Abstract
Objective
Just-in-time adaptive interventions (JITAIs) use mobile computers, sensors, and software analytics to automatically detect behavior and deliver tailored treatment. However, little is known about how JITAIs influence patterns of behavior or how best to design JITAIs for maximum effect.
Methods
This study examined prompts and behavioral response to the B-MOBILE JITAI for reducing sedentary behavior (SB) in overweight/obese individuals. Thirty participants (83% women; 67% White, mean ± SD body mass index = 36.2 kg/m2) tested three conditions presented in a randomized counterbalanced order involving smartphone-based prompts for walking breaks of (1) 3-min after 30 SB min; (2) 6-min after 60 SB min; and (3) 12-min after 120 SB min.
Results
Participants carried the smartphone an average of 6.90 days during each 7-day condition, for an average of 14.94 hours per day. The 3- and 6-min conditions resulted in the greatest number of prompts, walking breaks, the best adherence to prompts, the greatest amount of daily time spent in walking breaks, and fastest adherence to prompts (ps < .01). Small but statistically significant decreases in the number of daily walking breaks, adherence to prompts, and minutes per day spent in walking breaks were observed as a function of the number of days spent in a condition (ps < .05).
Conclusions
The B-MOBILE JITAI was effective in prompting breaks in sedentary behavior when it is most clinically relevant. Frequent prompts for small change may be an optimal strategy for shaping sedentary behavior, although more research is needed to determine how best to promote long-term adherence.
Keywords: technology, mHealth, eHealth, just-in-time adaptive intervention, obesity
Much has been made of the potential for health technology to transform the treatment and prevention of disease (Lupton, 2014; Pagoto & Bennett, 2013; Topol, 2012). Behavioral health interventions, in particular, are poised to benefit from novel mobile health (mHealth) approaches such as “just-in-time adaptive intervention” (JITAI), which allows a highly personalized behavioral treatment to be delivered in real-time in a patient’s natural environment (Nahum-Shani et al., 2014; Spruijt-Metz & Nilsen, 2014). JITAIs use mobile technology such as smartphones, sensors, and software analytics to automatically detect patient behavior and deliver intervention content that is most relevant to a patient’s needs, at the time that it is most needed and/or likely to improve health-related behaviors (Nahum-Shani et al., 2014;Spruijt-Metz & Nilsen, 2014).
Relatively few JITAIs have thus far been developed and tested. One example is A-CHESS (Alcohol – Comprehensive Health Enhancement Support System), a smartphone-based intervention for individuals recovering from alcoholism (McTavish, Chih, Shah, & Gustafson, 2012). Among other functions, A-CHESS uses global positioning system (GPS) data to detect when a participant approaches an area historically associated with alcohol use and connects them with treatment resources. It has also been suggested that smartphone-based sensing systems could be used with individuals attempting to quit smoking to detect antecedents of smoking lapse and prevent relapse (McClernon & Choudhury, 2013). Most relevant to the current study, a smartphone application aimed at increasing physical activity and reducing sedentary behavior in aging adults was developed to track time spent activity/sedentary and provide real-time feedback using one of three motivational frames (i.e., “analytic, social, or affective”; King et al., 2013).
The newness of the technology and the substantial challenge of developing these complex interventions, which require collaboration among experts in multiple disparate disciplines (e.g., engineers, computer scientists, behavioral intervention scientists), largely explains the relative scarcity of JITAI to date. However, lack of understanding of optimal intervention strategies may also be a factor. While there has been decades of research on general principles of behavioral intervention, very little is known about how to combine those principles with novel technology-based methods of delivering treatment. JITAIs are defined by their ability to intervene with patients at almost any time, with personalized behavioral prescriptions; thus, it is particularly important to understand how the frequency of intervention, and the type of behavioral prescription, affects targeted health behaviors. A question of particular significance is whether more frequent prompts for behavior change may ultimately result in suboptimal adherence due to intervention fatigue or habituation to the prompts, for example.
