Abstract
p53 has been shown to mediate cancer stem-like cell function by suppressing pluripotency and cellular dedifferentiation. However, there have been no studies to date which have addressed the specific effects of p53 loss in colonic adult stem cells. In this study, we investigated the consequences of conditionally ablating p53 in the highly relevant Lgr5+ stem cell population in the crypt on tumor initiation and progression in the colon. In a mouse model of carcinogen (AOM)-induced colon cancer, tamoxifen-inducible Lgr5-driven deletion of p53 reduced apoptosis and increased proliferation of crypt stem cells, but had no effect on tumor incidence or size. Conversely, in a mouse model of colitis-associated cancer, in which mice are exposed to AOM and the potent inflammation inducer DSS, stem cell-specific p53 deletion greatly enhanced tumor size and incidence in the colon. These novel findings suggest that the loss of p53 function in stem cells enables colonic tumor formation only when combined with DNA damage and chronic inflammation. Furthermore, we propose that stem cell targeting approaches are valuable for interrogating prevention and therapeutic strategies that aim to specifically eradicate genetically compromised stem cells.
Keywords: p53, Lgr5, colon cancer, azoxymethane, dextran sodium sulphate
Introduction
The p53 gene is involved in cell cycle regulation and functions as a “guardian of the genome” to prevent DNA damage from being propagated. Using genetic engineering, it has been demonstrated that transition from precancerous lesions to cancer is accelerated in p53-deficient mice (1)(2). This is attributed in part to the fact that many tissues undergo p53-dependent apoptosis as a means to eliminate cells in the organism that exhibit DNA damage during the transformation process (3). In addition, p53 has been shown to be a critical mediator of stem cell function during the oncogenic process by suppressing pluripotency and cellular dedifferentiation (4). For example, p53 deletion impairs clearance of chromosomal-instable stem cells in response to telomere dysfunction, leading to accumulation of chromosomal instability (5).
The colonic epithelial lining represents one of the most intensively self-replenishing organs in mammals. Cell homeostasis is sustained by crypt-resident multi-potent stem cells (6),(7). Stem cells in adult tissues produce large numbers of differentiated progeny. Since transformation of adult colonic stem cells is an extremely important route towards initiating colon cancer (7),(9) targeting stem cell apoptotic programming may be a very effective approach for cancer prevention and treatment. However, to date, no investigation has determined the in vivo effects of p53 loss specifically targeted to colonic adult stem cells. Typically, deletion models initiate DNA damage following homologous recombination (2) or the use of an inducible intestinal (villin-CreERT2) knock out of p53 (10). This type of approach, although informative, non-selectively impacts all cell types in the colon, i.e., stem and non-stem cells. Since colon cancer has been suggested to follow a cancer stem cell (CSC) hierarchical model (11)(12), we determined how the selective loss of p53 targeted to the highly relevant Lgr5+ stem cell population in the crypt influences tumor initiation and progression in the colon. These actively cycling, long lived crypt stem cells self-renew and generate progeny comprising all the differentiated lineages of the intestinal epithelium (7). Due to the fact that competition between normal and mutated stem cells in the crypt is influenced by inflammation (13),(14), we further assessed the effects of both carcinogen and chronic inflammation in the context of intestinal stem cell-specific p53 function. Our analysis exploits aspects of the CSC hierarchical model and therefore has utility in assessing how therapeutics modulate the eradication of deviant stem cells.
Materials and Methods
Animals
To delete exons 2–10 of Trp53 in colonic stem cells, Trp53flox/flox mice (Jackson, 008462) or Rosa26-LacZ mice (Jackson, 003474) were crossed with Lgr5-EGFP-IRES-creERT2 mice (15) (Jackson, 008875). All mice were crossed onto a C57BL/6 background for at least 10 generations. Details related to the tamoxifen induced Cre-mediated recombination in the colon of Lgr5-EGFP-CreERT2 / R26R-LacZ reporter mice have been reported (16). Mice were maintained on an AIN-76A semi-purified diet (Research Diets, D10001), fed ad libitum and housed on a 12h-12h light-dark cycle. For genotyping analysis, DNA was extracted from tails using DNeasy Blood and Tissue Kit (Qiagen, 69506). PCR was performed using the following primers: p53flox (5'-GGTTAAACCCAGCTTGACCA-3' and 5'-GGAGGCAGAGACAGTTGGAG-3') and cre recombinase (5'-GCATTACCGGTCGATGCAACGAGTG-3' and 5'-GAACGCTAGAGCCTGTTTTGCACGTTC-3').
