Abstract
Introduction
The WHO established the MPOWER policy package to boost the implementation of the WHO Framework Convention for Tobacco Control (WHO FCTC) in 2008 and to provide practical guidance on policies effective at reducing smoking rates. An easily applied Abridged SimSmoke was developed to help countries gauge the effect of these policies using data from the WHO MPOWER/WHO Report (MPOWER Report) and is applied to four Eastern Mediterranean countries.
Methods
The number of smokers in a country is calculated using the country’s smoking prevalence and population. Policy effect sizes, based on previously validated SimSmoke models, are applied to the smoker populations to determine the reduction in the number of smokers resulting from implementing policies. The number of smoking-attributable deaths is derived based on findings that half of those smokers alive today will die from smoking.
Results
Within 40 years, implementing the complete set of MPOWER policies is projected to reduce smoking prevalence by 29% (range 15%, 41%) and avert almost 1 (range 0.5, 1.4) million deaths in Egypt, reduce smoking prevalence by 52% (range 36%, 66%) and avert 156 000 (106 000, 196 000) deaths in Lebanon, reduce smoking prevalence by 56% (range 40%, 69%) and avert 3.5 (range 2.5, 4.3) million deaths in Pakistan, and reduce smoking prevalence by 37% (range 21%, 51%) and avert 245 000 (range 138 000, 334 000) deaths in Tunisia.
Conclusions
The Abridged SimSmoke model has been used to show the number of deaths from smoking and how MPOWER policies can be used to reach the WHO non-communicable deaths voluntary target for cigarette use reduction in four countries.
INTRODUCTION
Smoking is globally responsible for at least 8 million non-communicable deaths (NCD) per year.1 To reduce NCD, the WHO, as part of its global NCD agenda, set a voluntary target to reduce smoking rates by 30% by 2025.2
The WHO provides technical guidance to help countries reach these goals by fully implementing the WHO Framework Convention for Tobacco Control (WHO FCTC) and, to fulfil this commitment, a policy package that focuses on selected demand side measures under the name of MPOWER was launched in 2008.3 This package includes: Monitor tobacco use and prevention policies, Protect people from tobacco smoke, Offer help to quit tobacco use, Warn about the dangers of tobacco, Enforce bans on tobacco advertising, promotion and sponsorship and Raise taxes on tobacco.
The magnitude of the effect of each MPOWER policy on smokers varies and depends on the policies implemented at a country level, how these are implemented, and the policies that were previously in effect.4 To achieve the target of 30% reduction in smoking rates set by WHO and its Member States, policymakers will need to know the impact of each MPOWER policy individually and in various combinations. The complete SimSmoke model requires a large scale survey of tobacco use to measure smoking prevalence by age and gender, and to develop initiation rates and cessation rates by age and gender. Many countries, especially low-income and middle-income nations not actively implementing tobacco control policies, do not have the necessary data. In addition, expertise is required to calibrate and validate the model.
In a previous application5 we developed a simplified form of SimSmoke to evaluate country-level reductions in smoking-related deaths from implementing target MPOWER policies between 2007 and 2010. In this paper, we present a new form of the model, Abridged SimSmoke, designed to project the effect of newly implemented policies. The data requirements are less than for SimSmoke and parallel to the data collected for the biennial WHO MPOWER/WHO Report on the Global Tobacco Epidemic6 that focuses on measuring the MPOWER policies implemented in all WHO Member States. Abridged SimSmoke does not have the same data requirements, nor require the same level of expertise.
Abridged SimSmoke is developed in Excel so that it is user-friendly and transparent. Like the complete SimSmoke, Abridged SimSmoke projects changes in smoking prevalence and smoking-attributable deaths resulting from the implementation of required MPOWER policies (individually and in combination). As such, the model can be used to develop a strategy for reducing smoking prevalence to its target level.
In this paper, the model is described and applied to four countries in the WHO Eastern Mediterranean Region, chosen based on the availability of data, population size and high-smoking rates. This region generally has high-smoking rates, especially among men, and the countries have not reached the required levels for each of the MPOWER policies.
METHODS
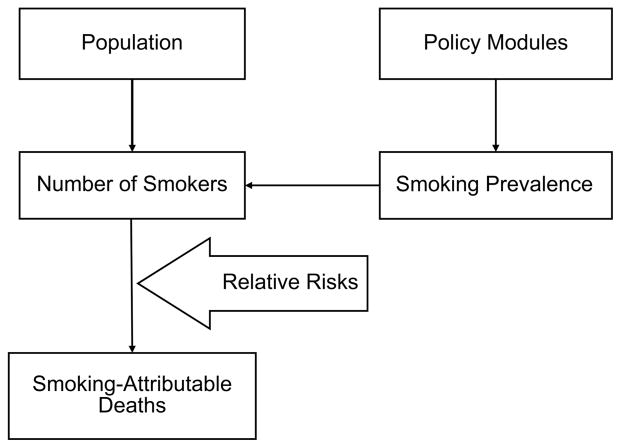
Abridged SimSmoke relies on three central components to make predictions: population size, smoking prevalence and policy modules (figure 1). Using formulas similar to those in SimSmoke, each policy module may reduce smoking prevalence. Unlike the complete SimSmoke, Abridged SimSmoke uses a single year to project short-term (5 years) and long-term (40 years) effects. Based on the effects of individual or combined policies on smoking prevalence, the model predicts a reduction in the number of smokers as a result of those policies which, in turn, is used to predict an effect on smoking-attributable deaths.
Figure 1.
Structure of Abridged SimSmoke.