Aiming to build understanding of optimal use of technology for behavioral intervention, we recently reported on B-MOBILE, a smartphone-based JITAI to reduce sedentary behavior (SB) in overweight/obese individuals (Bond et al., 2014). SB (i.e., activities performed during waking hours that require very low energy expenditure of <1.5 metabolic equivalents (METs) and occur while sitting or lying down; (Newton, Han, Zderic, & Hamilton, 2013; Sedentary Behaviour Research, 2012)) is highest in overweight/obese individuals (Chau, van der Ploeg, Merom, Chey, & Bauman, 2012; Du et al., 2013), and is associated with increased risk of poor cardiometabolic health (Bankoski et al., 2011; Henson et al., 2013), some cancers (Shen et al., 2014), and mortality (Leon-Munoz et al., 2013; Matthews et al., 2012). Conversely, emerging evidence suggests that interrupting prolonged periods of SB (e.g., 20-30 minutes) with brief (e.g., ≥1-2 minutes) physical activity breaks of even a light intensity has beneficial associations with several important indicators of cardiometabolic health (e.g., waist circumference, high-density lipoprotein (HDL) cholesterol, C-reactive protein, triglycerides, insulin, etc.) (Carson, et al., 2014; Dunstan, et al., 2012; Healy et al., 2008; Healy, Matthews, Dunstan, Winkler, & Owen, 2011). In B-MOBILE, a smartphone and its onboard accelerometer were used to automatically monitor prolonged bouts of SB and prompt brief walking breaks upon reaching a clinically significant SB threshold. Thirty overweight/obese wore an objective activity monitor for a week at baseline, and during three subsequent weeks during which three prompting and walking break conditions were tested to determine the optimal behavioral prescription for reducing total time spent in SB (< 1.5 METs) and increasing physical activity (PA; ≥ 1.5 METs): (1) 3-min break after 30 SB min; (2) 6-min break after 60 SB min; and (3) 12-min break after 120 SB min. These conditions are referred to as the 3-min, 6-min, and 12-min conditions, respectively. Given that prompts and feedback were tailored to participants at the unique times when the relevant behaviors were performed, but the three interventions arms were standardized, B-MOBILE meets the time-tailored but not necessarily the personally-tailored (i.e., personalized) criterion for JITAIs (Nahum-Shani et al., 2014;Spruijt-Metz & Nilsen, 2014).
The B-MOBILE JITAI produced significant reductions in daily time spent in SB in all 3 conditions (mean decrease of 47.2, 44.5, and 26.2 min/day, for the 3-min, 6-min, and 12-min conditions, respectively) (Bond et al., 2014). Likewise, significant increases were seen for time spent in light intensity (mean increase of 31.0, 31.0, and 15.3 min/day, respectively) and moderate to vigorous intensity (mean increase of 16.2, 13.5, and 10.8 min/day, respectively) PA. Compared to the 12-min condition, the 3-min condition produced significantly greater improvements in time spent in SB and light intensity PA. Thus, B-MOBILE had a positive effect on reducing an important health risk behavior and provided important novel information on the most effective approaches for improving SB and PA. However, it is equally important to understand more detailed patterns of behavioral response to the JITAI in order to identify strengths and weaknesses of the approach and how it can be optimized to have the greatest positive influence on behavior.
By comparing detailed patterns of prompt delivery and behavioral response in the three B-MOBILE conditions, this paper aims to demonstrate how these data may be used to improve a JITAI above and beyond what can be learned exclusively from analyzing effects on primary outcomes. Specifically, we explored how: (a) frequency of walking prompts, (b) adherence to walking prompts, (c) time spent in walking breaks, and (d) latency between walking prompts and the start of walking breaks varied by the 3 walking break conditions. Particular emphasis was placed on determining whether more frequent prompts produced lower rates of adherence. Given the newness of the JITAI approach, and the lack of previous research on the best approach to maximize walking break frequency and duration, no directional hypotheses were articulated.
Method
The B-MOBILE study design, intervention (including visual depictions of the smartphone application), and results of the primary outcomes analysis based on data collected using an objective multi-sensor monitor are described in a prior publication (Bond et al., 2014). Key aspects of the methodology are reported below, with an emphasis on the smartphone-based system for delivering prompts and detecting behavioral responses.