Cancer initiation and tumor studies
At 8–10 wks of age, male and female mice were injected i.p. with 1 mg of tamoxifen (Sigma, T5648) in corn oil once a day for 5 d. In select experiments, mice were injected once s.c. with azoxymethane (AOM) (Sigma, A5486). For initiation studies, mice were terminated 12 h post-AOM injection. For tumor studies, mice were injected with AOM (10 mg/kg bw) three times at one week intervals and subsequently terminated 24 wks post final injection. As a second (chronic inflammatory) model, mice were injected with AOM (10 mg/kg bw) one time followed by three cycles of DSS exposure and subsequently terminated 6 wks post final DSS treatment (17). Specifically, chronic inflammation was induced by exposure to three cycles of 2% DSS (MP Biomedicals, 160110) in the drinking water (1 cycle: 5 d of DSS, 16 d of fresh water). For proliferation assay, mice were injected i.p. with EdU (Life Technologies, A10044) 2 h prior to termination (18). At the time of euthanasia, colon tissue was flushed with PBS and, in a subset of animals, the entire colon was processed by the Swiss-roll technique. Colon lesions were measured, mapped and excised, and mucosal scrapings were subsequently collected from remaining uninvolved tissue and snap-frozen for further analysis. Swiss rolls of colon were fixed in 4% paraformaldehyde, embedded in paraffin, stained with hematoxylin-eosin, and evaluated in a blinded manner by a board-certified pathologist (B. Weeks). Colon lesions were typed, and the degree of epithelial injury (score 0–3) on microscopic cross sections of the colon was graded. For LacZ staining, sections were fixed in 1% formaldehyde/0.2% gluteraldehyde/0.02% NP-40 in PBS for 2 h at 4°C as previously described (19).
RNA isolation and quantitative real-time PCR
Uninvolved mucosa and tumor RNA were isolated using the RNAqueous-4-PCR kit (Ambion AM1914) and treated with DNA-free inactivation reagent (Ambion, AM1906). RNA integrity was assessed on a bioanalyzer 2100 (Agilent Technologies), quantified by Nanodrop and stored at −80°C. Real-time PCR was performed using an AB 7900 PCR system (Applied Biosystems) and Taqman probes (Assay-on-Demand, Applied Biosystems) for Waf1Cip1 (p21) (Mm04205640_g1) and Noxa (Mm00451763_m1). Target gene expression was normalized to ribosomal 18S expression (Mm03928990_g1).
Immunohistochemistry
Colonic cell proliferation was measured using the Click-IT EdU kit (Life Technologies, C10340). Apoptosis was assessed with a terminal deoxynucleotidyl transferase labeling kit (Trevigen, 4810-30) using ZYMAX Steptavidin-Cy3 (Life Technologies, 438315). Antigen retrieval was performed by sub-boiling in 10 mM sodium citrate (pH 6.0). Other antibodies used were: goat polyclonal ab to GFP (Abcam, ab6673) followed by Alexa-488 rabbit anti-goat secondary ab (Life Technologies, A-21222), rabbit polyclonal ab to Cre (Abcam, 190177) followed by donkey anti-rabbit Alexa-647 secondary ab (Jackson, 711-605-152). Prolong Gold antifade with DAPI (Life Technologies, P36935) was used to coverslip the slides. Images of colonic crypts were captured on an inverted TE 300 Nikon Eclipse fluorescence microscope equipped with a Photometrics Cool Snap EZ digital CCD camera. Images were processed using NIS Image software, version 3.2. For enumeration of immunohistochemical staining, the average number of positive cells from a minimum of 35 crypts (typically >50) was assessed from n=5 animals per treatment.
Statistical Analysis
Data were analyzed using t-tests with significance at P < 0.05. All data are presented as means ± SE, and all analyses were conducted using Prism 6 statistical software (GraphPad Software, Inc., La Jolla, CA).
