately, and a diagnosis of LC was made.
Figure 1.

Multiple oval or annular red patches and plaques scattered on his buttocks, thighs, back waist and part of them were scaling lesions
On the histopathologic examination, it showed a band-like and nodular infiltration into the dermis and subcutis [Figure 2], with the perivascular and periadnexal areas involved [Figure 3]. The infiltrated cells were medium-sized atypical cells with round to oval contours, scant cytoplasm, and finely dispersed chromatin [Figure 3]. Immunophenotyping showed that the atypical cells were positive for CD45, CD3ε, CD99, and Ki67 (about 70%) [Figure 4] and negative for CD20, CD30, CD56, CD117, MPO, CD68/(P), CD68/PCM-J, and TdT. Taking the patient's medical history and the histopathology into account, the patient was diagnosed with LC of ALL.
Figure 2.
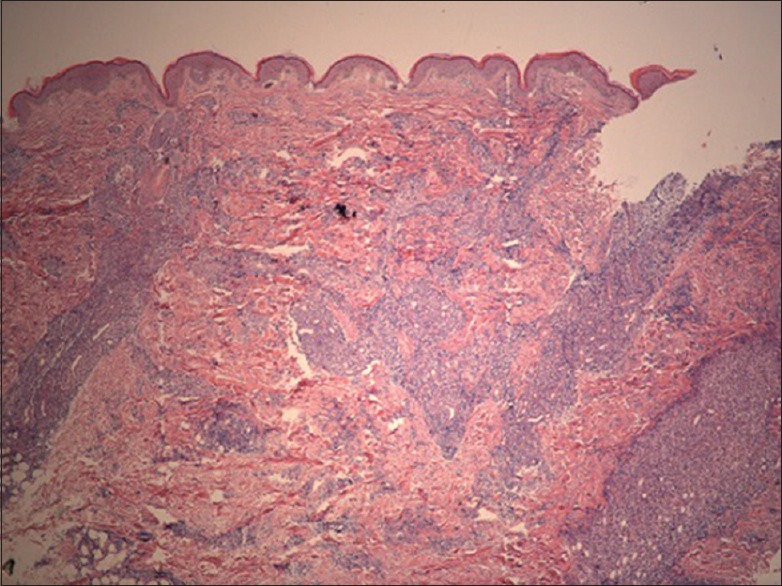
Histology showed a band-like and nodular infiltration of atypical cells into the dermis and sub cutis (H and E, ×25)
Figure 3.
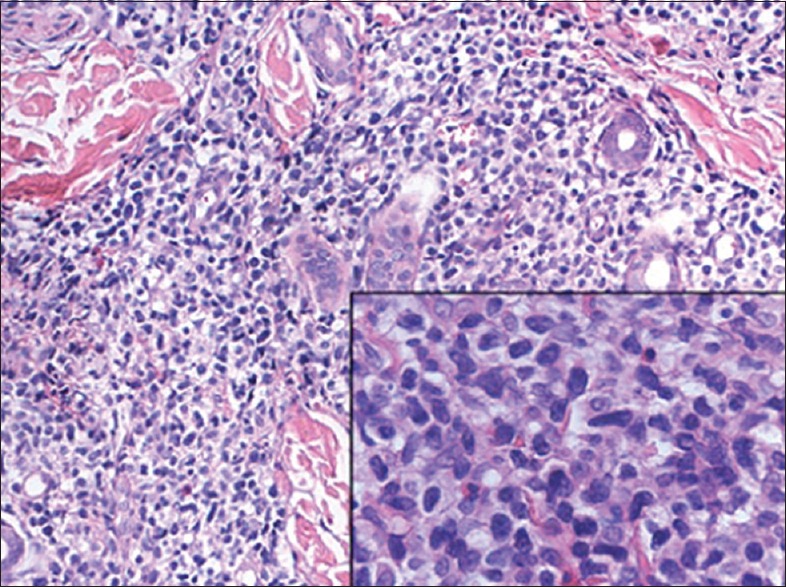
Histology showed a perivascular and periadnexal involvement of medium-sized atypical cells with scant cytoplasm, and finely dispersed chromatin (H and E, ×200; inset, ×400)
Figure 4.
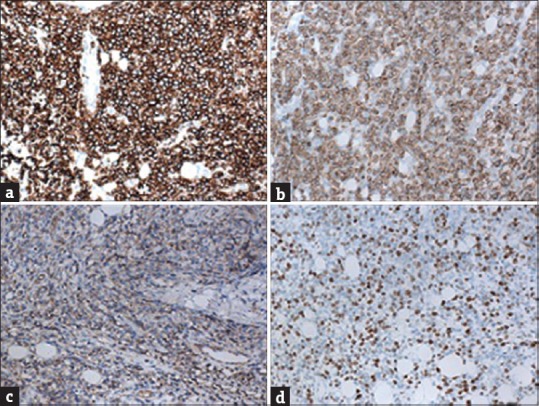
The infiltrated cells were positive for CD45 (a), CD3ε (b), CD99 (c), Ki67 (d) (Immunohistochemical, ×200)
The patient did not come back to our hospital for further investigation and treatment after his parents knew his diagnosis, so he lost of follow-up.