Procedures
A sample of 30 overweight/obese men and women with body mass index (BMI) ≥ 25 kg/m2 and age 21-70 years old were recruited via local media in Providence, RI, USA. After providing written consent, the within-subjects design involved a 7-day baseline assessment period followed by three 7-day SB intervention conditions presented in a randomized counterbalanced order: (1) prompt for a 3-min walking break after 30 continuous SB min; (2) prompt for a 6-min walking break after 60 continuous SB min; and (3) prompt for a 12-min walking break after 120 continuous SB min. The intervention targeted walking breaks instead of standing breaks due to the comparative difficulty of measuring inclination (e.g., standing versus sitting or lying down) compared to movement using a smartphone accelerometer and because of the greater energy cost of walking versus standing. During the intervention period, participants were provided with an Android smartphone and software application (“app”) that automatically monitored and categorized their behavior as either SB or non-SB in one minute epochs using the onboard accelerometer and a previously validated algorithm. These data were used to automatically drive prompts and to determine when the walking requirement had been met. Reminders to meet the walking prompt were triggered after 5 and 10 minutes of continued SB. A persistent display on the smartphone screen showed minutes until the next walking prompt, total daily SB minutes, total daily PA minutes, and a daily count of walking prompts that had been met. Participants were asked to carry the smartphone on their person during all waking hours, including during walking breaks and while performing other types of physical activity, in a pocket or using a clip supplied by the researchers to attach the phone to their clothing at the waist. All study procedures were approved by the Institutional Review Board of The Miriam Hospital.
Measures
Participant demographic characteristics were collected at baseline via self-report questionnaire. All aspects of the JITAI were measured and recorded automatically by the B-MOBILE application. Engagement with the B-MOBILE intervention system was measured by the number of days, and hours per day, that the smartphone was powered on and carried by the participant in a pocket or via the provided clip (i.e., accelerometer not completely at rest). Daily number of walking prompts was determined for each participant. Adherence was measured by % of walking prompts that resulted in a walking break of the prescribed duration. For each prompt that resulted in a walking break of the prescribed duration, the latency (minutes) between the prompt and the start of the walking break, and the total duration of the walking break was calculated.
Statistical Analysis
Analyses were conducted in 2014 using PASW Statistics 20 (SPSS, Inc., 2011, Chicago, IL, www.spss.com). Demographic characteristics were summarized using mean and standard deviation or counts and % as appropriate. Means (reported with SE and 95% CI) were compared across conditions via linear mixed models using a Restricted Maximum Likelihood (REML) approach for all outcome variables including number of days and minutes per day that the smartphone was active and not completely at rest, daily number of walking prompts and walking breaks, % adherence (i.e., the proportion of walking prompts that produced a walking break), latency from prompt to walking break, duration of walking breaks, and average daily number of minutes spent in walking breaks. Subject intercepts were treated as random effects in these models. In a second step of each analysis, change over the course of each 7-day condition was evaluated by adding number of days in the condition to the model as a predictor to test for patterns collapsing across the conditions, and then condition was added to the model to test for temporal patterns specific to each intervention. Analyses focused on number of prompts per day, walking breaks per day, and adherence to walking prompts controlled for hours per day that the smartphone was powered on and not completely at rest. The day of the week, time of day, and order of presentation of the conditions were tested as potential covariates but were ultimately excluded from the models reported below due to a lack of predictive power. All tests of significance were conducted at α = .05.
Results
Participant Characteristics
The 30 participants had an average age of 47.5 years (SD = 13.5), were primarily female (83%, n = 25,), White (67%, n = 20,), Non-Hispanic (90%, n = 27,), employed full or part-time (60%, n = 18), with at least some post-high school education (80%, n = 24). Participants mean weight was 98.1 kg (SD = 21.6) and mean body mass index (BMI) was 36.2 kg/m2 (SD = 7.5).
Intervention Engagement
Engagement was high in all three conditions. Participants carried the smartphone an average of 6.90 days (SE = .04, 95% CI [6.81, 6.99]) during each 7-day condition, for an average of 14.94 hours per day (SE = .48, 95% CI [13.96, 15.91]). There was no statistically significant difference by condition in number of days, F(2,58) = .635, p = .534, or hours per day, F(2,590.23) = 1.351, p = .260, that the smartphone was carried. The number of hours per day that the smartphone was carried did not significantly increase or decrease as a function of days accrued within a condition, b = .09, t(589.44) = 1.21, p = .225, 95% CI [−.06, .24] when collapsing across conditions, and there was no difference in the trend between conditions F(2,587.31) = 1.22, p = .226.