Smokers and smoking-attributable deaths
First, the number of smokers, by gender, is obtained by multiplying the respective smoking prevalence and the corresponding population size. Applying the relevant policy effect sizes to the number of smokers, as described in the next section, we then calculate the reduction in smokers as a result of a specific policy or group of policies.
The number of deaths attributable to smoking is determined with a formula based on the relative risks of smoking. Doll et al8 concluded that “half of all regular cigarette smokers will eventually be killed by their habit.” The number of deaths averted for each country is calculated by applying the estimate that 50% of smokers will die prematurely due to smoking. Since studies find that low-income and middle-income countries (LMICs) have lower relative mortality risks, we multiply the smoking-attributable death estimates by 0.65 based on studies for South Korea and Taiwan.9,10
Policy effect sizes
Abridged SimSmoke uses SimSmoke policy effect size estimates which are based on literature reviews,4 the advice of expert panels and model validation.11–17 For each policy, the effect size is applied as a percentage reduction in smoking prevalence. For LMICs the effect size is adjusted by a health-awareness adjustor (Aware >1 in LMIC, and Aware=1 in high-income countries (HICs), reflecting the ability of non-price policies to affect health awareness) and an urban adjustor, measured as (1–employed in agriculture), reflecting the ability of these policies to influence a population. Using SimSmoke, a long-term multiplier is estimated for each policy as the ratio of the relative change in prevalence (after 40 years) to the relative change in short-term prevalence (after 5 years). This method is applied to the MPOWER policies. These policies are described and their effect sizes listed in table 1, with upper and lower bound ranges provided in terms of percentage increases and reductions in effect size. The bounds are based on the range of results in the better evaluation studies for each policy, as applied in previous SimSmoke analyses.12,14
Table 1.
Policies, specifications and effect sizes used in Abridged SimSmoke
| Policy | Specification | Description | Effect size (% effect)* | Ranges for sensitivity analysis* | Long-term multiplier* | Awareness adjustor† | Urban adjustor‡ |
|---|---|---|---|---|---|---|---|
| Tax as a per cent of retail price of cigarettes | Tax as a per cent of price | Excise tax in MPOWER, uses arc elasticity formula | Based on price elasticities, −0.15 for HICs and −0.2 for MICs and LICs | (−25%, +25%) | 2 | No | No |
| Smoke-free air laws | |||||||
| Ban in all indoor workplaces | MPOWER | Ban in all indoor private workplaces | 6% | (−50%, +50%) | 1.4 | 1.5 | Yes |
| Ban in indoor offices only | MPOWER | Ban, except ventilated workplaces | 4% | (−50%, +50%) | 1.4 | 1.5 | Yes |
| Ban in health facilities, univ, govt. facilities (2 of 3) | MPOWER | Ban in work areas only | 2% | (−50%, +50%) | 1.4 | 1.5 | Yes |
| Restaurants: smoke-free in all indoor areas | MPOWER | 2% | (−50%, +50%) | 1.4 | 1.5 | Yes | |
| Pubs and bars: smoke-free | MPOWER type | 1% | (−50%, +50%) | 1.4 | 1.5 | Yes | |
| Enforcement | MPOWER: 0–10 | 25% of effect depends on % enforcement (of 10) | |||||
| Publicity | Based on level of tobacco control funding | 25% of above effect depends on publicity | |||||
| Mass media campaigns (policies are mutually exclusive) | |||||||
| Highly publicised campaign | MPOWER: Campaign funds and media campaign | Tobacco control spending ≥US$0.50 per capita and media campaign | 6.5% reduction | (−50%, +50%) | 1.2 | 1 | No |
| Moderately publicised campaign | MPOWER: Campaign funds and media campaign | Tobacco control spending is ≥$0.05 and <US $0.50 per capita, w/agency for tobacco control | 3.5% reduction | (−50%, +50%) | 1.2 | 1 | No |
| Low publicised campaign | MPOWER: Campaign funds and agency for tobacco control | If tobacco control spending is <US$0.05 per capita, w/agency for tobacco control | 1% reduction | (−50%, +50%) | 1.2 | 1 | No |
| Marketing bans¶ | |||||||
| Ban on direct and indirect marketing | MPOWER: score=4 | Ban on all direct and indirect advertising | 5% | (−50%, +50%) | 1.3 | 2 | No |
| Ban on advertising | MPOWER: score=3 | Ban on all direct advertising | 3% | (−50%, +50%) | 1.3 | 2 | No |
| Partial ban on advertising | MPOWER: score=2 | Ban on some direct or indirect advertising | 1% | (−50%, +50%) | 1.3 | 2 | No |
| Enforcement | MPOWER: 0–10 | 0–1.0 | 50% of effect depends on enforcement | ||||
| Health warnings¶ | |||||||
| Complete | MPOWER: score=4 | Bold and graphic, and covers 50% of package | 1% | (−50%, +50%) | 3 | 2 | No |
| Strong | MPOWER: score=3 | Warning 30–50% of package | 0.75% | (−50%, +50%) | 3 | 2 | No |
| Weak | MPOWER: score=2 | Small warning, <30% of package | 0.50% | (−50%, +50%) | 3 | 2 | No |
| Cessation treatment policies** | |||||||
| Nicotine replacement therapy | MPOWER: NRT is provided by general store or pharmacy (no Rx) | Designates if sold by pharmacy or general store and if prescription is required | Prev. reduced 0.667% if available at w/out Rx, 0.334% if Rx | (−75%, +75%) | 2.5 | 1.5 | Yes |
| Bupropion and varenicline | MPOWER: If Bupropion or Varenicline is provided by Rx | Designates if sold by pharmacy with prescription | Prev. reduced 0.334% | (−75%, +75%) | 2.5 | 1.5 | Yes |
| Provision of treatments | Type of facilities: primary care, hospitals, health professionals, community and other | MPOWER: 0=None, Yes in some=0.125, Yes in most=0.5 | If provided in in most, prevalence reduced 2.25% | (−75%, +75%) | 2.5 | 1.5 | Yes |
| Quitline type | MPOWER: 0=None, 1=Yes | Operating active quitline | Prev. reduced 0.5% | (−75%, +75%) | 2.5 | 1.5 | Yes |
| Overall effect | Publicity based on tobacco control funding | Campaign publicised, w/all above policies | Prev. reduced 4.75%, 25% of effect depends on publicity | (−75%, +75%) | 2.5 | 1.5 | Yes |
Short-term effect size is defined as the relative percentage change in smoking prevalence in first 5 years of policy implementation. The long-term effect is short-term-effect multiplied by the long-term multiplier, adjusted by awareness and urban status adjustors. We also provide ranges for the effect sizes, which are measured as percentage variation in the effect sizes compared to the level in the preceding column.
