Abstract
Chronic cough that is dry, non-productive and without constitutional symptoms is often thought to have a non-malignant etiology such as asthma, post-nasal drip or gastroesophageal reflux disease (GERD). We present a case of a patient with a 3 year history of ‘chronic cough’ that was dry, non-productive cough and without any constitutional symptoms. Initial chest x-ray (CXR) done 3 years ago showed some streaky atelectasis in the right middle lobe along with some volume loss on that side. Another CXR performed one and half years later showed progression to a complete right middle lobe collapse. She ultimately presented to our facility a year later with stable CXR findings, but persistent cough. A chest CT scan was suspicious for a right lower lobe mass. A PET scan subsequently confirmed a hypermetabolic right hilar mass causing extrinsic compression of the bronchus intermedius. She ultimately required a complete right pneumonectomy with partial pericardiectomy and had complete resolution of her cough. This case highlights the fact that ‘chronic cough’ should always be thoroughly investigated and should remain a diagnosis of exclusion until all sinister pathologies have been ruled out.
Keywords: Chronic cough, Lung cancer, Lung adenocarcinoma
1. Case
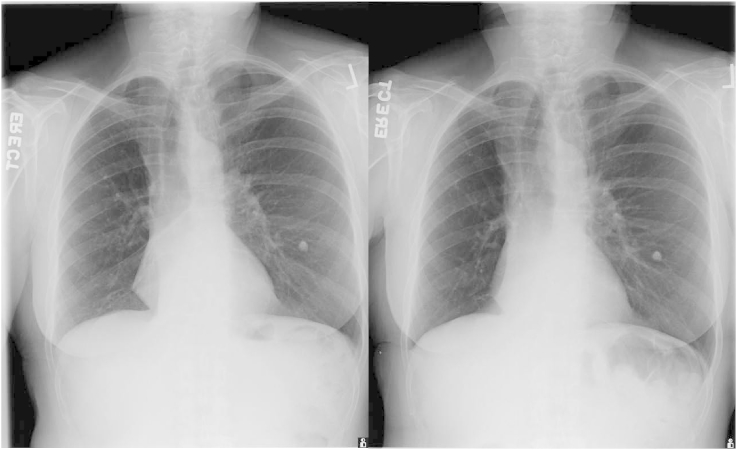
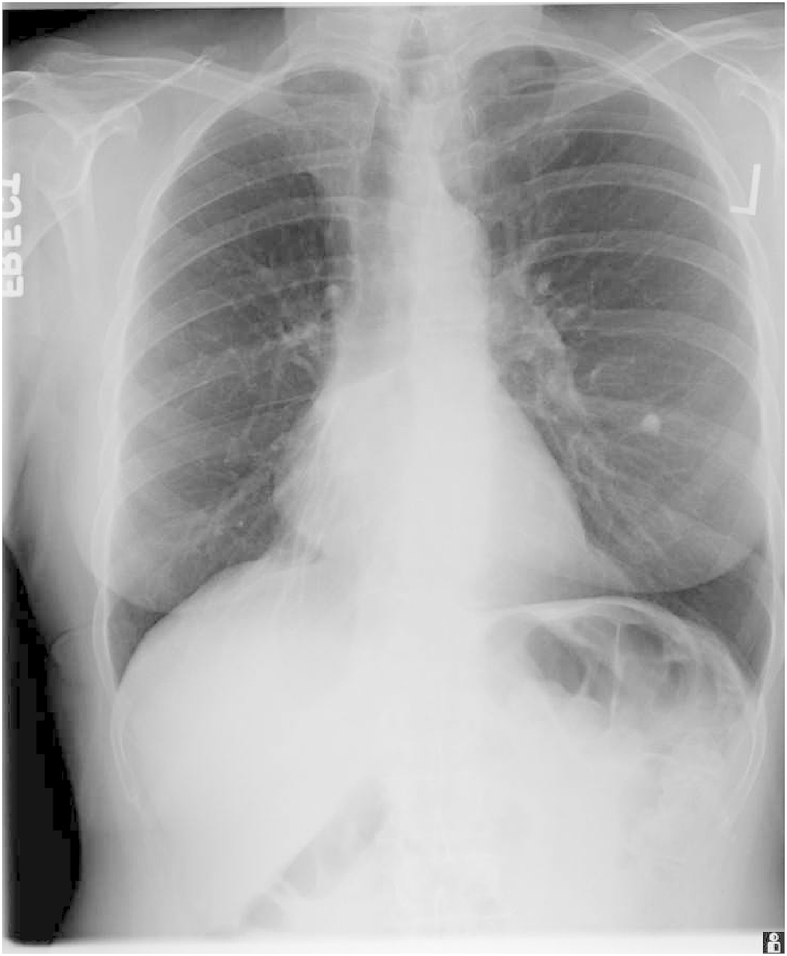
A 67 year old nonsmoker Caucasian female presented with a three year history of dry, non-productive cough without any constitutional symptoms. She did not have any history suggestive of postnasal drip, asthma or GERD. Patient denied symptoms such as fever, nights-sweats, weight loss or lack of appetite. A chest x-ray (CXR) performed three years ago (Fig. 1) at the time of cough onset had showed some streaky atelectasis in the right middle lobe area along with some right sided tracheal deviation suggestive of volume loss. No further investigations or therapies were administered at that time. She continued to cough and a repeat CXR performed a year and half later showed progression to complete right middle lobe collapse (Fig. 2). Nothing further was done given her benign clinical course. About 2 months prior to her presentation to our facility, she underwent another CXR (Fig. 2) which again showed stable right middle lobe collapse. She also underwent a bronchoscopy which apparently showed a slit like entrance to the bronchus intermedius with extrinsic compression. No endobronchial lesions were noted and the bronchial washings were non-diagnostic. She then presented to our facility for evaluation of her ‘chronic cough’. There was no history to suggest GERD, asthma or postnasal drip. She also did not have features to suggest laryngeal hypersensitivity symptoms such as