Walking Prompts
As depicted in Figure 1, the 3-min condition (prompt for a 3-min walking break after 30 continuous SB min) resulted in the highest number of prompts per day (M = 7.01, SE = .25, 95% CI [6.51, 7.51]), followed by 4.53 prompts per day (SE = .25, 95% CI [4.03, 5.02]) in the 6-min condition (prompt for a 6-min walking break after 60 continuous SB min), and 2.29 prompts per day (SE = .25, 95% CI [1.78, 2.79]) in the 12-min condition (prompt for a 12-min walking break after 120 continuous SB min), F(2,533.83) = 230.25, p <.001; p < .001 for all pairwise comparisons). The number of prompts per day did not significantly increase or decrease as a function of days accrued within a condition, b = −.07, t(533.39) = 1.69, p = .092, 95% CI [−.16, .1 ] when collapsing across conditions, and there was no difference in the trend between conditions, F(2,530.86) = 1.19, p =.304.
Figure 1.
Model estimates of mean number of walking prompts and walking breaks per day in the B-MOBILE just-in-time adaptive intervention. 95% confidence intervals are represented in the figure by the error bars attached to each column.
Walking Breaks Produced by Walking Prompts
As depicted in Figure 1, the 3-min condition resulted in the highest number of walking breaks per day (M = 6.52, SE = .26, 95% CI [5.99, 7.05]), followed by 4.08 walking breaks per day (SE = .26, 95% CI [3.55, 4.60]) in the 6-min condition, and 1.81 walking breaks per day (SE = .27, 95% CI [1.28, 2.35]) in the 12-min condition, F(2,536.78) = 226.29, p <.001; p < .001 for all pairwise comparisons. The number of walking breaks per day decreased significantly as a function of days accrued within a condition, b = −.11, t(536.35) = 2.412, p = .016, 95% CI [−.19, −.2 ] when collapsing across conditions, and there was no difference in the trend between conditions, F(2,533.58) = 1.66, p =.190.
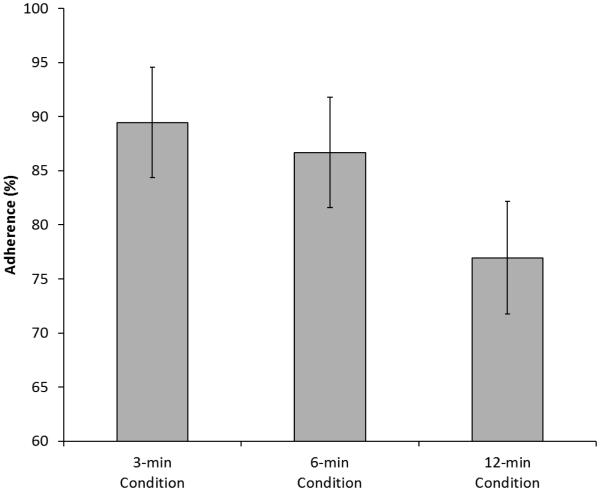
Compared to the other two conditions, adherence (i.e., percent of prompts resulting in a walking break) was lower in the 12-min condition (M = 76.95, SE = 2.59, 95% CI [71.76, 82.15]) compared to the other two conditions F(2,537.146) = 15.83, p <.001; p < .001 for both pairwise comparisons (Figure 2). Adherence in the 3-min (M = 89.44, SE = 2.53, 95% CI [84.35, 94.53]) and 6-min (M = 86.67, SE = 2.53, 95% CI [81.58, 91.75]) conditions did not differ (p = .216 for the pairwise comparison). Adherence decreased significantly as a function of days accrued within a condition, b = −1.14, t(536.85) = 2.465, p = .014, 95% CI [−2.05, −.23] when collapsing across conditions, and there was no difference in the trend between conditions, F(2,533.95) = .249, p =.780.
Figure 2.
Model estimates of adherence (% of walking prompts that resulted in a walking break of the prescribed duration) in the B-MOBILE just-in-time adaptive intervention. 95% confidence intervals are represented in the figure by the error bars attached to each column.