The awareness adjustor is multiplied by the effect size for low-income and middle-income countries.
The urban adjustor reduces the effect to reflect the percentage of the rural population not affected by the policies indicated.
See Levy et al7 for a description of the calculations.
Categories are mutually exclusive categories.
Effects are additive over policies.
HIC, high-income country; LIC, low-income country; MIC, middle-income country; NA, not applicable; NRT, nicotine replacement therapy.
Three types of smoke-free air policies (as applied to work-sites, restaurants and bars and other public places) are included in Abridged SimSmoke, with the effect of worksite bans further distinguished by their stringency: (1) partial, as designated by a ban in two of the three following types of facilities: health, university and government facilities, (2) a ban in indoor offices only, and (3) a ban in all indoor workplaces. The effects are halved in the absence of publicity (based on tobacco control campaign spending as described below) and complete enforcement (an index based on MPOWER reports from 1 to 10, where 10=complete enforcement).
MPOWER cessation treatment has three subpolicies: pharmacotherapy (PT) availability, financial coverage of treatments, and quit lines. The PT availability subpolicy examines whether nicotine replacement treatment (NRT), and bupropion and varenicline are available, as well as their accessibility. Financial coverage distinguishes the provision of cessation treatments in primary care facilities, hospitals, health professionals’ offices, community and other locations. Quit lines reflect the presence of a national quit line.
The category health warnings on packs has four levels: no policy, a minimal policy (<30% of the principal display area of the pack), a moderate policy (a warning that covers at least 30% of the principal display area of the pack, and meets 1–7 of the seven pack warning criteria outlined in MPOWER) and a complete policy (a warning that covers at least 50% of the principal display area of the pack and includes all seven-pack warning criteria, including graphic warnings, as well as a ban on deceitful terms). An additional educational policy involves media campaigns, based on the existence of a media campaign and the funding levels specified for tobacco control campaigns.
Four levels of marketing restriction policies are designated: none, minimal, moderate and comprehensive restrictions. These include restrictions on advertising as well as marketing practices such as branding and sponsorship. For marketing restrictions, no enforcement will reduce the impact of the policy by half.
Cigarettes taxation affects cigarette price which, in turn, influences cigarette use. Taxes are specified as a percent of the retail cigarette price. In accordance with MPOWER policies, we consider the effect of increasing excise taxes (including ad valorem taxes or specific (per unit) taxes directly on cigarettes) to 75% of price. The value added tax (VAT) applies to all goods, not just cigarettes, but amplifies the effect of an excise tax on cigarette price. The change in excise taxes is first translated into the implied percentage change in price. The prevalence elasticity is applied to the percentage change in price to obtain the percentage change in prevalence.
The effect of combined policies is calculated with all policies reaching their MPOWER targets. The effects are proportionally (ie, multiplicatively) reduced for each additional policy. Thereby, relatively conservative assumptions are made about the effects of combined policies (eg, some overlapping effects), and the overall effect is bounded between zero and one.
However, synergies are built into the model through media campaigns that enhance the effect of smoke-free air laws and cessation treatment policies.
Data
Four countries in the Eastern Mediterranean region were chosen based on data availability, size and to reflect different tobacco use behaviours. Egypt and Tunisia are middle-income countries with high-smoking rates for males and low rates for females. Pakistan also has relatively high-smoking rates for males, but is a low-income country. Lebanon is a middle-income country with high-smoking rates for both males and females.
We used country-level data on smoking prevalence from the most recent nationally representative survey on smoking prevalence, collected as part of the MPOWER report population data for 2010 from the United Nations18 by age and gender and policy data from MPOWER reports.6 We used the 2013 MPOWER report for the policy level, but checked earlier reports (including the 2008 report) for recent changes in policy. We use World Fact book19 data on the percent of the population employed in agriculture to calculate the urban adjustor and on income to determine whether the country is high, medium or low income. Sources are presented in table 2.
Table 2.
