Abstract
Endobronchial ultrasound (EBUS) imaging is commonly used to evaluate and aid in biopsy of mediastinal lymph nodes. Pulmonary arteries are readily viewable with this type of imaging modality. We present a case report of a pulmonary embolism (PE) diagnosed by EBUS. Our patient had no smoking history and presented with respiratory and constitutional symptoms, urinary retention, and leg weakness suspicious for malignancy with metastasis to spine. Chest computed tomography (CT) was suggestive of lung carcinoma and specifically showed no PE. EBUS with TBNA was requested for tissue diagnosis. A mobile filling defect consistent with a PE was observed and reported to primary team. Follow-up chest CT showed an acute PE which confirmed the diagnosis originally made by EBUS. Bronchoscopists should be aware of potential to diagnose a PE while performing EBUS. Additionally, there may be a role in using EBUS specifically to diagnose a PE in the right patient population.
Keywords: Pulmonary embolus, Endobronchial ultrasound
Abbreviations: EBUS, Endobronchial ultrasound; TBNA, Transbronchoscopic needle aspiration; PE, Pulmonary embolism
1. Introduction
Endobronchial ultrasound (EBUS) imaging is commonly performed as an adjunct to transbronchoscopic needle aspiration (TBNA) of mediastinal and hilar lymph nodes to diagnose and stage malignancy. While the usual focus of EBUS examination is guidance of TBNA, major vascular structures like the pulmonary arteries are also imaged. Bronchoscopists therefore have the potential opportunity to diagnose pulmonary embolisms (PEs). We present a case report of a PE diagnosed by EBUS.
2. Case report
A 56 year old male without a past smoking history presented to the emergency department with upper respiratory symptoms, fevers, night sweats, urinary retention, and leg weakness. On admission, chest computed tomography (CT) with contrast demonstrated a right perihilar mass with mediastinal extension, prominent mediastinal and paraesophageal lymphadenopathy, and was negative for PE (Fig. 1). Based on focal neurologic findings, magnetic resonance imaging of the head/spine was performed and showed lesions consistent with metastatic disease. Because the clinical-radiographic diagnosis suggested metastatic carcinoma, bronchoscopy with EBUS-guided TBNA of the invasive mediastinal mass was performed. EBUS imaging from the right main stem bronchus demonstrated a mobile filling defect within the right pulmonary artery (Fig. 2) which was confirmed by Doppler (Fig. 3). These characteristics were consistent with a PE. A repeat chest CT with contrast confirmed an acute PE involving the right main pulmonary artery and bilateral segmental pulmonary arteries (Fig. 4). The patient was treated with the preferred anticoagulation in the setting of malignancy; subcutaneous low molecular weight heparin [1]. Pathology from the TBNA biopsy was positive for primary lung adenocarcinoma and the patient was initiated on systemic chemotherapy. Follow-up CT angiogram 3-months later showed resolution of the PE and tumor response to chemotherapy.
Fig. 1.
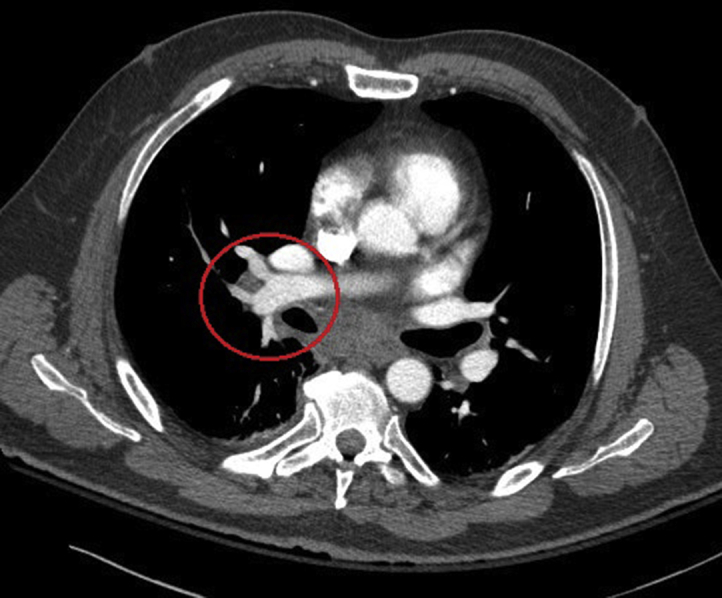
Computed tomography of the chest without a pulmonary embolus obtained prior to the EBUS.
Fig. 2.

Endobronchial ultrasound diagnosing the pulmonary embolus.
Fig. 3.