Time to and Duration of Prompted Walking Breaks
The latency between prompts and the beginning of walking breaks was shortest in the 3-min condition (M = 22.95, SE = 3.32, 95% CI [16.19, 29.70]), followed by the 6-min condition (M = 30.02, SE = 3.50, 95% CI [22.95, 37.08]) and the 12-min condition (M = 47.33, SE = 4.12, 95% CI [39.13, 55.54]), F(2,2363.68) = 29.33, p <.001; p < .001 for all pairwise comparisons). The latency between prompts and the beginning of walking breaks did not significantly increase or decrease as a function of days accrued within a condition, b = .90, t(2364.29) = 1.69, p = .092, 95% CI [−.15, 1.94] when collapsing across conditions, and there was no difference in the trend between conditions, F(2,2363.57) = .1.18, p =.308. Despite the high average latency between prompts and the beginning of walking breaks, 40.9%, 41.4%, and 33.8% of walking breaks were initiated within 5 minutes of the prompt in the 3-min, 6-min, and 12-min conditions, respectively.
Prompted walking breaks were longest in the 12-min condition (M = 15.92 minutes, SE = .32, 95% CI [15.30, 16.55]), followed by the 6-min condition (M = 9.12, SE = .25, 95% CI [8.61, 9.63]), and the 3-min condition (M = 5.71, SE = .24, 95% CI [5.23, 6.18]), F(2, 2430.38) = 691.74 , p <.001; p < .001 for all pairwise comparisons (Figure 3). The duration of walking breaks did not significantly increase or decrease as a function of days accrued within a condition, b = −.03, t(2431.01) = .633, p = .527, 95% CI [−.12, .06] when collapsing across conditions and there was no difference in the trend between conditions, F(2,2430.22) = .255, p =.775.
Figure 3.
Model estimates of minutes spent in each prompted walking break and total daily time spent in prompted walking breaks in the B-MOBILE just-in-time adaptive intervention. 95% confidence intervals are represented in the figure by the error bars attached to each column.
There was a statistically significant difference between the three conditions in the average daily number of minutes accrued in walking breaks, F(2,511.83) = 5.627, p =.004 (Figure 3). The number of daily minutes accrued in walking breaks was highest in the 3-minute (M = 37.24, SE = 1.85, 95% CI [33.53, 40.94]) and 6-minute (M = 38.73, SE = 1.86, 95% CI [35.02, 42.45]) conditions, which did not differ (p = .419 for the pairwise comparison), and were both higher than the number of minutes accrued in the 12-minute condition (M = 32.49, SE = 1.93, 95% CI [28.64, 36.33]; p = .014 for the pairwise comparison with the 3-minute condition and p < .001 for the comparison with the 6-minute condition). The number of daily minutes accrued in walking breaks decreased significantly as a function of number of days accrued within a condition, b = −1.06, t(512.39) = 2.761, p = .006, 95% CI [−1.81, −.31] when collapsing across conditions and there was no difference in the trend between conditions, F(2,509.23) = .506, p =.603.
Discussion
This study is the first to explore detailed patterns of behavioral response in a JITAI with varying behavioral prescriptions. We previously showed that the three B-MOBILE intervention conditions were all effective in reducing time spent sedentary and increasing time spent physically active (Bond et al., 2014). We now also show that the three conditions differed in behavioral response, in ways that could have important implications for JITAIs broadly and interventions focused on sedentary behavior and physical activity in particular.
A key finding of this study is that more frequent prompts for behavior change resulted in the highest levels of adherence. Specifically, the conditions with the greatest number of walking prompts resulted in the greatest number of walking breaks. In particular, the 3-min condition resulted in an average of 7 prompts and 6.5 walking breaks per day, thus demonstrating that prompts occurring as often as several times per day can be an effective strategy for driving health behavior change, at least in the short-term. This finding is particularly important for situations in which maximizing the frequency of a behavior is just as, or more important than maximizing the duration and/or intensity of the behavior. This applies to SB, as it is believed that breaking up prolonged bouts of time spent sedentary may be just as important for reducing health risks as limiting total time spent sedentary (Healy et al., 2008).