Data used in the country models
| Country | Population (source) | Income status | Percentage employed in agriculture | Smoking prevalence survey* | Year | Website (smoking prevalence) |
|---|---|---|---|---|---|---|
| Egypt | 78 728 000 (Central Agency for Population Mobilisation and Statistics) | Middle | 32% | Global Adult Tobacco Survey (21 398) | 2009 | http://www.who.int/tobacco/surveillance/gats_rep_egypt.pdf |
| Lebanon | 3 759 134 (Living conditions survey) | Middle | 5% | STEPS Survey (2671) | 2009 | http://www.who.int/chp/steps/lebanon/en/index.html |
| Pakistan | 149 860 388 (UN data) | Low | 45% | World Health Survey (6472) | 2003 | http://www.who.int/healthinfo/survey/whspak-pakistan.pdf |
| Tunisia | 10 673 800 (National Institute of Statistics) | Middle | 10% | World Health Survey (5107) | 2003 | http://www.who.int/healthinfo/survey/whstun-tunisia.pdf |
Sample size is in parentheses under the survey name.
RESULTS
The results of each country’s model are presented in tables 3–6. The tables first present the initial levels for smoking prevalence (by gender) and the total number of smokers. The final column shows deaths adjusted to reflect low-income/middle-income status of all four countries. Next, the tables show the effects of each policy individually and in combination. The effects are short-term and long-term percentage reductions in smoking prevalence and the long-term effects on the number of smokers and adjusted smoking-attributable deaths.
Table 3.
Policy effects by MPOWER policy, individual and total: Egypt
| Initial smoking prevalence and deaths | Smoking prevalence
|
Number of smokers Total 10 445 839 |
Smoking-attributable deaths adjusted* Total 3 394 898 |
|
|---|---|---|---|---|
| Male 37.7% |
Female 0.5% |
|||
| Effect of policies on the status quo | ||||
| Original policy | Short-term effect size† | Long-term effect size† | Total reduction in number of smokers | Reduction in smoking attributable deaths adjusted* |
| Protect through smoke-free air laws | ||||
| Low level | −8.9% | −11.1% | 1 162 000 | 378 000 |
| Offer cessation treatments | ||||
| Low level | −2.5% | −6.3% | 658 500 | 214 000 |
| Mass media campaigns | ||||
| Low level | −5.5% | −6.6% | 689 400 | 224 100 |
| Warnings on cigarette packages | ||||
| High level | – | – | – | – |
| Enforcement of marketing restrictions | ||||
| Low level | −3.6% | −4.7% | 488 900 | 158 900 |
| Raise cigarette taxes | ||||
| Excise tax=72.5 | −1.9% | −3.8% | 397 900 | 129 300 |
| Combined policies | ||||
| −20.6% | −28.7% (−14.7%, −40.9%)‡ | 2 996 700 | 973 900 (500 000, 1 387 200)‡ | |
Smoking-attributable deaths are based on relative risks from high-income nations8 and are adjusted downward by 35% to reflect low-income or middle-income status.9,10
Short-term and long-term effect size are measured in terms of the percentage reduction in smoking prevalence from the initial prepolicy level, that is, (postpolicy smoking prevalence —prepolicy smoking prevalence)/prepolicy smoking prevalence.
The lower and upper bounds for the long-term effect size and the reduction in smoking-attributable deaths adjusted for combined policies are based on the lower and upper ranges for sensitivity analysis for each policy from table 1. For individual policies, bounds can be calculated using the ranges for that policy in table 1.
Table 6.
Policy effects by MPOWER policy, individual and total: Tunisia
| Initial smoking prevalence and deaths | Smoking prevalence
|
Number of smokers Total 2 033 300 |
Smoking-attributable deaths adjusted* Total 660 800 |
|
|---|---|---|---|---|
| Male 53.3% |
Female 1.5% |
|||
| Effect of policies on the status quo | ||||
| Original policy | Short-term effect size† | Long-term effect size† | Total reduction in number of smokers | Reduction in smoking attributable deaths adjusted* |
| Protect through smoke-free air laws | ||||
| Moderate level | −9.7% | −12.1% | 239 400 | 80 150 |
| Offer cessation treatments | ||||
| Low level | −2.7% | −6.6% | 131 000 | 43 900 |
| Mass media campaigns | ||||
| Low level | −5.5% | −6.6% | 130 300 | 43 600 |
| Warnings on cigarette packages | ||||
| Low level | −3% | −6% | 118 550 | 39 650 |
| Enforcement of marketing restrictions | ||||
| Low level | −2.8% | −3.6% | 71 900 | 24 100 |
| Raise cigarette taxes | ||||
| Excise tax=70% | −4.7% | −9.4% | 185 500 | 62 100 |
| Combined policies | ||||
| −25.4% | −37.1% (−20.9%, −50.5%)‡ | 732 800 | 245 300 (138 300, 334 000)‡ | |
Smoking-attributable deaths are based on relative risks from high-income nations8 and are adjusted downward by 35% to reflect low-income or middle-income status.9,10
Short-term and long-term effect size are measured in terms of the percentage reduction in smoking prevalence from the initial prepolicy level, that is, (postpolicy smoking prevalence—prepolicy smoking prevalence)/prepolicy smoking prevalence.
The lower and upper bounds for the long-term effect size and the reduction in smoking-attributable deaths adjusted for combined policies are based on the lower and upper ranges for sensitivity analysis for each policy from table 1. For individual policies, bounds can be calculated using the ranges for that policy in table 1.
Egypt
According to the 2013 MPOWER report, Egypt had weak worksite laws, no bans in restaurants or bars, minimal smoking cessation coverage in health treatment centres, a low-level media campaign and a partial marketing ban. Health warnings on packs meet MPOWER requirements. Excise cigarette taxes are at 72.5% with no VAT. The Egypt model uses the 2009 Global Adult Tobacco Survey, which indicated that 37.7% of men and 0.5% of women smoked cigarettes, from which the model estimates almost 3.4 million premature (adjusted) deaths of cigarette smokers alive in 2010.