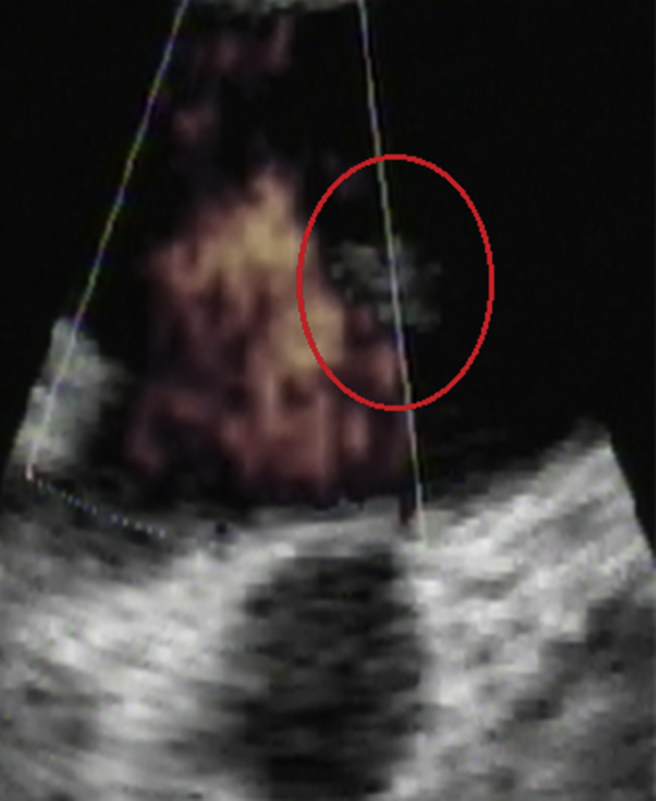
Endobronchial ultrasound diagnosing the pulmonary embolus confirmed by Doppler.
Fig. 4.
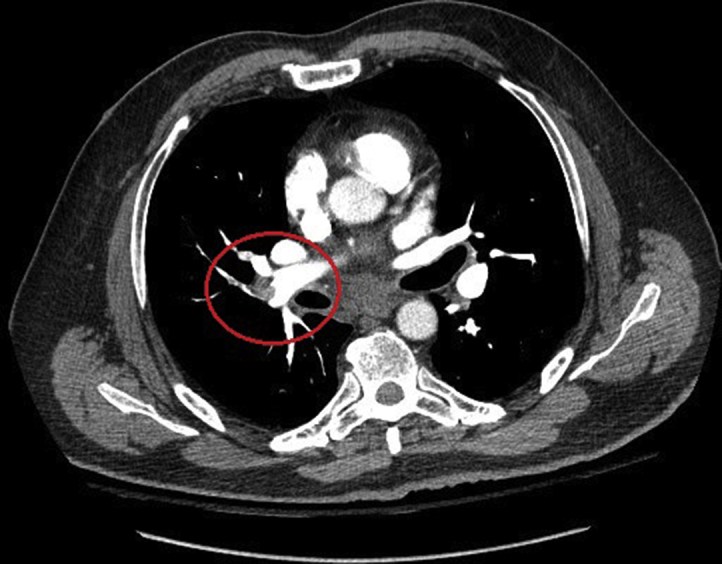
Computed tomography of the chest confirming the pulmonary embolus that was originally diagnosed by EBUS.
3. Discussion
Pulmonary thromboembolism has an incidence up to 15% in patients with malignancy and may present with symptoms indistinguishable from thoracic malignancy. Despite the high prevalence and clinical importance of PE in this patient population, it has historically eluded prompt diagnosis [2], [3]. Our patient had a PE initially diagnosed through EBUS imaging which identified a filling defect within the pulmonary arteries. The diagnosis of acute PE was then confirmed by CT angiography.
Bronchoscopists should be aware of the potential to identify vascular filling defects at EBUS imaging and consider the diagnosis of a PE. CT angiography is usually the preferred method for diagnosing a PE except in certain patient populations including those with iodine contrast allergy, impaired renal function, women of reproductive age, pregnancy, or those in extremis [4]. In addition to the possibility of EBUS diagnosing a PE while performing TBNA, there may be a role for using EBUS specifically to diagnose a PE. This would not be practical in the general population because of the cost and invasiveness, but consideration should be given to the potential for its use in future practice in the right subpopulation.
Summary conflict of interest statements
Justin M. Segraves and Craig E. Daniels have no conflicts of interest to report.
Funding information
No funding sources to report.
Notation of prior abstract publication/presentation
Pulmonary Embolus Diagnosed by Endobronchial Ultrasound case report poster presented at American Thoracic Society International Conference May 18th, 2015 in Denver, Colorado.
Contributor Information
Justin M. Segraves, Email: segraves.justin@mayo.edu.
Craig E. Daniels, Email: daniels.craig@mayo.edu.
References
- 1.Imberti Treatment of venous thromboembolism in patients with cancer: guidelines of the Italian society for haemostasis and thrombosis (SISET) Thromb. Res. 2009;124:e32–e40. doi: 10.1016/j.thromres.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Shinagare Incidence of pulmonary embolism in oncologic outpatients at a tertiary cancer center cancer. Cancer. 2011;117(16):3860–3866. doi: 10.1002/cncr.25941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tiseo Asymptomatic pulmonary embolism in lung cancer: prevalence and analysis of clinical and radiological characteristics in 141 outpatients. Tumori. 2012;98(5):594–600. doi: 10.1177/030089161209800509. [DOI] [PubMed] [Google Scholar]
- 4.Stein Diagnostic pathways in acute pulmonary embolism: recommendations of the PIOPED II investigators. Am. J. Med. 2006;119(12):1048–1055. doi: 10.1016/j.amjmed.2006.05.060. [DOI] [PubMed] [Google Scholar]