In addition to producing the most frequent walking breaks, the conditions that required the shortest walking breaks per prompt resulted in the greatest number of total daily minutes spent in walking breaks. This further illustrates the power of frequent prompts for a small behavior change. Importantly, the 3-minute condition was able to produce a total amount of time spent in walking breaks that was equivalent to the 6-minute condition only because participants spent more time in walking breaks than was required to fill the requirement of the prompt. With an average frequency of 6.5 walking breaks per day in the 3-minute condition and 4.1 walking breaks per day in the 6-minute condition, we would expect participants to spend approximately 20 and 25 minutes per day in walking breaks in the two conditions, respectively, if participants only met the minimum requirement of the prompts. In contrast, we see that participants spent about 38 minutes per day in walking breaks in both the 3-and 6-minute conditions. This is because participants continued walking for about 3 additional minutes after fulfilling the requirements of the prompt in both conditions, and the greater frequency of walking breaks in the 3-minute condition resulted in more frequent accrual of these “extra” minutes. Thus, prompting a relatively small behavior change can yield more than the minimum amount of intended change, and frequent prompts for small changes may produce an equivalent amount of total behavior change compared to prompting a larger change less often. The results of this study also suggest that when a fast response to a prompt is considered important, it may be advantageous to limit the required duration and/or intensity of the prompted behavior change. The latency between prompts and the beginning of walking breaks was about 25% shorter in the 3-minute condition compared to the 6-minute condition, and about 50% shorter in the 3-minute condition compared to the 12-minute condition. This is particularly important given that greater latency between prompts and the beginning of walking breaks translates into longer periods of uninterrupted sedentary behavior, which could lead to greater health risks (Healy et al., 2008; Healy et al., 2011). The latency issue may be even more important for other health behaviors, such as when a patient with diabetes is alerted by a real-time continuous glucose monitor to correct hypoglycemia.
A question that could be asked of JITAIs is whether shifting some of the burden of knowing when and how to implement intervention strategies to an electronic system could interfere with participants’ ability to generalize strategies on their own. We therefore examined whether the frequency of walking prompts decreased as a function of the number of days accrued in a condition, which might suggest that participants were learning to interrupt bouts of sedentary behavior on their own without the requiring a prompt. While there was no statistically significant effect of days accrued in a condition, the trend was in the expected direction and the borderline statistically significant p-value suggests that an effect might be detected over a period greater than the seven days spent in each condition in this study. Thus, more research is needed to determine whether behavior change prompted by a JITAI may become increasingly habitual over time and may require gradually less frequent prompting.
Beyond the description of the behavioral patterns above, this study does little to elucidate psychological factors that may explain why more frequent prompts for smaller behavior change produced superior outcomes. One possible explanation among many is that more frequent prompts provided increased opportunity for reinforcement (Kelleher & Gollub, 1962). Upon meeting the walking break goal, participants received an immediate feedback message praising them for their accomplishment. B-MOBILE also tracked accumulation of daily walking breaks via “Go Lights” that accumulated on the application dashboard (Bond et al., 2014). The more frequent feedback and more rapid accumulation of “Go Lights” may have served as a powerful reinforcer of adherence in the conditions with more frequent prompts. More research is clearly needed to understand the psychological underpinnings of response to JITAIs.
A major limitation of this study is that participants spent only seven days testing each of the conditions. The high levels of engagement and responsiveness to the intervention may be due to novelty, and might not be maintained over a longer period. In fact, small but statistically significant decreases were seen in adherence, number of walking breaks per day, and number of minutes spent in walking breaks as a function of the number of days accrued in a condition. However, participants experienced the intervention for a total of 3 weeks (a duration similar to other studies of SB interventions; Dutta, Koepp, Stovitz, Levine, & Pereira, 2014; Fitzsimons et al., 2013; Gardiner, Eakin, Healy, & Owen, 2011) with the conditions presented in a randomized counterbalanced order. Thus, the generally high rates of adherence apply to three weeks of use, not just one. In addition, the decline in adherence was consistent across conditions, and there was no indication that providing more frequent prompts resulted in a faster deterioration in adherence. A second major limitation of this study is the confounding of the frequency of prompts with the burden of the behavioral prescription (i.e., the duration of walking breaks). This study cannot determine the degree to which more frequent prompts versus the lower burden of the behavioral prescription was responsible for optimal outcomes.
The primary strength of this study was the detailed analysis of prompts and behavioral response in a JITAI with varying behavioral prescriptions, which yielded important information that can be used to guide future implementations of JITAI. Beyond reporting this information, this paper also serves as a call to, (a) continue to explore the interface between behavioral intervention strategies and technology, and (b) encourage similar analyses of behavioral response in future JITAI, in addition to the standard analysis of primary outcome measures that is typically reported for traditional behavioral interventions.
Future research involving JITAI should continue to explore questions such as how often and how intensively to intervene on health behaviors in order to maximize intervention effects. As technology evolves, it will also be advantageous to use multi-sensor systems and advanced analytics to predict when an intervention can be initiated to prevent occurrence of a behavior associated with health risk rather than merely reacting to correct the behavior. Lastly, it should be mentioned that participants’ preferences and attitudes should be taken into account when developing and testing JITAIs in order to maximize the potential for acceptability, engagement, and therefore health behavior improvement.