In the short term, smoking prevalence would be reduced by 9% from well-enforced, comprehensive smoke-free air laws, 5.5% from a high-level media campaign, 4% from a well-enforced comprehensive marketing ban, 3% from a well-publicised and comprehensive cessation policy, and 2% from increasing excise taxes from 72.5% to 75%. With the complete set of policies implemented, the model projects that smoking prevalence would be reduced by 21% in 5 years. In the long term (40 years), the model calculated (with the upper and lower bound in parentheses) a 29% (15%, 41%) reduction in smoking prevalence within 40 years, averting almost 1 (0.5, 1.4) million deaths.
Lebanon
Lebanon has relatively strong worksite laws, moderate smoking cessation coverage in health treatment centres, a low-level media campaign, non-graphic health warnings, a partial marketing ban, and excise taxes at 33% with a 9% VAT. Based on the nationwide 2010 Lebanese National Tobacco Programme Survey, the current tobacco smoking prevalence for those of age 25–65 is 45.1% for males and 29.1% for females. For cigarette smokers of age 25 and above, nearly 300 000 premature adjusted deaths of the smokers alive in 2010 are projected.
In 5 years, Abridged SimSmoke projects that smoking prevalence would be reduced 18% by increasing excise taxes from 33% to 75%, 5.5% from a high-level media campaign, 4% by implementing comprehensive smoke-free air laws, 4% from a comprehensive marketing ban with enforcement, 3% from a well-publicised and comprehensive cessation policy and 2% from stronger health warnings. With all MPOWER policies fully implemented, the model projects that smoking prevalence would decrease by 32% in 5 years and by 52% (36%, 66%) and avert 156 000 (106 000, 196 000) deaths within 40 years.
Pakistan
Most public places in Pakistan had smoke-free laws, but minimal enforcement, smoking cessation coverage was minimal, a low-level media campaign, moderately strong health warnings and a partial marketing ban. Of the 60% of the retail price that is the tax component, 14% is VAT and 46% is excise tax. Based on the nationwide 2003 Pakistan World Health Survey, 32.4% of men and 5.5% of women smoked tobacco.
The model projects nearly 6.3 million premature deaths of the smokers alive in 2010.
In 5 years, Abridged SimSmoke projects that smoking prevalence would be reduced 20% by increasing excise cigarette taxes, 9% from a comprehensive marketing ban from enforcement, 5.5% from a high-level media campaign, 2% from a well-publicised and comprehensive cessation policy, 2% from strong health warnings and 3% by implementing comprehensive smoke-free air laws. With the stronger set of policies consistent with MPOWER requirements, the model projects that smoking prevalence would be reduced by 35% within 5 years, and by 56% (40%, 69%) and avert 3.5 (2.5, 4.3) million deaths within 40 years.
Tunisia
In Tunisia, smoking is allowed in separate areas, there is minimal smoking cessation coverage, a low-level media campaign, weak health warnings, a partial marketing ban and excise cigarette taxes are at 70% of the retail price. Based on the 2003 Tunisia World Health Survey, 53.3% of men and 1.5% of women smoked tobacco. The model projects about 661 000 premature deaths of the smokers alive in 2010.
In 5 years, Abridged SimSmoke projects that smoking prevalence will be reduced by 10% by implementing comprehensive smoke-free air laws, 5.5% with a high-level media campaign, 3% with strong health warnings, 3% with a comprehensive marketing ban with enforcement, 3% with comprehensive cessation policy and 5% by increasing excise cigarette taxes to 75%. With the complete set of policies, smoking prevalence would be reduced by 25% in 5 years, and by 37% (21%, 51%) and avert 245 000 (138 000 334 000) deaths within 40 years.
DISCUSSION
Abridged SimSmoke may serve advocacy and strategic planning purposes.20,21 For example, of the smokers alive in 2010, the model projects 2.9 million premature adjusted deaths in Egypt, 300 000 in Lebanon, 6.3 million in Pakistan and 661 000 in Tunisia, thus, demonstrating the need for potent policies. In addition, by comparing reductions in smoking prevalence and the number of smoking-attributable deaths from meeting MPOWER policies, the models show how tobacco control measures included in the WHO FCTC and MPOWER policies work and will save lives once fully implemented.22
In this paper, we show how cigarette use in four Eastern Mediterranean countries can be reduced and thus save many lives. With a complete implementation of policies, two of the four countries, Lebanon and Pakistan, will reach the goal of reducing smoking rates by 30% within the next 5 years, and Tunisia will reach the goal in about 15 years. However, Egypt will need to raise excise taxes beyond 75% to reach the 30% goal. The MPOWER policies are predicted to avert 3.5 million deaths in Pakistan alone.
The full implementation of the WHO FCTC requires a whole-governmental approach and is not limited to the ministry of health as the lead agency in tobacco control at a country level.23 Legislative changes must be in line with the maximum measures of the WHO FCTC and the MPOWER policies with continued monitoring of compliance. The anticipated benefit predicted by Abridged SimSmoke will take place only if the legislation is fully implemented.
Abridged SimSmoke can also play an important role in planning by predicting the effects of specific policies before an actual expenditure of funds is required to implement policies. By examining the relative reduction in smoking prevalence from implementing different policies, policies can be prioritised. Increasing tax rates should be a priority in Pakistan and Lebanon, while smoke-free air laws should be a priority in Egypt and Tunisia. Cessation treatment policies and mass media campaigns play an important role in all four countries.