allotussia and hypertussia. She was on no medications and the rest of the review of systems was entirely normal. Family history was also unremarkable. Baseline pulmonary function studies were obtained and showed mild obstruction. A chest CT scan was then performed and showed findings suspicious for a large right lower lobe lung mass causing extrinsic compression of the bronchus intermedius. A whole body PET scan was then ordered and revealed a hypermetabolic right lower lobe lung mass with possible cardiac (posterior right atrial wall) invasion. MRI brain and the PET scan were both negative for distant metastasis. Bronchoscopy was performed and showed some hypervascular mucosa at the entrance of the bronchus intermedius. Transbronchial biopsies and EBUS-guided mediastinal lymph node sampling confirmed a diagnosis of primary lung adenocarcinoma without mediastinal lymph node involvement. Thoracic surgery consultation was obtained and the patient was presented at the tumor board. A decision was made to proceed towards complete surgical excision given the excellent performance status and lack of evidence for mediastinal involvement or distant metastasis. Patient underwent a right posterior-lateral thoracotomy, mediastinal lymph node dissection, resection of a portion of her pericardium, and a right pneumonectomy. Pathology demonstrated a pT2a, pN2 well differentiated primary lung adenocarcinoma with a 3.6 cm maximal diameter. Visceral pleural invasion was seen, but bronchial margins were negative. Adjuvant radiation was not given due to risk of pneumonectomy stump non-healing and possible necrosis. Patient recovered well from the procedure and was discharged 3 days after the pneumonectomy. She declined adjuvant chemotherapy due to personal reasons.
Fig. 1.
Initial chest X-ray.
Fig. 2.
Chest X-ray done 1½ and 3 years later.
2. Discussion
Chronic cough is often the only symptom of underlying lung pathology. This case is unique because of the finding of an advanced primary lung adenocarcinoma in a non-smoker with a 3 year history of chronic cough without other systemic or pulmonary manifestations. Most patients with a primary lung malignancy present with cough along with other symptoms such as chest pain, dyspnea, hemoptysis or systemic symptoms such as weight loss and loss of appetite. In addition, more than 80% of primary lung cancers are found in smokers. An abnormal chest X-ray (CXR) or CT scan usually provides the first hint of the underlying problem. In this case the CXR showed stable findings of middle lobe collapse for more than 1 year before the correct diagnosis was made. Moreover, the CXR showed no hint of a lung mass or other sinister pathologies that would have prompted further imaging studies.