Acknowledgments
This research was supported by a grant from the National Institutes of Health (R03 DK095740).
References
- Bankoki A, Harris TB, McClain JJ, Brychta RJ, Caserotti P, Chen KY, Koster A. Sedentary activity associated with metabolic syndrome independent of physical activity. Diabetes Care. 2011;34(2):497–503. doi: 10.2337/dc10-0987. doi: 10.2337/dc10-0987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond DS, Thomas JG, Raynor HA, Moon J, Sieling J, Trautvetter J, Wing RR. B-MOBILE--a smartphone-based intervention toreduce sedentary time in overweight/obese individuals: A within-subjects experimental trial. PLoS ONE. 2014;9(6):e100821. doi: 10.1371/journal.pone.0100821. doi: 10.1371/journal.pone.0100821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson V, Wong SL, Winkler E, Healy GN, Colley RC, Tremblay MS. Patterns of sedentary time and cardiometabolic risk among Canadian adults. Prev Med. 2014;65:23–27. doi: 10.1016/j.ypmed.2014.04.005. doi: 10.1016/j.ypmed.2014.04.005. [DOI] [PubMed] [Google Scholar]
- Cell Phone and Smartphone Ownership Demographics. 2013 Dec 17; Retrieved from http://www.pewinternet.org/data-trend/mobile/cell-phone-and-smartphone-ownership-demographics/
- Chau JY, van der Ploeg HP, Merom D, Chey T, Bauman AE. Cross-sectional associations between occupational and leisure-time sitting, physical activity and obesity in working adults. Preventive Medicine. 2012;54(3-4):195–200. doi: 10.1016/j.ypmed.2011.12.020. doi: 10.1016/j.ypmed.2011.12.020. [DOI] [PubMed] [Google Scholar]
- Du H, Bennett D, Li L, Whitlock G, Guo Y, Collins R, Chen Z. Physical activity and sedentary leisure time and their associations with BMI, waist circumference, and percentage body fat in 0.5 million adults: The China Kadoorie Biobank study. American Journal of Clinical Nutrition. 2013;97(3):487–496. doi: 10.3945/ajcn.112.046854. doi: 10.3945/ajcn.112.046854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunstan DW, Kingwell BA, Larsen R, Healy GN, Cerin E, Hamilton MT, Owen N. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care. 2012;35(5):1497–1502. doi: 10.2337/dc11-1931. Doi.10.2337/dc10-2386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutta N, Koepp GA, Stovitz SD, Levine JA, Pereira MA. Using sit-stand workstations to decrease sedentary time in office workers: A randomized crossover trial. International Journal of Environmental Research and Public Health. 2014;11(7):6653–6665. doi: 10.3390/ijerph110706653. doi: 10.3390/ijerph110706653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzsimons CF, Kirk A, Baker G, Michie F, Kane C, Mutrie N. Using an individualised consultation and activPAL feedback to reduce sedentary time in older Scottish adults: Results of a feasibility and pilot study. Preventive Medicine. 2013;57(5):718–720. doi: 10.1016/j.ypmed.2013.07.017. doi: 10.1016/j.ypmed.2013.07.017. [DOI] [PubMed] [Google Scholar]
- Gardiner PA, Eakin EG, Healy GN, Owen N. Feasibility of reducing older adults' sedentary time. American Journal of Preventive Medicine. 2011;41(2):174–177. doi: 10.1016/j.amepre.2011.03.020. doi: 10.1016/j.amepre.2011.03.020. [DOI] [PubMed] [Google Scholar]
- Healy GN, Dunstan DW, Salmon J, Cerin E, Shaw JE, Zimmet PZ, Owen N. Breaks in sedentary time: Beneficial associations with metabolic risk. Diabetes Care. 2008;31(4):661–666. doi: 10.2337/dc07-2046. [DOI] [PubMed] [Google Scholar]
- Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003-2006. Eur Heart J. 2011;32(5):590–597. doi: 10.1093/eurheartj/ehq451. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henson J, Yates T, Biddle SJ, Edwardson CL, Khunti K, Wilmot EG, Davies MJ. Associations of objectively measured sedentary behaviour and physical activity with markers of cardiometabolic health. Diabetologia. 2013;56(5):1012–1020. doi: 10.1007/s00125-013-2845-9. doi: 10.1007/s00125-013-2845-9. [DOI] [PubMed] [Google Scholar]