Limitations
Abridged SimSmoke has been developed based on an extensively validated simulation model, providing support for our estimates. The model has been found to predict well by age and gender for countries that have and have not implemented many strong policies.11–17 We were able to validate the complete model for Egypt, where the complete model predicted the smoking prevalence as 37.6% for men compared to 37.5% from the GATS data and 0.5% for women compared to 0.5% from GATS.
To explicitly consider the predictions of the abridged model, we have previously compared predictions from the unabridged SimSmoke for nine countries that have reached MPOWER goals to results from complete SimSmoke models for those countries and found that the results predicted by the Abridged SimSmoke for smoking prevalence and deaths were reasonably close to the reported findings from the complete model.5 For the future projection model presented here, we compared projections from two abridged model to two complete SimSmoke models. For Egypt, we found that the abridged model over-predicted smoking-attributable deaths by about 10%, but the predicted per cent reductions in smoking prevalence and the change in smoking-attributable deaths was within 5% for all policies, except cessation treatment policies. For Pakistan, the level of smoking attributable deaths was within 5%, and the predicted changes in smoking prevalence and smoking-attributable deaths were within 5% for the policies individually and combined. Nevertheless, the findings from the Abridged SimSmoke should be interpreted in light of the model’s limitations.
Abridged SimSmoke does not incorporate changes in demographics or smoking prevalence nor the effects of recent policy changes. The abridged model utilises data from the most recent year for which smoking prevalence data are available. It does not incorporate changes in smoking trends, including those that may be influenced by policies implemented just prior to the survey year. In addition, the model only attempts to incorporate the effects of policies on those who were smokers in the survey year, and does not incorporate the effect of any policy that have been implemented since that year. The model does not include people who may initiate smoking in future years (in the absence of strong policies) and, therefore, it does not incorporate any benefits of newly implemented policies from reducing future initiation.
Smoking prevalence data for Pakistan and Tunisia were from 2003. For Tunisia, a 2005 survey reports a higher rate for women (8%), but a lower rate for men (48%) than the survey we used. However, the survey interviewed only those in the age group 35–70. More recent data is needed for surveillance in these countries. For Egypt and Lebanon, more recent data has been used, but it will be important to examine recent trends in smoking prevalence and changes in policies that may have affected these trends. For example, if the smoking prevalence (especially those of age 18–24) is decreasing in recent years, then our results may not incorporate the benefits from newly implemented policies that already reduced the higher prevalence rates.
The model developed here only applies to cigarettes and does not incorporate shisha (water pipe) use, which is highly prevalent in the region,24 or smokeless tobacco use. In Lebanon, 20% of tobacco users smoke shisha and in Pakistan, 27% of males and 4% of females use smokeless tobacco.25 If tax increases and other policies are only directed at cigarette smokers, there may be a substitution toward greater usage of other tobacco products. While these products may have less adverse health effects than cigarettes,26 the health gains from reduced cigarette-oriented policies will be partially offset if smokers who quit cigarettes begin or continue to use more of these products. By directing policies (eg, media campaigns) at non-cigarette products, some of the substitution into those products may be avoided.
We use relative risks from high-income nations. For low-income and middle-income countries, premature deaths of the smokers themselves may be lower than projected due to higher background health risks, from initiating cigarette smoking at later ages and from smoking fewer cigarettes per day. Consequently, we have adjusted downward smoking-attributable deaths for these countries. However, smoking has a long tradition in Eastern Mediterranean countries and as these countries move to higher income levels, the higher relative risk of smokers in high-income countries becomes increasingly relevant. Furthermore, two recent studies27,28 found that about 65% rather than half of deaths of current smokers are attributable to smoking. In addition, we have not included deaths due to secondhand smoke and the effect of smoking on maternal and child health outcomes, and we have not estimated the cost saving from each policy relative to the costs of implementation.
Abridged SimSmoke has been developed to use data from the biennial WHO MPOWER Reports. The MPOWER policy data are restricted to a specific set of policies and definition for each policy. The model does not consider policies directed at price minimising behaviour, enforcement against smuggling, product regulation and youth access policies. The MPOWER policy definitions may not incorporate relevant components in gauging policy effectiveness, such as potential effectiveness of media in reaching the smoking population. The MPOWER measures of enforcement level for smoke-free air laws and marketing bans are based on laws surrounding enforcement; alternative measures are exposure to secondhand smoke and to advertising.
CONCLUSIONS
Abridged SimSmoke shows that the required MPOWER tobacco control policies will save lives and will eventually control tobacco use. The model enables the user to consider policies individually and in combination to observe how policies in different combinations lead to reductions in smoking prevalence and smoking attributable deaths, and translates empirical information into a user-friendly format that can be easily interpreted. While recognising the limitations of the model, SimSmoke projections can be used to justify the need for policies, and provide information for planning and implementing public health interventions.20,21
Table 4.
