Abstract
Primary effusion lymphoma (PEL) is a subtype of non-Hodgkin lymphoma that presents as serous effusions without detectable masses or organomegaly. Here we report a case of PEL-like lymphoma in a patient with past asbestos exposure. A 65-year-old man was referred to our hospital due to dyspnea upon exertion. He had been exposed to asbestos for three years in the construction industry. Chest X-ray and CT images demonstrated left pleural effusion. Cytological analysis of the pleural effusion revealed large atypical lymphocytes with distinct nuclear bodies and high nucleus-to-cytoplasm ratio. Immunohistochemical analyses showed that the cells were CD20+, CD3−, CD5−, and CD10−. These findings led to a diagnosis of diffuse large B-cell lymphoma. PEL or PEL-like lymphoma should be considered a potential cause of pleural effusion in subjects with past asbestos exposure.
Keywords: Asbestos, Lymphoma, Mesothelioma, Pleural effusion, Thoracoscopy
Abbreviations: PEL, primary effusion lymphoma; HHV, human herpesvirus; CT, computed tomography; DLBCL, diffuse large B-cell lymphoma
1. Introduction
Primary effusion lymphoma (PEL) is a subtype of non-Hodgkin lymphoma that presents as serous effusions without detectable masses or organomegaly. PEL usually occurs in the setting of immunodeficiency and is associated with human herpesvirus (HHV) - 8. Here we report a case of PEL-like lymphoma in a subject with a history of asbestos exposure.
2. Case report
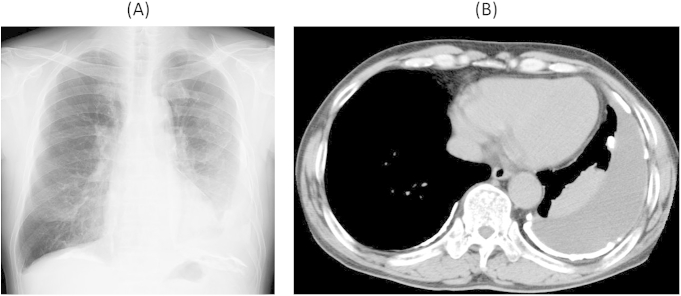
A 65-year-old man was referred to our hospital due to dyspnea upon exertion. He was an occasional smoker and had been exposed to asbestos from 18 to 20 years old while employed in the construction industry, cutting asbestos-containing building material. Chest X-ray showed left pleural effusion (Fig. 1A), and computed tomographic (CT) images revealed left pleural effusion and calcified pleural plaques without pleural tumor (Fig. 1B). Thoracoscopic exploration revealed red–brown pleural effusion and plaques, but no tumor was detected on the pleura. Culture of the pleural effusion was negative, and cytological examination revealed a cellular distribution of 1.0% macrophages, 1.5% neutrophils, and 97.5% lymphocytes. Other examinations of the fluid showed nonspecific findings. Pleural biopsy showed no evidence of malignancy.
Fig. 1.
Left pleural effusion and calcified pleural plaques visible on chest X-ray (A) and computed tomographic (B) images.
During follow-up, the patient repeatedly exhibited accumulation of left pleural effusion, which was treated each time with thoracentesis. Four years after the first admission, analysis of pleural effusion from the fourth thoracentesis revealed large atypical lymphocytes with distinct nuclear bodies and a high nucleus-to-cytoplasm ratio (Fig. 2). Malignant lymphoma was suspected and thoracoscopic pleural biopsy was performed again, and the biopsy specimen from the fibrin tissues attached to the parietal pleura showed several groups of small round atypical lymphocytes. All of acid-fast bacteria stain, PCR analysis of tuberculosis, and culture for acid fast bacillus were negative. A culture test for standard plate count bacteria was also negative. Immunohistochemical analyses revealed that these cells were CD20+ (Fig. 3), CD3−, CD5−, and CD10−. Based on these findings, the diagnosis was confirmed as diffuse large B-cell lymphoma (DLBCL). Contrast-enhanced CT imaging of whole body (neck to pelvis) revealed no lymphadenopathy or tumor. Serological tests for hepatitis-C virus, human T-cell lymphoma virus-1, and Epstein–Barr virus were negative, as was the immunohistochemical analysis for HHV8. The patient has been followed-up, and has shown no disease progression for 3 years.
Fig. 2.
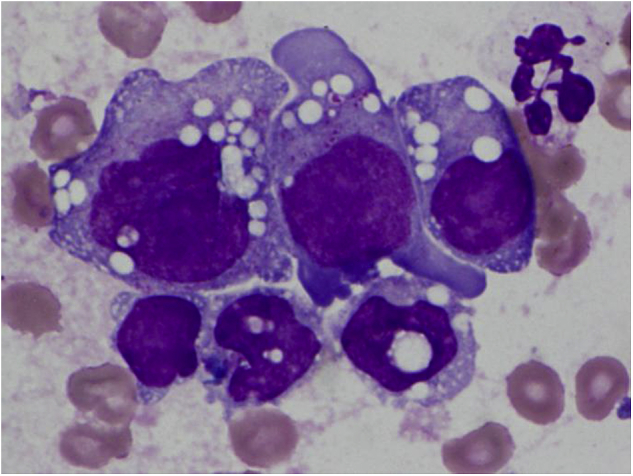
Cytological analysis of pleural effusion revealed large atypical lymphocytes with distinct nuclear body and high nucleus-to-cytoplasm ratio (×40).