Results
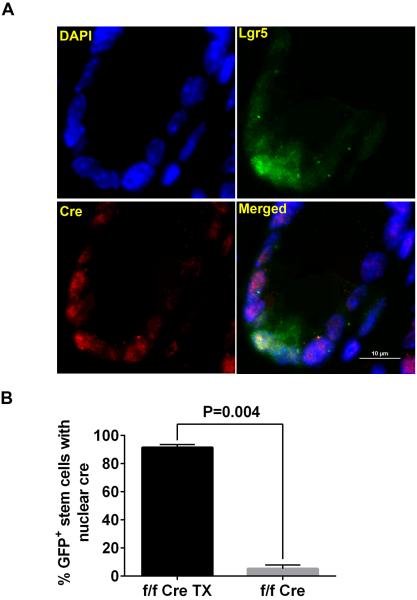
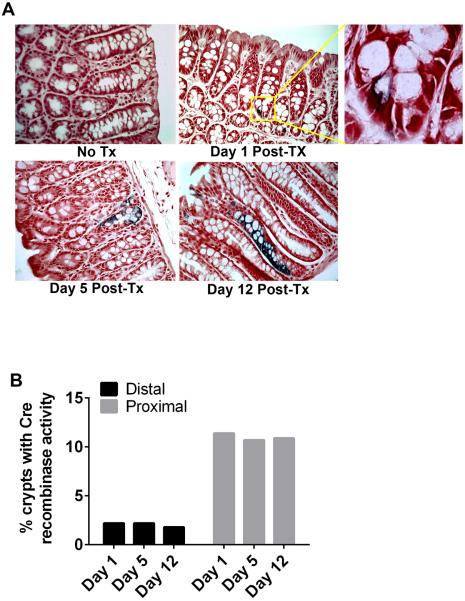
It is becoming increasingly evident that cancer can be initiated at the level of stem cells. This “cancer stem cell model” implies that tissue-resident (normal) adult stem cells are the target of oncogenic processes (20). For the purpose of disrupting p53 exclusively in Lgr5+ stem cells, a compound Lgr5CreERT2 × p53lox/lox mouse was generated. Since the levels of CreERT2 nuclear translocation and genomic recombination associated with the Lgr5-CreERT2 driver in the colon have not been rigorously quantified to date, i.e., previous investigations have exclusively focused on the small intestine (15)(21), following the crossing stem-cell-specific Lgr5-EGFP-IRES-creERT2 knockin mice to p53lox/lox mice (both on a C57BL/6 background), the targeting of activated Cre recombinase in colonic Lgr5+ stem cells was assessed (Figure 1). Following tamoxifen injection, inducible Cre recombinase fused to a mutant estrogen ligand-binding domain enters the nucleus, where it excises the “floxed” cassette. Thus, only nuclear localized Cre in GFP+ stem cells is “activated” for recombination purposes. Stem cell targeted recombination of p53 was further assessed by crossing Lgr5CreERT2 with Rosa26-LacZ mice (Figure 2A). The inducible Cre present in the Lgr5 knock-in allele crossed into the background of the LacZ floxed reporter irreversibly activates β-galactosidase, marking cells in which Cre is expressed, including the descendants. The initial tracing event (~24 h post tamoxifen injection) revealed a stem cell-specific expression of the reporter (LacZ). At 5 and 12 d post tamoxifen administration, a blue ribbon was observed because the genetic modification event is irreversible and inherited by all progeny of the initially labeled stem cell. The percentage of crypts exhibiting Cre recombination ranged from 2.1 ± 0.1% in the distal colon to 11.0 ± 0.2% in the proximal colon (Figure 2B).
Figure 1. Stem cell targeted Cre recombination assessed by crossing Lgr5CreERT2 with Rosa26-LacZ mice.
A. Representative images of X-gal staining with no tamoxifen, and 1, 5, and 12 days post tamoxifen (1 mg) injection. X-gal staining (blue) after 1 tamoxifen injection indicates Cre recombinase activity at the crypt base. Days 5 and 12 denote lineage tracing. B. Percentage of crypts expressing Cre recombinase activity 1, 5, and 12 days post tamoxifen injection (means from 3 mice).
Figure 2. Cre targeting in large intestinal stem cells.
p53lox/lox × Lgr5CreERT2 mice were injected with tamoxifen (f/f Cre TX) (1 mg/day) for 5 consecutive days. Control p53lox/lox × Lgr5CreERT2 mice were not injected with tamoxifen (f/f Cre). A. Representative image of Cre+ cells (white) colocalized with GFP+ stem cells (green) and nuclei (blue). Following tamoxifen injection, inducible Cre recombinase fused to a mutant estrogen ligand-binding domain was able to enter the nucleus, where it excised the “floxed” cassette. Therefore, only the nuclear localized Cre is considered “activated” for recombination purposes. B. Percentage of GFP+ stem cells that are positive for nuclear Cre (mean ± SE, from 3 mice).