Policy effects by MPOWER policy, individual and total: Lebanon
| Initial smoking prevalence and deaths | Smoking prevalence
|
Number of smokers Total 582 100 |
Smoking-attributable deaths adjusted* Total 298 200 |
|
|---|---|---|---|---|
| Male 45.1% |
Female 29.1% |
|||
| Effect of policies on the status quo | ||||
| Original policy | Short-term effect size† | Long-term effect size† | Total reduction in number of smokers | Reduction in smoking attributable deaths adjusted* |
| Protect through smoke-free air laws | ||||
| Low level | −3.9% | −4.9% | 45 200 | 14 700 |
| Offer cessation treatment | ||||
| Low level | −3.2% | −8.1% | 74 300 | 24 200 |
| Mass media campaigns | ||||
| Low level | −5.5% | −6.6% | 60 600 | 19 700 |
| Warnings on cigarette packages | ||||
| Moderate level | −2.0% | −4.0% | 36 700 | 11 900 |
| Enforcement of marketing restrictions | ||||
| High, but low compliance | −3.6% | −4.7% | 42 900 | 14 000 |
| Raise cigarette taxes | ||||
| Excise tax=33% | −18.1% | −36.3% | 332 800 | 108 200 |
| Combined policies | ||||
| −32.1% | −52.4% (−35.6%, −65.8%)‡ | 481 000 | 156 300 (106 200, 196 200)‡ | |
Smoking-attributable deaths are based on relative risks from high-income nations8 and are adjusted downward by 35% to reflect low-income or middle income status.9,10
Short-term and long-term effect size are measured in terms of the percentage reduction in smoking prevalence from the initial prepolicy level, that is, (postpolicy smoking prevalence —prepolicy smoking prevalence)/prepolicy smoking prevalence.
The lower and upper bounds for the long-term effect size and the reduction in smoking-attributable deaths adjusted for combined policies are based on the lower and upper ranges for sensitivity analysis for each policy from table 1. For individual policies, bounds can be calculated using the ranges for that policy in table 1.
Table 5.
Policy effects by MPOWER policy, individual and total: Pakistan
| Initial smoking prevalence and deaths | Smoking prevalence
|
Number of smokers total Total 19 341 200 |
Smoking-attributable deaths adjusted* Total 6 285 900 |
|
|---|---|---|---|---|
| Male 32.4% |
Female 5.5% |
|||
| Effect of policies on the status quo | ||||
| Original policy | Short-term effect size† | Long-term effect size† | Total reduction in number of smokers | Reduction in smoking attributable deaths adjusted* |
| Protect through smoke-free air laws | ||||
| High, but low compliance | −2.6% | −3.2% | 623 300 | 202 600 |
| Offer cessation treatment | ||||
| Low level | −1.6% | −4.1% | 785 600 | 255 300 |
| Mass media campaigns | ||||
| Low level | −5.5% | −6.6% | 1 276 500 | 414 900 |
| Warnings on cigarette packages | ||||
| Moderate level | −2% | −4% | 773 600 | 251 400 |
| Enforcement of marketing restrictions | ||||
| Low level | −8.7% | −11.3% | 2 187 500 | 710 900 |
| Raise cigarette taxes | ||||
| Excise Tax=46.2% | −20.2% | −40.3% | 7 794 700 | 2 533 300 |
| Combined policies | ||||
| −35.3% | −55.9% (−39.9%, −69.2%)‡ | 10 815 900 | 3 515 200 (2 506 100, 4 346 700)‡ | |
Smoking-attributable deaths based on relative risks from high-income nations8 and are adjusted downward by 35% to reflect low-income or middle-income status.9,10
Short-term and long-term effect size are measured in terms of the percentage reduction in smoking prevalence from the initial prepolicy level (ie, (postpolicy smoking prevalence—postpolicy smoking prevalence)/postpolicy smoking prevalence).
The lower and upper bounds for the long-term effect size and the reduction in smoking-attributable deaths adjusted for combined policies are based on the lower and upper ranges for sensitivity analysis for each policy from table 1. For individual policies, bounds can be calculated using the ranges for that policy in table 1.
What this paper adds.
The WHO established the MPOWER policy package to boost the implementation of the WHO Framework Convention for Tobacco Control (WHO FCTC) in 2008. An easily applied Abridged SimSmoke was developed to help countries gauge the effect of MPOWER policies using data from the WHO MPOWER/WHO Report.
The Abridged SimSmoke model is used to show the reduction in smoking prevalence and the number of deaths from smoking and how MPOWER policies can be used to reach the WHO non-communicable deaths voluntary target for cigarette use reduction. The model is applied to four countries in the WHO Eastern Mediterranean Region.
Acknowledgments
Funding WHO-EMRO (Cairo) and Tobacco Control Research Branch, National Cancer Institute, National Institutes of Health (USA).
Footnotes
Contributors DTL was involved in every stage of the development of the model, writing and revision of the paper. HF was involved in the development of the model and writing of the paper. JL inputted data into the model, ran the model and wrote the initial version of the results section of the paper. ADD checked the model results, participated in the writing of the paper and the revisions. FE-A helped in the development of the model and writing of the paper.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement The abridged model and user’s manual may become available through the journal website.