Fig. 3.
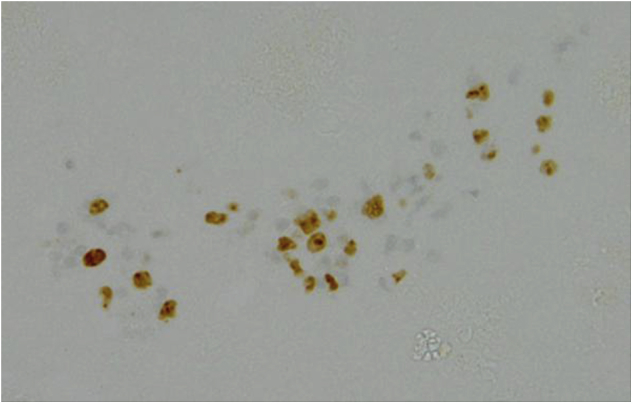
Immunohistochemical analyses revealed that the cells were CD20+ (×10).
3. Discussion
The 2001 World Health Organization classification defines PEL as a disease entity representing a part of diffuse large B-cell lymphoma [1]. PEL is commonly associated with HHV8 infection [2]; however, PEL-like disease processes have recently been reported in HHV8-negative patients. Those cases are considered a rare disease entity called HHV8-unrelated PEL-like lymphoma [3]. Advanced age [4] remains the only known risk factor for PEL-like lymphoma, and the pathogenic mechanisms remain unclear. It has been reported that patients with HHV8-unrelated PEL-like lymphoma show better outcomes than patients with PEL [5].
In our present case, the patient was elderly and had a past occupational history of asbestos exposure, but showed no immunological deterioration. To our knowledge, this is the first report of PEL-like lymphoma in a subject with past asbestos exposure. While no association has been established between lymphoproliferative disorder and asbestos exposure, it is possible that asbestos-induced chronic inflammation, in addition to advanced age, may have triggered lymphoproliferative disorder in the current case, though we cannot deny the possibility that the disease developed independently, considering relative short term of asbestos exposure.
In conclusion, here we report a rare manifestation of PEL-like lymphoma from a subject with past asbestos exposure. Subjects with past asbestos exposure sometimes develop pleural effusion, and suspected diagnoses include malignant pleural mesothelioma, lung cancer, benign asbestos pleural effusion, or tuberculous pleuritis. Our present case suggests that PEL or PEL-like lymphoma should also be considered as a potential cause of pleural effusion in subjects with past asbestos exposure.
Conflict of interest
I declare on behalf of my co-authors and myself that we do not have any conflict of interest to declare.
Source of funding
This study was supported by Research and Development and the Dissemination of Projects Related to the Nine Fields of Occupational Injuries and Illnesses of the Japan Labour Health and Welfare Organization. This work is also supported by grants-in-aid from the Ministry of Health, Labor and Welfare (grant number: 150401-02), Japan. These study sponsors had no involvement in study design, writing of the manuscript, the collection of data, and decision to submit the manuscript.
References
- 1.Banks P.M., Warnke R.A. Primary effusion lymphoma. In: Jaffe E.S., Harris N.L., Stein H., Verdiman J.W., editors. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of Haematopietic and Lymphoid Tissues. IARC Press; Lyon: 2001. [Google Scholar]
- 2.Karcher D.S., Alkan S. Human herpesvirus-8-associated body cavity-based lymphoma in human immunodeficiency virus-infected patients: a unique B-cell neoplasm. Hum. Pathol. 1997;28:801–808. doi: 10.1016/s0046-8177(97)90153-2. [DOI] [PubMed] [Google Scholar]
- 3.Carbone A., Gloghini A. PEL and HHV8-unrelated effusion lymphomas: classification and diagnosis. Cancer. 2008;114:225–227. doi: 10.1002/cncr.23597. [DOI] [PubMed] [Google Scholar]
- 4.Mohammad F., Siddique M.N., Siddiqui F., Popalzai M., Asgari M., Odaimi M. A unique case of malignant pleuropericardial effusion: HHV-8-unrelated PEL-like lymphoma-a case report and review of the literature. Case Rep. Oncol. Med. 2014:436821. doi: 10.1155/2014/436821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kobayashi Y., Kamitsuji Y., Kuroda J., Tsunoda S., Uoshima N., Kimura S. Comparison of human herpes virus 8 related primary effusion lymphoma with human herpes virus 8 unrelated primary effusion lymphoma-like lymphoma on the basis of HIV: report of 2 cases and review of 212 cases in the literature. Acta Haematol. 2007;117:132–144. doi: 10.1159/000097460. [DOI] [PubMed] [Google Scholar]