Since loss of p53 alone is not sufficient to initiate intestinal neoplasia (10), we examined the functional role of p53 in colonic Lgr5+ stem cell homeostasis in the context of carcinogen-induced tumor initiation. For this purpose, the induction of apoptosis in response to colon-specific carcinogen-induced DNA damage was assessed in tamoxifen injected p53lox/lox × Lgr5CreERT2 (f/f, Cre, TX) and uninjected (f/f, Cre) control mice. One day following tamoxifen injection, mice were treated with AOM and terminated 12 h later (Supplemental Figure 1A). As shown in Figure 3A, Lgr5 targeted knock out of p53 reduced the percentage of apoptotic TUNEL+, GFP+ stem cells by 3.5-fold and the number of apoptotic cells per colonic crypt by 3.3-fold during the initiation phase of tumorigenesis. To rule out any non-specific effects related to Cre activation (22), tamoxifen injected Lgr5CreERT2 mice were also exposed to AOM (Supplemental Figure 2). These mice exhibited a phenotype similar to AOM exposed p53f/f × Cre (no tamoxifen) control mice, indicating that the elimination of early AOM-initiated stem cells is only impaired in p53lox/lox × Lgr5CreERT2 as compared to control mice. In contrast, with respect to cell proliferation, the percentage of actively dividing EdU+, GFP+ stem cells and the total number of proliferating cells per crypt were elevated by 2.4-fold and 2.1-fold, respectively, in p53lox/lox × Lgr5CreERT2 as compared to control mice (Figure 3B). As a comparative reference, the effect of AOM vs saline in p53f/f × Cre (no tamoxifen) control mice was also determined (Supplemental Figure 3A). These findings suggest that the synchronous inhibition of mitosis typically observed in the colonic epithelium immediately after AOM exposure (23),(24) is compromised following stem cell targeted deletion of p53.
Figure 3. Reduced apoptosis and increased proliferation in colonic stem cells following AOM exposure.
p53lox/lox × Lgr5CreERT2 were injected with tamoxifen as described in Figure 1. One day later, mice were injected with AOM and terminated after 12 h (see Supplemental Figure 1A for details). A. Representative image of IHC stained apoptotic cells (red) and GFP+ stem cells (green) and nuclei (blue). Data are expressed as the percentage of GFP+ stem cells undergoing apoptosis and total apoptotic cells per crypt (mean ± SE, from 5 mice). B. Representative image of IHC stained proliferating cells (red) and GFP+ stem cells (green). Overlapping GFP+ stem cells that are proliferating appear white. Data are expressed as the percentage of GFP+ stem cells undergoing proliferation and total proliferating cells per crypt (mean ± SE, from 5 mice).
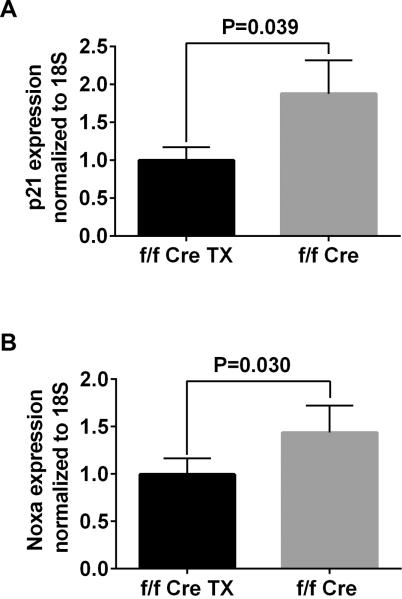
The failure to eliminate AOM-initiated stem cells in p53lox/lox × Lgr5CreERT2 mice was further assessed using a tumorigenesis mouse model of colitis-associated cancer(25) (Supplemental Figure 1B). For this purpose, the DSS-induced chronic inflammation is an excellent preclinical model of colitis that exhibits many phenotypic characteristics relevant to the human disease(26). When combined with AOM, at least 80% of the animals (C57BL/6 mice) develop colonic adenocarcinomas(17),(27). Consistent with the perturbation in the acute apoptosis and cell cycle activity response to AOM (Figure 3), stem cell targeted p53 knock out mice exhibited an increased tumor incidence and size (Figure 4). Specifically, p53f/f × Cre, tamoxifen-injected mice exhibited a 3.4-fold higher number of tumors per cm of colon, with an average 3.6-fold increase in tumor volume as compared to p53f/f × Cre (control) mice. Tumors were confined predominantly to the distal colon and rates of cell proliferation in uninvolved regions of the colon were independent of p53 status (Supplemental Figure 3B&C). Since stress induced cell cycle arrest and apoptosis is mediated by p53 target genes(28), the expression of p21 Waf1/Cip1 and Noxa was subsequently examined. For this purpose, tumors from p53lox/lox × Lgr5CreERT2 mice with and without tamoxifen injection were isolated. Consistent with the targeted deletion of p53, p21 and Noxa expression levels were decreased by 1.9 and 1.6-fold, respectively, in tumors from p53f/f × Cre, tamoxifen-injected mice. Since the non-targeted loss of p53 in enterocytes in the presence of AOM exposure promotes lymph node metastasis (10), the inguinal lymph nodes and liver were inspected for metastases by a blinded pathologist. In contrast to p53f/f mice crossed with villin-Cre (10) in which oncogenic gain of function is non-selectively targeted to all cells in the intestinal mucosa, i.e., stem and non-stem cells, there was no evidence of tumor invasion (data not shown). This suggests that stem cell-specific loss of p53 may be less important for the invasive phenotype compared to loss of p53 in differentiated cells.