References
- 1.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. WHO discussion paper: a comprehensive global monitoring framework and voluntary global targets for the prevention and control of NCDs. Comprehensive global monitoring framework including indicators and a set of voluntary global targets for the prevention and control of NCD. [accessed 2 Jan 2014];2012 Apr; 2013 http://www.who.int/nmh/events/2012/consultation_april_2012/en/
- 3.World Health Organization. WHO Report on the Global Tobacco Epidemic, 2008: The MPOWER package. Geneva: World Health Organization; 2008. [accessed 2 Oct 2013]. http://www.who.int/tobacco/global_report/2008/en/ [Google Scholar]
- 4.Levy DT, Gitchell JG, Chaloupka F. The effects of tobacco control policies on smoking rates: a tobacco control scorecard. J Public Health Manag Pract. 2004;10:338–51. doi: 10.1097/00124784-200407000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Levy DT, Ellis JA, Mays D, et al. Smoking-related deaths averted due to three years of policy progress. Bull World Health Organ. 2013;91:509–18. doi: 10.2471/BLT.12.113878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. WHO report on the global tobacco epidemic, 2013: enforcing bans on tobacco advertising, promotion and sponsorship. Geneva: World Health Organization; 2013. [accessed 2 Oct 2013]. http://www.who.int/tobacco/global_report/2013/en/ [Google Scholar]
- 7.Levy DT, Cummings KM, Hyland A. Increasing taxes as a strategy to reduce cigarette use and deaths: results of a simulation model. Prev Med. 2000;31:279–86. doi: 10.1006/pmed.2000.0696. [DOI] [PubMed] [Google Scholar]
- 8.Doll R, Peto R, Boreham J, et al. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ. 2004;328:1519. doi: 10.1136/bmj.38142.554479.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jee SH, Lee JK, Kim IS. Smoking-attributable mortality among Korean adults: 1981–2003. Korean J Epidemiol. 2006;28:92–9. doi: 10.4178/epih.e2024011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wen CP, Tsai SP, Chen CJ, et al. The mortality risks of smokers in Taiwan; Part I: cause-specific mortality. Prev Med. 2004;39:528–35. doi: 10.1016/j.ypmed.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 11.Levy D, Benjakul S, Ross H, et al. The role of tobacco control policies in reducing smoking and deaths in a middle income nation: results from the Thailand SimSmoke simulation model. Tob Control. 2008;17:53–9. doi: 10.1136/tc.2007.022319. [DOI] [PubMed] [Google Scholar]
- 12.Levy DT, Hyland A, Higbee C, et al. The role of public policies in reducing smoking prevalence in California: results from the California tobacco policy simulation model. Health Policy. 2007;82:167–85. doi: 10.1016/j.healthpol.2006.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Levy D, Rodriguez-Buno RL, Hu TW, et al. The potential effects of tobacco control in China: projections from the China SimSmoke simulation model. BMJ. 2014;348:g1134. doi: 10.1136/bmj.g1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levy DT, Blackman K, Currie LM, et al. Germany SimSmoke: the effect of tobacco control policies on future smoking prevalence and smoking-attributable deaths in Germany. Nicotine Tob Res. 2013;15:465–73. doi: 10.1093/ntr/nts158. [DOI] [PubMed] [Google Scholar]
- 15.Levy D, de Almeida LM, Szklo A. The Brazil SimSmoke policy simulation model: the effect of strong tobacco control policies on smoking prevalence and smoking-attributable deaths in a middle income nation. PLoS Med. 2012;9:e1001336. doi: 10.1371/journal.pmed.1001336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Levy DT, Currie L, Clancy L. Tobacco control policy in the UK: blueprint for the rest of Europe? Eur J Public Health. 2013;23:201–6. doi: 10.1093/eurpub/cks090. [DOI] [PubMed] [Google Scholar]
- 17.Levy DT, Huang AT, Currie LM, et al. The benefits from complying with the framework convention on tobacco control: a SimSmoke analysis of 15 European nations. Health Policy Plan. 2014;29:1031–42. doi: 10.1093/heapol/czt085. [DOI] [PubMed] [Google Scholar]
- 18.United Nations. World Population Prospects 2012 Revision. United Nations. New York: Department of Economic and Social Affairs, Population Division; 2013. [accessed 3 Jan 2014]. http://esa.un.org/unpd/wpp/Excel-Data/population.htm. [Google Scholar]
- 19.Central Intelligence Agency. [accessed 3 Jan 2014];World Factbook. 2014 http://www.theodora.com.
- 20.Levy DT, Bauer JE, Lee HR. Simulation modeling and tobacco control: creating more robust public health policies. Am J Public Health. 2006;96:494–8. doi: 10.2105/AJPH.2005.063974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Levy DT, Chaloupka F, Gitchell J, et al. The use of simulation models for the surveillance, justification and understanding of tobacco control policies. Health Care Manag Sci. 2002;5:113–20. doi: 10.1023/a:1014476916361. [DOI] [PubMed] [Google Scholar]
- 22.Fouad H, El Awa F, Naga RA, et al. Prevalence of tobacco use among adults in Egypt. Global Health Promot. 2009 doi: 10.1177/1757975913499801. Published Online First: 16 September 2013. [DOI] [PubMed] [Google Scholar]
- 23.El Awa F. The WHO Framework Convention on Tobacco Control as a tool for advancing health promotion: perspective from the Eastern Mediterranean Region. Global Health Promotion. 2010;17(1 Suppl):60–6. doi: 10.1177/1757975909358252. [DOI] [PubMed] [Google Scholar]
- 24.Morton J, Song Y, Fouad H, et al. Cross-country comparison of waterpipe use: nationally representative data from 13 low and middle-income countries from the Global Adult Tobacco Survey (GATS) Tob Control. 2014;23:419–27. doi: 10.1136/tobaccocontrol-2012-050841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sreeramareddy CT, Pradhan PMS, Al MIr I, et al. Smoking and smokeless tobacco use in nine South and Southeast Asian countries: prevalence estimates and social determinants from Demographic and Health Surveys. Popul Health Metr. 2014;12:22. doi: 10.1186/s12963-014-0022-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Critchley JA, Unal B. Health effects associated with smokeless tobacco: a systematic review. Thorax. 2003;58:435–43. doi: 10.1136/thorax.58.5.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jha P, Ramasundarahettige C, Landsman V, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368:341–50. doi: 10.1056/NEJMsa1211128. [DOI] [PubMed] [Google Scholar]
- 28.Thun MJ, Carter BD, Feskanich D, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med. 2013;368:351–64. doi: 10.1056/NEJMsa1211127. [DOI] [PMC free article] [PubMed] [Google Scholar]