Abstract
Although percutaneous tracheostomy is a standardized procedure, rare major complications are still being evaluated and discussed. We describe a case of patient, with hemodynamic and respiratory stability, who displayed massive hemorrhage after 16 days of “Ciaglia Blue Rhino” tracheostomy. Unfortunately, neither prompt resuscitation maneuvers nor the surgical approach saved the life of patient.
Keywords: Percutaneous tracheostomy, Surgical tracheostomy, Indications, Complications
1. Introduction
The tracheostomy is a surgical technique that originated more than 4000 years ago [1]. The percutaneous tracheostomy in the twentieth century became a common method in the management of critical patients due to the spread of polio in the 50's. Several mini-invasive procedures has been proposed, allowing the management of serious health conditions directly at the bedside of patient. Although there are no statistically significant differences in regard to complications [2], percutaneous methods compared to the surgical approach reduce costs and time of intervention [3]. Currently, the percutaneous tracheostomy have reached a significant standard of safety and efficacy so as to restrict the indications for open surgery only to those few pathologies with reduced access to the anterior surface of the neck.
2. Case presentation
Sixty-one year-old patient arrived at the Emergency Department complaining of strong headache and vomiting. She underwent 3-dimension (3D) thin-section computed tomography (TSCT) of the brain that showed the presence of sub-arachnoid haemorrhaging and supra-infratentorial ventricular blood. The angiographic sequences of 3D-TSCT displayed two aneurysmal malformations of pericallosal artery (right and left side) and two additional aneurysms of middle cerebral artery of the left and right side. Patient carried out cerebral angiography in general anesthesia, that confirmed the presence of four aneurysmal malformations of the anterior intracranial circulation; two lesions located near the emergency of right side pericallosal artery and two additional aneurysms at the bifurcation of the two middle cerebral arteries. After careful neuroradiological and neurosurgical evaluation, it was decided to proceed with embolization of both aneurysms of the right pericallosal artery. The procedure was completed without difficulty and final inspection showed regular intracranial circulation in the absence of the brain spasm. Patient was transferred to the Department of Intensive Care for the stabilization of vital parameters. Four days after the endovascular procedure and TSCT of brain, neck and thorax with contrast she underwent percutaneous “Blue Rhino Ciaglia” tracheostomy and at day 15 she was transferred to the department of neurosurgery, conscious with valid and spontaneous breath. At day 16 the patient displayed sudden, copious and uncontrollable bleeding from the orifice of tracheotomy. Despite the attempt to vascular clamping in the anterior side of the neck and maneuvers of resuscitation, the patient died from hemorrhagic shock. Dissection up to the vascular level revealed injury of the right common carotid artery at the origin of the innominate artery (Fig. 1).
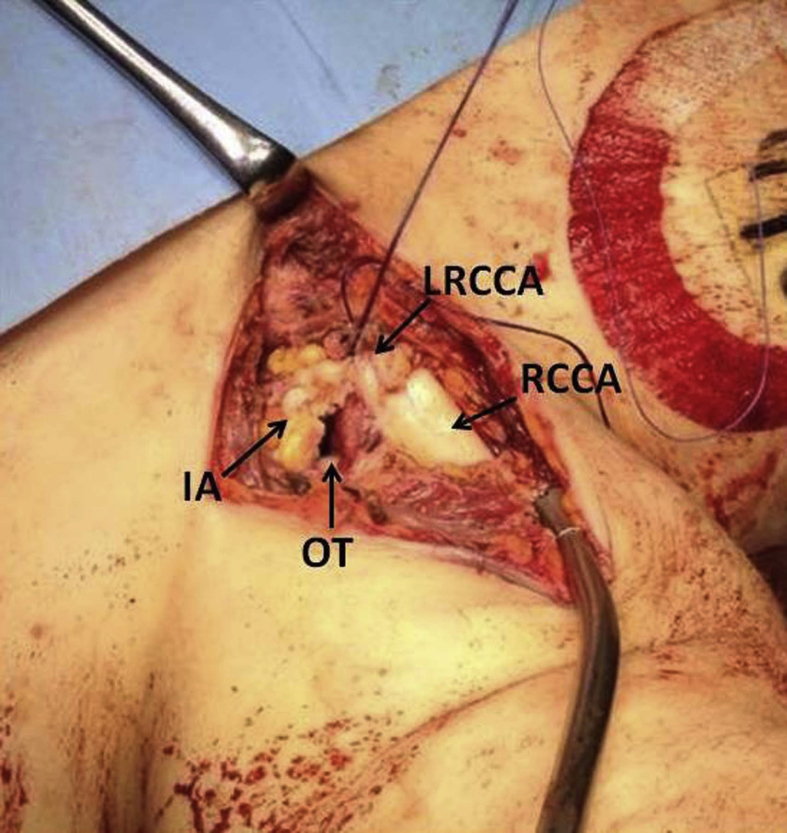
Fig. 1.