Figure 4. Stem cell targeted p53 deletion increases tumor incidence following AOM/DSS exposure.
p53lox/lox × Lgr5CreERT2 and control mice were injected with tamoxifen as described in Figure 2. Subsequently, mice were injected once with AOM (10 mg/kg bw) and challenged with 3 cycles of DSS (see Supplemental Figure 1B for details). A. Representative colon from p53lox/lox × Lgr5CreERT2 mice without tamoxifen. B. p53lox/lox × Lgr5CreERT2 mice injected with tamoxifen. C. Tumor incidence data are expressed as the total number of tumors per cm colon and as average tumor size (cm3) (mean ± SE, from 5 mice).
To further probe the mechanisms by which p53 controls alternative stem cell fate, a separate cohort of mice were exclusively exposed to AOM (three weekly injections) and subsequently terminated 24 wks after the final injection (Supplemental Figure 4). Interestingly, in the absence of inflammation-induced cell stress, stem cell targeted p53 deletion did not affect tumor incidence or size following repeated cycles of AOM exposure (Supplemental Figure 5).
Discussion
Significant progress has been made regarding the identity of cells at the foundation of tumorigenesis. The majority of data suggest that resident adult stem cells serve as the primary initiators of colon cancer (29)(30). This is significant because stem cell-derived long-lived CSCs are resistant to current therapies, which have been linked to cancer recurrence and metastasis (30). Therefore, it is essential to study prevention/therapeutic strategies within the context of a CSC hierarchical model in which oncogenic gain of function has been targeted to stem cells. Although p53 is a critical mediator of stem cell function and suppresses self renewal during the oncogenic process (4)(31), previous studies have probed its function by (i) systemic deletion using homologous recombination (2) and (ii) using a villin-CreERT2;p53-flox/flox strategy (10) which non-selectively targets p53 in all epithelial lineages, e.g., stem and differentiated cell populations. Therefore, we targeted disruption of p53 within the Lgr5-GFP+ intestinal cell population. Using this approach, crypts exhibited a low level of targeted Cre recombination ranging from ~2% in the distal colon to 11% in the proximal colon. This is a relevant attribute of the Lgr5-CreERT2 model, because the frequency of genetic hits is similar to the typical levels in which oncogenic mutations/deletions are acquired in bona fide cancer (32).
In the present study, we demonstrate for the first time that Lgr5+ cell targeted deletion of p53 reduces apoptosis and increases cell proliferation in colonic stem cells following AOM-induced DNA damage. This phenotype is consistent with the well documented role of p53 in the regulation and cellular response to DNA damage in tumor initiating stem cells (33)(34)(35). Importantly, these changes in stem cell dynamics at the tumor initiation stage were associated with a greatly enhanced tumor size and incidence in the distal colon of AOM/DSS treated mice. Interestingly, stem cell targeted p53 deletion had no effect at the tumor stage in AOM injected animals. This finding is consistent with recent evidence that extrinsic factors such as inflammation can reprogram stem cells to become CSCs (29)(36). Indeed, the competition between normal and mutated stem cells in the crypt has been shown to be influenced by inflammation (13). Presumably, therefore, AOM-damaged - p53 mutated clones do not have a benefit over wild-type stem cells in the normal epithelium but tend to prevail in an inflamed intestine. Thus, p53 compromised stem cells display a condition-dependent advantage, and in the chronically inflamed colon, clones harboring deletions in this gene are favored. Our data suggest that the precise cellular target of p53 inactivation, e.g., stem cell vs differentiated cell, could determine whether individuals suffering from chronic intestinal inflammation progress to colorectal cancer. This is relevant because an increased p53 mutation load is a frequent early event associated with ulcerative colitis (37)(38).