Lung cancer remains the leading cause of cancer related mortality in both men and women with more than 150,000 deaths occurring per year from this disease [1], [2]. Several studies have investigated the delay from onset of symptoms to the eventual diagnosis of lung cancer [3], [4], [5]. For instance Walter and colleagues reported that only half of patients with lung cancer presented with a single discrete symptom [3]. The vast majority developed multiple symptoms such as hemoptysis, dyspnea, chest/shoulder pain, decreased appetite, unexplained weight loss, cough or fatigue before the diagnosis of lung cancer was eventually made. Their study also found that hemoptysis was the only symptom that was specific for a diagnosis of lung cancer as compared to other non-malignant pulmonary conditions. In addition, they found that ‘time to diagnosis’ of lung cancer averaged about 3 months from the first appearance of symptoms. A similar study by Lovgren showed that there were significant delays between symptom onset and eventual referral/diagnosis of lung cancer [4]. Similar to our case, there were several patients reported in their study that had delays of 1–2 years between symptom onset and diagnosis because of ‘stable’ chest x-ray changes. They also found that the presence of ‘tumor specific’ symptoms such as a lump, neurologic symptoms, hemoptysis, appetite loss and non-thoracic pain were associated with shorter times to diagnosis. In both these studies, cough was present in a majority of patients. Similarly, the study by Corner and colleagues again showed that cough (along with fatigue) was the most common symptom noted in about 68% of patients [5]. They found that symptoms preceded lung cancer diagnosis by a median of 12 months (range 4 months- 2 years). They also noted a median delay of 7 months between the first changes in health status to the onset of symptom(s) that prompted the patient to seek medical care. In addition, they found that patients who were evaluated by their primary care physicians had significantly less diagnostic delay. The ACCP published an evidence based clinical practice guideline on the relationship between chronic cough and lung tumors. They found that cough was present in more than 65% of patients at the time of lung cancer diagnosis [6]. However, the study also found that less than 2% of chronic cough patients had lung cancer as the underlying cause. Thus it appears that isolated chronic cough as a presenting symptom of lung cancer is indeed very rare.
3. Conclusion
In conclusion, we present a rare and unusual case of lung adenocarcinoma in a non-smoking female presenting with the isolated symptom of chronic cough of 3 years duration. The diagnostic delays in this case were likely caused by her non-specific presentation, lack of tumor specific or alarming symptoms such as hemoptysis or unintentional weight loss. Clinicians need to be very mindful of these pitfalls and should maintain a very low threshold for performing definitive diagnostic studies in uncertain situations.
Funding
None.
Disclosure
None for all authors.
References
- 1.Molina J.R. Non-small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin. Proc. 2008;83(5):584–594. doi: 10.4065/83.5.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldstraw P. Non-small cell lung cancer. Lancet. 2011;378:1727–1740. doi: 10.1016/S0140-6736(10)62101-0. [DOI] [PubMed] [Google Scholar]
- 3.Walter F.M. Symptoms and other factors associated with time to diagnosis and stage of lung cancer: a prospective cohort study. Br. J. Cancer. 2015;31(112):30. doi: 10.1038/bjc.2015.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lovgren M. Time spans from first symptom to treatment in patients with lung cancer-the influence of symptoms and demographic characteristics. Acta Oncol. 2008;47:397–405. doi: 10.1080/02841860701592392. [DOI] [PubMed] [Google Scholar]
- 5.Corner J. Is late diagnosis of lung cancer inevitable? Interview study of patients' recollections of symptoms before diagnosis. Thorax. 2005;60(4):314–319. doi: 10.1136/thx.2004.029264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kvale P. Chronic cough due to lung tumors. ACCP evidence-based clinical practice guidelines. CHEST. 2006;129:1478–1538. doi: 10.1378/chest.129.1_suppl.147S. [DOI] [PubMed] [Google Scholar]