Anatomy of the surgical site, revealing the proximal displacement of the brachiocephalic trunk. RCCA: right common carotid artery; LRCCA: lesion of right common carotid artery; IA: innominate artery; OT: orifice of tracheostomy.
3. Discussion
In recent years, surgical tracheostomy has been supplanted by the different techniques of percutaneous tracheostomy [3]. This happened due to the easy execution of the procedure and the possibility of performing it outside the operating room, with significant cost savings compared to the traditional method. It has been widely demonstrated that perioperative complications between the minimally invasive and open approaches seem to balance out but are unclear what the indications for one or the other technique are, the ideal timing for performing such procedures and which radiological evaluations are essential to prevent morbidity [4]. In our case the upwards dislocation of the aortic arch and innominate artery, not highlighted by the TSCT of the thorax before intervention, explains the delayed lethal complication likely due to injury of the vessel through contact with the cannula. The diagnostic failure of computed tomography may be due: a) a misinterpretation of vascular topography linked to the marked kyphosis of the dorsal spine; b) a shift in cranial vessels secondary to upper mediastinal adhesions, based on prolonged mechanical ventilation beyond the first week. Rajajee et al. [5] performed the percutaneous tracheostomy under ultrasound guidance in 13 patients in order to avoid vascular structures during the needle path and to allow the appropriate placement of tracheal tube at targeted distance from vessels. This latter assumption is on the basis of surgical tracheostomy that would ensure the correct positioning of the cannula without risk of chafing and subsequent vessel lesion. In fact, the careful dissection of the neck structures would have highlighted the right common carotid artery at the basis of the cervical trachea advising the continuation of tracheal intubation or the application of a patch reinforcement around the vascular wall. Thus, percutaneous tracheostomy cannot be considered the first line technique in any situation of prolonged mechanical ventilation as the perfect anatomical dissection guaranteed by traditional surgical method reduces the chances of major complications. Therefore, it is obvious to ask who should lead to the indication of one method over the other. We believe that the choice of the technique to be employed must always start from the thoracic surgeon or otolaryngologist, with solid experience in tracheal surgery in order to minimize the risk of injury due to an inappropriate initial approach. We consider it incorrect to leave the tracheostomy management exclusively to the anesthesiologist or intensivist. The ideal condition would be a multidisciplinary briefing, which also includes the radiologist in order to plan the most suitable tracheostomy procedure step-by-step. Our negative finding shows that the use of a surgical tracheostomy should not be considered only in case of contraindication to percutaneous. Furthermore, anyone starting a minimally invasive tracheal approach should have extensive surgical and interventional experience.
Conflict of interest
None declared.
References
- 1.Szmuk P., Ezri T., Evron S., Roth Y., Katz J. A brief history of tracheostomy and tracheal intubation from the bronze age to the space age. Intensive Care Med. 2008;34:222–228. doi: 10.1007/s00134-007-0931-5. [DOI] [PubMed] [Google Scholar]
- 2.Sue R.D., Susanto I. Long-term complications of artificial airways. Clin. Chest Med. 2003;24:457–471. doi: 10.1016/s0272-5231(03)00048-0. [DOI] [PubMed] [Google Scholar]
- 3.Divisi D., Altamura G., Di Tommaso S., Di Leonardo G., Rosa E., De Sanctis C., Crisci R. Fantoni translaryngeal tracheostomy versus Ciaglia Blue Rhino percutaneous tracheostomy: a retrospective comparison. Surg. Today. 2009;39:387–392. doi: 10.1007/s00595-008-3899-z. [DOI] [PubMed] [Google Scholar]
- 4.De Leyn P., Bedert L., Delcroix M., Depuydt P., Lauwers G., Sokolov Y., Van Meerhaeghe A., Van Schil P. Tracheotomy: clinical review and guidelines. Eur. J. Cardiothorac. Surg. 2007;32:412–421. doi: 10.1016/j.ejcts.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 5.Rajajee V., Fletcher J.J., Rochlen L.R., Jacobs T. Real-time ultrasound-guide percutaneous dilatational tracheostomy: a feasibility study. Crit. Care. 2011;15:R67. doi: 10.1186/cc10047. [DOI] [PMC free article] [PubMed] [Google Scholar]