The vast majority of studies on intestinal stem cells have focused on the small intestine, while, surprisingly, stem cells of the large intestine remain poorly characterized. For example, tumor suppressor gene deletion targeted to Lgr5+ stem cells has been utilized to demonstrate that a stem cell/cancer stem cell hierarchy is maintained in early neoplastic lesions of the small intestine (11). Although the intestinal loss of p53 alone is insufficient to initiate colon tumorigenesis (10)(29), our data extend these findings and suggest that the oncogenic gain of function targeted to stem cells is an efficient route towards enabling colonic tumors only when combined with DNA damage and chronic inflammation. This reinforces two important points, (i) that colon cancer is strongly linked to the presence of an altered stem cell pool; and (2) that the microenvironment has enormous influence in determining the fate and function of stem cells. With respect to translation of our data, we propose that the stem cell targeting approach provides a powerful tool to interrogate primary prevention strategies, e.g., diet and exercise, to specifically eradicate genetically compromised stem cells. Ultimately, this strategy will provide a better understanding of the origins of cancer and the development of diagnostic tests that can detect cancer development at its earliest stages, which will improve overall survival.
Supplementary Material
Figure 5. Tumor gene expression of p53 regulated genes.
Tumors from p53lox/lox × Lgr5CreERT2 mice with and without tamoxifen injection were analyzed with respect to the expression of p21 waf1/cyp1 and Noxa, downstream markers of p53. Data are normalized to 18S (mean ± SE, from 5 mice).
Acknowledgements
We thank Hans Clevers for generously providing the Lgr5 reporter mice.
Funding: This work was supported by NIH CA164623, CA129444, CA168312, P30ES023512 and the American Institute for Cancer Research.
Footnotes
No author has a conflict of interest.
References
- 1.Halazonetis TD, Gorgoulis VG, Bartek J. An oncogene-induced DNA damage model for cancer development. Science. 2008;319:1352–5. doi: 10.1126/science.1140735. [DOI] [PubMed] [Google Scholar]
- 2.Halberg RB, Katzung DS, Hoff PD, Moser a R, Cole CE, Lubet R a, et al. Tumorigenesis in the multiple intestinal neoplasia mouse: redundancy of negative regulators and specificity of modifiers. Proc Natl Acad Sci U S A. 2000;97:3461–6. doi: 10.1073/pnas.050585597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu D, Ou L, Clemenson GD, Chao C, Lutske ME, Zambetti GP, et al. Puma is required for p53-induced depletion of adult stem cells. Nat Cell Biol. 2010;12:993–8. doi: 10.1038/ncb2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao T, Xu Y. P53 and Stem Cells: New Developments and New Concerns. Trends Cell Biol. 2010;20:170–5. doi: 10.1016/j.tcb.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Begus-Nahrmann Y, Lechel A, Obenauf AC, Nalapareddy K, Peit E, Hoffmann E, et al. P53 Deletion Impairs Clearance of Chromosomal-Instable Stem Cells in Aging Telomere-Dysfunctional Mice. Nat Genet. 2009;41:1138–43. doi: 10.1038/ng.426. [DOI] [PubMed] [Google Scholar]
- 6.Barker N, Bartfeld S, Clevers H. Tissue-resident adult stem cell populations of rapidly self-renewing organs. Cell Stem Cell. 2010;7:656–70. doi: 10.1016/j.stem.2010.11.016. [DOI] [PubMed] [Google Scholar]
- 7.Tetteh PW, Farin HF, Clevers H. Plasticity within stem cell hierarchies in mammalian epithelia. Trends Cell Biol. 2015;25:100–8. doi: 10.1016/j.tcb.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Lin SA, Barker N. Gastrointestinal stem cells in self-renewal and cancer. J Gastroenterol. 2011;46:1039–55. doi: 10.1007/s00535-011-0424-8. [DOI] [PubMed] [Google Scholar]