Discussion
The cutaneous manifestation of leukemia can be divided into LC and leukemid. LC is the infiltration of neoplastic leukocytes or their precursors into the skin. The majority of LC occur concomitantly or follow with the setting of established systemic leukemia, but rarely, it may precede observable peripheral blood or bone marrow involvement, which is known as aleukemic LC (ALC). The LC is most common in patients with acute myelogenous leukemia (10–15%) and congenital leukemia (25–30%), but rare in ALL (1–3%).[3,4] Moreover, there was a review showed that skin infiltration of leukemia account for 30% of all skin biopsy specimens in leukemia patients without clinic skin findings,[5] which meant the evaluation of incidence of LC may be lower than the fact. The appearances of LC are variable, including nodules, papules, plaques, and ulcers, swellings, vesicles are rare presentations, and the locations are usually the extremities, trunk, and sites of herpetic lesions,[3] intravenous catheters,[4] lips,[6] trauma and recent surgeries[7] have been reported. LC of ALL is commonly presented by single or multiple, red-to-violaceous papules or nodules on the head and neck,[4] but our case showed oval or annular scaling red patches and plaques on buttocks, thighs, and back waist, which is rare in clinic.
Leukemid means nonspecific cutaneous conditions associated with leukemia, which commonly manifests petechiae, purpura, ecchymosis, leukocytoclastic vasculitis and neutrophilic dermatoses. Leukemid has a higher incidence in leukemia (40% or more) than LC.[3] In one series, 30% of all skin biopsy of leukemia patients who have cutaneous lesions can be found LC, and the other diagnoses are graft versus host disease, drug reaction, infections, purpura, and small vessel vasculitis.[8]
LC is always a local manifestation of systemic leukemia, so systemic chemotherapy or stem cell transplant can be the primary choice to remission the disease, and radiation therapy can be used in patients who are not candidates for chemotherapy and stem cell transplant. And the limited lesions of ALC can be treated with radiation therapy either.
In general, the cutaneous infiltration of leukemia portends a poor prognosis, and many patients with LC have some other extramedullary diseases. A study from Korea showed that the mean interval between diagnosis of LC and death was 8.3 months, and the majority died within 1 year,[2] and several other studies also indicated that the median survival <1 year.[9,10,11]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
What is new?
The presentation of leukemia cutis (LC) in acute lymphoblastic leukemia can be oval or annular scaling red patches and plaques which are not reported by now
The real incidence of LC in leukemia may be higher than the estimated data at present.
References
- 1.Su WP, Buechner SA, Li CY. Clinicopathologic correlations in leukemia cutis. J Am Acad Dermatol. 1984;11:121–8. doi: 10.1016/s0190-9622(84)70145-9. [DOI] [PubMed] [Google Scholar]
- 2.Kang YS, Kim HS, Park HJ, Lee JY, Kim HO, Cho BK, et al. Clinical characteristics of 75 patients with leukemia cutis. J Korean Med Sci. 2013;28:614–9. doi: 10.3346/jkms.2013.28.4.614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cho-Vega JH, Medeiros LJ, Prieto VG, Vega F. Leukemia cutis. Am J Clin Pathol. 2008;129:130–42. doi: 10.1309/WYACYWF6NGM3WBRT. [DOI] [PubMed] [Google Scholar]
- 4.Lee JI, Park HJ, Oh ST, Lee JY, Cho BK. A case of leukemia cutis at the site of a prior catheter insertion. Ann Dermatol. 2009;21:193–6. doi: 10.5021/ad.2009.21.2.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Longacre TA, Smoller BR. Leukemia cutis. Analysis of 50 biopsy-proven cases with an emphasis on occurrence in myelodysplastic syndromes. Am J Clin Pathol. 1993;100:276–84. doi: 10.1093/ajcp/100.3.276. [DOI] [PubMed] [Google Scholar]
- 6.Obi C, Holler P, Pugliese D, Abraham R, Xu X, Sobanko J, et al. Leukemia labialis: A rare presentation of leukemia cutis limited to the lips. J Am Acad Dermatol. 2012;67:e146–7. doi: 10.1016/j.jaad.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rao AG, Danturty I. Leukemia cutis. Indian J Dermatol. 2012;57:504. doi: 10.4103/0019-5154.103086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Winfield HL, Smoller BR. Other lymphoproliferative and myeloproliferative diseases. In: Bolognia JL, Jorizzo JL, Schaffer JV, editors. Dermatology. 3rd ed. Amsterdam: Elsevier Saunders; 2012. p. 2042. [Google Scholar]
- 9.Jang IG, Lee DW, Han CW, Kim CC, Cho BK. A clinical observation on leukemia cutis. Korean J Dermatol. 1996;34:507–14. [Google Scholar]
- 10.Shaikh BS, Frantz E, Lookingbill DP. Histologically proven leukemia cutis carries a poor prognosis in acute nonlymphocytic leukemia. Cutis. 1987;39:57–60. [PubMed] [Google Scholar]
- 11.Kaddu S, Smolle J, Cerroni L, Kerl H. Prognostic evaluation of specific cutaneous infiltrates in B-chronic lymphocytic leukemia. J Cutan Pathol. 1996;23:487–94. doi: 10.1111/j.1600-0560.1996.tb01440.x. [DOI] [PubMed] [Google Scholar]