- Kelleher RT, Gollub LR. A Review of PositiveConditioned Reinforcement. Journal of the Experimental Analysis of Behavior. 1962;5(4 Suppl):543–597. doi: 10.1901/jeab.1962.5-s543. doi:10.1901/jeab.1962.5-s543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AC, Hekler EB, Grieco LA, Winter SJ, Sheats JL, Buman MP, Cirimele J. Harnessing different motivational frames via mobile phones to promote daily physical activity and reduce sedentary behavior in aging adults. PLoSONE. 2013;8(4):e62613. doi: 10.1371/journal.pone.0062613. doi: 10.1371/journal.pone.0062613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon-Munoz LM, Martinez-Gomez D, Balboa-Castillo T, Lopez-Garcia E, Guallar-Castillon P, Rodriguez-Artalejo F. Continued sedentariness, change in sitting time, and mortality in older adults. Medicine and Science in Sports and Exercise. 2013;45(8):1501–1507. doi: 10.1249/MSS.0b013e3182897e87. doi: 10.1249/MSS.0b013e3182897e87. [DOI] [PubMed] [Google Scholar]
- Lupton D. Critical perspectives on digital health technologies. Sociology Compass. 2014;8(12):1344–1359. doi: 10.1111/soc4.12226. [Google Scholar]
- Matthews CE, George SM, Moore SC, Bowles HR, Blair A, Park Y, Schatzkin A. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. American Journal of Clinical Nutrition. 2012;95(2):437–445. doi: 10.3945/ajcn.111.019620. doi: 10.3945/ajcn.111.019620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClernon FJ, Roy Choudhury R. I am your smartphone, and I know you are about to smoke: The application of mobile sensing and computing approaches to smoking research and treatment. Nicotine and Tobacco Research. 2013;15(10):1651–1654. doi: 10.1093/ntr/ntt054. doi: 10.1093/ntr/ntt054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McTavish FM, Chih M-Y, Shah D, Gustafson DH. How patients recovering from alcoholism use a smartphone intervention. Journal of Dual Diagnosis. 2012;8(4):294–304. doi: 10.1080/15504263.2012.723312. doi: 10.1080/15504263.2012.723312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2014 Mobile Behavior Report. 2014 Feb 25; Retrieved from http://www.exacttarget.com/sites/exacttarget/files/deliverables/etmc-2014mobilebehaviorreport.pdf.
- Nahum-Shani I, Smith SN, Tewari A, Witkiewitz K, Collins LM, Spring B, Murphy S. Just in time adaptive interventions (jitais): An organizing framework for ongoing health behavior support. Methodology Center technical report. 2014:14–126. doi: 10.1007/s12160-016-9830-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton RL, Jr., Han H, Zderic T, Hamilton MT. The energy expenditure of sedentary behavior: A whole room calorimeter study. PLoS ONE. 2013;8(5):e63171. doi: 10.1371/journal.pone.0063171. doi: 10.1371/journal.pone.0063171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagoto S, Bennett GG. How behavioral science can advance digital health. Translational Behavioral Medicine. 2013;3(3):271–276. doi: 10.1007/s13142-013-0234-z. doi: 10.1007/s13142-013-0234-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedentary Behaviour Research, N. Letter to the editor: Standardized use of the terms "sedentary" and "sedentary behaviours". Applied Physiology, Nutrition, and Metabolism. 2012;37(3):540–542. doi: 10.1139/h2012-024. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- Shen D, Mao W, Liu T, Lin Q, Lu X, Wang Q, Wijndaele K. Sedentary behavior and incident cancer: A meta-analysis of prospective studies. PLoS ONE. 2014;9(8):e105709. doi: 10.1371/journal.pone.0105709. doi: 10.1371/journal.pone.0105709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spruijt-Metz D, Nilsen W. Dynamic models of behavior for just-in-time adaptive interventions. IEEE Pervasive Computing. 2014;13(3):13–17. [Google Scholar]
- Topol EJ. The creative destruction of medicine: Howthe digital revolution will create better health care. Basic Books; New York, NY: 2012. [Google Scholar]