- 9.Asfaha S, Hayakawa Y, Muley A, Stokes S, Graham TA, Ericksen RE, et al. Krt19+/Lgr5− Cells Are Radioresistant Cancer-Initiating Stem Cells in the Colon and Intestine. Cell Stem Cell. 2015;16:627–38. doi: 10.1016/j.stem.2015.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schwitalla S, Ziegler PK, Horst D, Becker V, Kerle I, Begus-Nahrmann Y, et al. Loss of p53 in enterocytes generates an inflammatory microenvironment enabling invasion and lymph node metastasis of carcinogen-induced colorectal tumors. Cancer Cell. 2013;23:93–106. doi: 10.1016/j.ccr.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 11.Barker N, Ridgway R a, van Es JH, van de Wetering M, Begthel H, van den Born M, et al. Crypt stem cells as the cells-of-origin of intestinal cancer. Nature. 2014;457:608–11. doi: 10.1038/nature07602. [DOI] [PubMed] [Google Scholar]
- 12.Chandler JM, Lagasse E. Cancerous stem cells: deviant stem cells with cancer-causing misbehavior. Stem Cell Res Ther. 2010;1:13. doi: 10.1186/scrt13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vermeulen L, Morrissey E, van der Heijden M, Nicholson AM, Sottoriva A, Buczacki S, et al. Defining stem cell dynamics in models of intestinal tumor initiation. Science. 2013;342:995–8. doi: 10.1126/science.1243148. [DOI] [PubMed] [Google Scholar]
- 14.Zeuner A, Todaro M, Stassi G, Maria R De, Elena VR. Colorectal Cancer Stem Cells : From the Crypt to the Clinic. Cell Stem Cell. 2014;15:692–705. doi: 10.1016/j.stem.2014.11.012. [DOI] [PubMed] [Google Scholar]
- 15.Barker N, van Es JH, Kuipers J, Kujala P, van den Born M, Cozijnsen M, et al. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature. 2007;449:1003–7. doi: 10.1038/nature06196. [DOI] [PubMed] [Google Scholar]
- 16.Feng Y, Sentani K, Wiese A, Sands E, Green M, Bommer GT, et al. Sox9 induction, ectopic Paneth cells, and mitotic spindle axis defects in mouse colon adenomatous epithelium arising from conditional biallelic Apc inactivation. Am J Pathol. 2013;183:493–503. doi: 10.1016/j.ajpath.2013.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jia Q, Lupton JR, Smith R, Weeks BR, Callaway E, Davidson L a, et al. Reduced colitis-associated colon cancer in Fat-1 (n-3 fatty acid desaturase) transgenic mice. Cancer Res. 2008;68:3985–91. doi: 10.1158/0008-5472.CAN-07-6251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Turk HF, Monk JM, Fan Y-Y, Callaway ES, Weeks B, Chapkin RS. Inhibitory effects of omega-3 fatty acids on injury-induced epidermal growth factor receptor transactivation contribute to delayed wound healing. Am J Physiol Cell Physiol. 2014;304:C905–17. doi: 10.1152/ajpcell.00379.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davidson L a, Goldsby JS, Callaway ES, Shah MS, Barker N, Chapkin RS. Alteration of colonic stem cell gene signatures during the regenerative response to injury. Biochim Biophys Acta. 2012;1822:1600–7. doi: 10.1016/j.bbadis.2012.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vermeulen L, Snippert HJ. Stem cell dynamics in homeostasis and cancer of the intestine. Nat Rev Cancer. 2014;14:468–80. doi: 10.1038/nrc3744. [DOI] [PubMed] [Google Scholar]
- 21.Li N, Yousefi M, Nakauka-Ddamba A, Jain R, Tobias J, Epstein JA, et al. Single-Cell Analysis of Proxy Reporter Allele-Marked Epithelial Cells Establishes Intestinal Stem Cell Hierarchy. Stem Cell Reports. 2014;3:876–91. doi: 10.1016/j.stemcr.2014.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li Y, Choi PS, Casey SC, Felsher DW. Activation of Cre Recombinase Alone Can Induce Complete Tumor Regression. PLoS One. 2014;9:e107589. doi: 10.1371/journal.pone.0107589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hirose Y, Yoshimi N, Makita H, Hara A, Tanaka T, Mori H. Early alterations of apoptosis and cell proliferation in azoxymethane-initiated rat colonic epithelium. Jpn J Cancer Res. 1996;87:575–82. doi: 10.1111/j.1349-7006.1996.tb00262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wargovich MJ, Medline A, Bruce WR. Early histopathologic events to evolution of colon cancer in C57BL/6 and CF1 mice treated with 1,2-dimethylhydrazine. J Natl Cancer Inst. 1983;71:125–31. [PubMed] [Google Scholar]
- 25.Bollrath J, Greten FR. IKK/NF-kappaB and STAT3 pathways: central signalling hubs in inflammation-mediated tumour promotion and metastasis. EMBO Rep. 2009;10:1314–9. doi: 10.1038/embor.2009.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tanaka T, Kohno H, Suzuki R, Hata K, Sugie S, Niho N, et al. Dextran sodium sulfate strongly promotes colorectal carcinogenesis in ApcMin/+ mice: Inflammatory stimuli by dextran sodium sulfate results in development of multiple colonic neoplasms. Int J Cancer. 2006;118:25–34. doi: 10.1002/ijc.21282. [DOI] [PubMed] [Google Scholar]
- 27.Greten FR, Eckmann L, Greten TF, Park JM, Li ZW, Egan LJ, et al. IKKbeta links inflammation and tumorigenesis in a mouse model of colitis-associated cancer. Cell. 2004;118:285–96. doi: 10.1016/j.cell.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 28.Vousden KH, Ryan KM. P53 and Metabolism. Nat Rev Cancer. 2009;9:691–700. doi: 10.1038/nrc2715. [DOI] [PubMed] [Google Scholar]
- 29.White AC, Lowry WE. Refining the role for adult stem cells as cancer cells of origin. Trends Cell Biol. 2015;25:11–20. doi: 10.1016/j.tcb.2014.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yang T, Rycaj K, Liu Z-M, Tang DG. Cancer stem cells: constantly evolving and functionally heterogeneous therapeutic targets. Cancer Res. 2014;74:2922–7. doi: 10.1158/0008-5472.CAN-14-0266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu D, Ou L, Clemenson GD, Chao C, Lutske ME, Zambetti GP, et al. Puma is required for p53-induced depletion of adult stem cells. Nat Cell Biol. 2010;12:993–8. doi: 10.1038/ncb2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jones S, Chen W, Parmigiani G, Diehl F, Beerenwinkel N, Antal T, et al. Comparative lesion sequencing provides insights into tumor evolution. Proc Natl Acad Sci U S A. 2008;105:4283–8. doi: 10.1073/pnas.0712345105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Choi M, Shi J, Jung SH, Chen X, Cho K-H. Attractor landscape analysis reveals feedback loops in the p53 network that control the cellular response to DNA damage. Sci Signal. 2012;5:ra83. doi: 10.1126/scisignal.2003363. [DOI] [PubMed] [Google Scholar]
- 34.Aloni-Grinstein R, Shetzer Y, Kaufman T, Rotter V. p53: The barrier to cancer stem cell formation. FEBS Lett. 2014;588:2580–9. doi: 10.1016/j.febslet.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 35.Hu Y, Le Leu RK, Young GP. Absence of acute apoptotic response to genotoxic carcinogens in p53-deficient mice is associated with increased susceptibility to azoxymethane-induced colon tumours. Int J Cancer. 2005;115:561–7. doi: 10.1002/ijc.20876. [DOI] [PubMed] [Google Scholar]
- 36.Westphalen CB, Asfaha S, Hayakawa Y, Takemoto Y, Lukin DJ, Nuber AH, et al. Long-lived intestinal tuft cells serve as colon cancer – initiating cells. J Clin Invest. 2014;124:1283–95. doi: 10.1172/JCI73434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hussain SP, Amstad P, Raja K, Ambs S, Nagashima M, Bennett WP, et al. Increased p53 Mutation Load in Noncancerous Colon Tissue from Ulcerative Colitis : A Cancer-prone Chronic Inflammatory Disease Increased p53 Mutation Load in Noncancerous Colon Tissue from Ulcerative Colitis : A Cancer-prone Chronic Inflammatory Disease. Cancer Res. 2000;60:3333–7. [PubMed] [Google Scholar]
- 38.Cooks T, Harris CC, Oren M. Caught in the cross fire: p53 in inflammation. Carcinogenesis. 2014;35:1680–90. doi: 10.1093/carcin/bgu134. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.